.jpg)
 |
 |
.jpg) |
|
 |
 |
 |
 |
Treatment Modalities for Anterior Periimplantitis
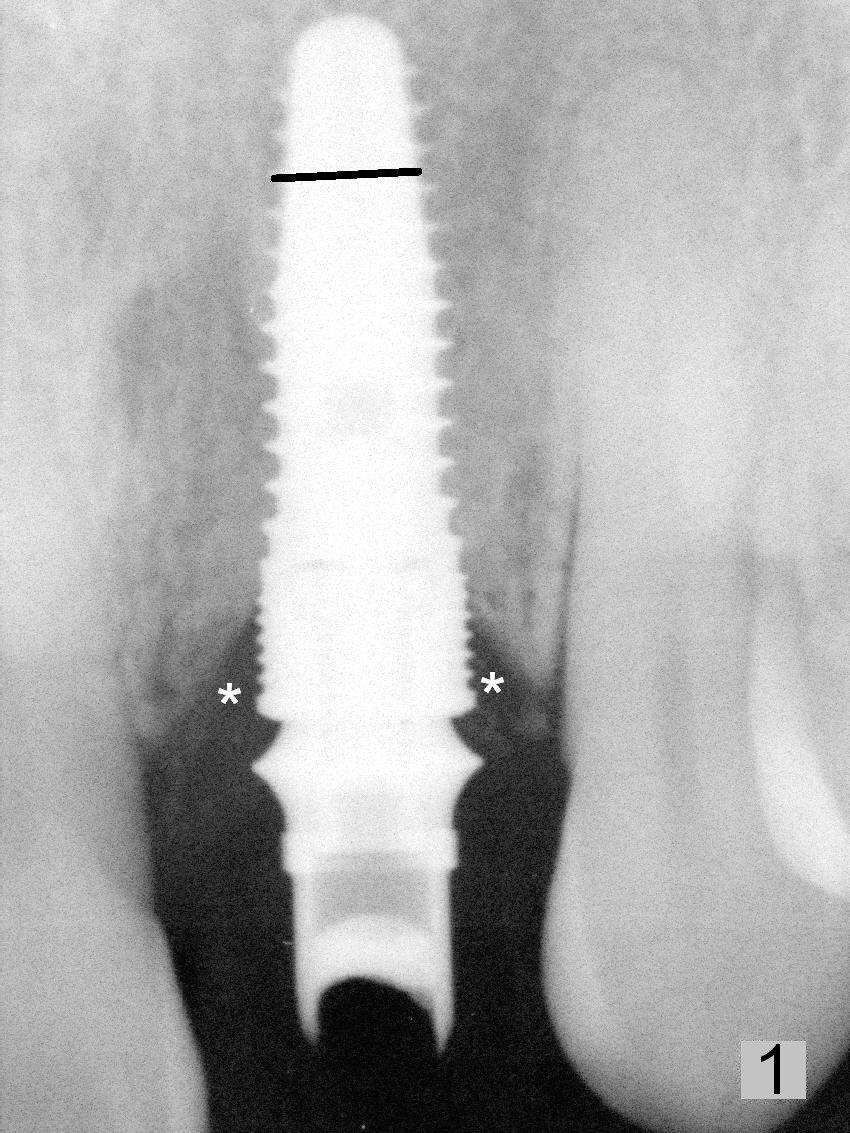
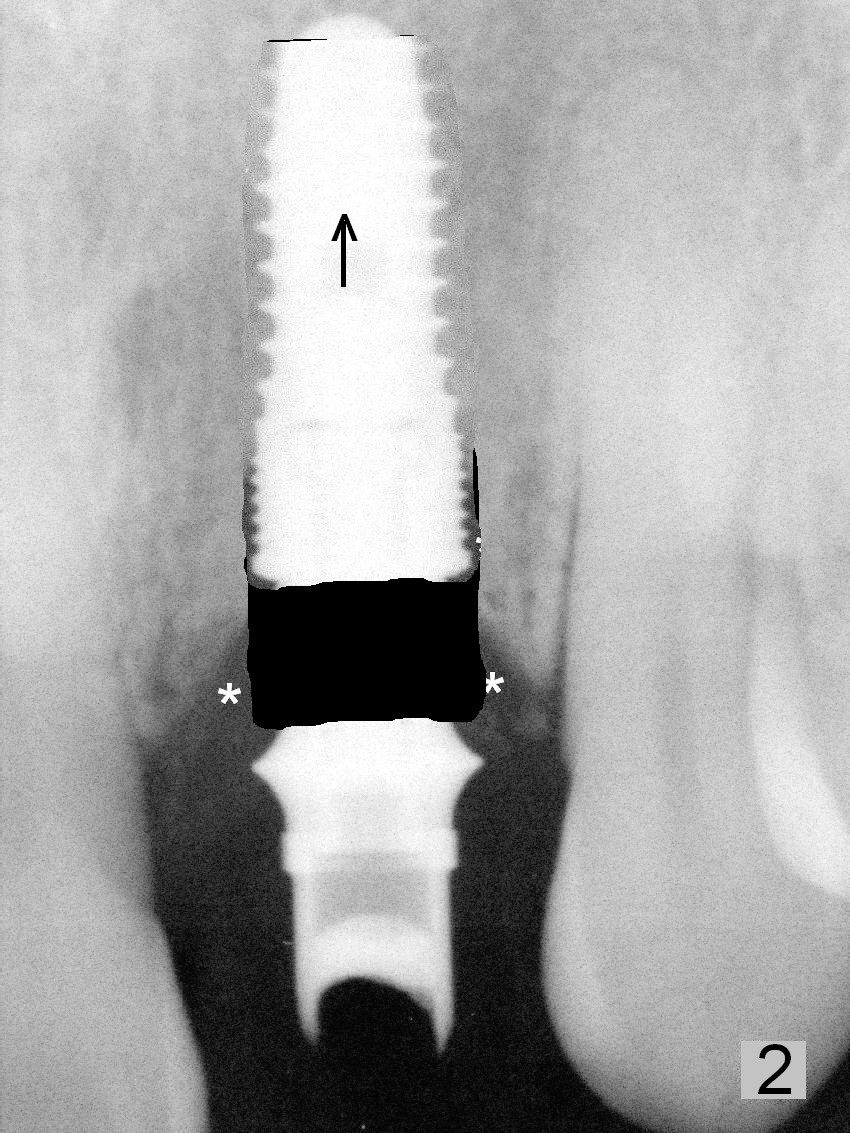
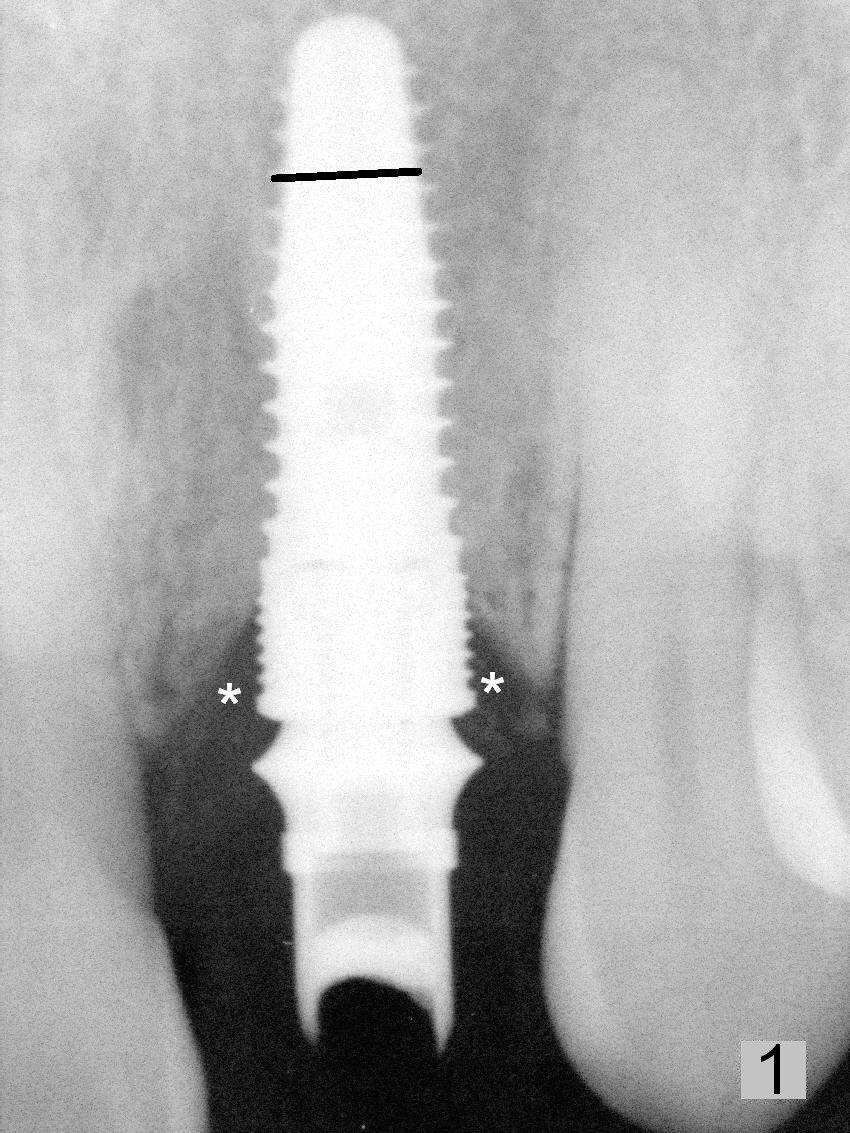
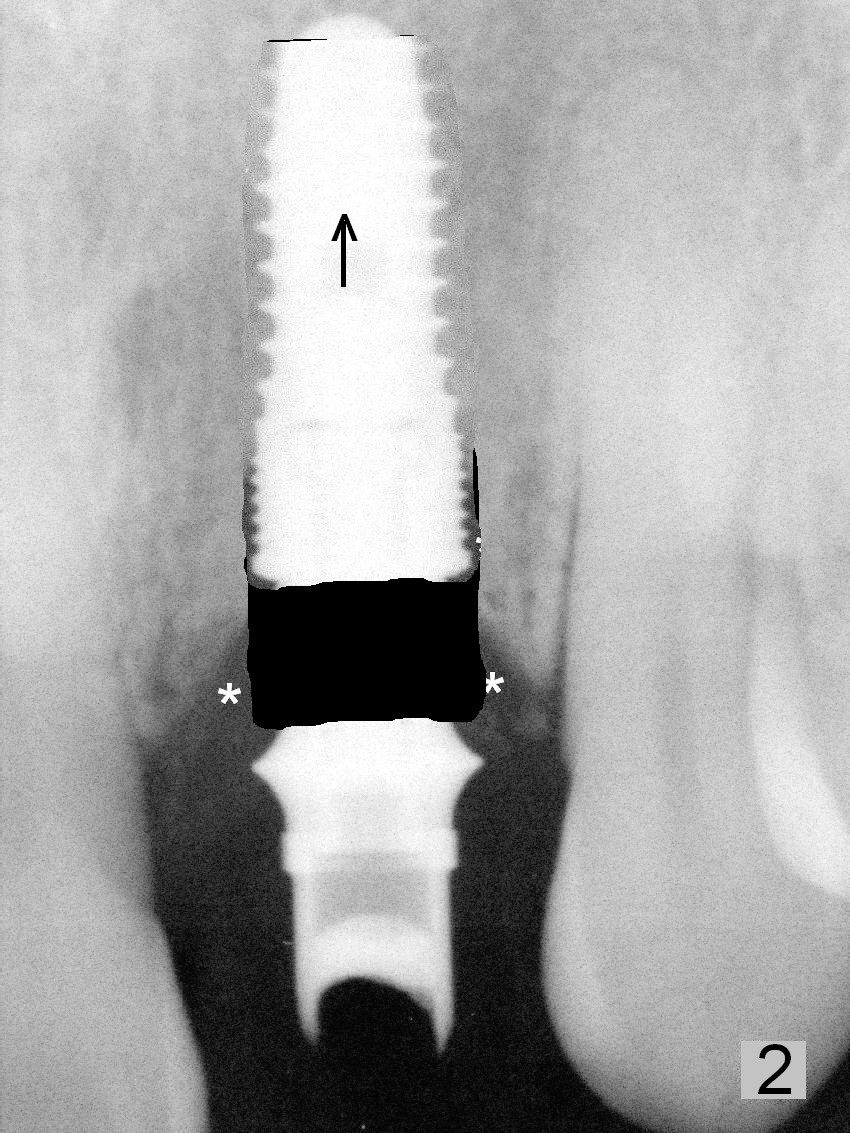
Incisional debridement for anterior peri-implantitis may cause gingival recession. The cause of periimplantitis in this case is probably coronal implant thread exposure (Fig.1 *). Since the access to the abutment is easy to get to, the implant is to be removed (9 months postop) by reverse torque. The labial plate is explored to determine the extent of defect. The osteotomy is soaked with Metronidazole gauze after copious irrigation with normal saline and H2O2. The exposed threads will be thoroughly cleaned in vitro and apex of the implant will be sectioned (Fig.1 black line). If most of the apical portion of the labial wall is intact, the implant will be returned and placed higher so that the most coronal threads will contact the mesial and distal crestal bone (Fig.2). An abutment with longer cuff will be inserted (Fig.3 white outline).
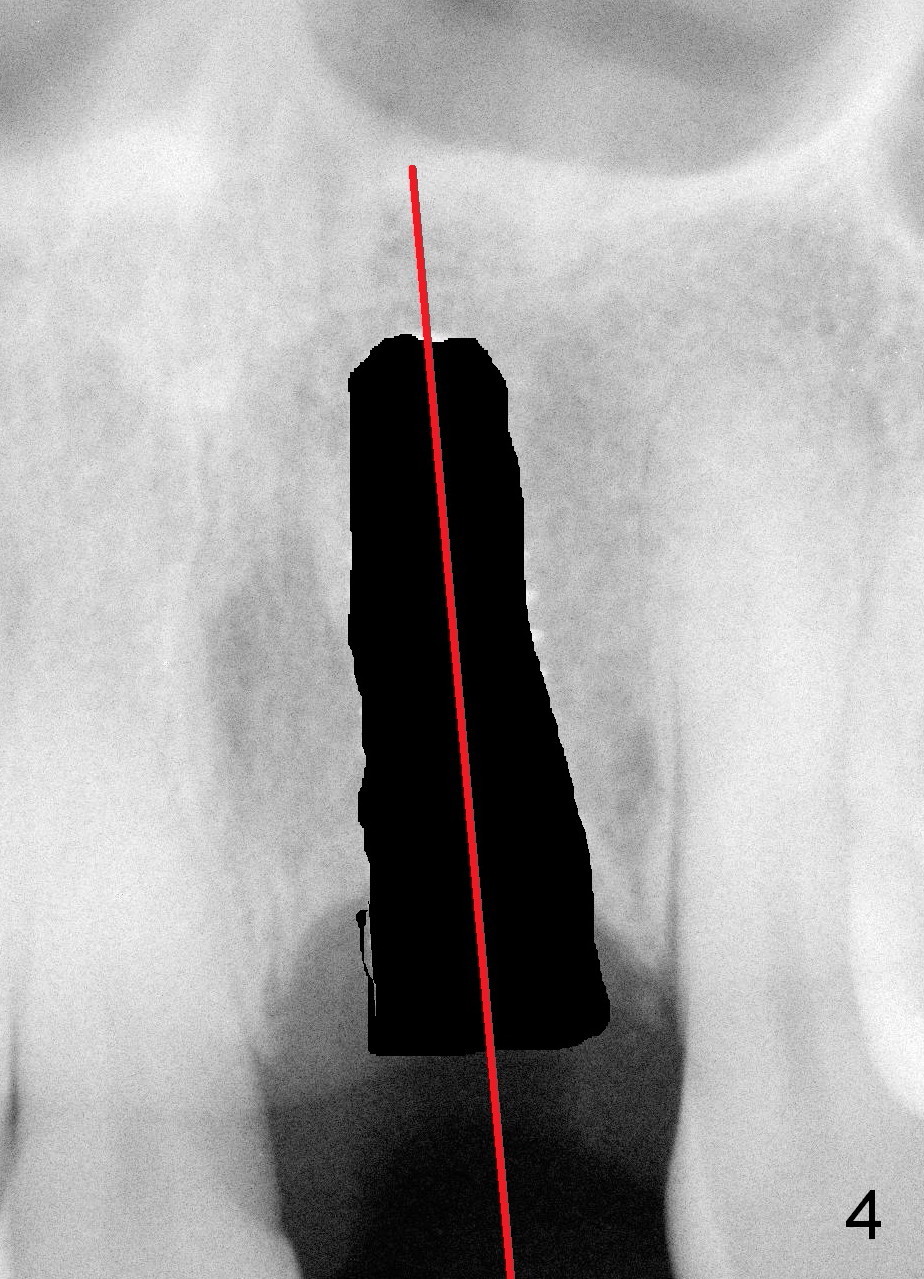
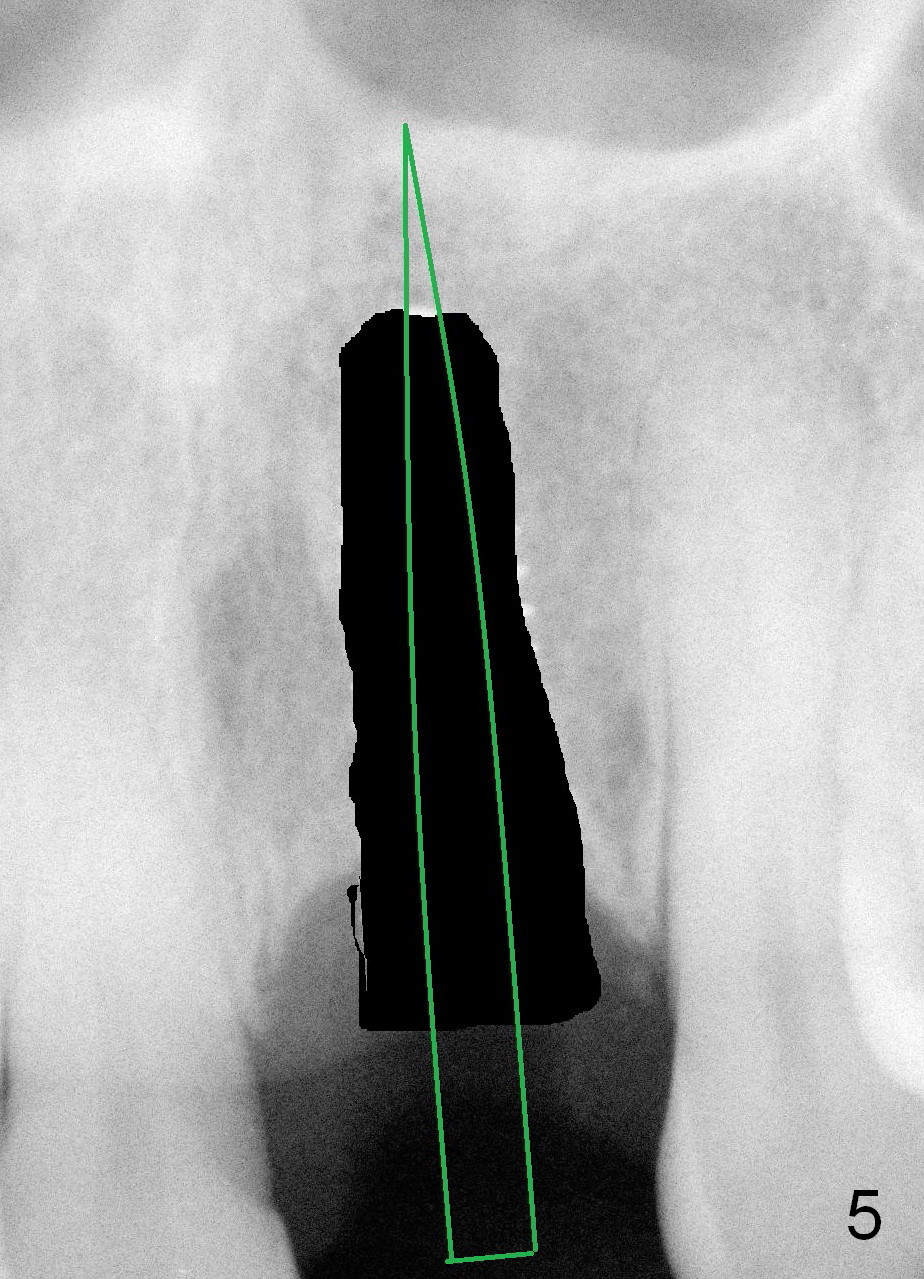
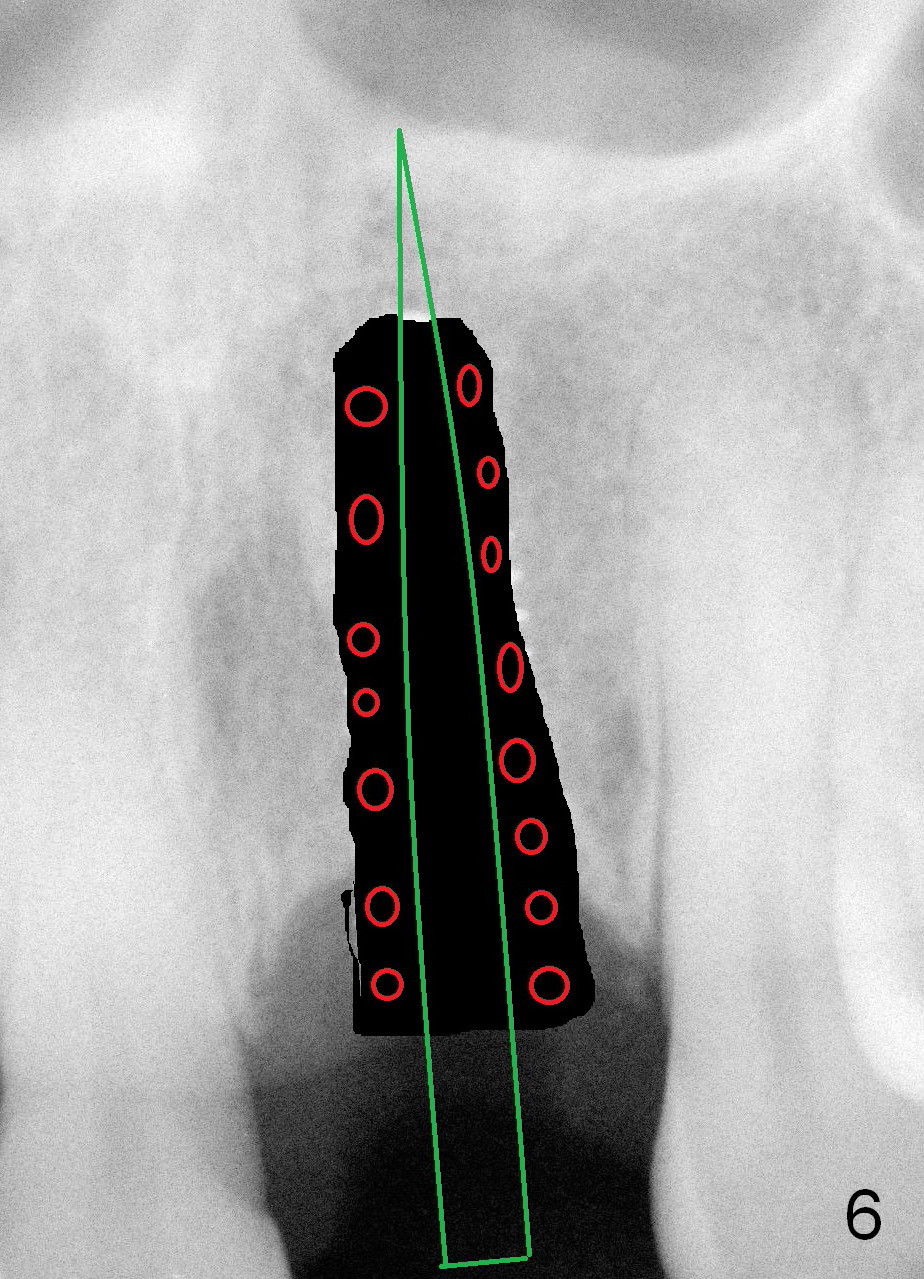
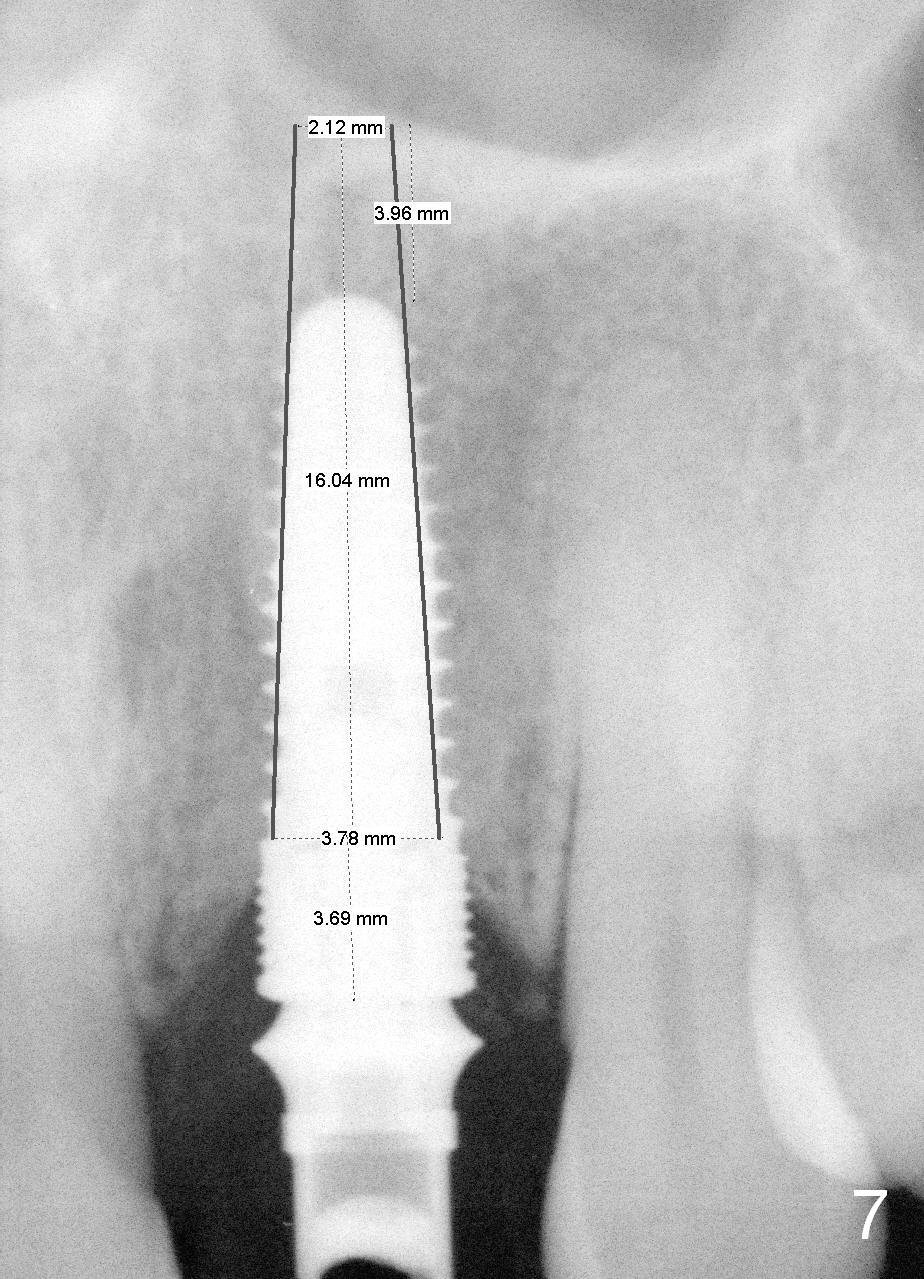
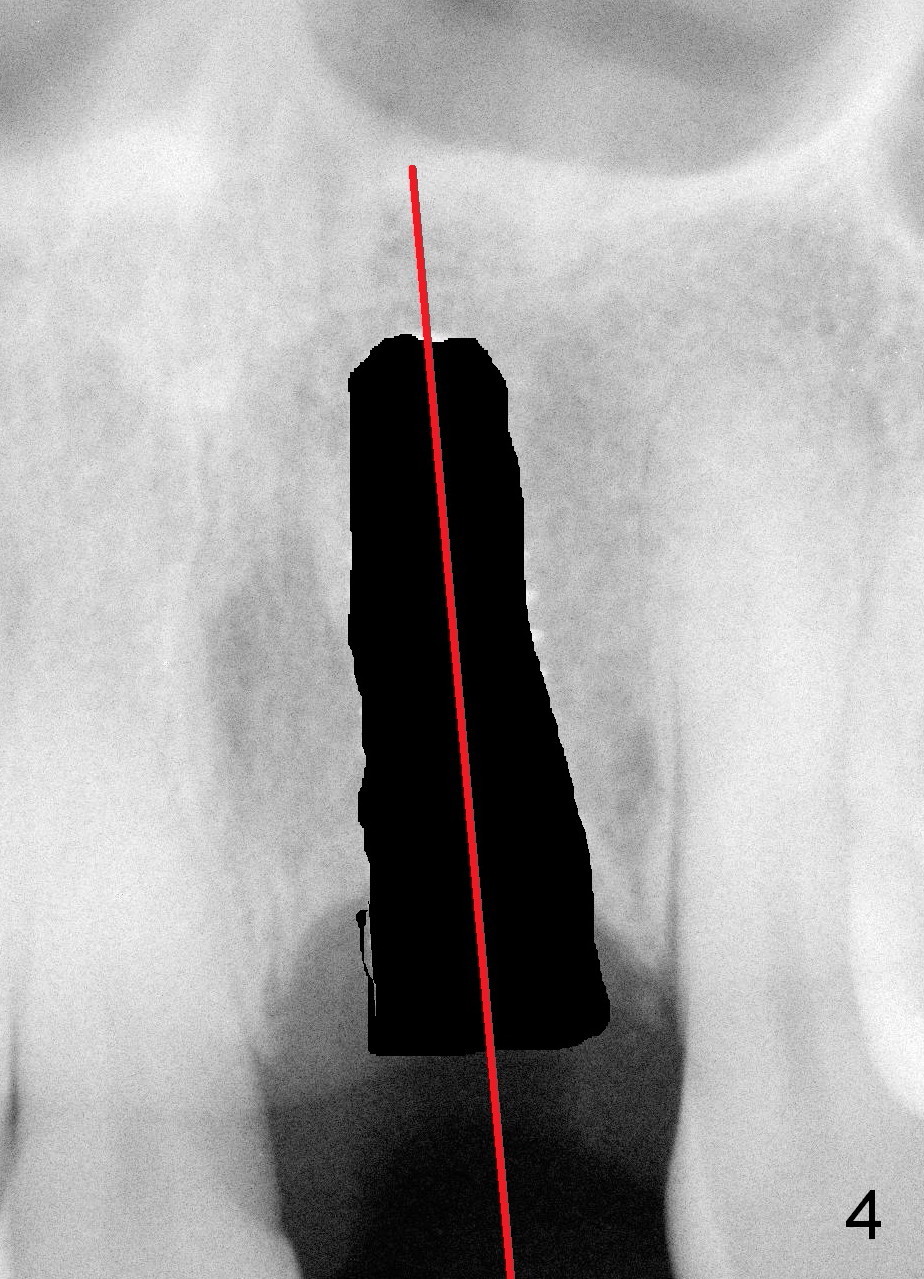
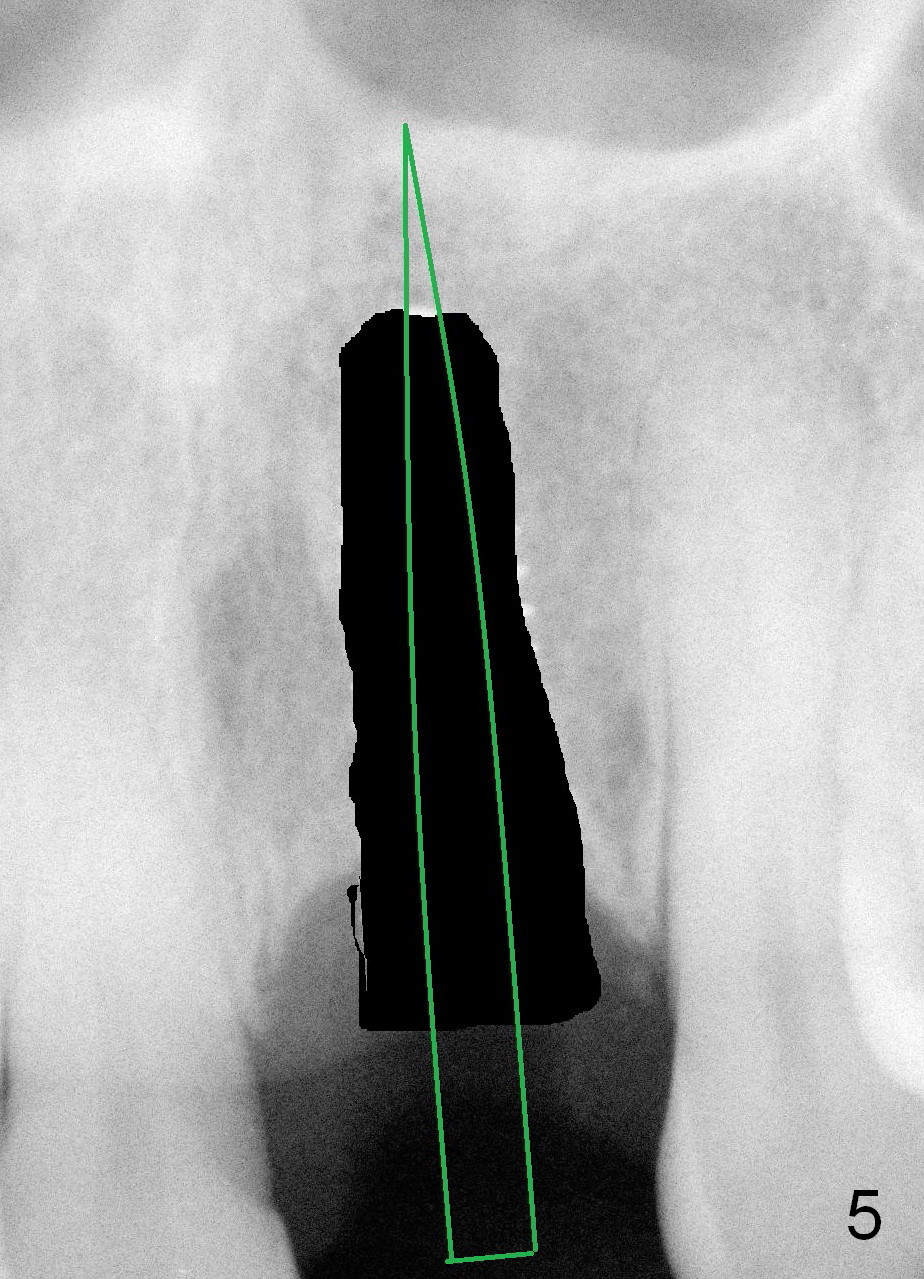
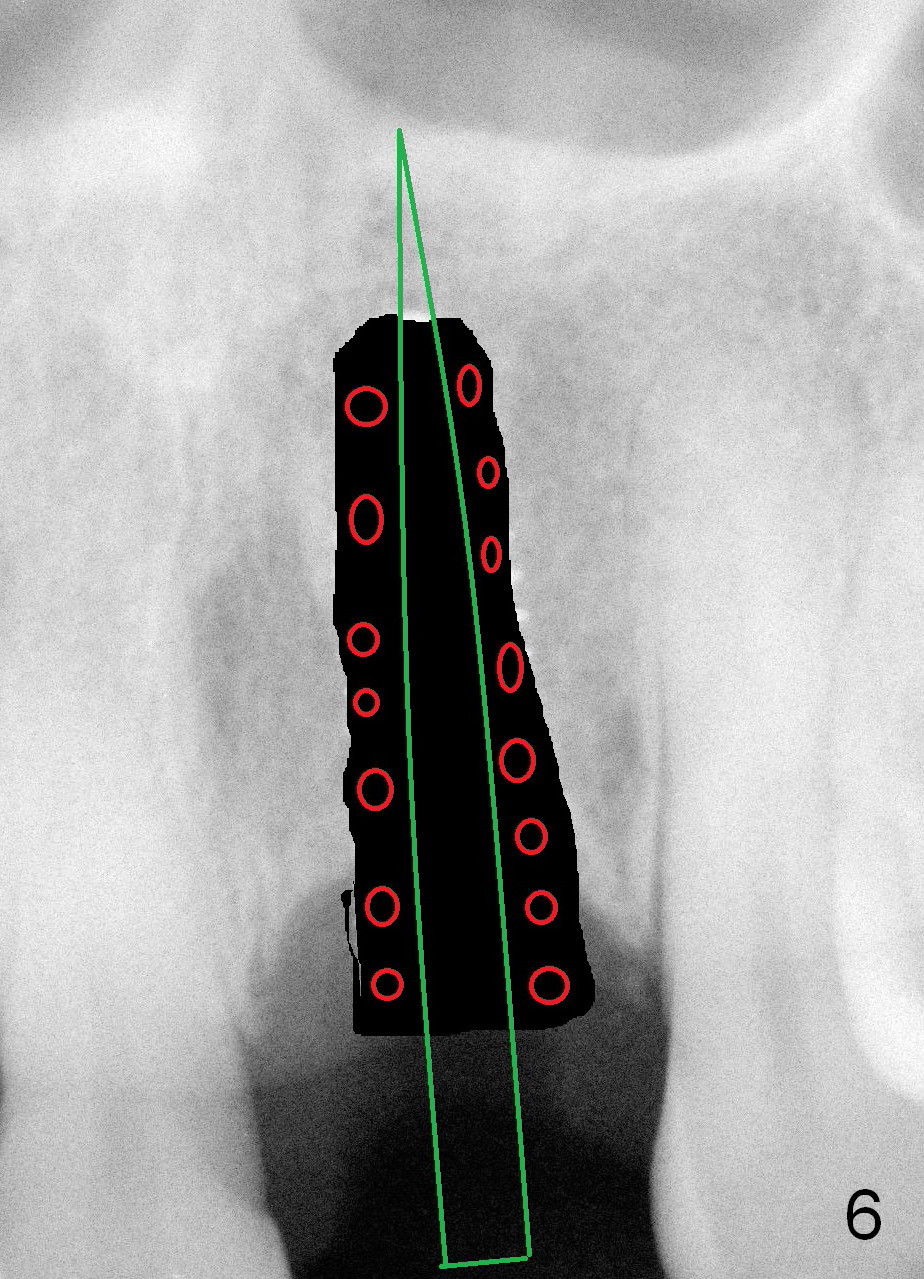
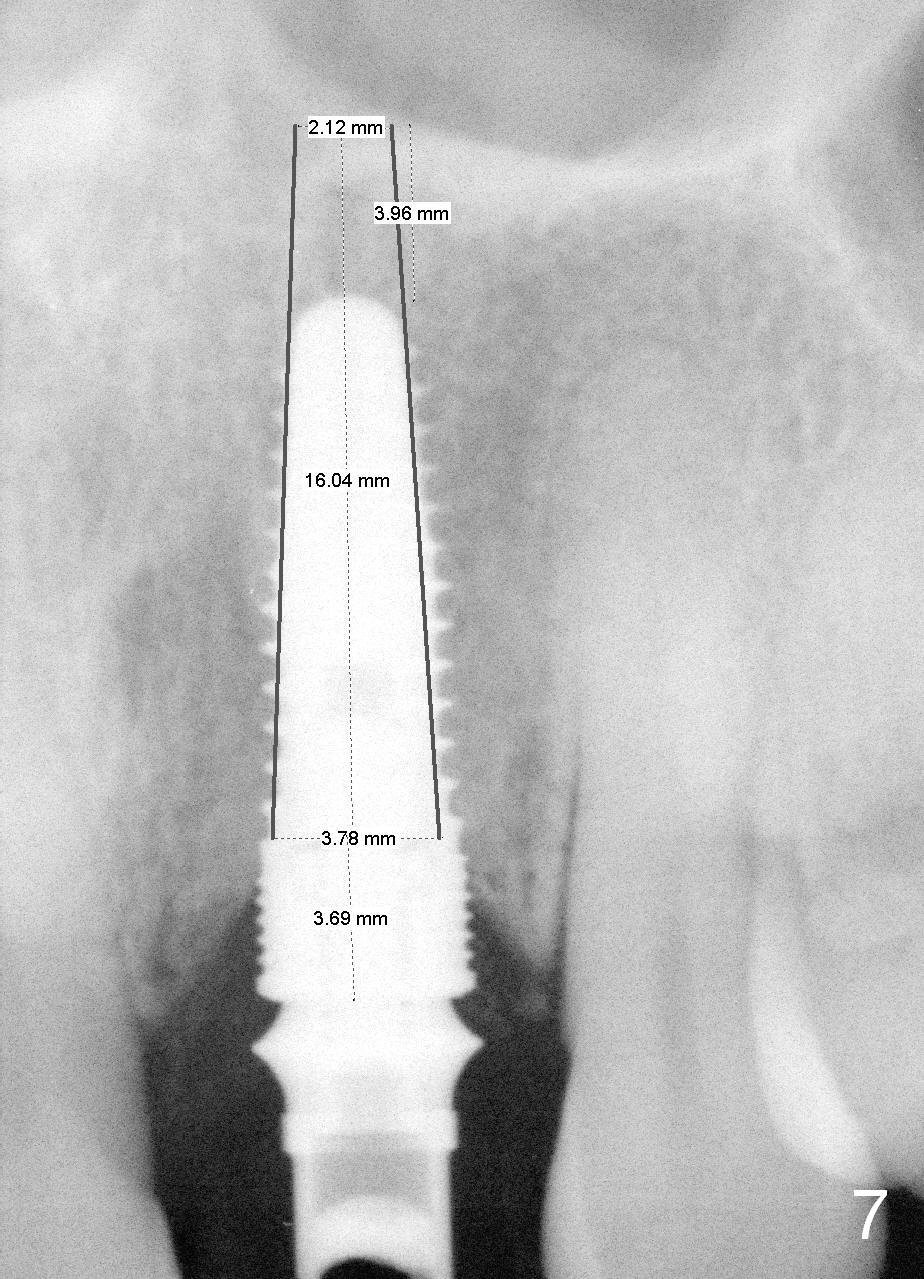
If primary stability cannot be achieved, obtain new osteotomy apically (Fig.4). Place a smaller and longer implant (Fig.5). Place Osteotape buccally prior to implantation. Bone graft (Fig.6 red circles) can be placed before (preferably) or after implantation. The new implant could be one or two-piece one. The latter could be UF 3.8x15,16 or 18 mm (Fig.7).
If the existing implant cannot be removed, an incision will be made.
In fact, there is no sign of peri-implantitis, although the gingiva remains erythematous (Fig.14). No treatment is rendered. Purulent smell persists for the next 4-5 months in spite of use of Water Pik. It seems that bone graft is needed.
Return to Upper Incisor Immediate Implant,
Peri-implantitis
Xin Wei, DDS, PhD, MS 1st edition 02/21/2016, last revision 07/10/2016