
















 |
 |
 |
|||
 |
 |
 |
 |
 |
|
 |
 |
 |
 |
||
 |
 |
 |
 |
||
 |
 |
 |
|||
 |
 |
 |
|||
 |
 |
 |
|||
 |
 |
 |
|||
 |
|||||
Loss of Buccal and Palatal Plates
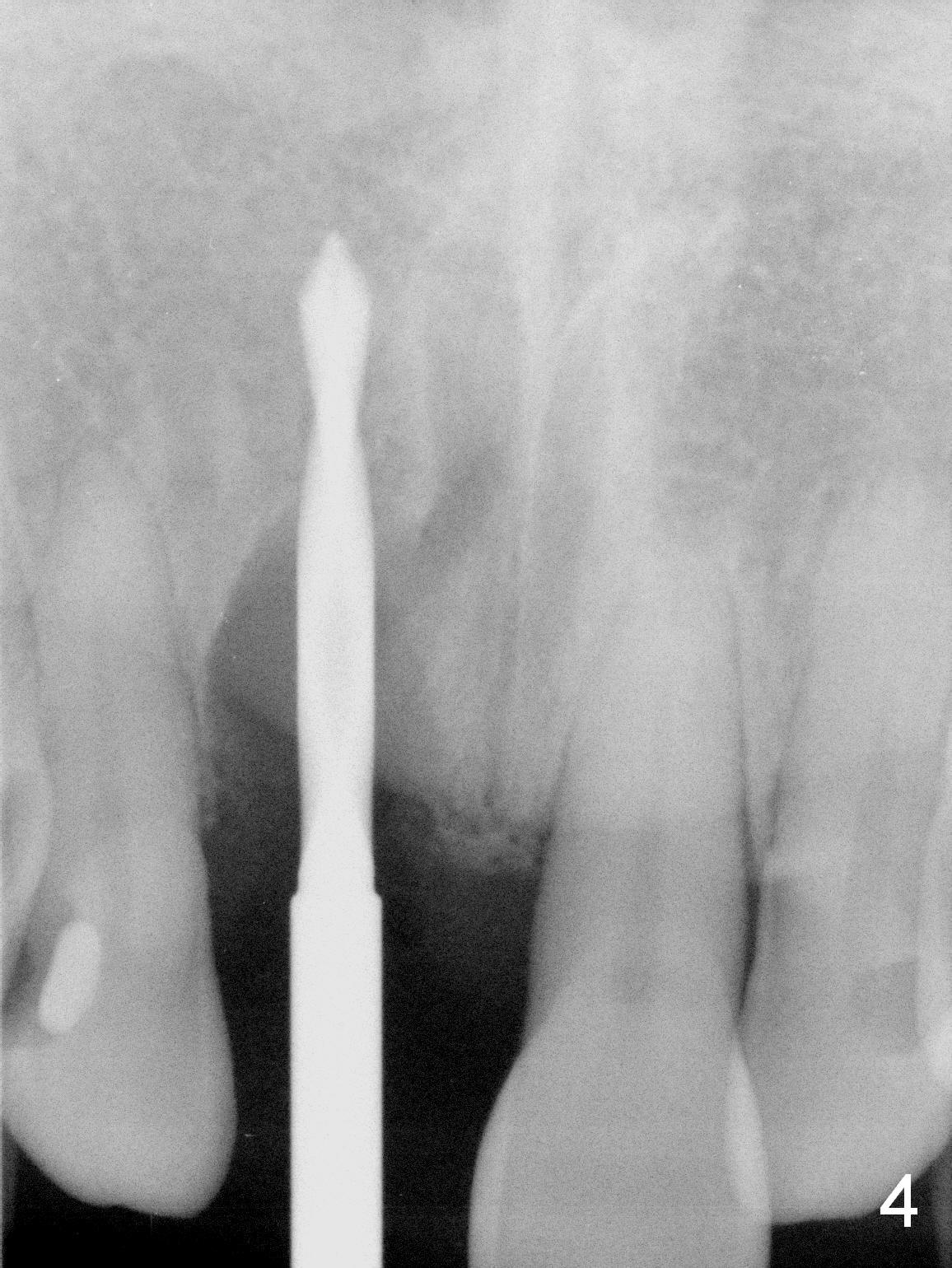
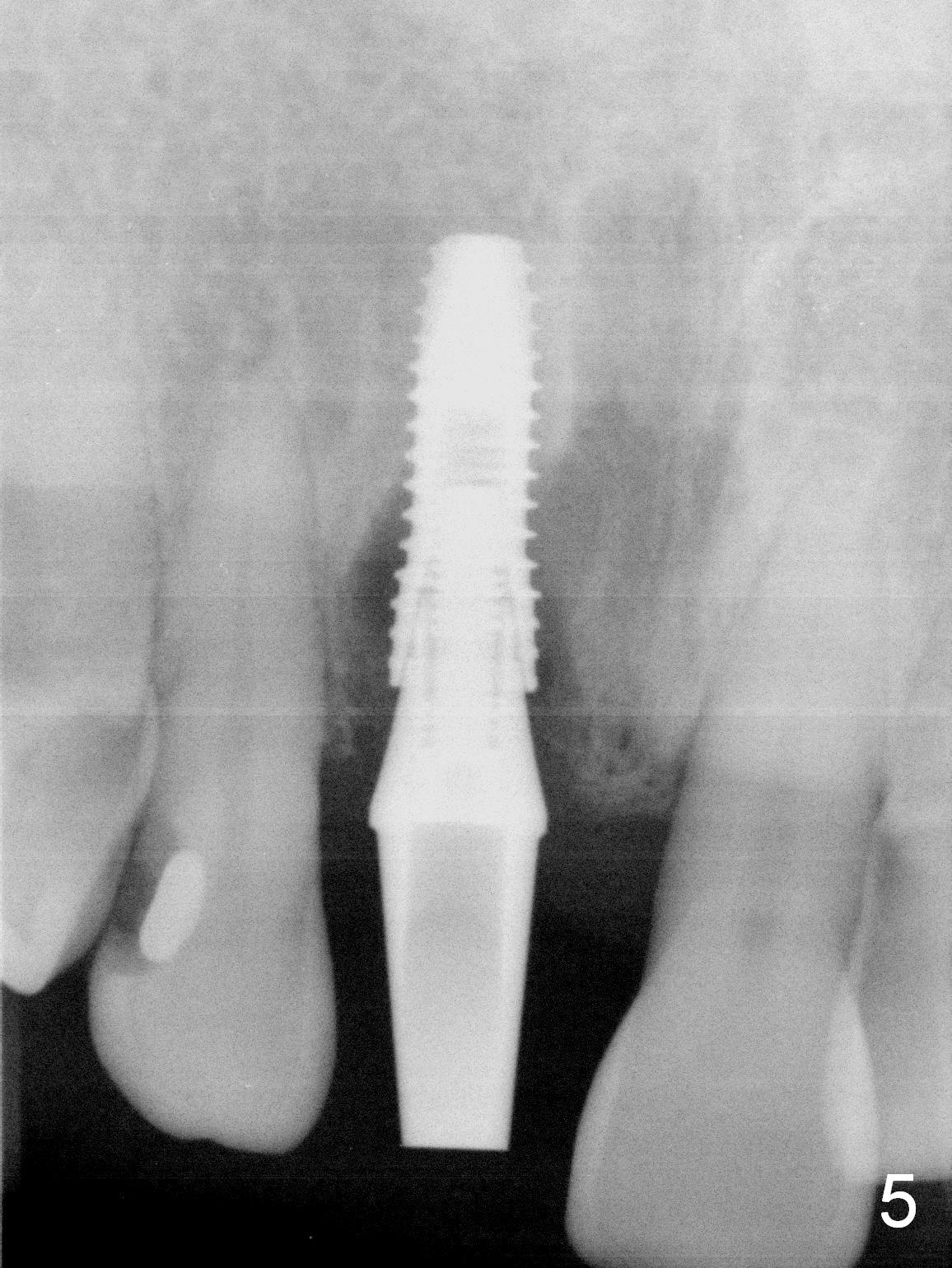
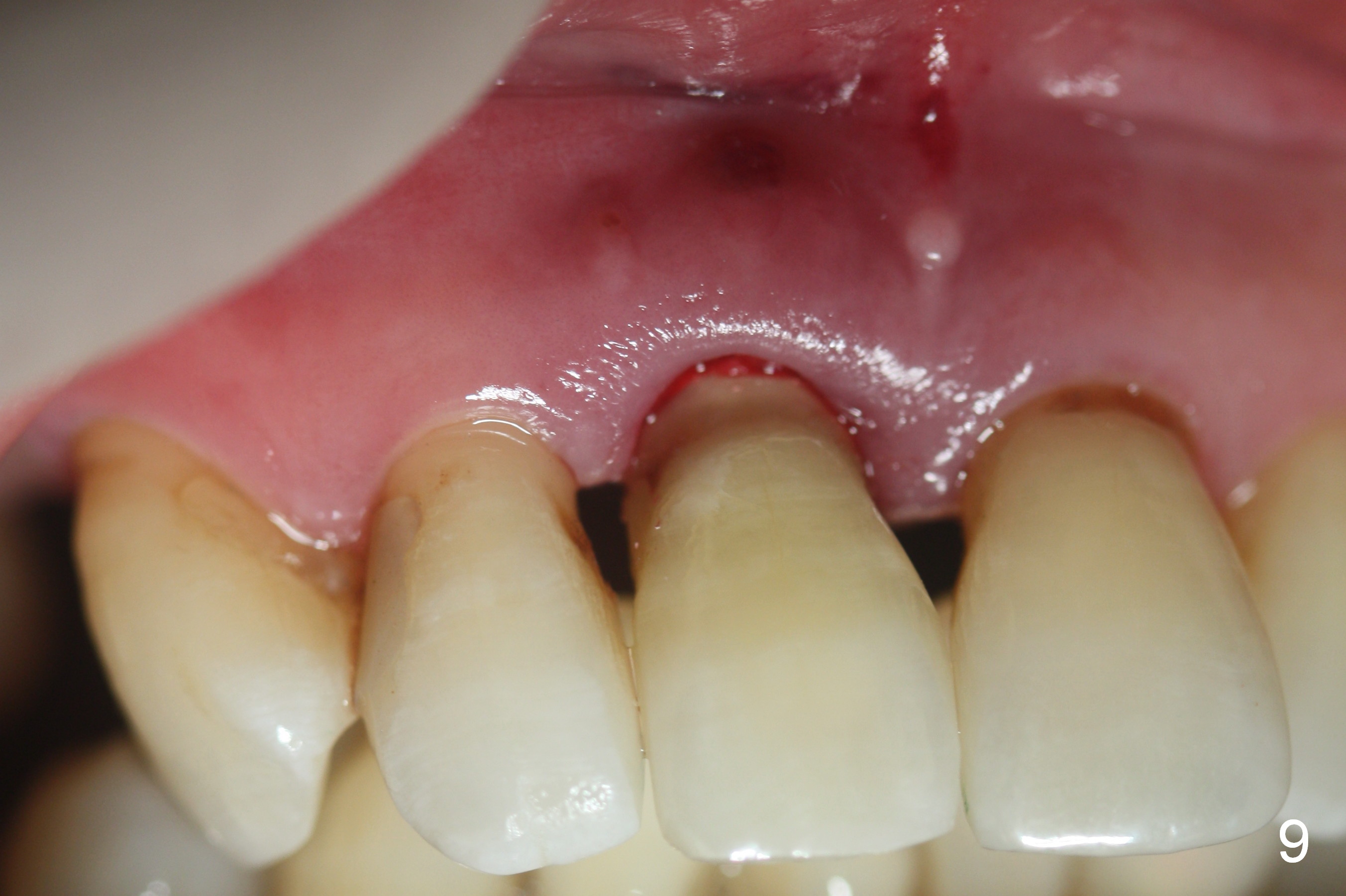
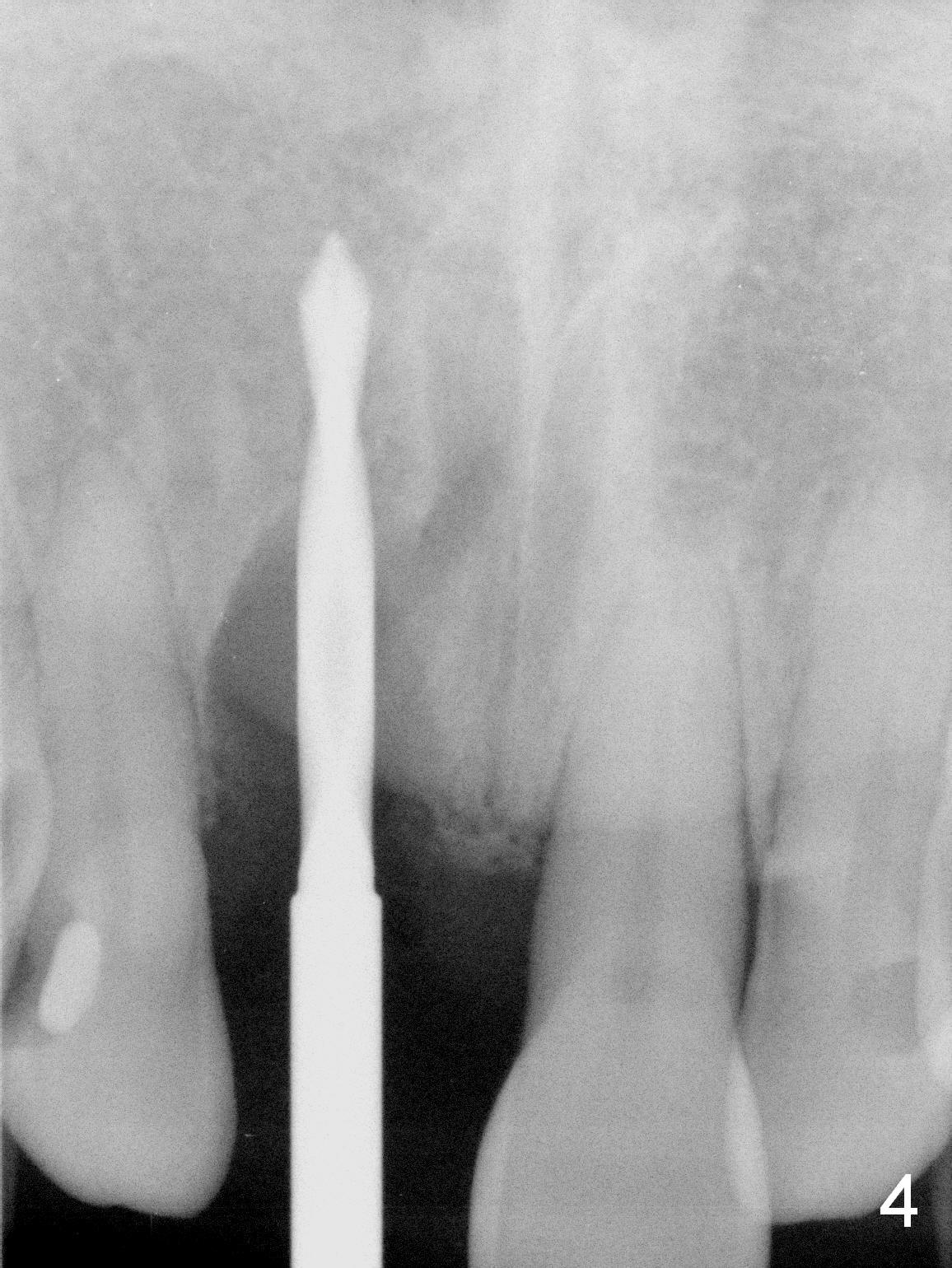
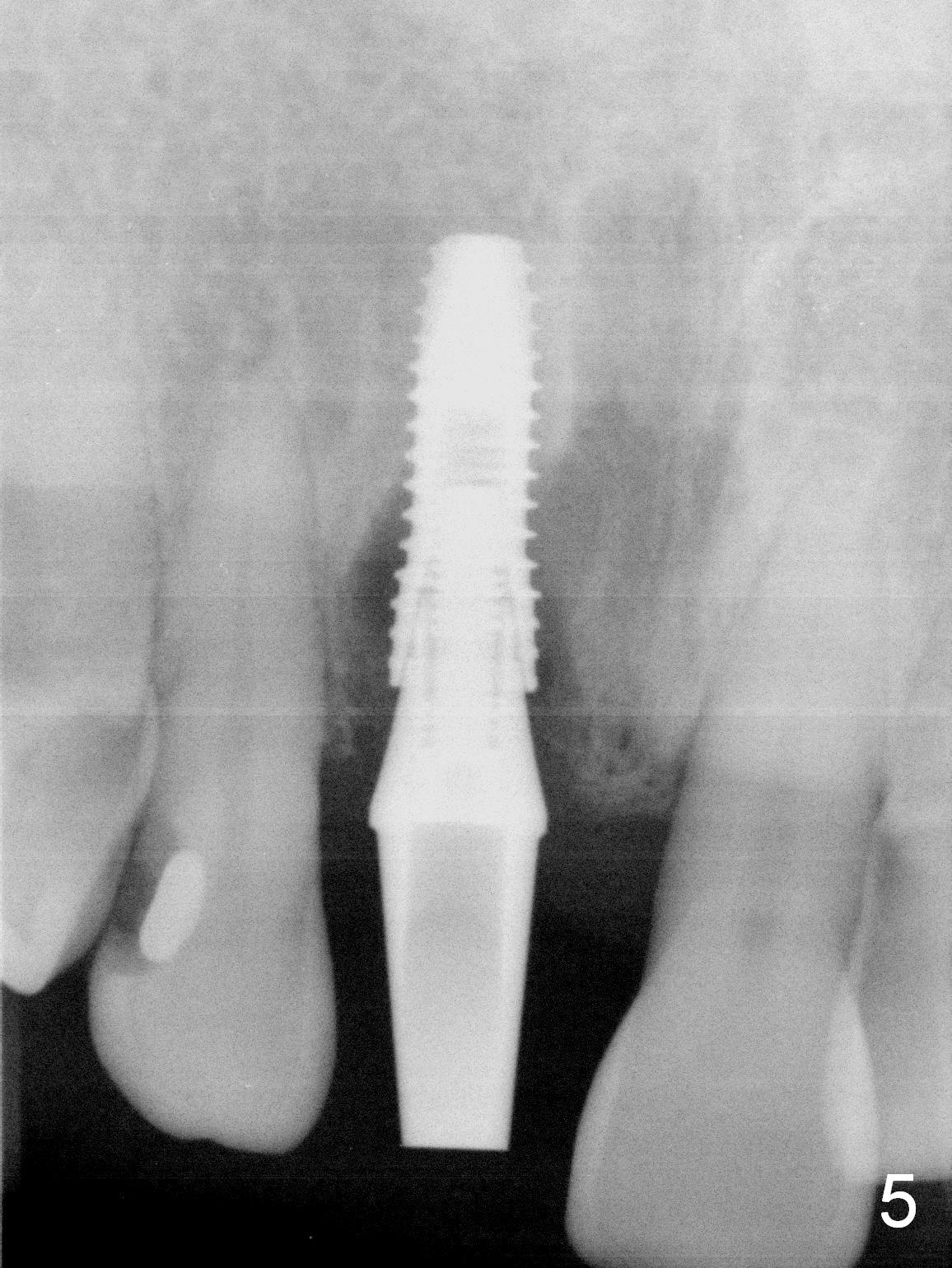
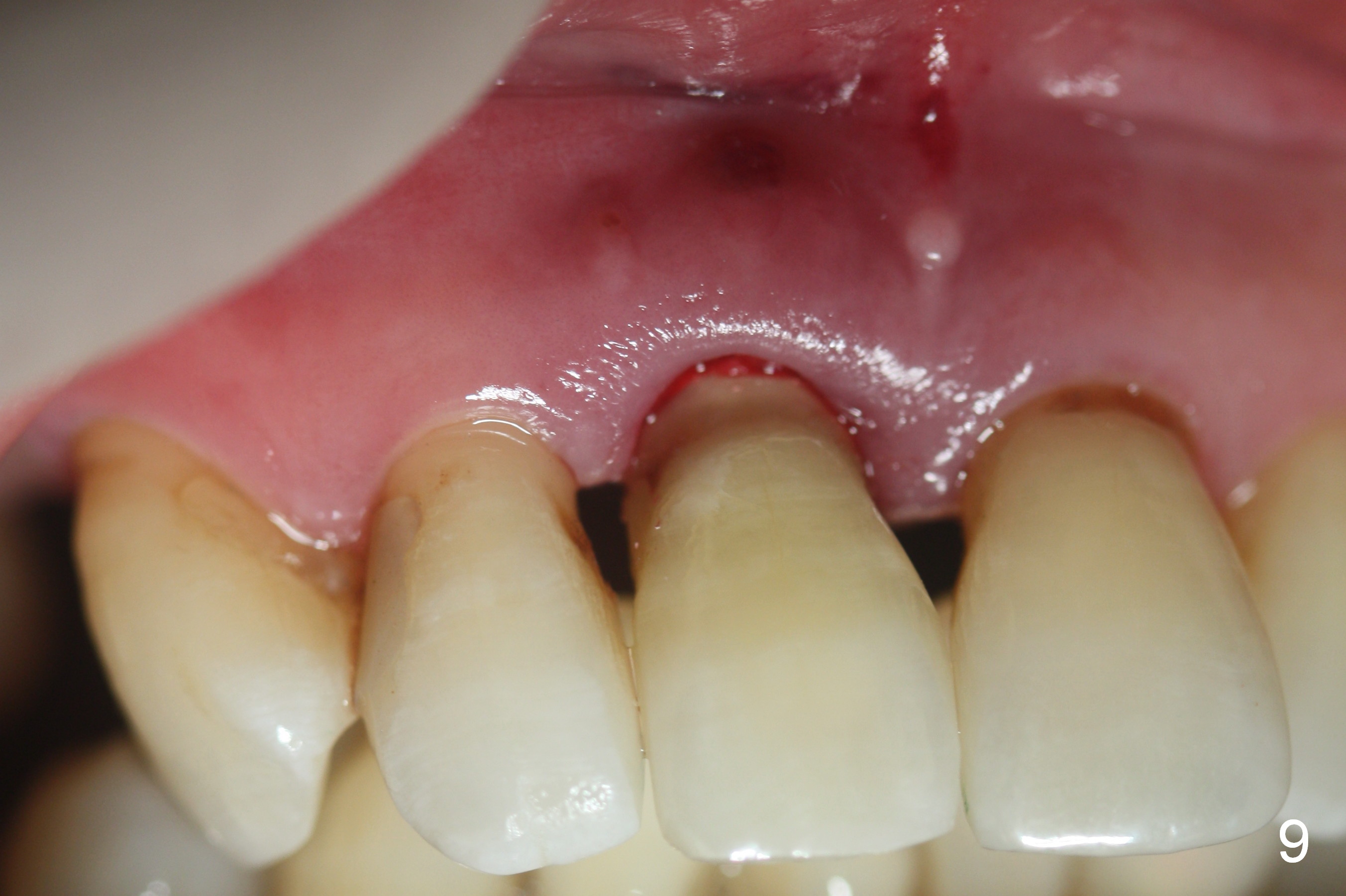
Fig.1,2 show the buccally displaced the tooth #8 with anterior deep over bite and overjet. The palatal gingival recession (Fig.3 *) is more severe than the buccal one (Fig.1). After extraction, there is ~7 and 3 mm loss of the buccal and palatal plates, respectively. Osteotomy is initiated with a 2 mm pilot drill in 6 mm native bone (Fig.4). After using 2.5 mm reamer for 3 mm (underprep), a 3.8x11.5 mm is placed with ~ 35 Ncm, followed by placement of a 4.5x15° (3 mm A) angled abutment (Fig.5). Clinically, the implant/abutment complex is buccally positioned. After removal of the abutment, the implant is backed up and re-directed palatally. When the angled abutment is re-inserted, the position of the implant/abutment complex is more favorable for restoration. The abutment is removed again; with a small piece of gauze in the implant well, the buccal and palatal plate defect is repaired with PRF and allograft (Fig.6 *) internally (through the socket, flapless). The angled abutment is re-inserted, hand tightened, prepared (from Fig.5 to Fig.6-8) and adapted to the crown shell (Fig.9). Before temp bond cementation, more bone graft and collagen plug (trimmed) are inserted in the remaining socket gap. Finally periodontal dressing is applied. To alleviate the deep bite, the incisal edge of the 2 opposing incisors is reduced prior to insertion of the crown shell.
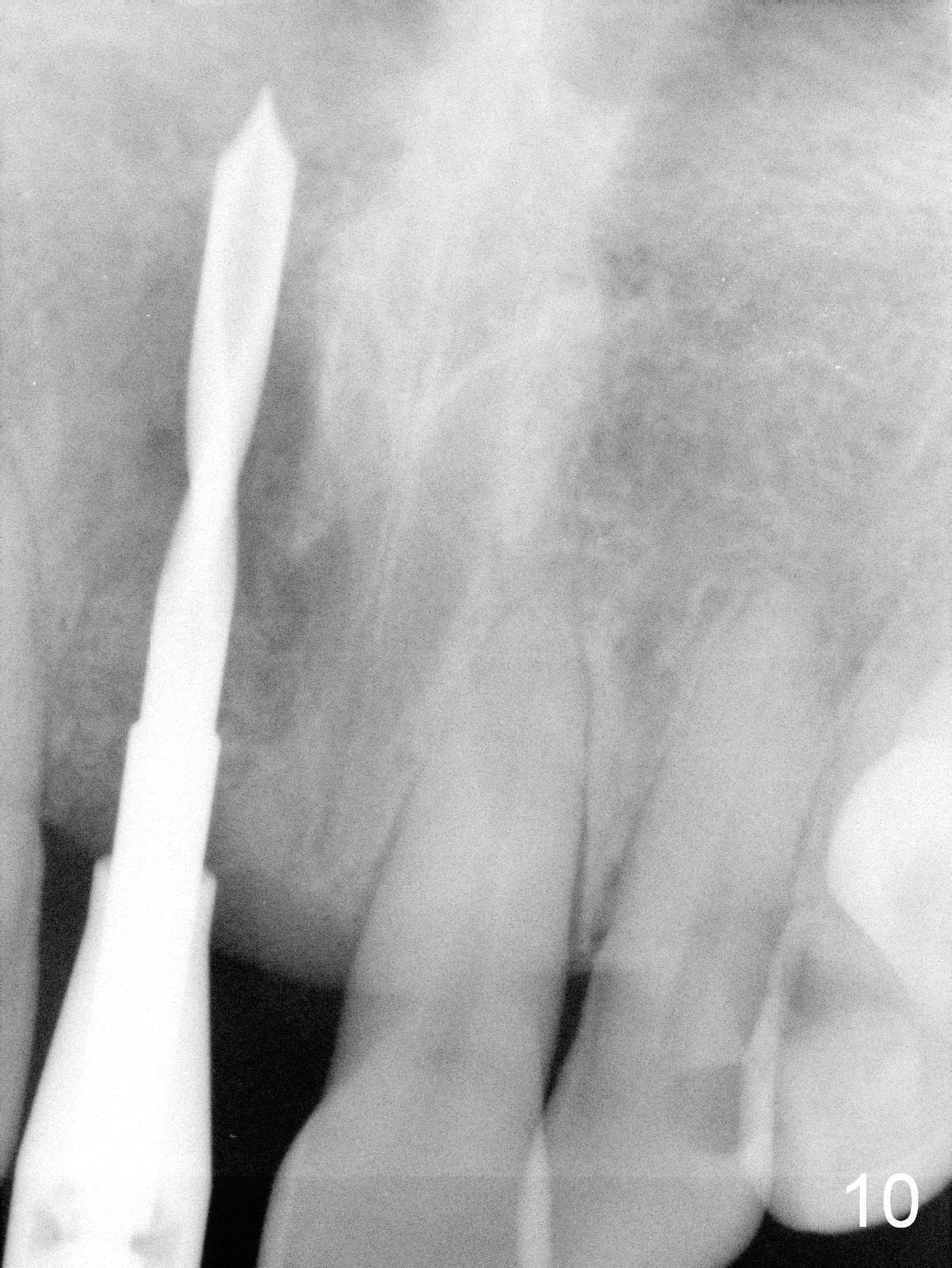
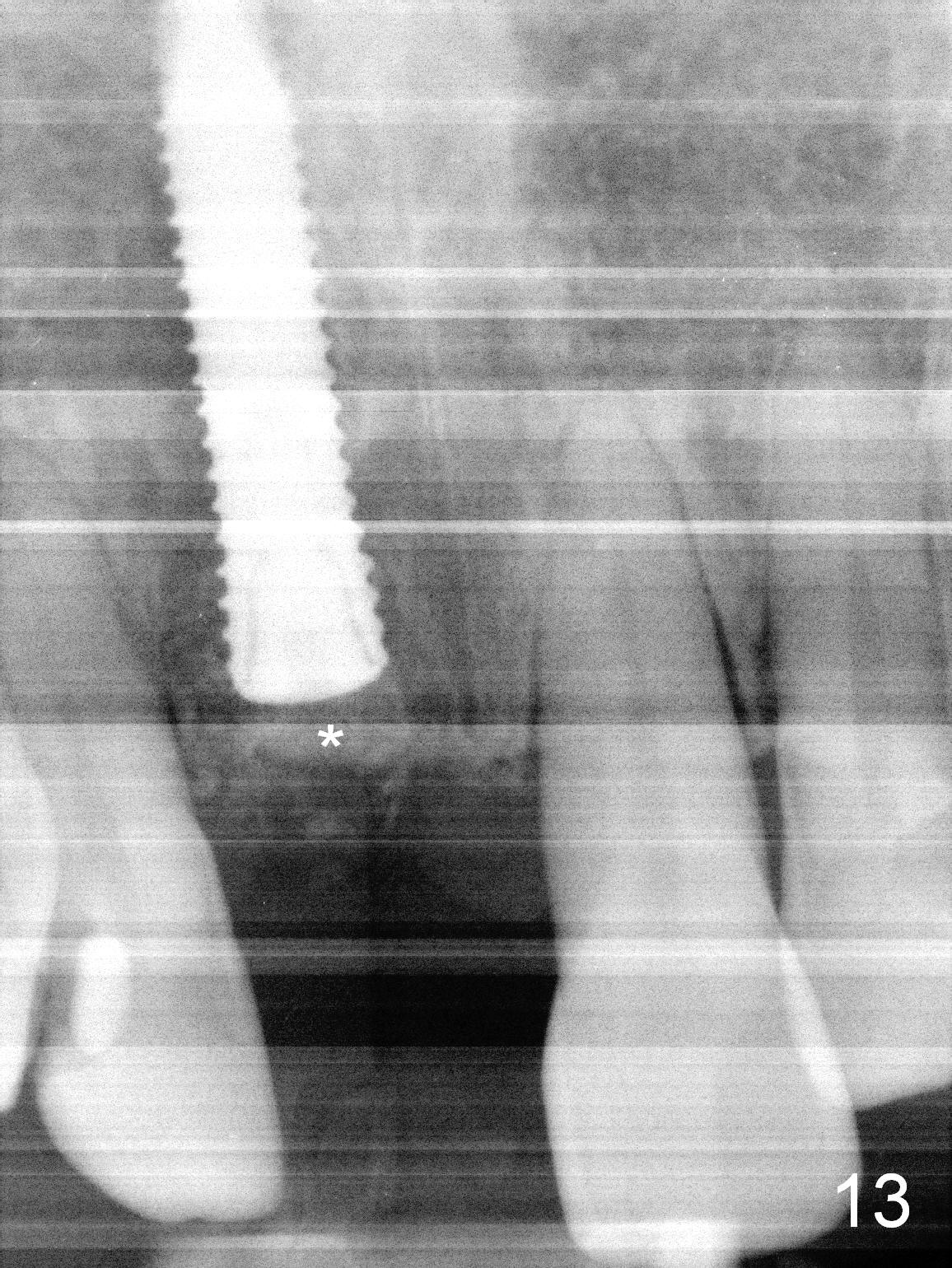
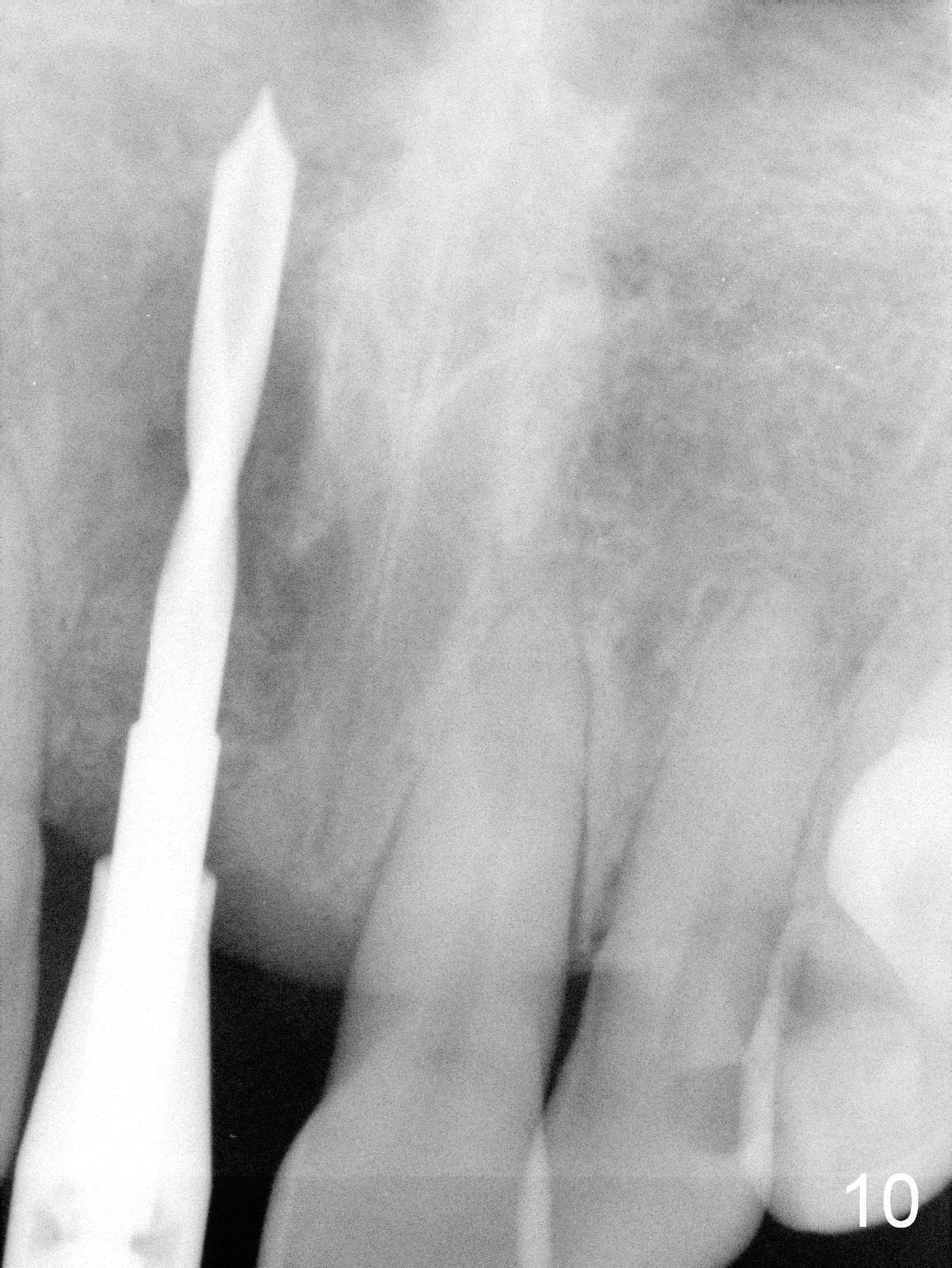
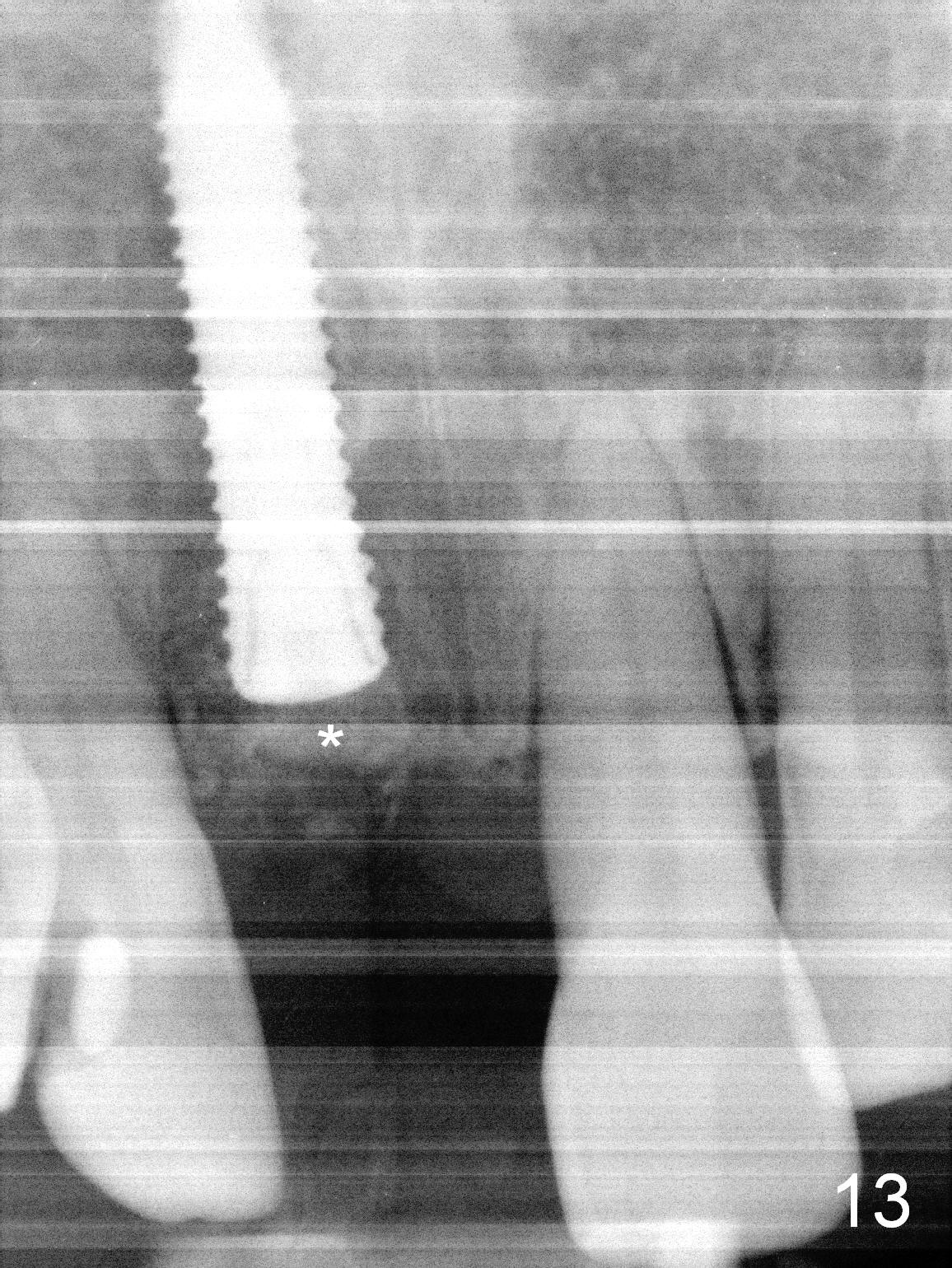
Twenty days postop, the implant is found to be loose and removed. It appears that deep bite, short implant (11 mm), osteoporosis and change in implant position in the previous placement are unfavorable factors. What can be changed now is an increase in the depth of osteotomy (Fig.10: 20 mm) and implant diameter (Fig.11-13:4 mm). It appears that the 4x18 mm implant is placed in a wrong position or direction with minimal stability (Fig.11) after 2 mm pilot drilling. The bone is soft. When a 3x18 mm drill is used in a more definitive palatal and mesial direction with apparent penetration of the relatively solid nasal floor, the stability of the re-inserted implant increases (~35 Ncm) with shallower placement (Fig.12: double arrows, as compared to Fig.11, to reduce blockage of the nasolacrimal duct). No bone graft is used for nasal floor lift (to reduce the chance of nasolacrimal duct blockage) prior to implantation. Instead bone graft is added mainly buccally after implantation (Fig.13 *, as compared to the old one in Fig.12 *).
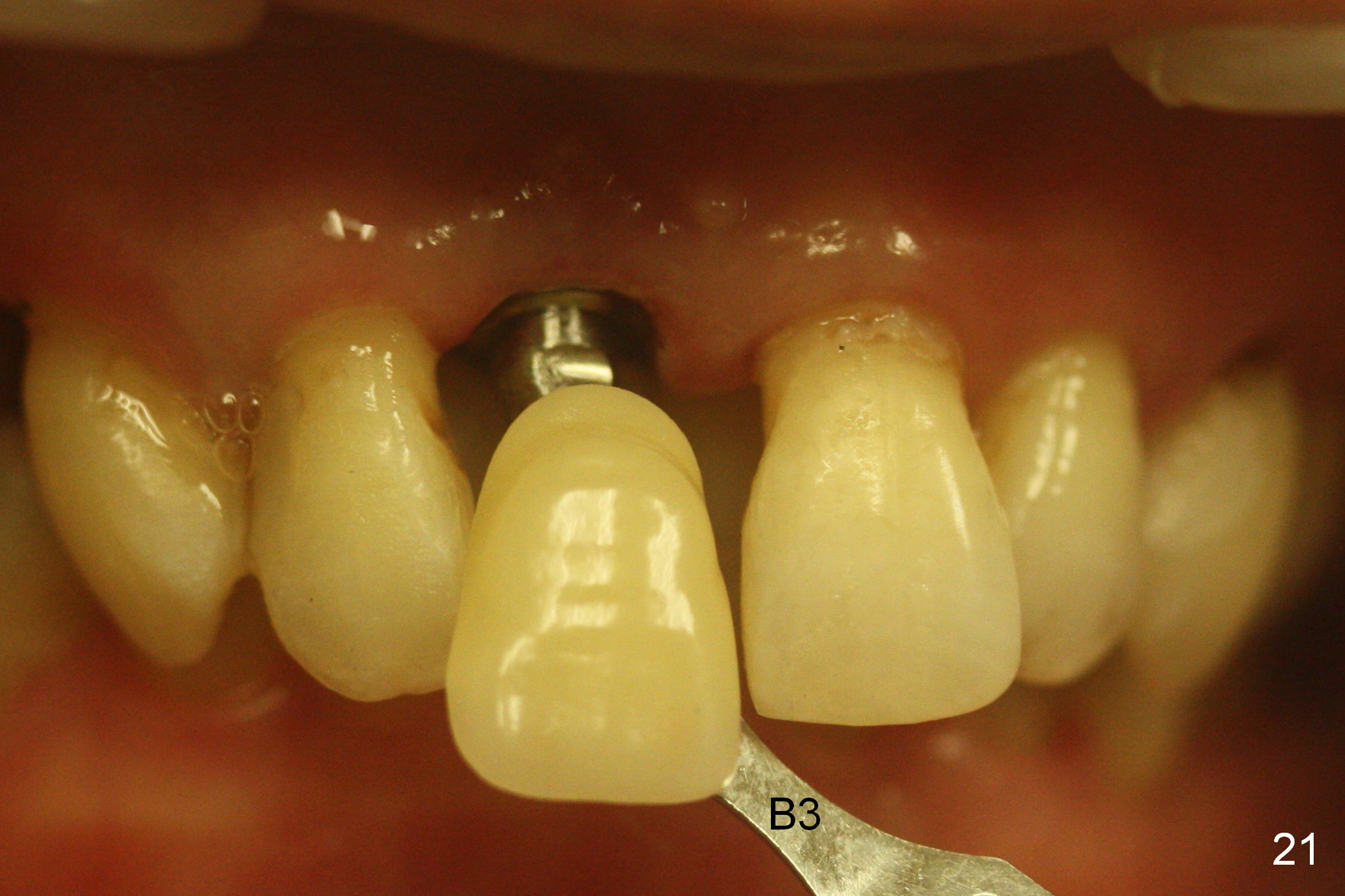
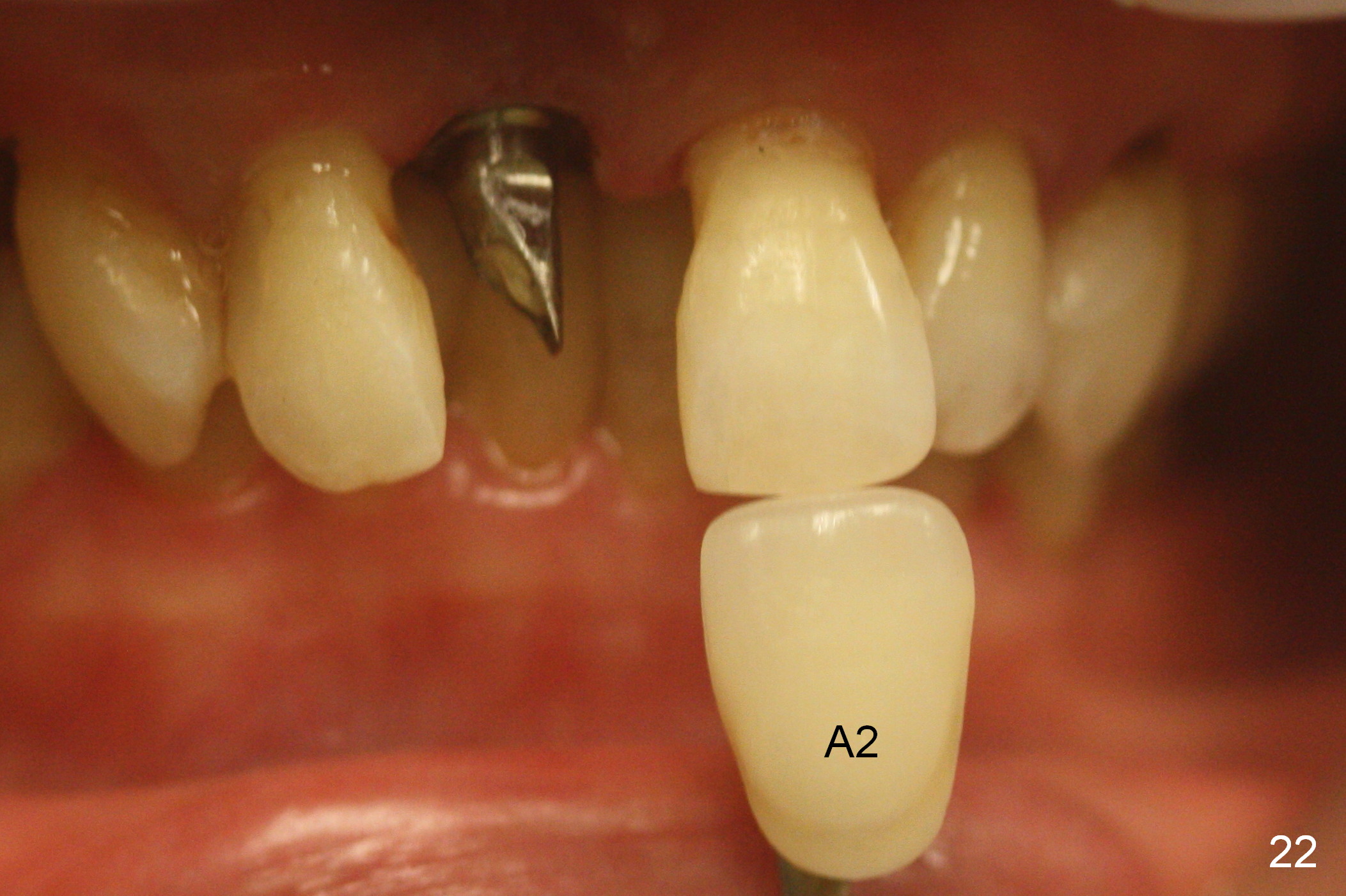
Five weeks post 2nd implant placement, the osteotomy opening has healed. After Cetacaine topical application, use an explorer to penetrate the gingiva and remove the underlying healing screw. A 4.5x7(3) mm cemented abutment is placed. Clearance from the lower incisor is provided by grinding the palatal surface of the abutment at the cervix (Fig.14). In addition, the palatal cervical extension is intentionally trimmed short of the early provisional (crown shell) (Fig.14,15). In contrast, there is no metal exposure labially (Fig.16). Fig.14-16 are taken 1 week after provisionalization. The crown shell cracks buccally (Fig.17 >) and palatally (Fig.18 <) 1.5 months post 2nd implant placement. It suggests magnitude of mastication force associated with deep bite.
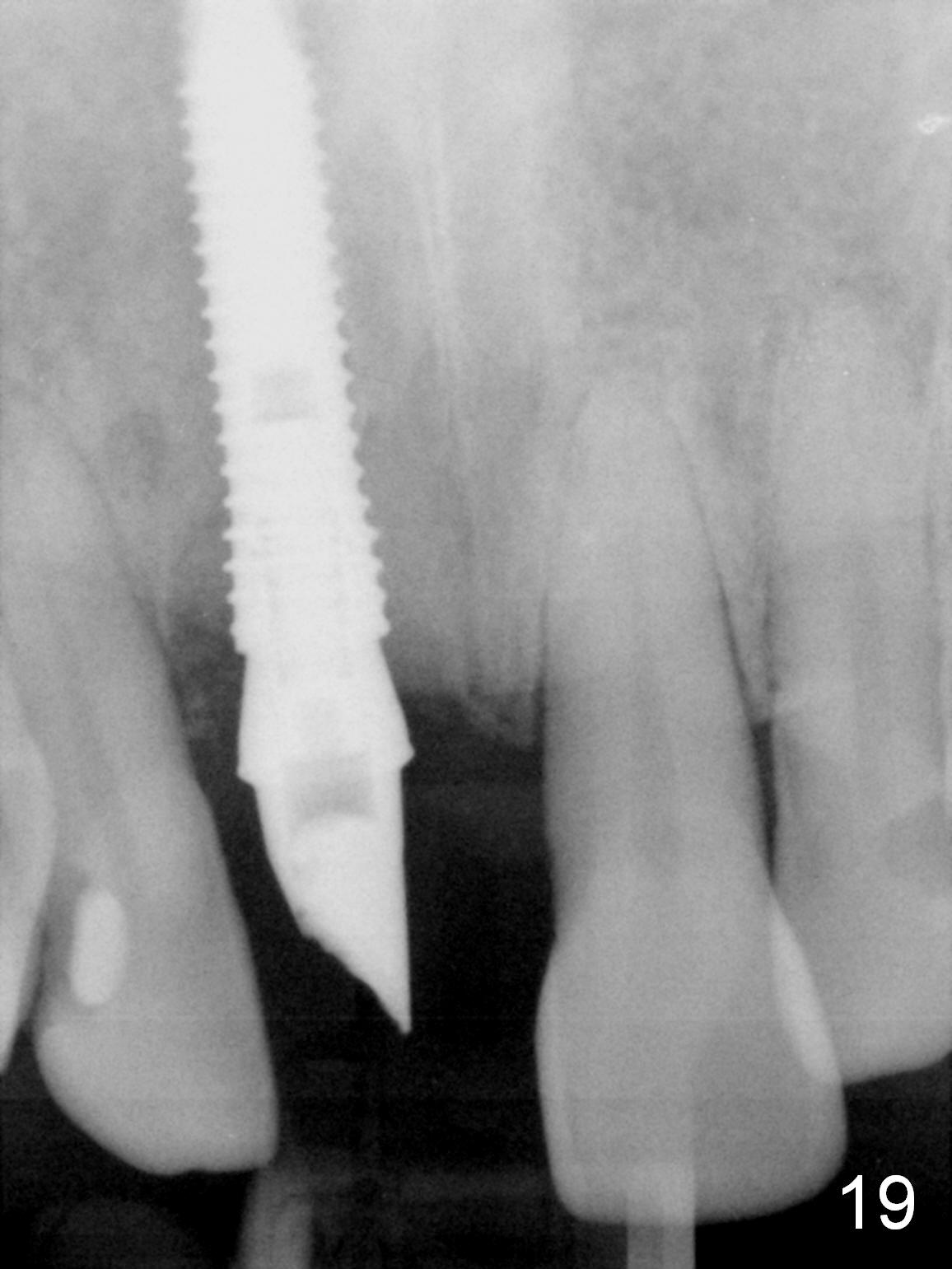
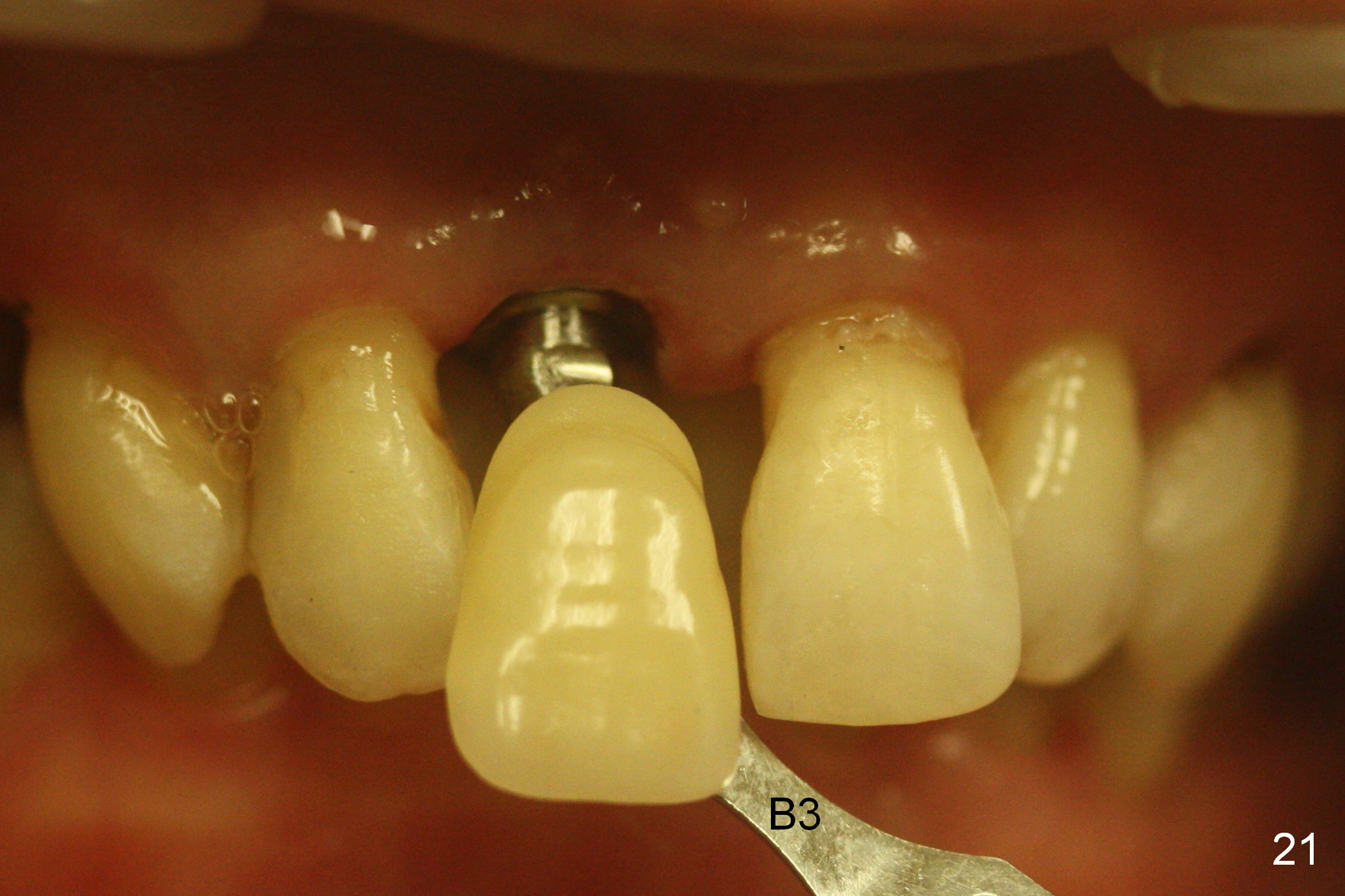
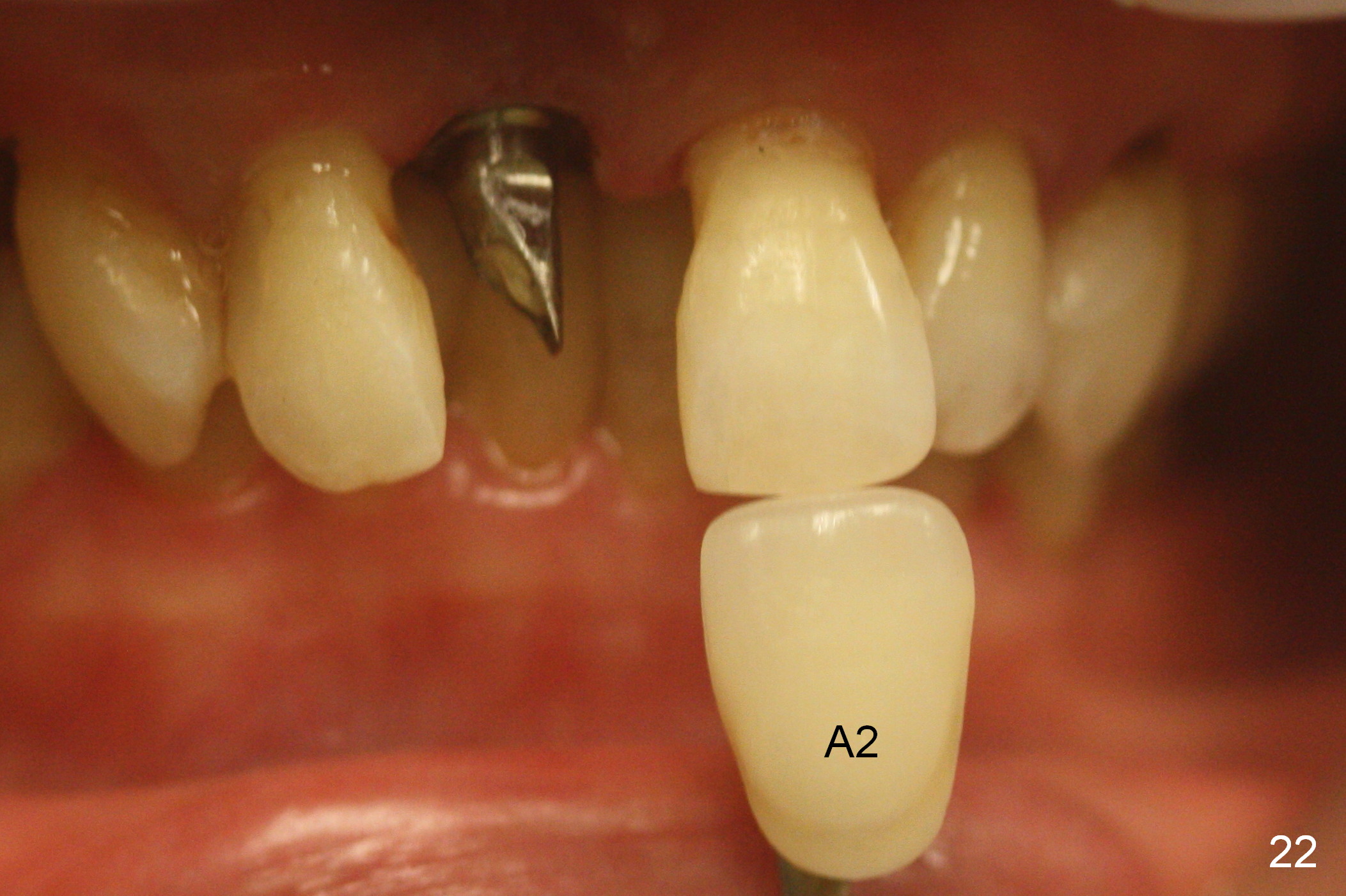
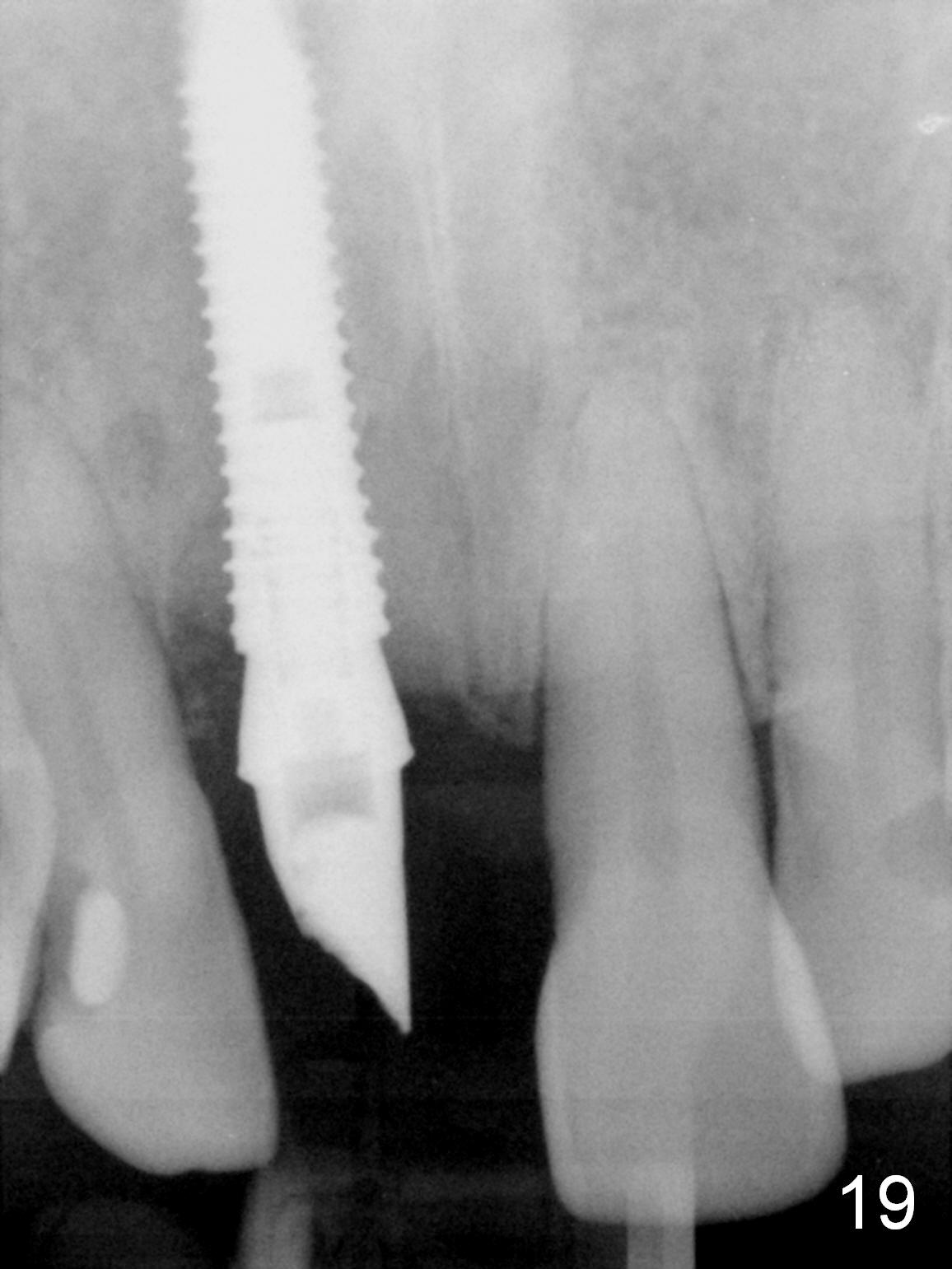
The repaired crown shell re-fractures 5 days later (<3 months postop). The implant appears to have been osteointegrated (Fig.19). Impression is taken for definitive restoration with intention to have palatal margin relief (Fig.14).
Also make a palatal access hole in the crown so that the abutment screw can be tightened after cementation in mouth (Fig.20 arrowheads).
Fig.23 and 24 (palatal access) show the crown after cementation before torque.
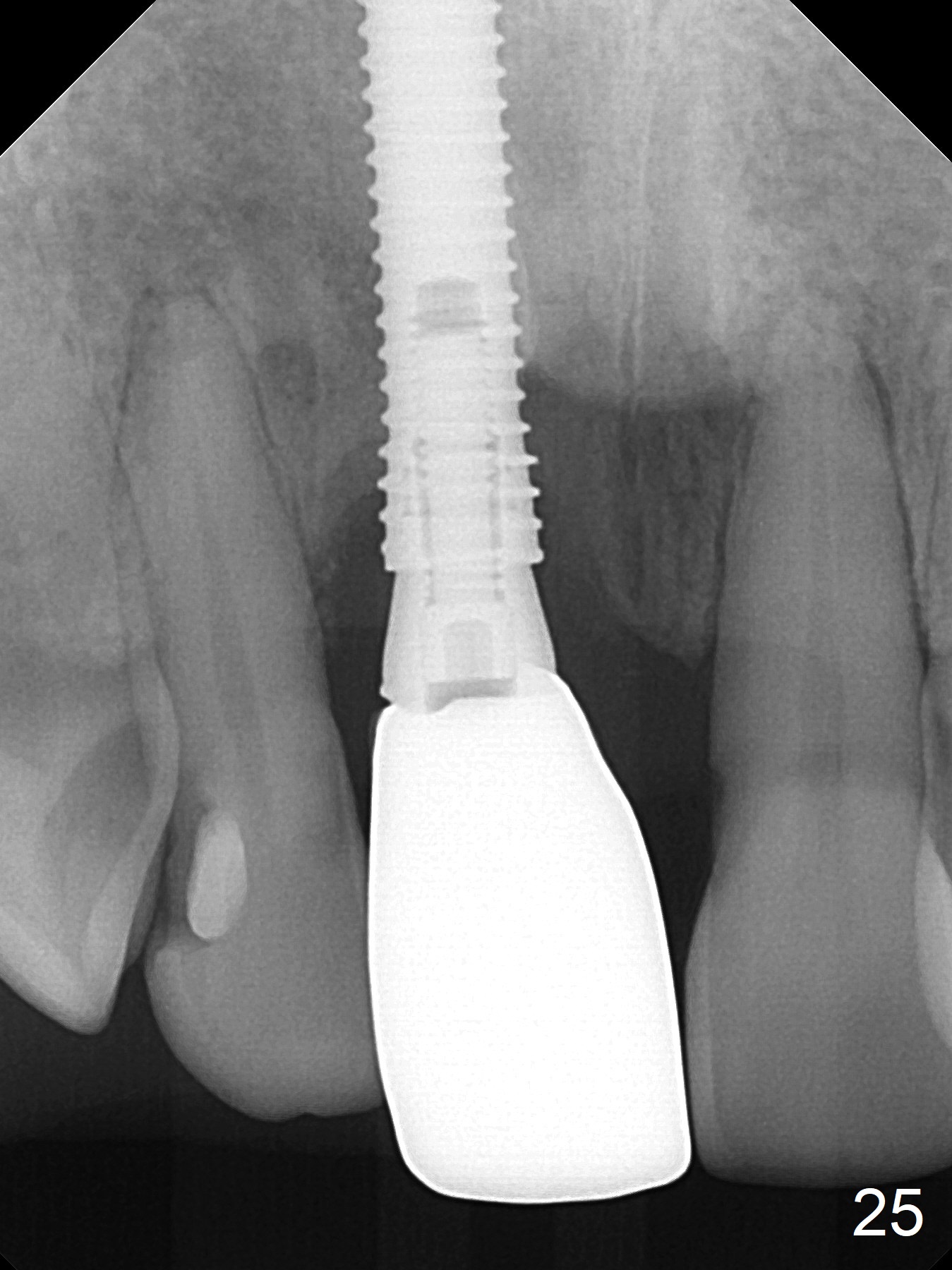
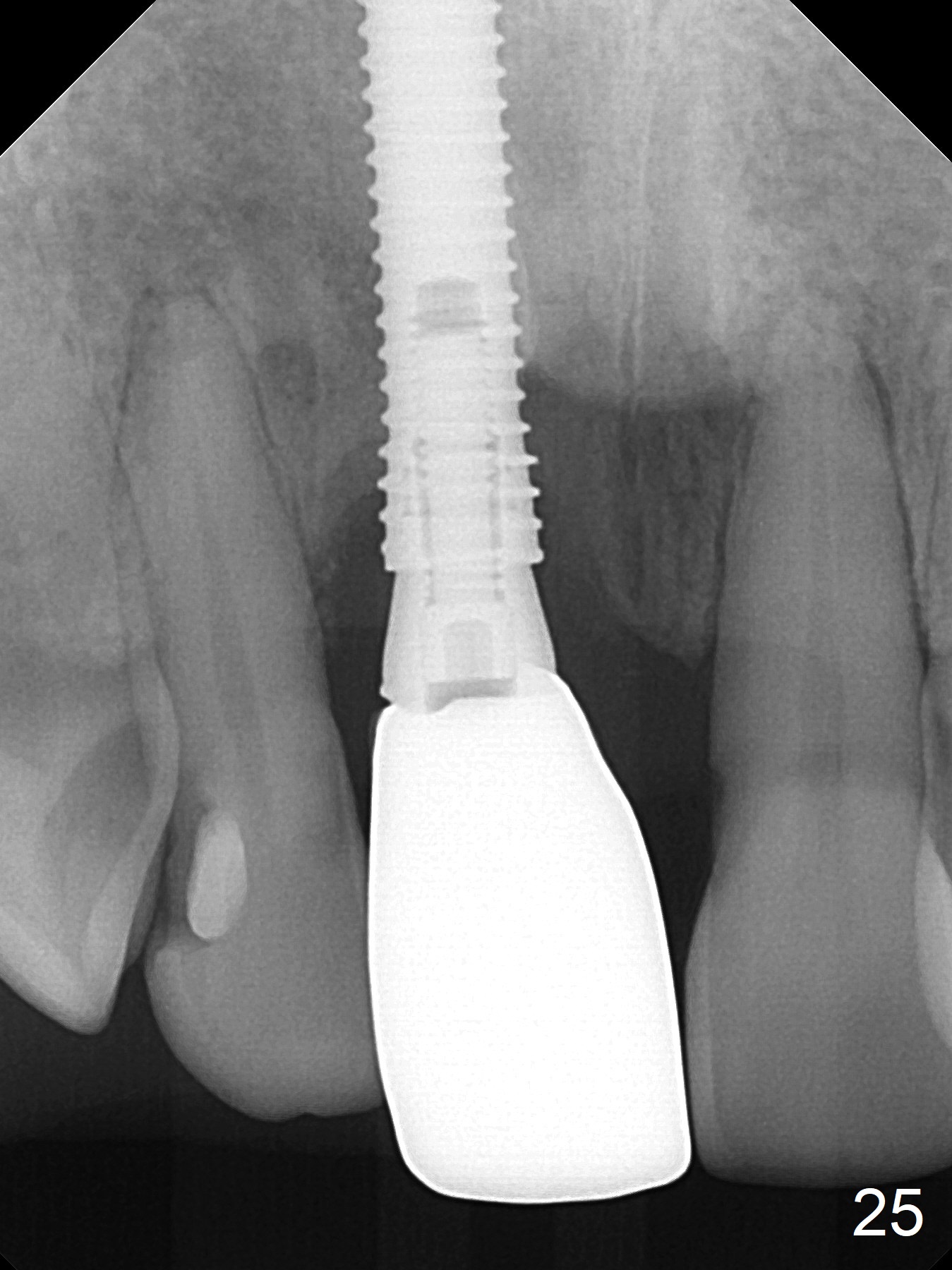
Bone defects appears to have reduced 1 year post comentation (Fig.25). The patient is satisfied with the appearance improvement over rotation (Fig.26, as compared to Fig.2,3). The cosmetics and deep bite remains the same, while more of the abutment is covered by the palatal gingiva 4 years post cementation (Fig.27-29).
Return to Upper Incisor Immediate Implant
Chinese
Xin Wei, DDS, PhD, MS 1st edition 04/26/2016, last revision 09/16/2020