











 |
 |
 |
||
 |
 |
 |
 |
|
 |
 |
 |
 |
|
 |
 |
 |
||
 |
 |
 |
||
 |
 |
|||
Immediate Implant in Soft Bone
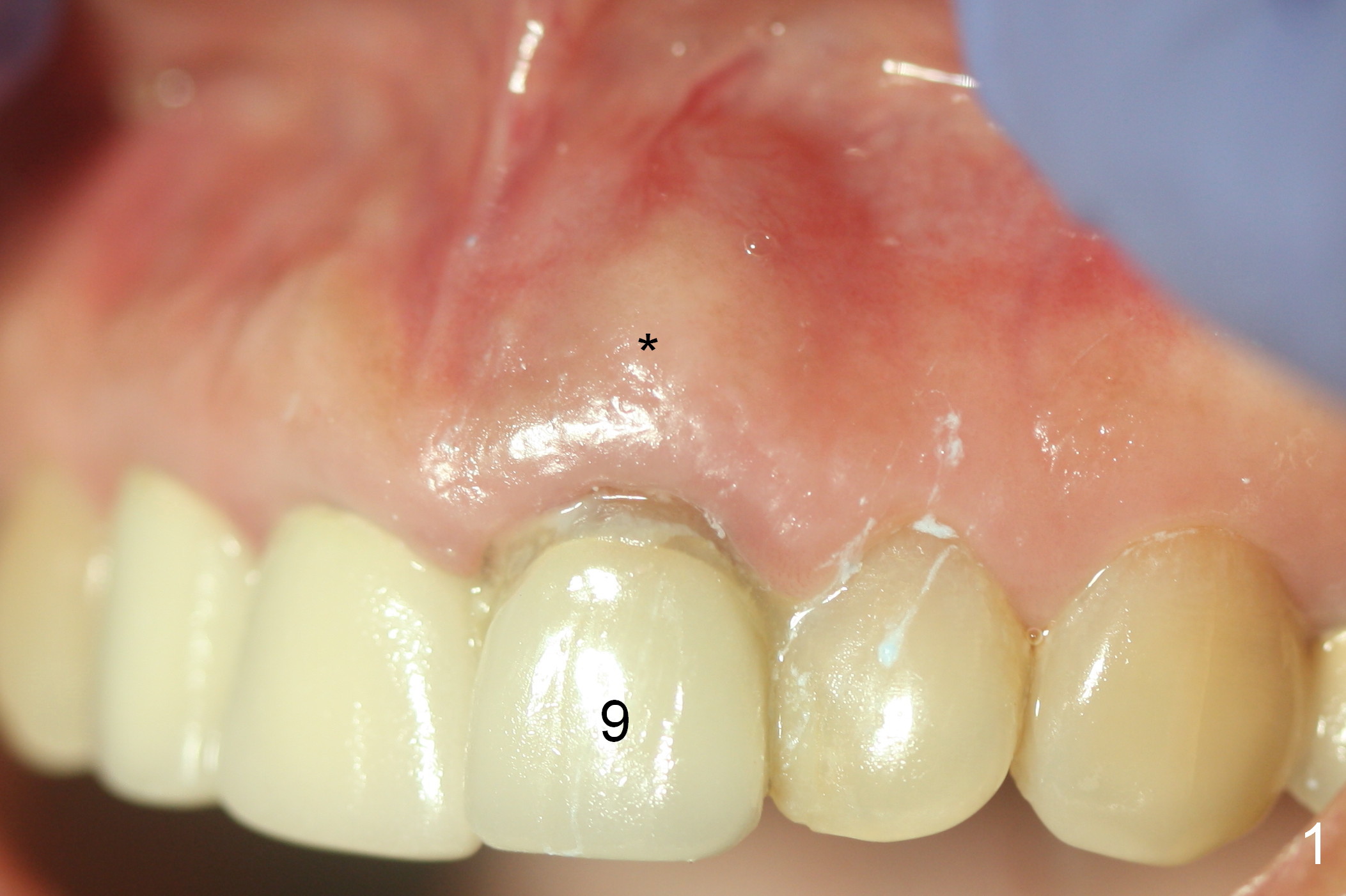
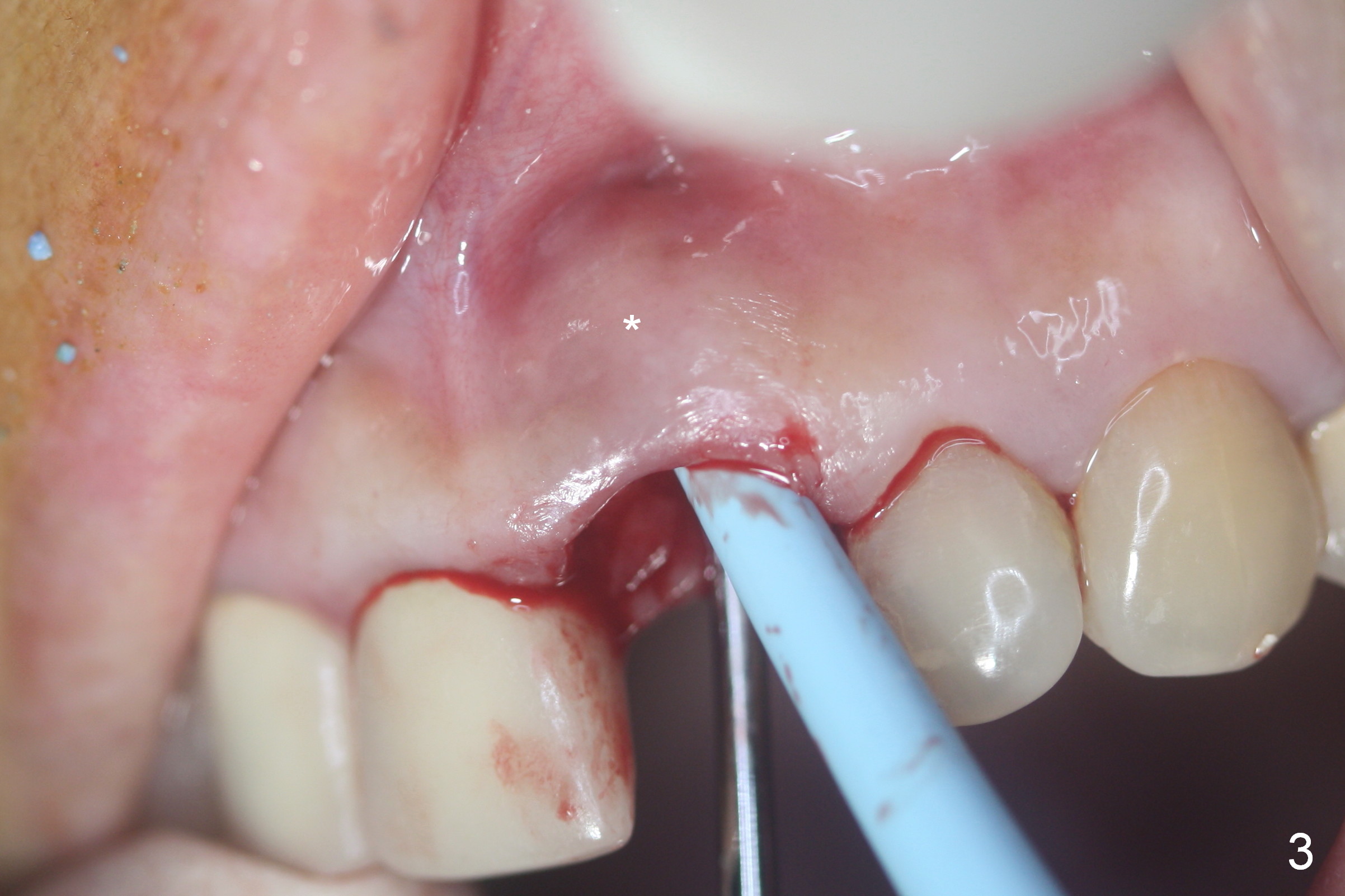
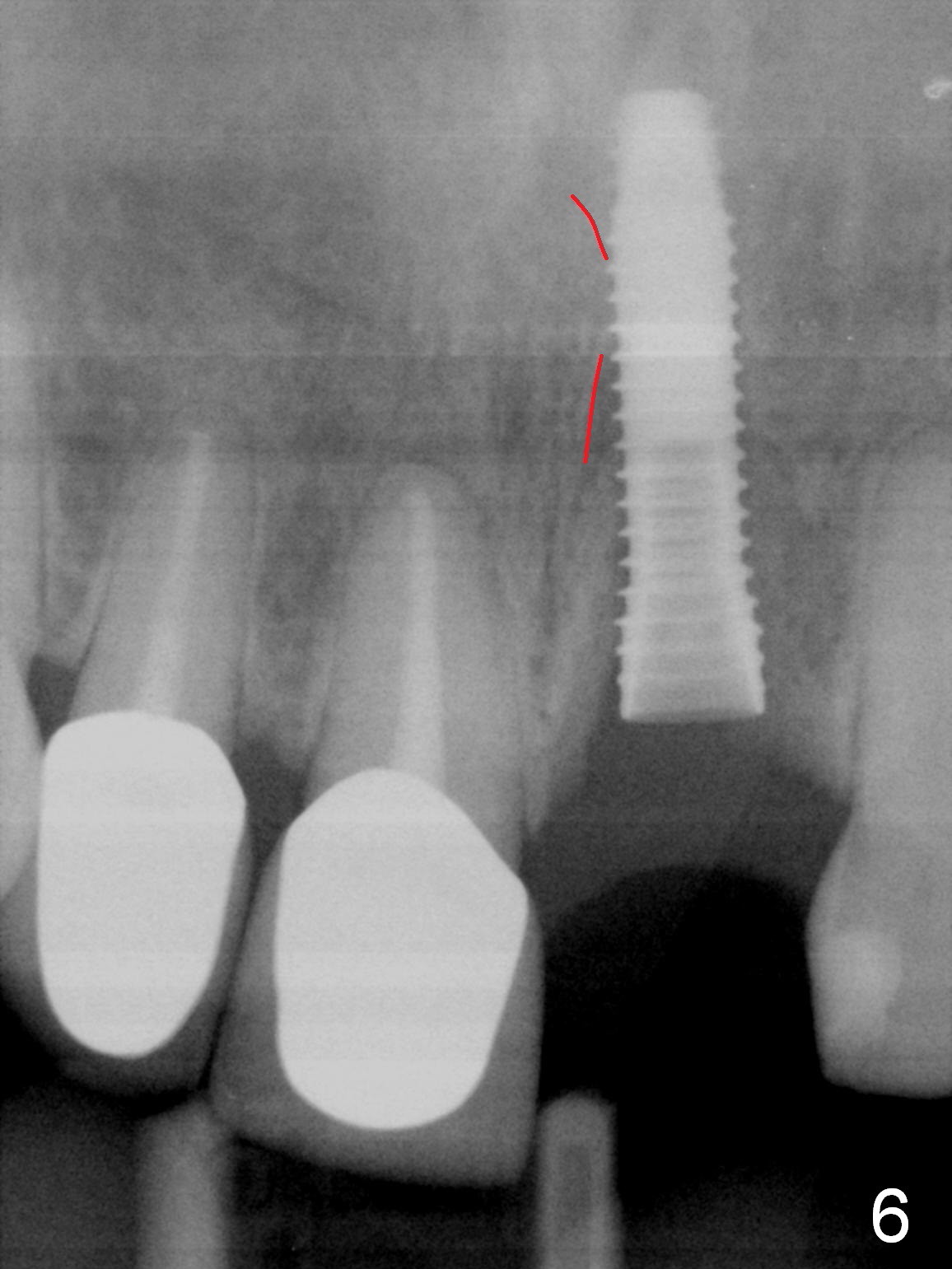
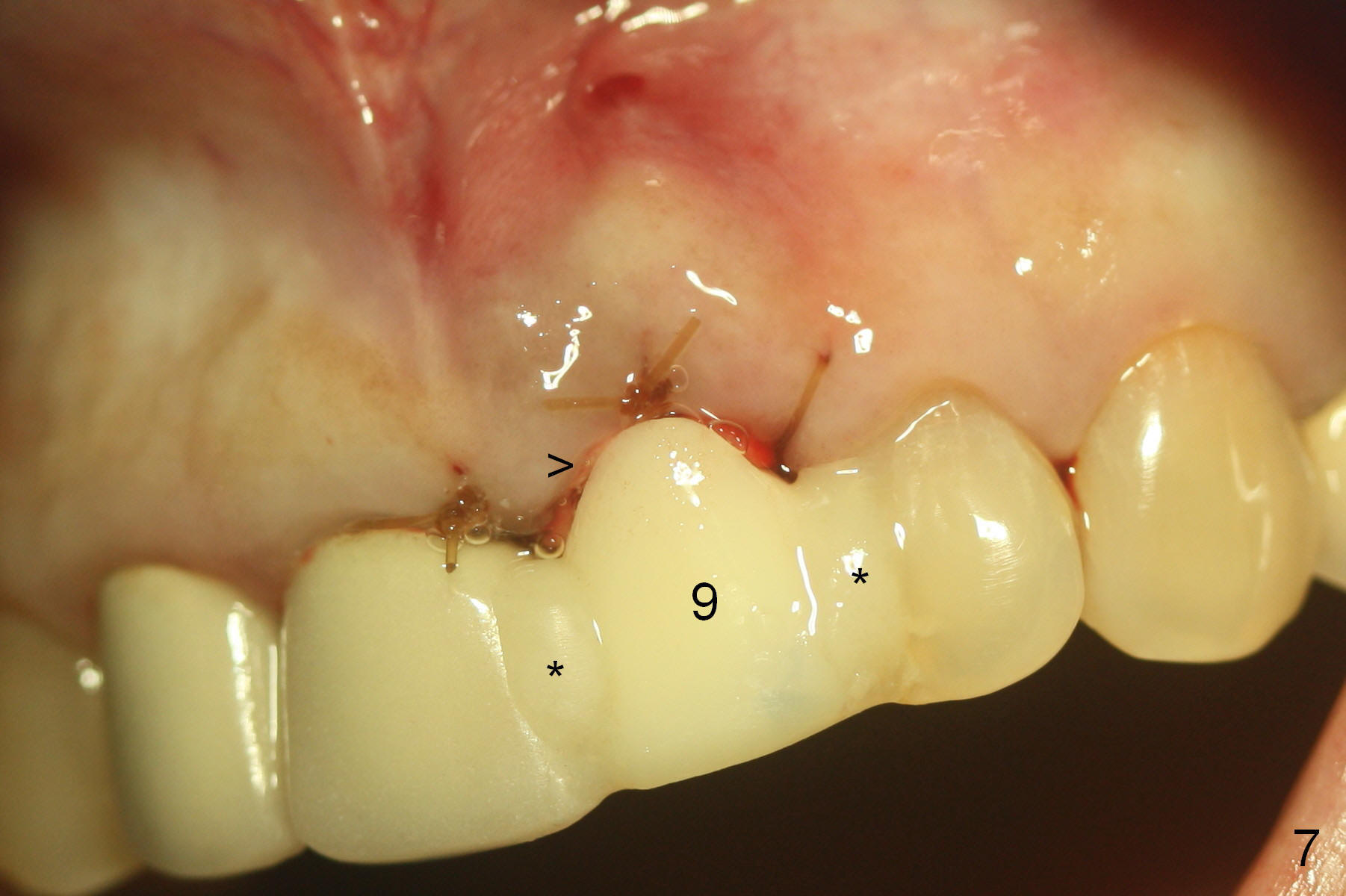
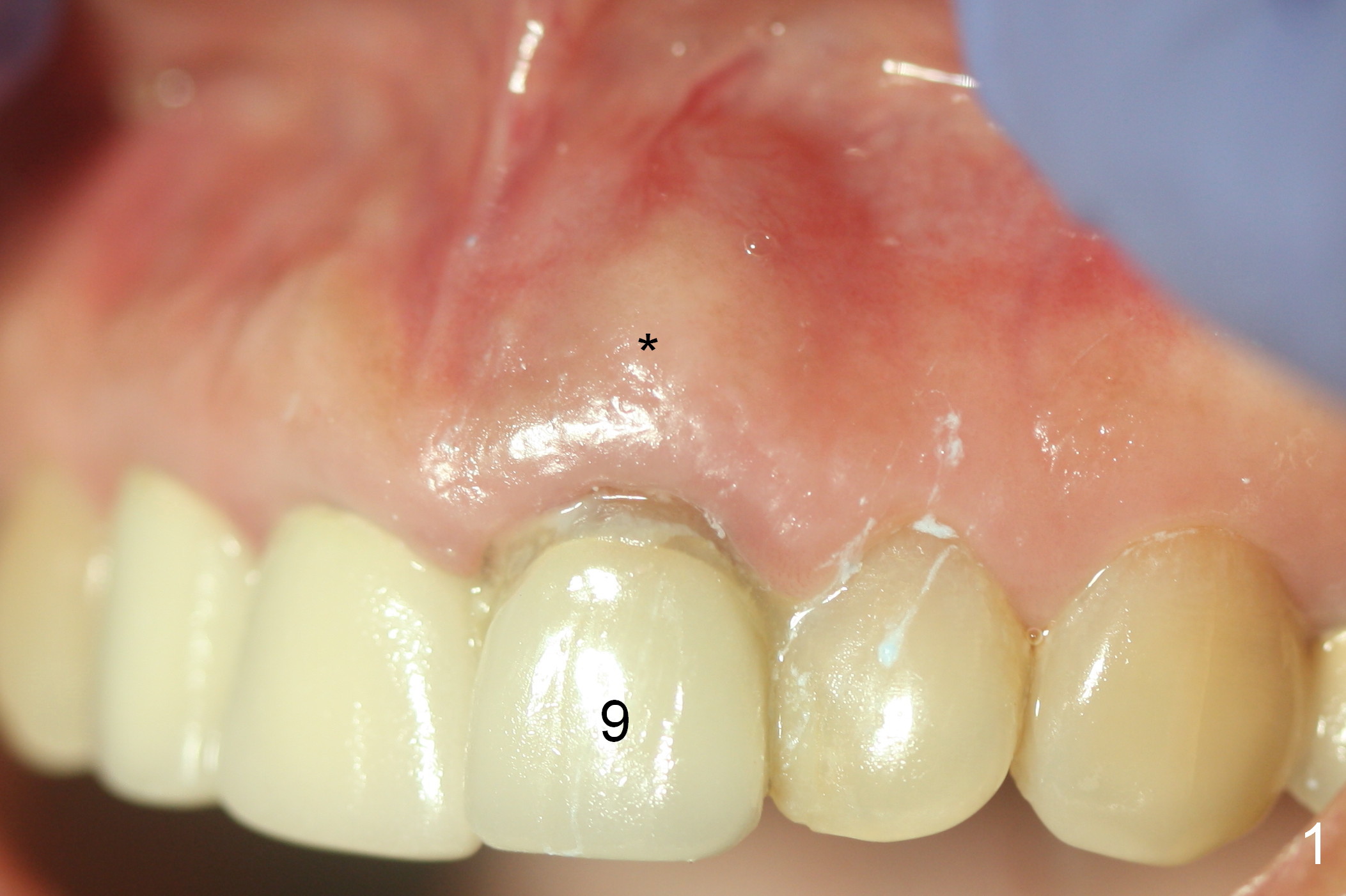
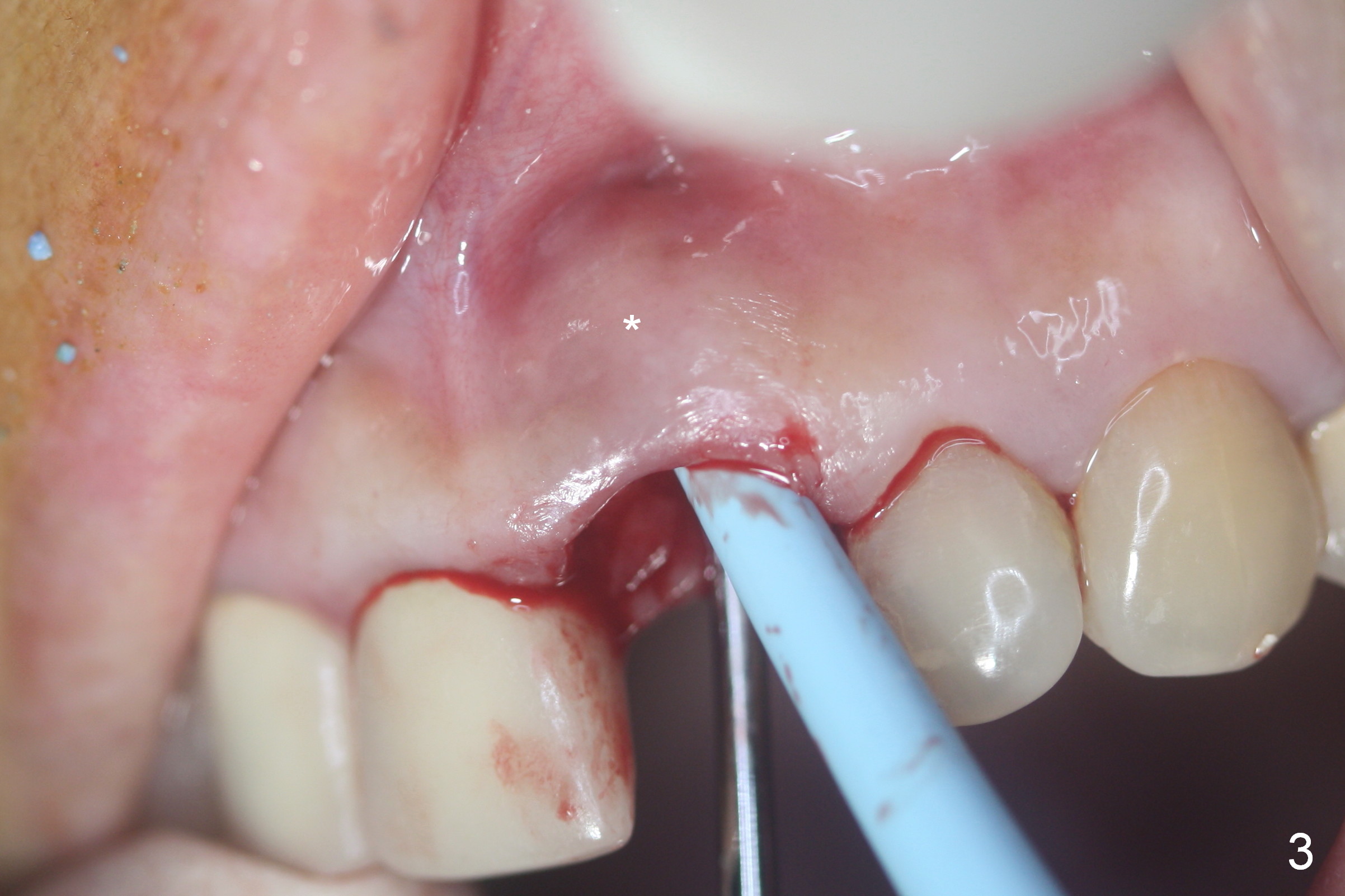
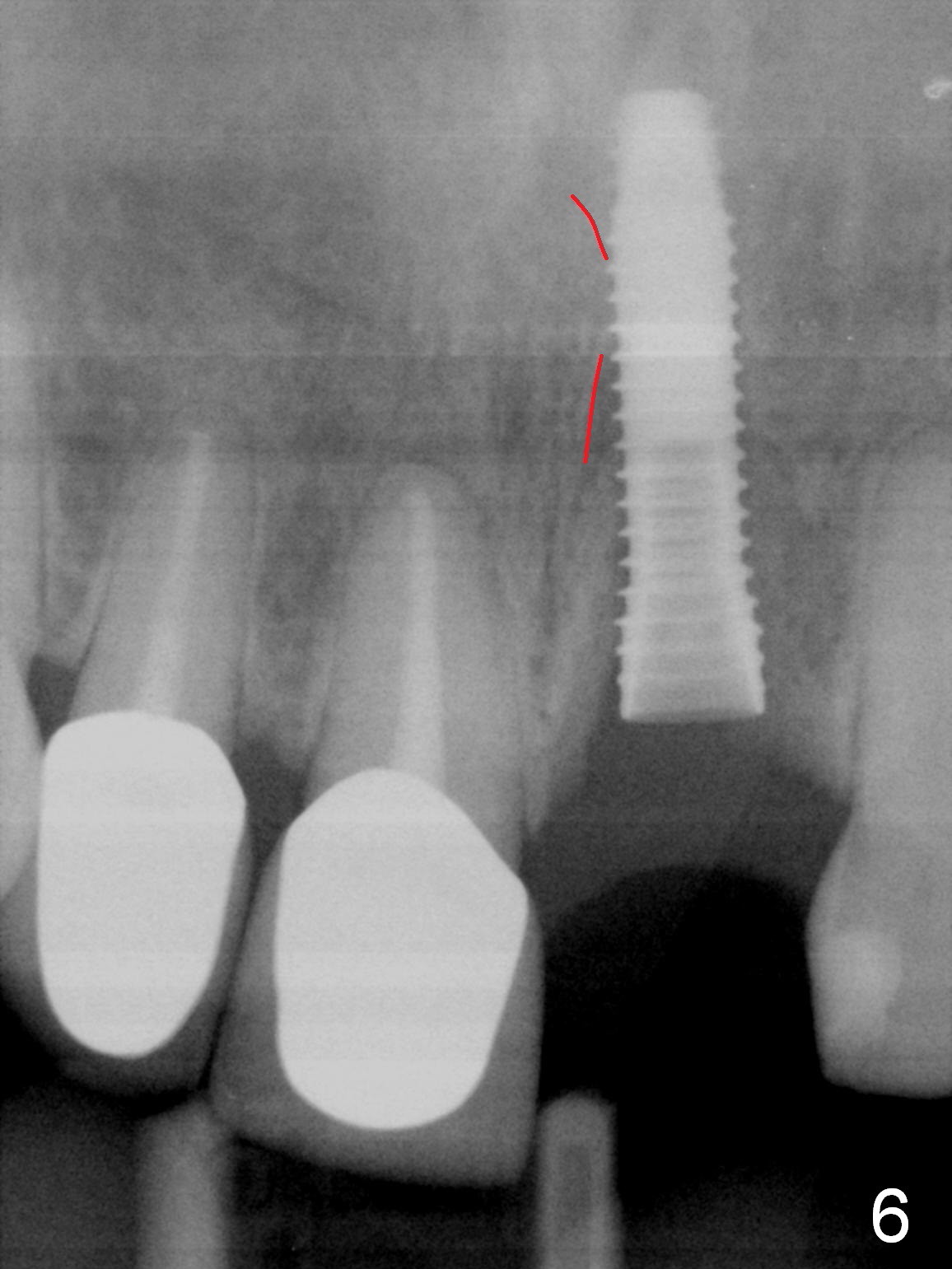
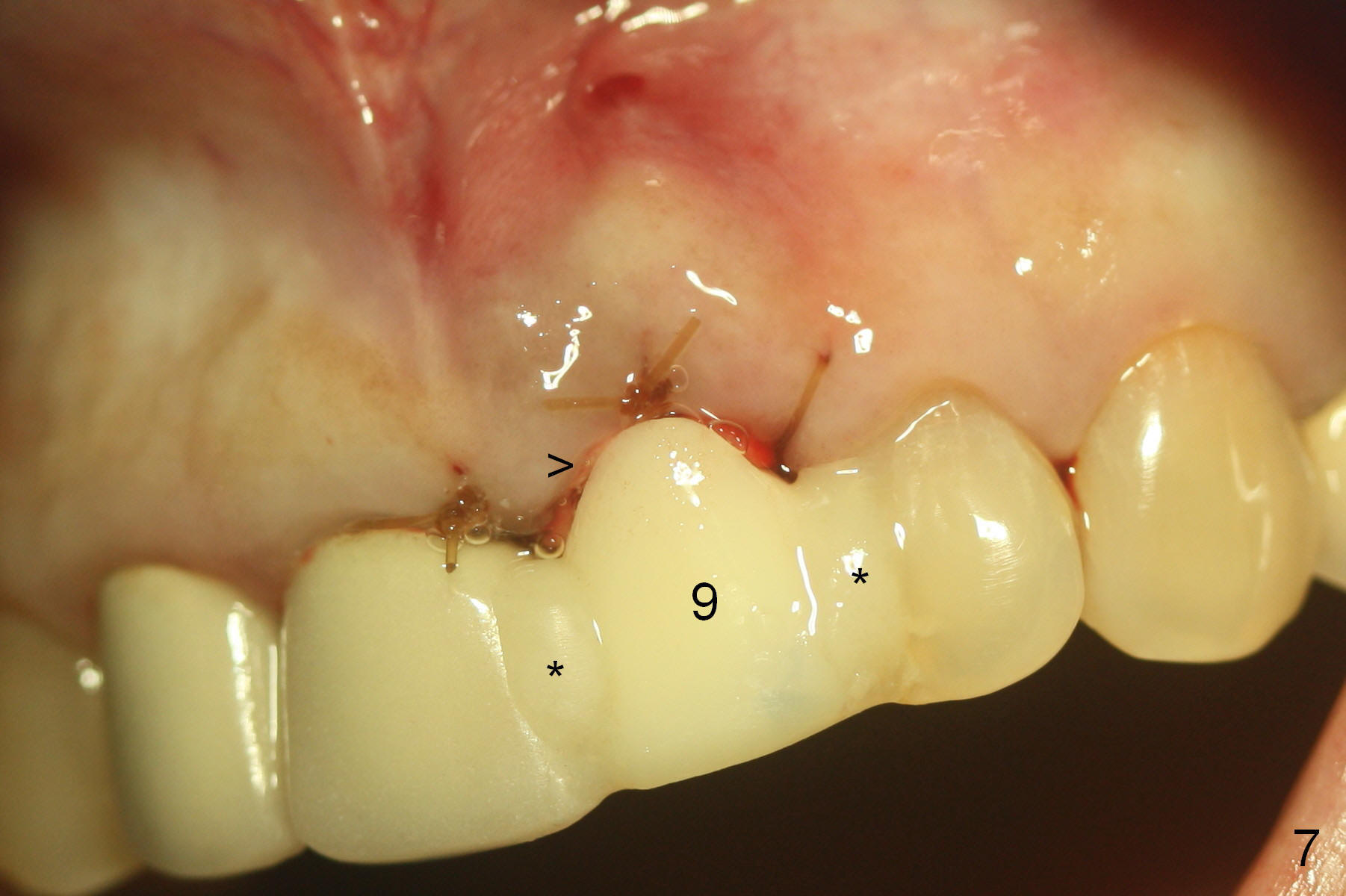
Preop exam confirms buccal gingival swelling at #9 (Fig.1 *) associated with purulent discharge from the gingival sulcus (Fig.2 <) when the swelling is pressed (*). As expected, the buccal plate is absent when the tooth is extracted (Fig.3 *). There is hemorrhage apically after socket debridement. Hemostasis is achieved when a piece of gauze is inserted into the buccoapical aspect of the socket (Fig.4 G), which is favorable for osteotomy in the palatal (P) wall. Initial osteotomy is ~ 4 mm superior to the apex (Fig.5). To place collagen membrane against the buccal gingiva securely, the gauze is removed prior to implant placement. Hemorrhage resumes, making implant placement difficult. The membrane does not possess hemostatic effect. Also because of low bone density, the apical end of a 3.8x16 mm implant feels like going to perforate the buccal apical plate while being placed. The trajectory has to be re-adjusted with the apical end directed palatodistally (away from the Incisive Foramen (Fig.6 red dashed line)). Finally primary stability is low (~ 15 Ncm). The immediate provisional (Fig.7: 9) is bonded (*) to the neighboring crown/tooth. Introspectively, the bonding seems to be strong enough to have abutment placement. The provisional securely keeps bone graft and collagen plug (Fig.7 >) in place.
In brief, bone density in the upper jaw of a senior lady is low, making immediate implant more challenging. Hemostasis is also critical.
Without immediate placement of an abutment, there is a gap between the provisional and the labial gingiva 4 weeks postop (Fig.8,9 <, as compared to Fig.7). It is planned to place an abutment 2 months postop. If the implant is stable, splinting may not be needed. Ideally, an abutment and splinting should have been placed together for stability initially.
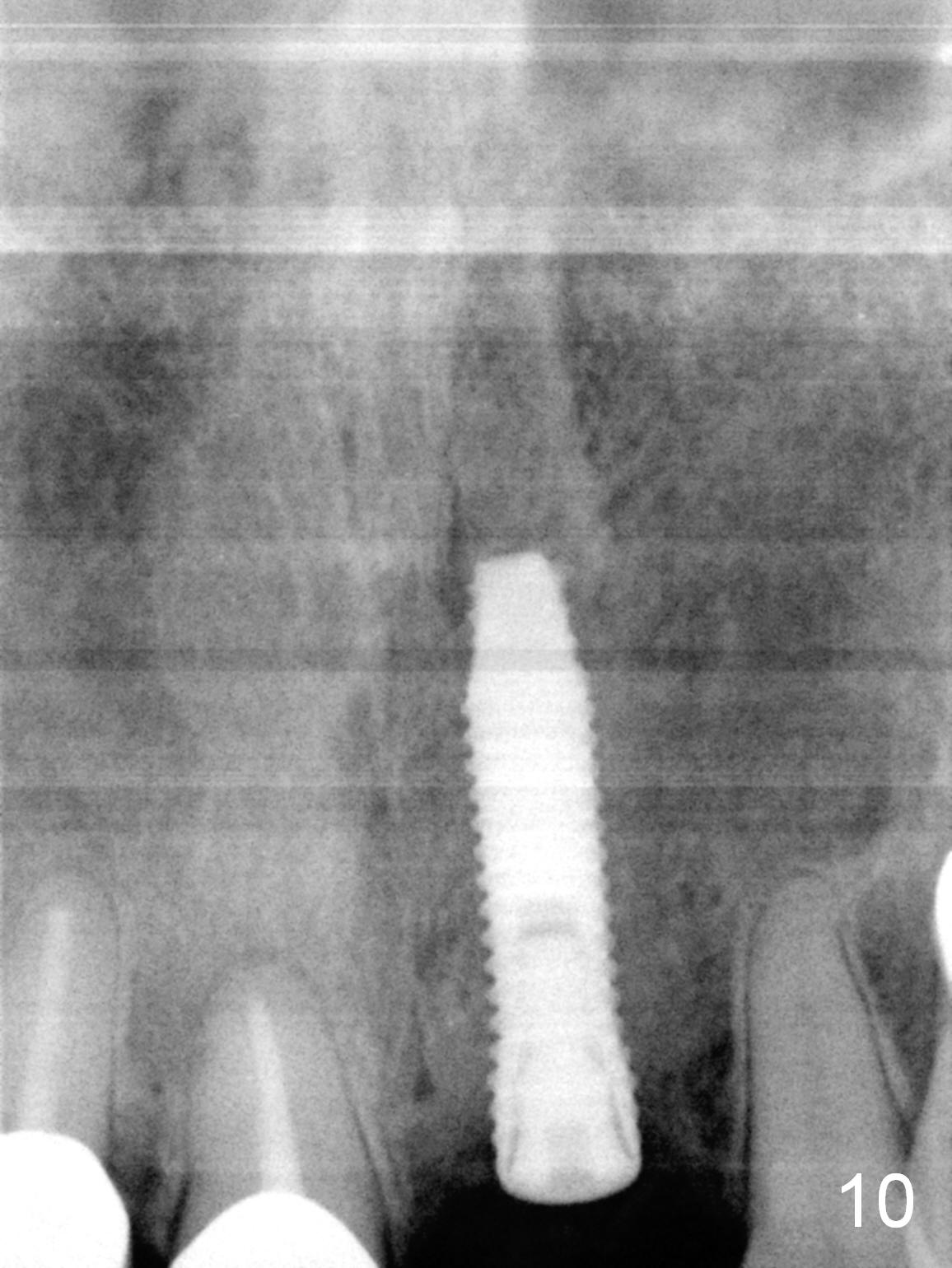
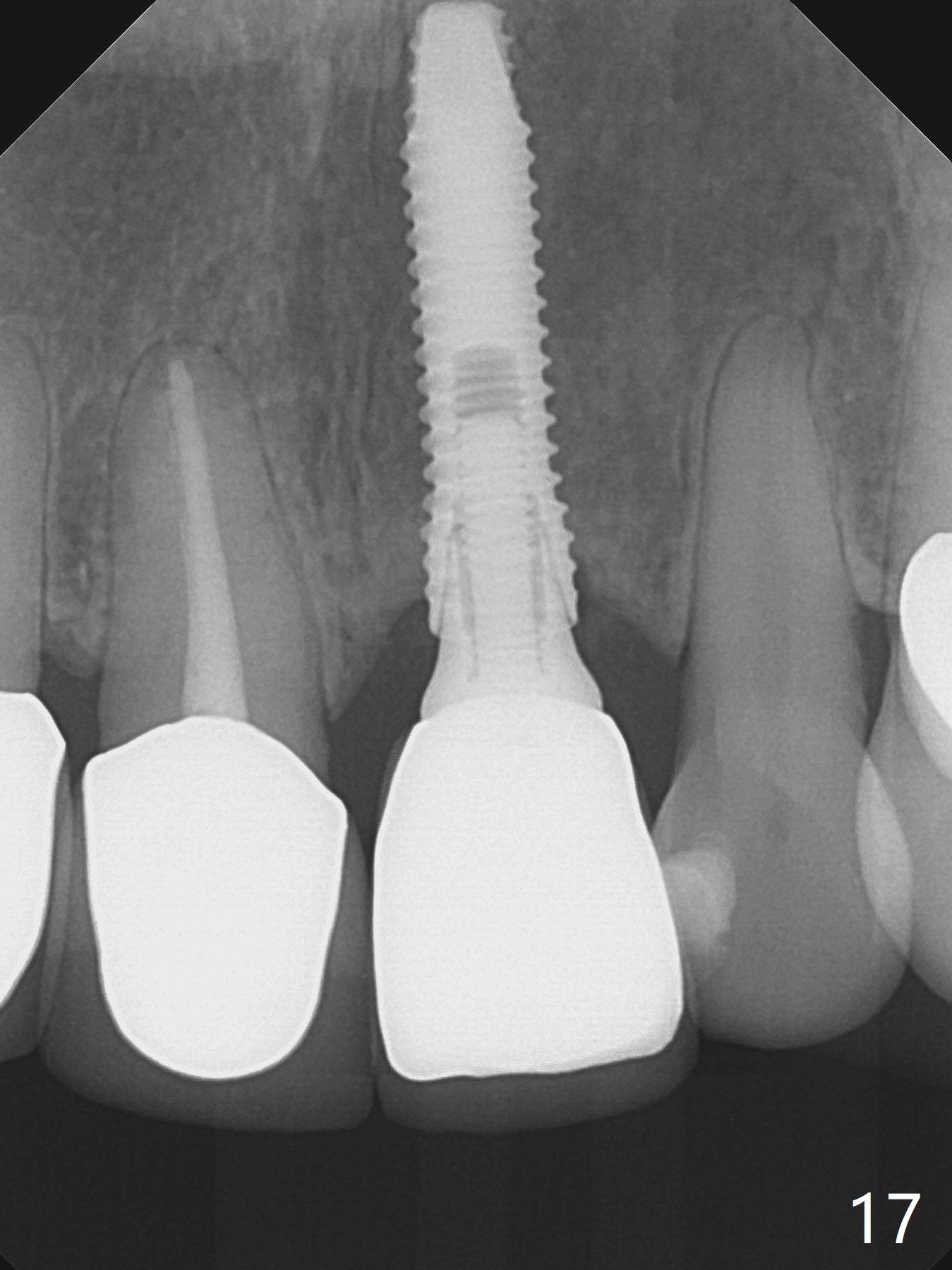
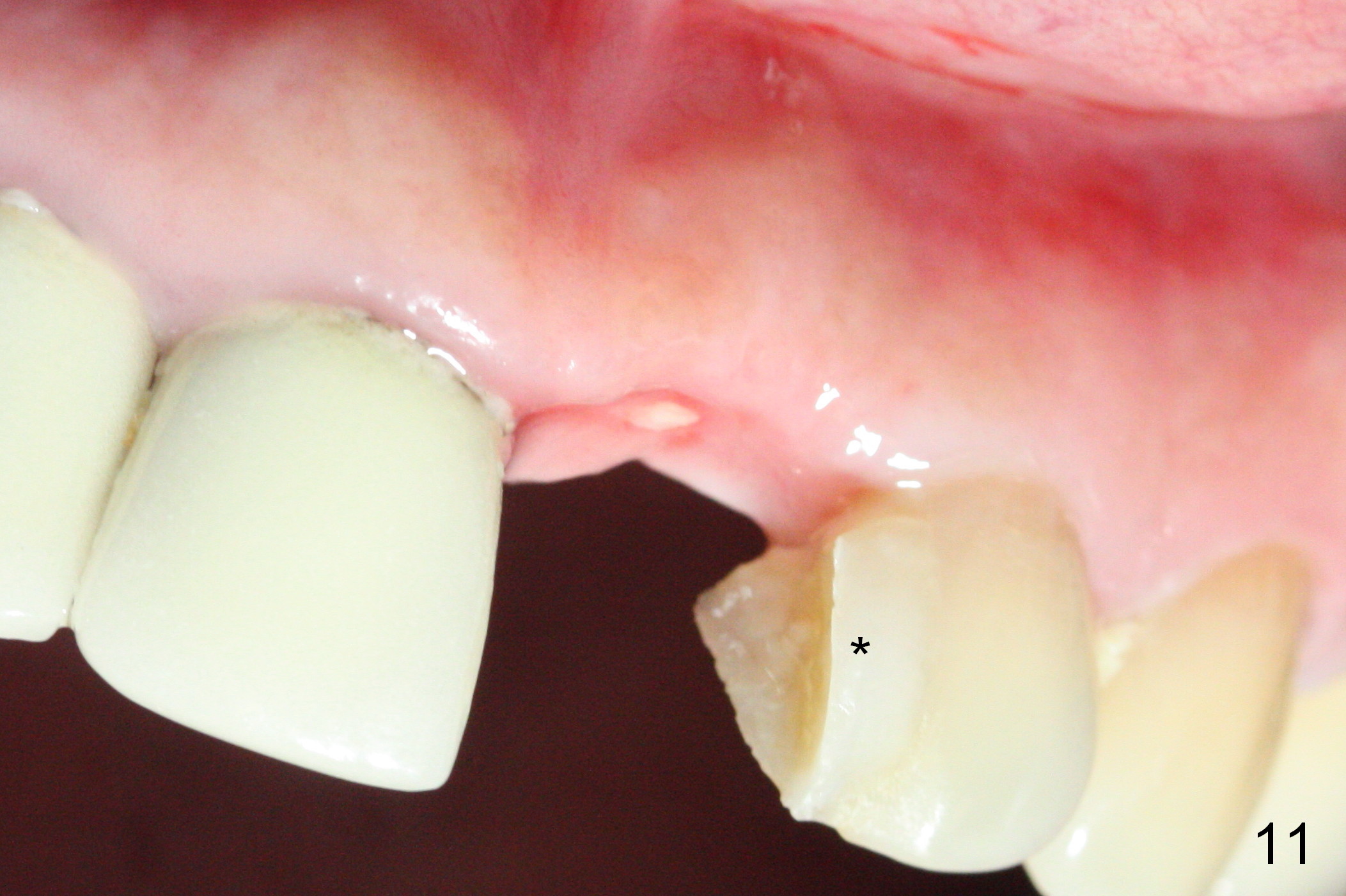
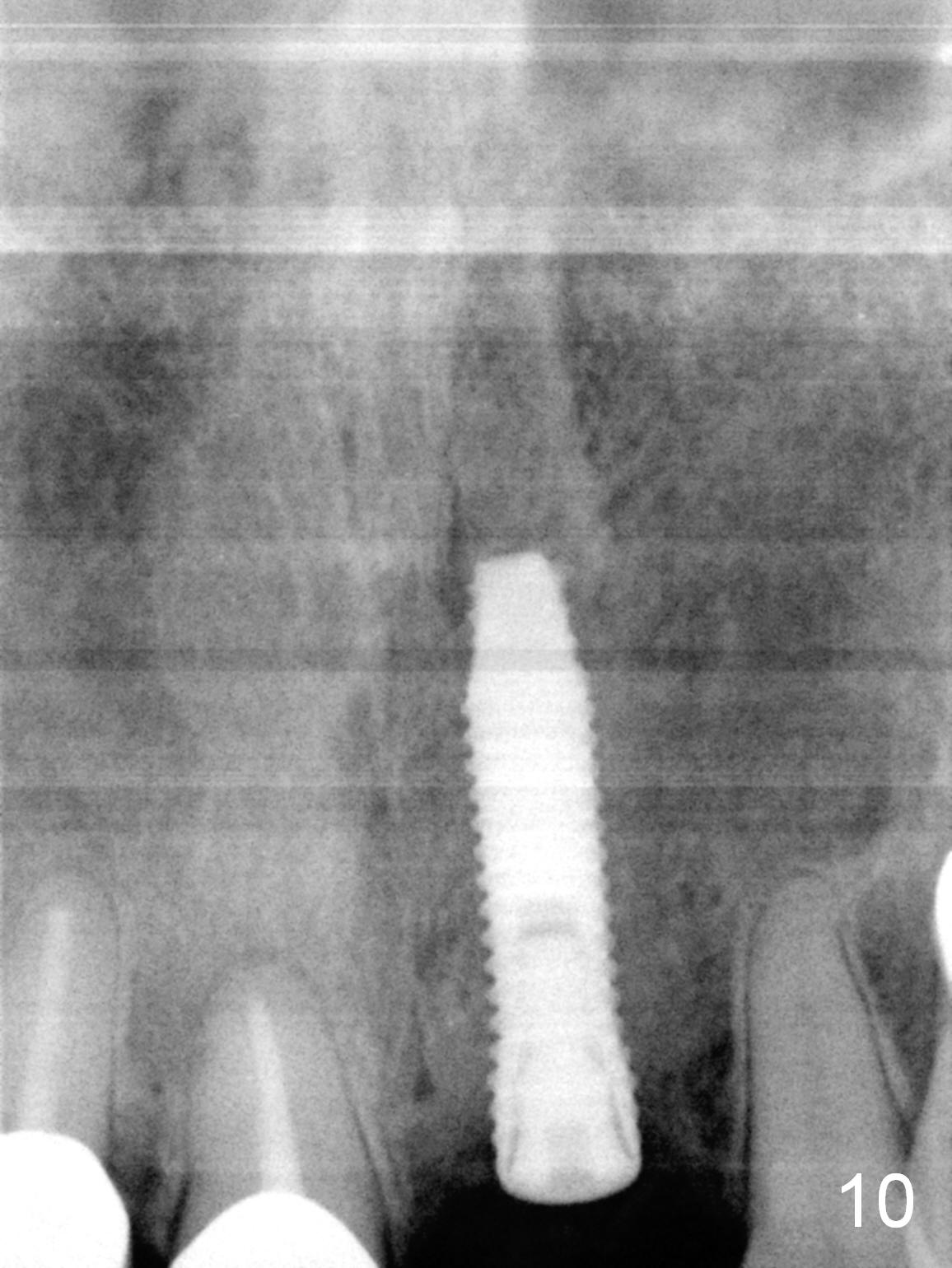
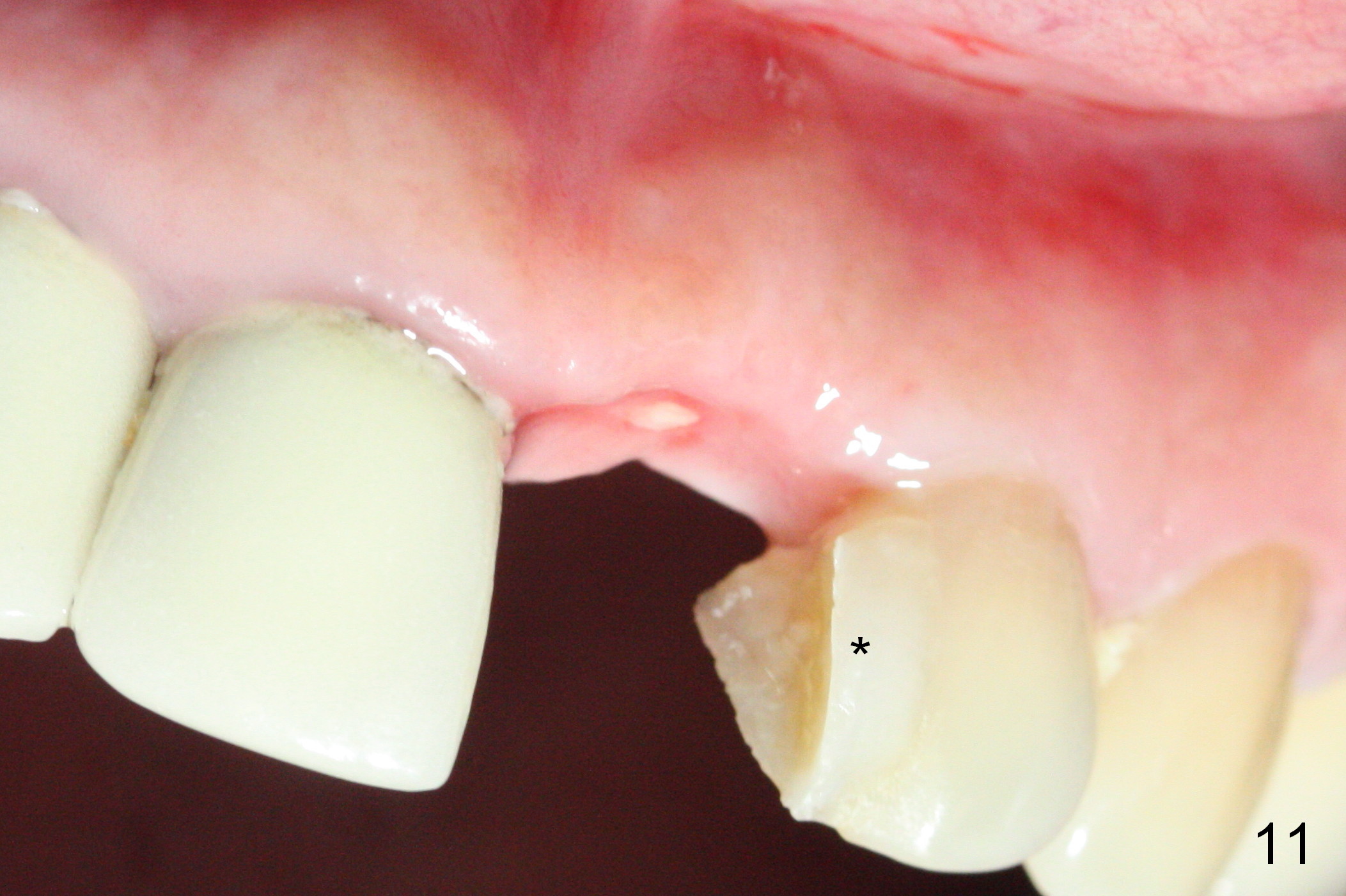
The implant appears to have osteointegrated 2.5 months postop (Fig.10). The provisional is debonded from the neighboring tooth (Fig.11 *) and crown. In spite of mild buccal plate atrophy (Fig.12), the gingival margin at the implant site does not recede (Fig.11). After placing and preparing an angled abutment (4.5x15° A, 3 mm cuff) atraumatically, the buccal gingival margin appears to recede (Fig.13, expected to be transient). Please block the metal shade while fabricating the crown with C2 (Fig.14).
In fact, the crown looks too bulky. After change in abutment without too much prep on gold coating, the new crown looks good in shade, although too long (Fig.15). The buccal plate seems to have minimal atrophy (Fig.16 *).
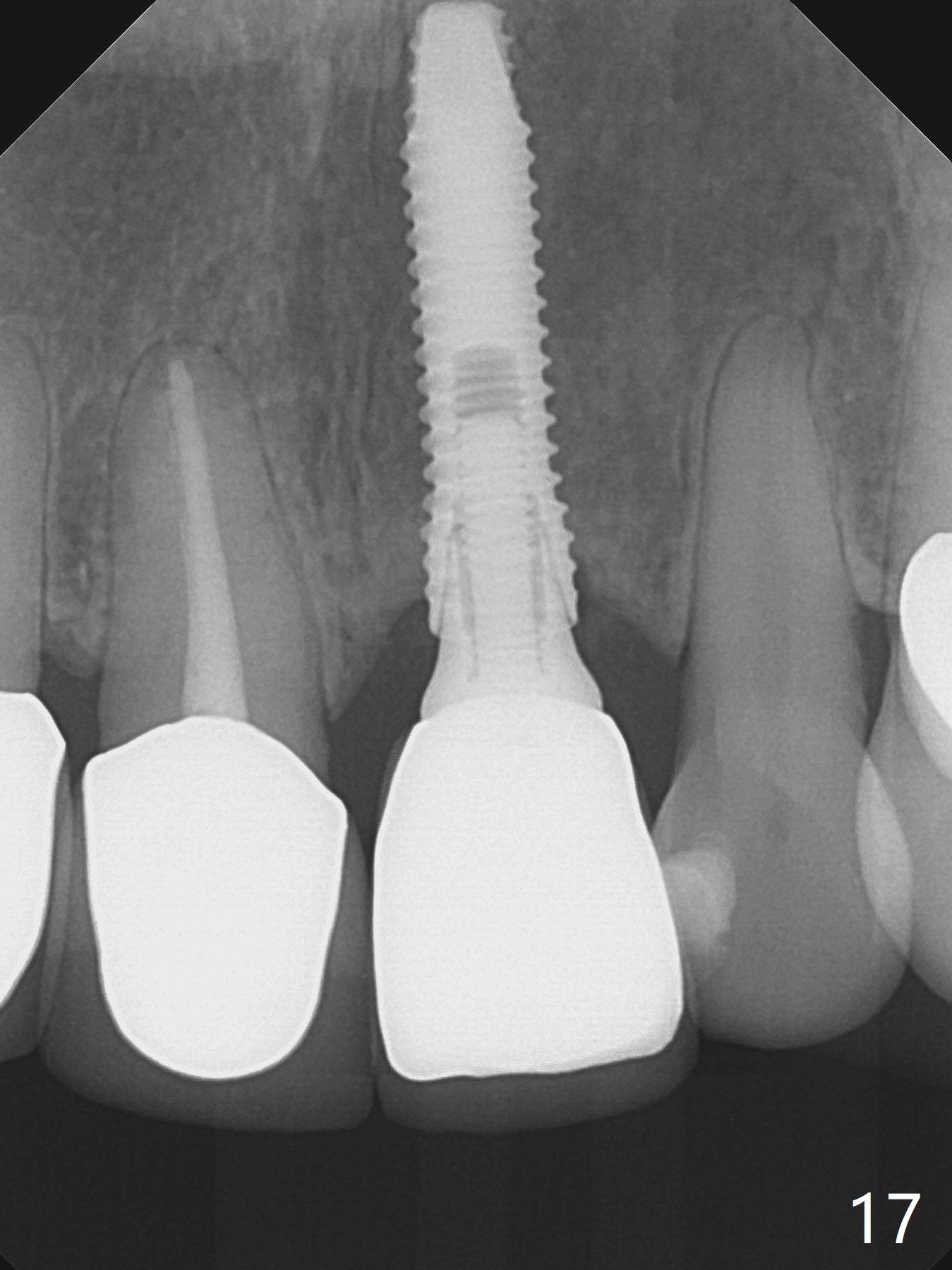
Take PA when the patient returns for follow up. The sensor should be placed parallel to the long axis of the implant so that threads are distinct.
The patient returns 9.5 months post cementation (Fig.17-19). There is mild gingival recession (Fig.18) and atrophy (Fig.19).
Return to
Upper Incisor Immediate
Implant
Xin Wei, DDS, PhD, MS 1st edition 08/09/2016, last revision 10/09/2017