.jpg)








 |
 |
 |
 |
 |
|
.jpg) |
 |
 |
 |
||
 |
 |
 |
 |
 |
|
 |
 |
 |
 |
||
 |
 |
||||
Clearance from Partial
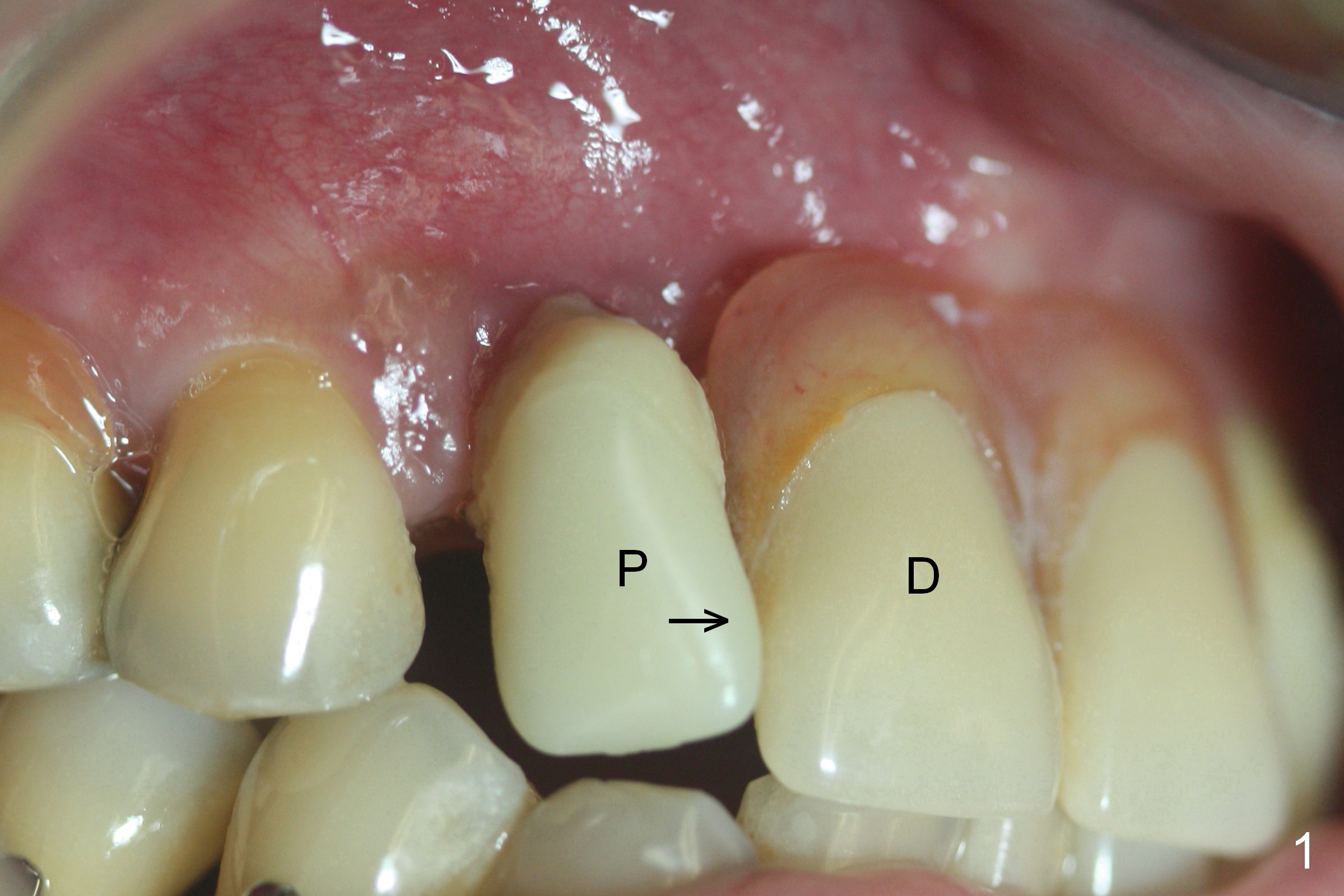
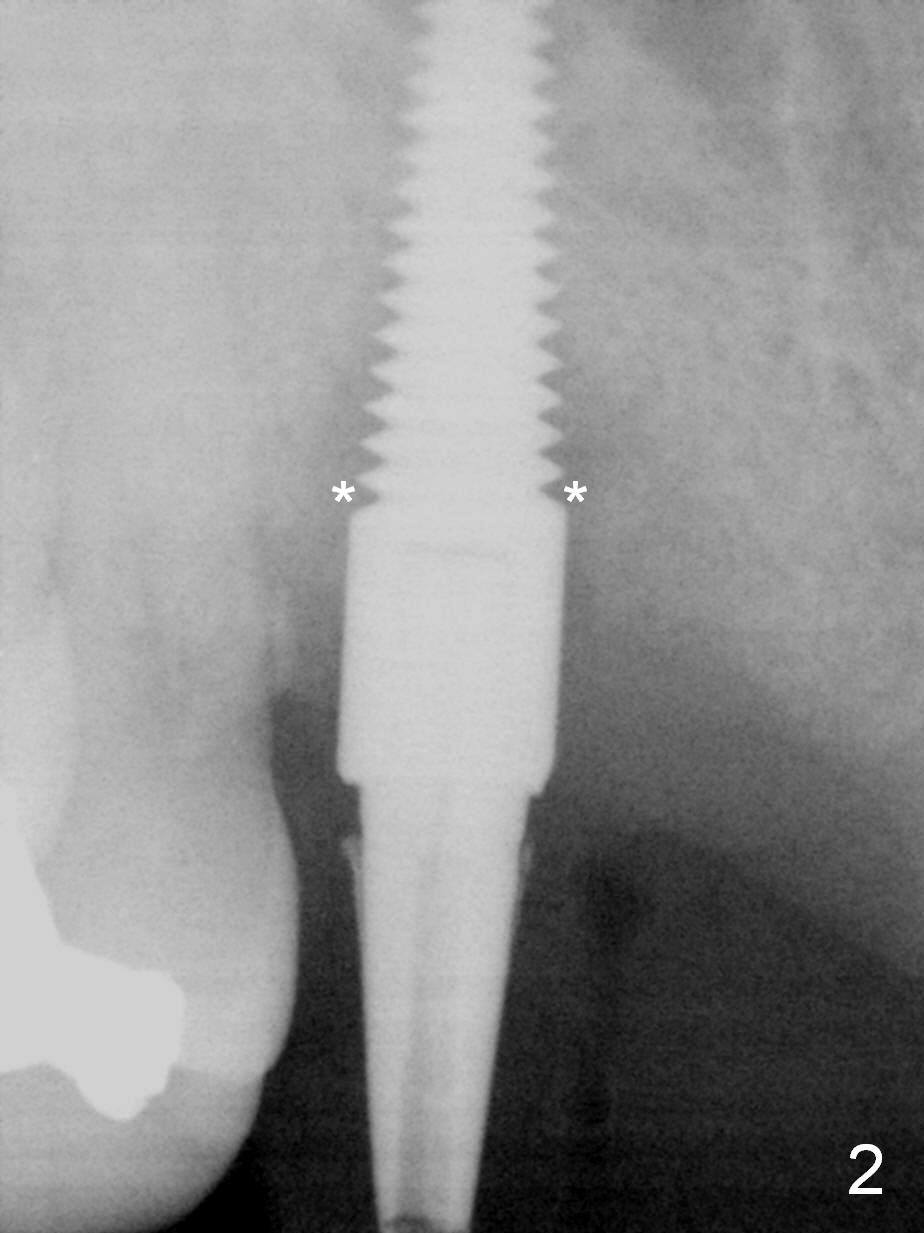
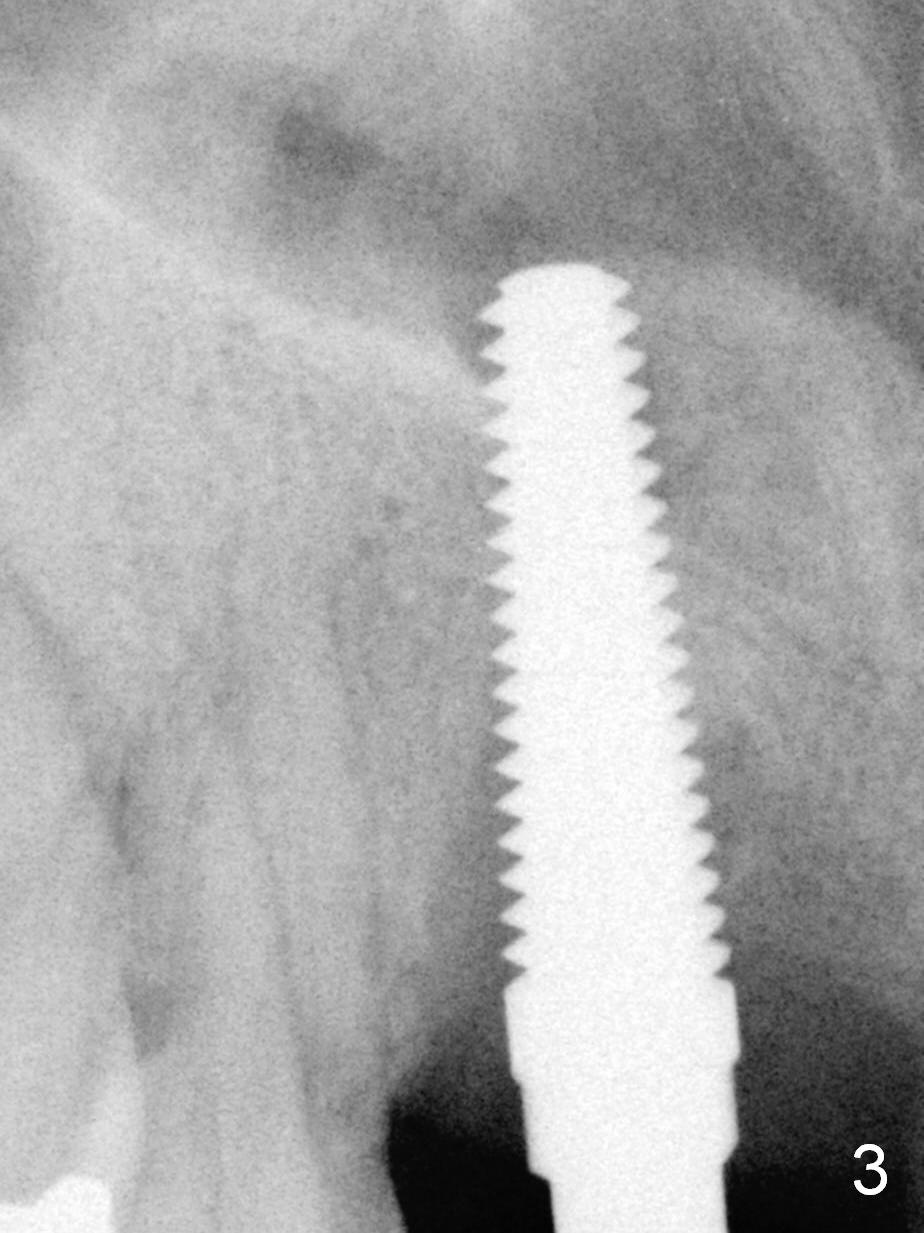
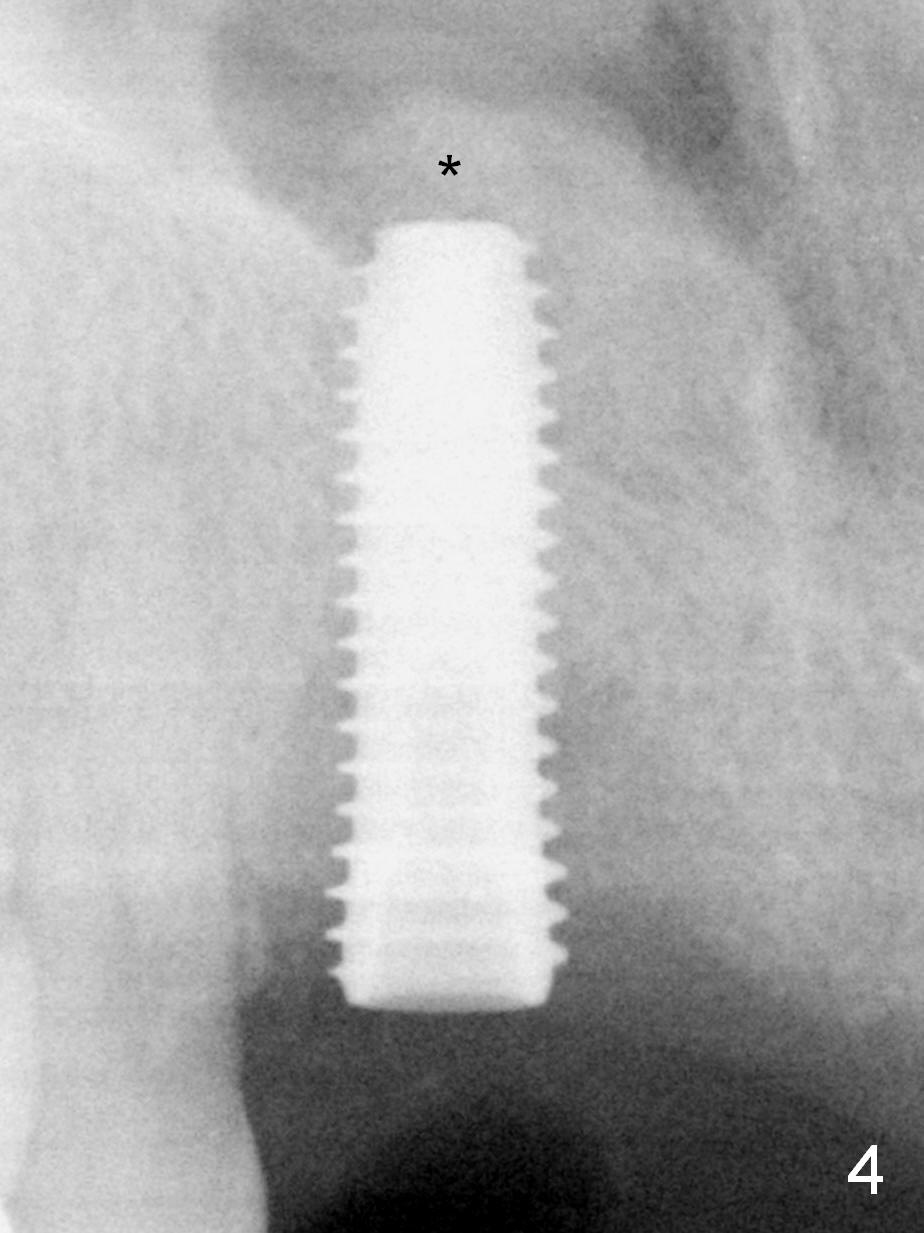
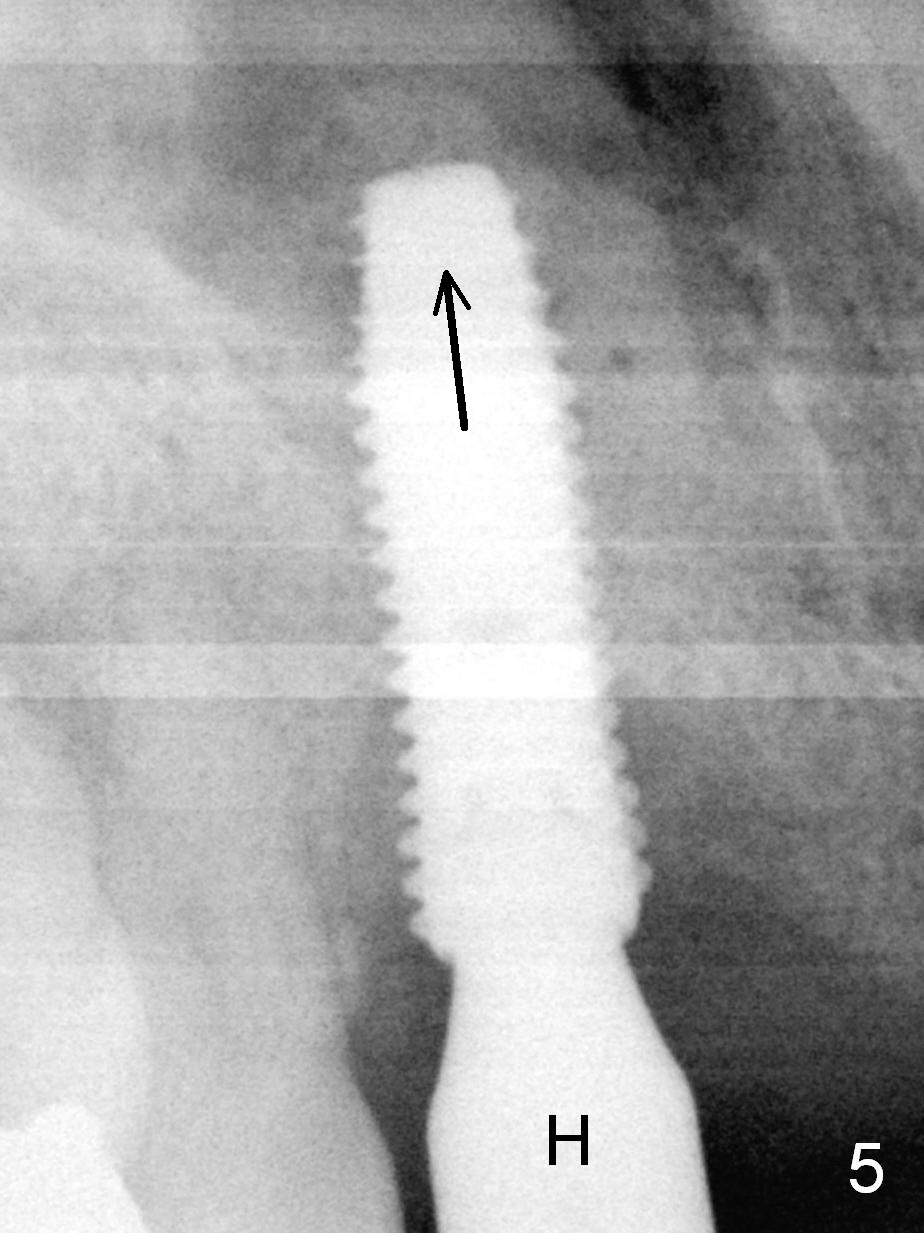
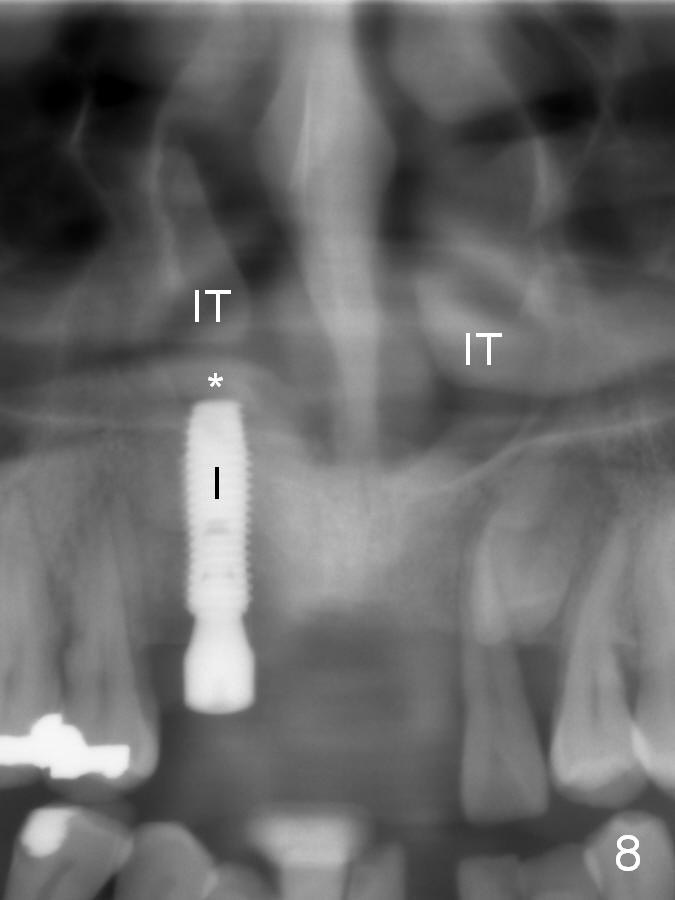
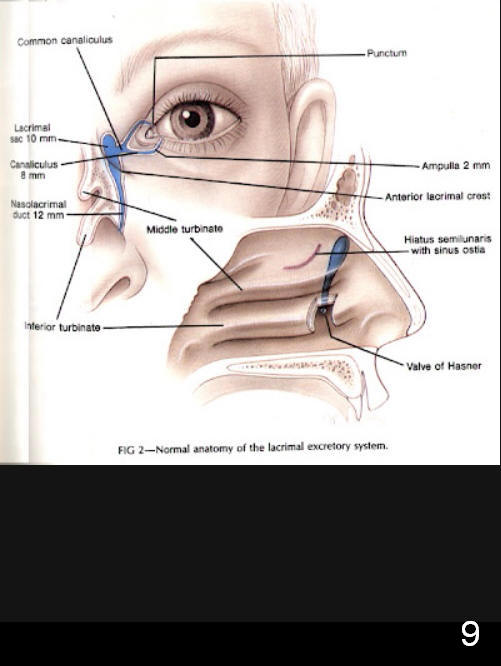
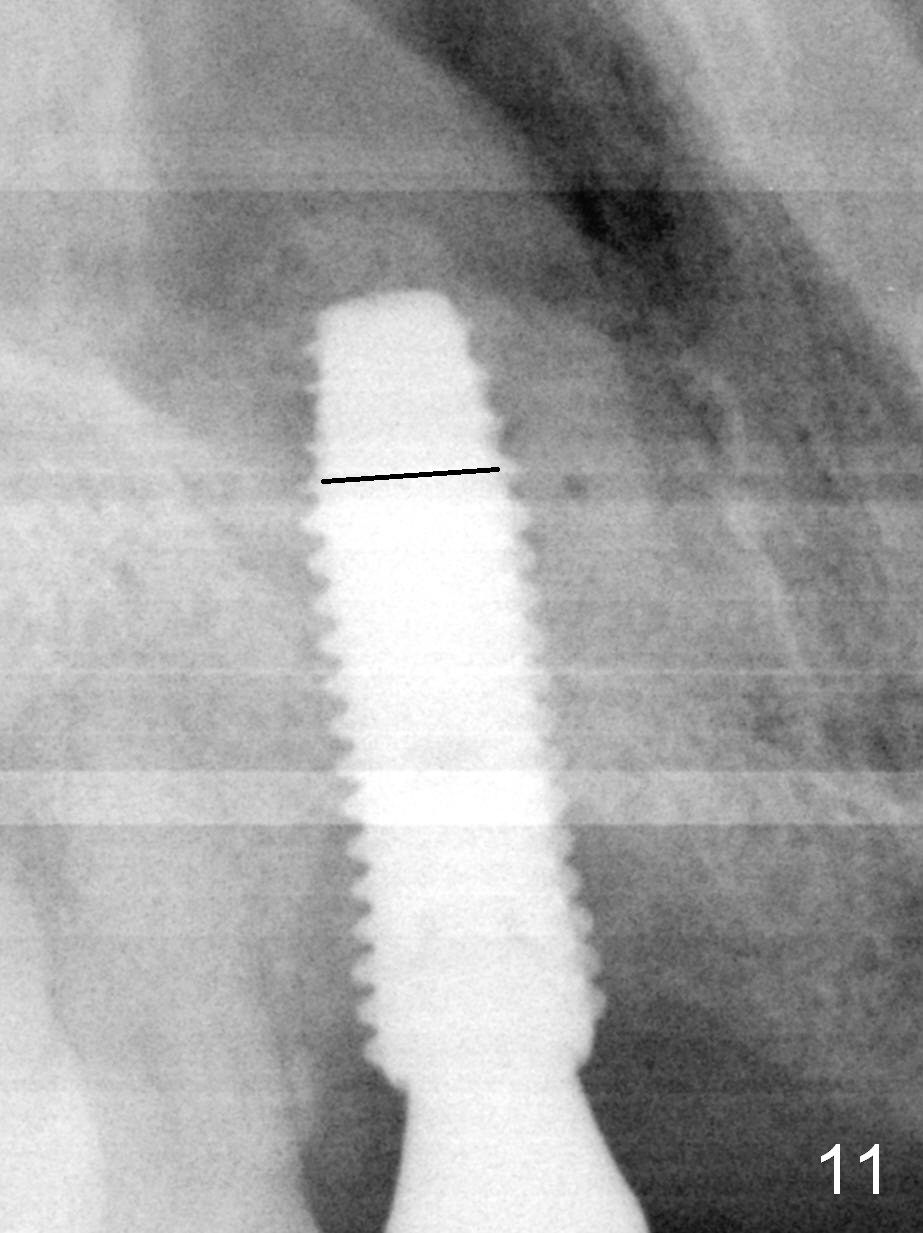
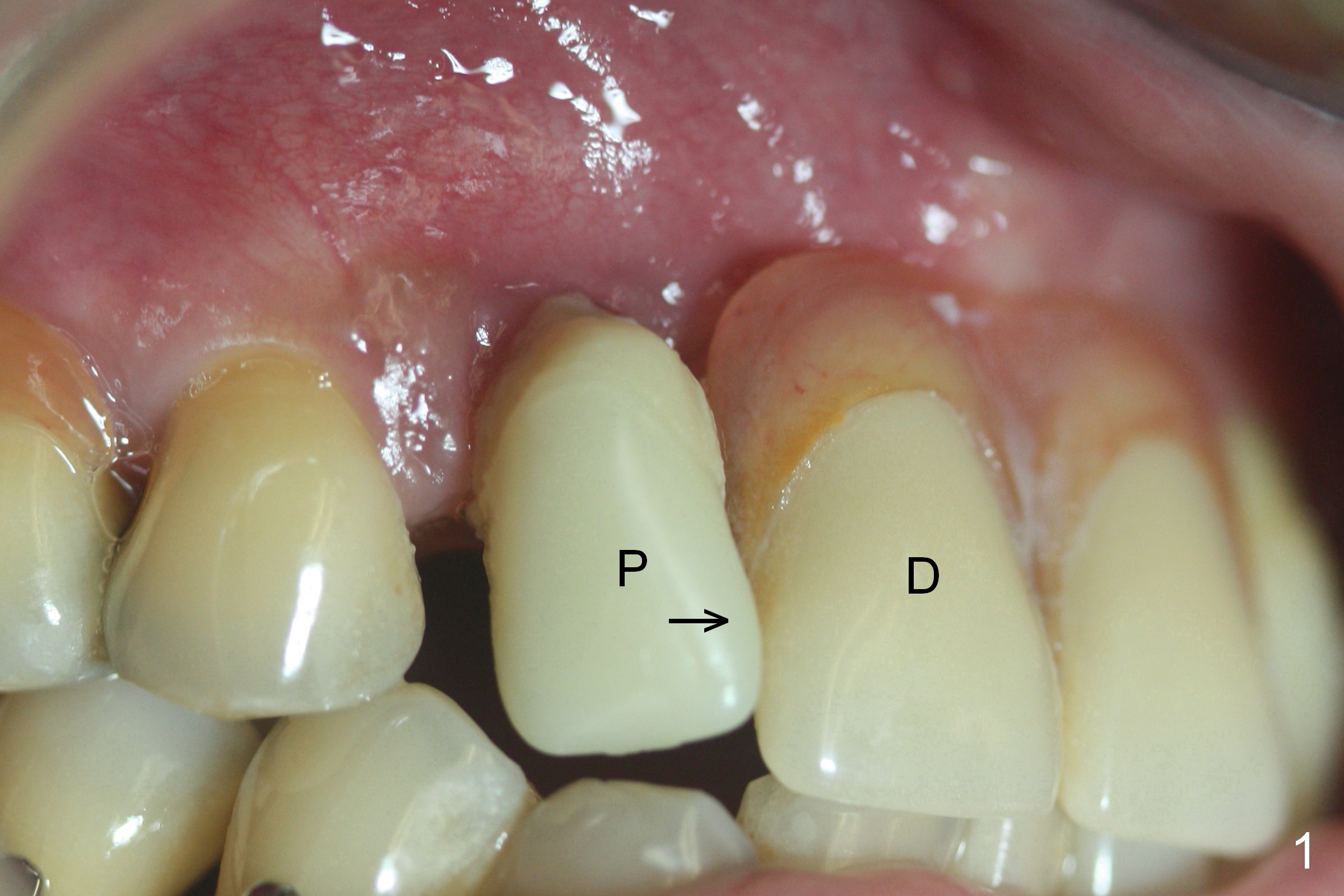
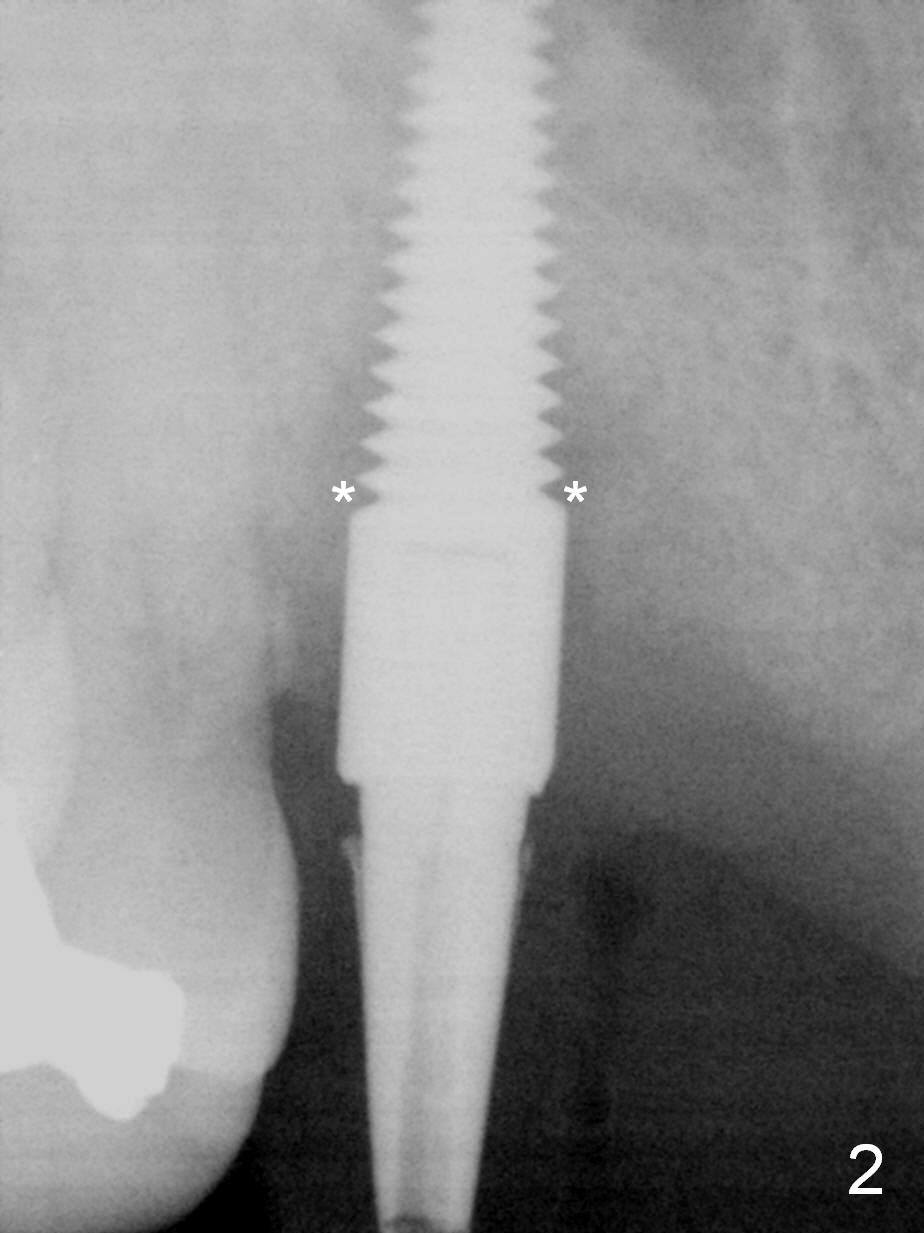
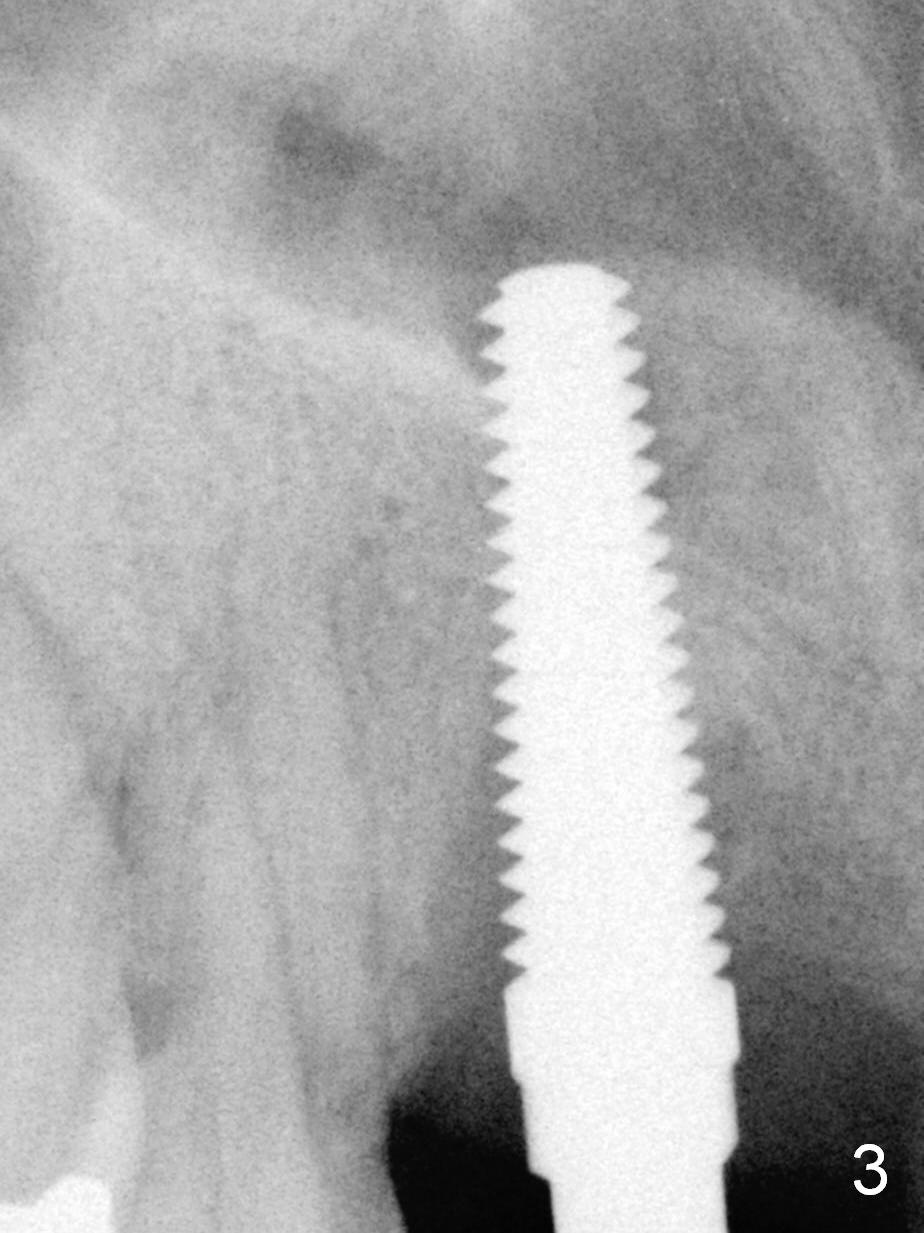
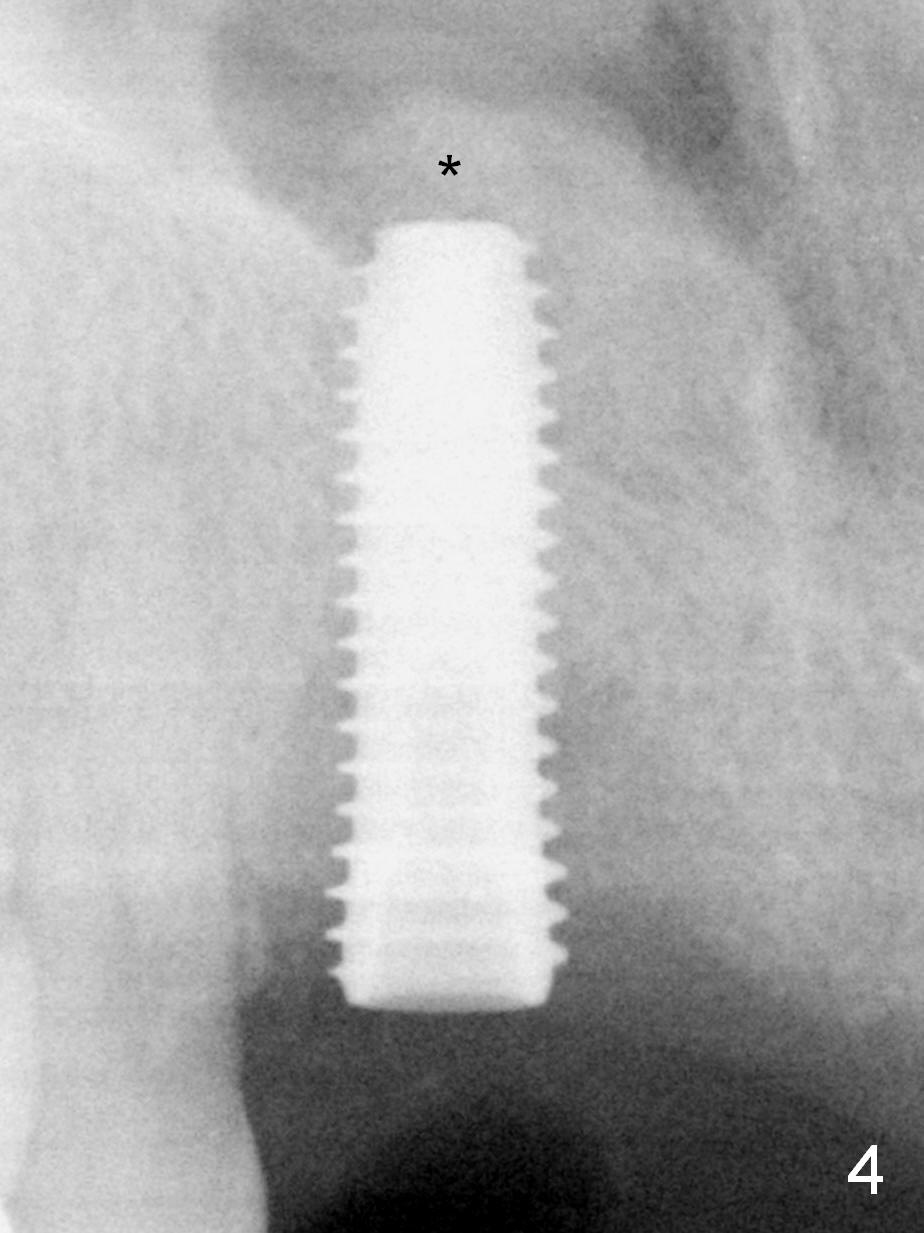
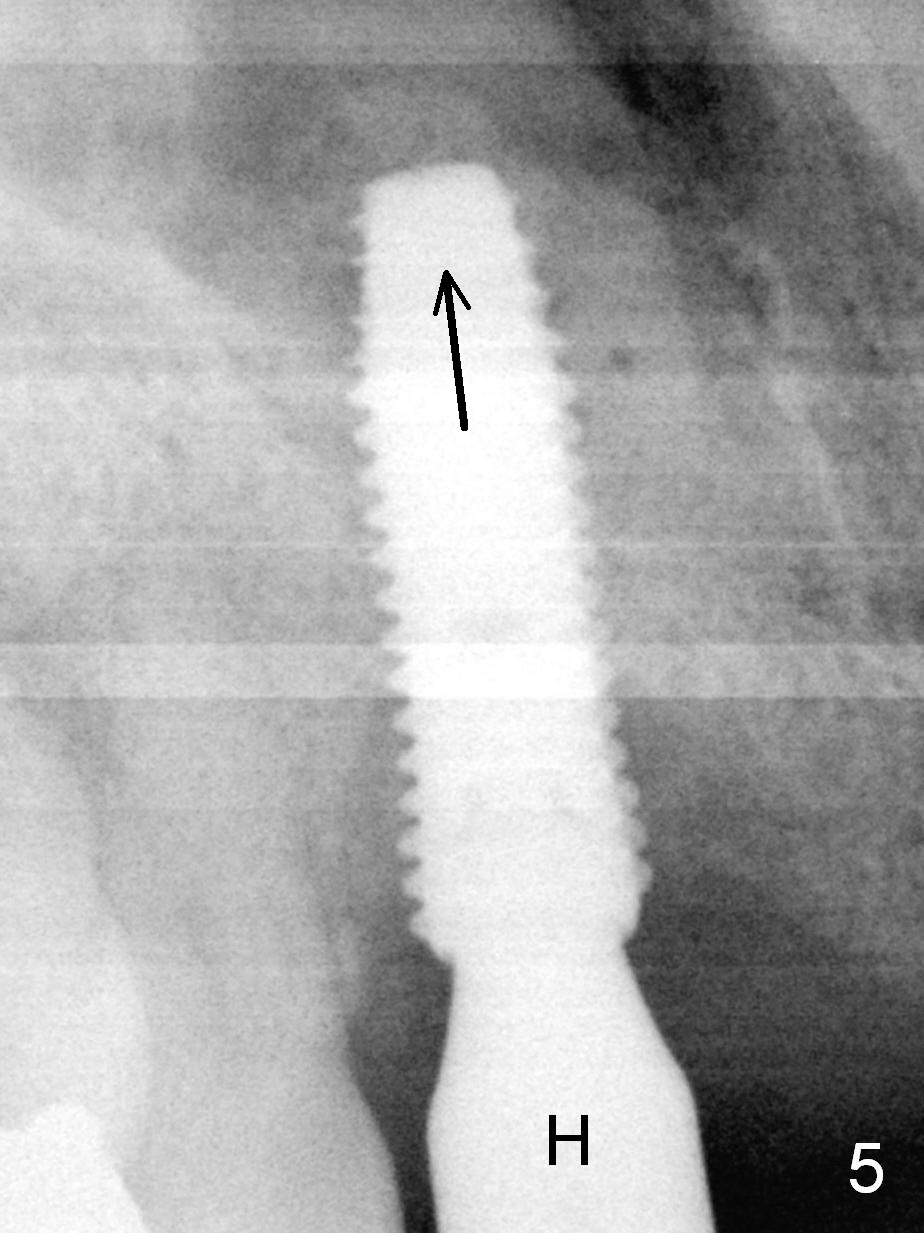
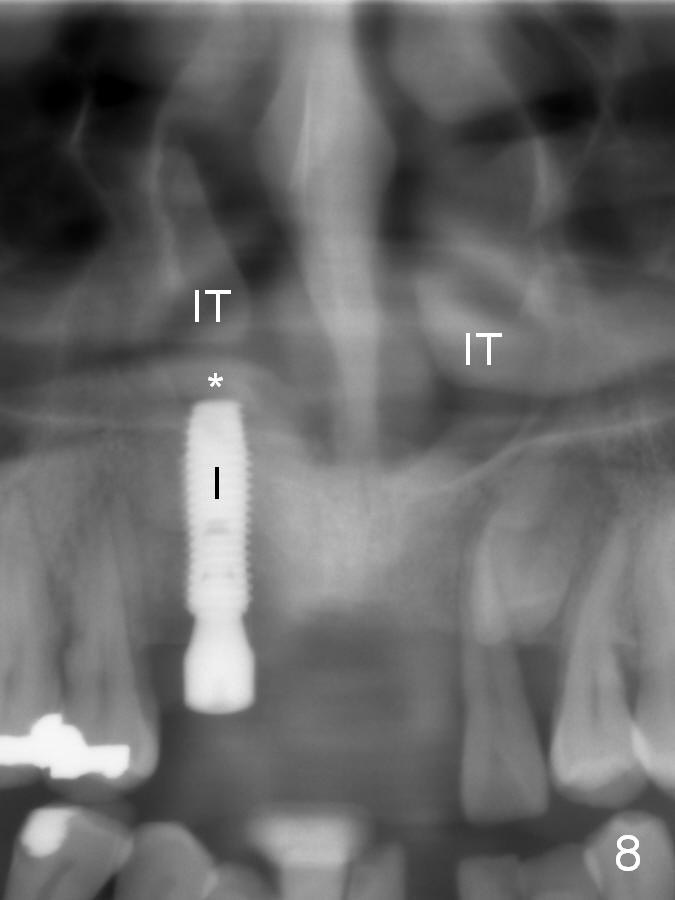
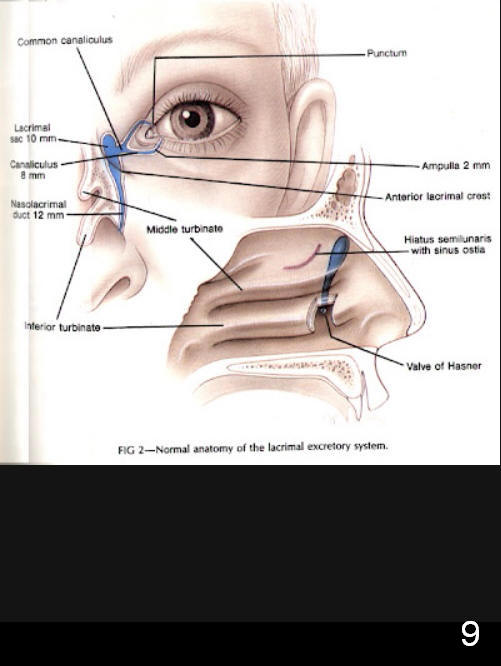
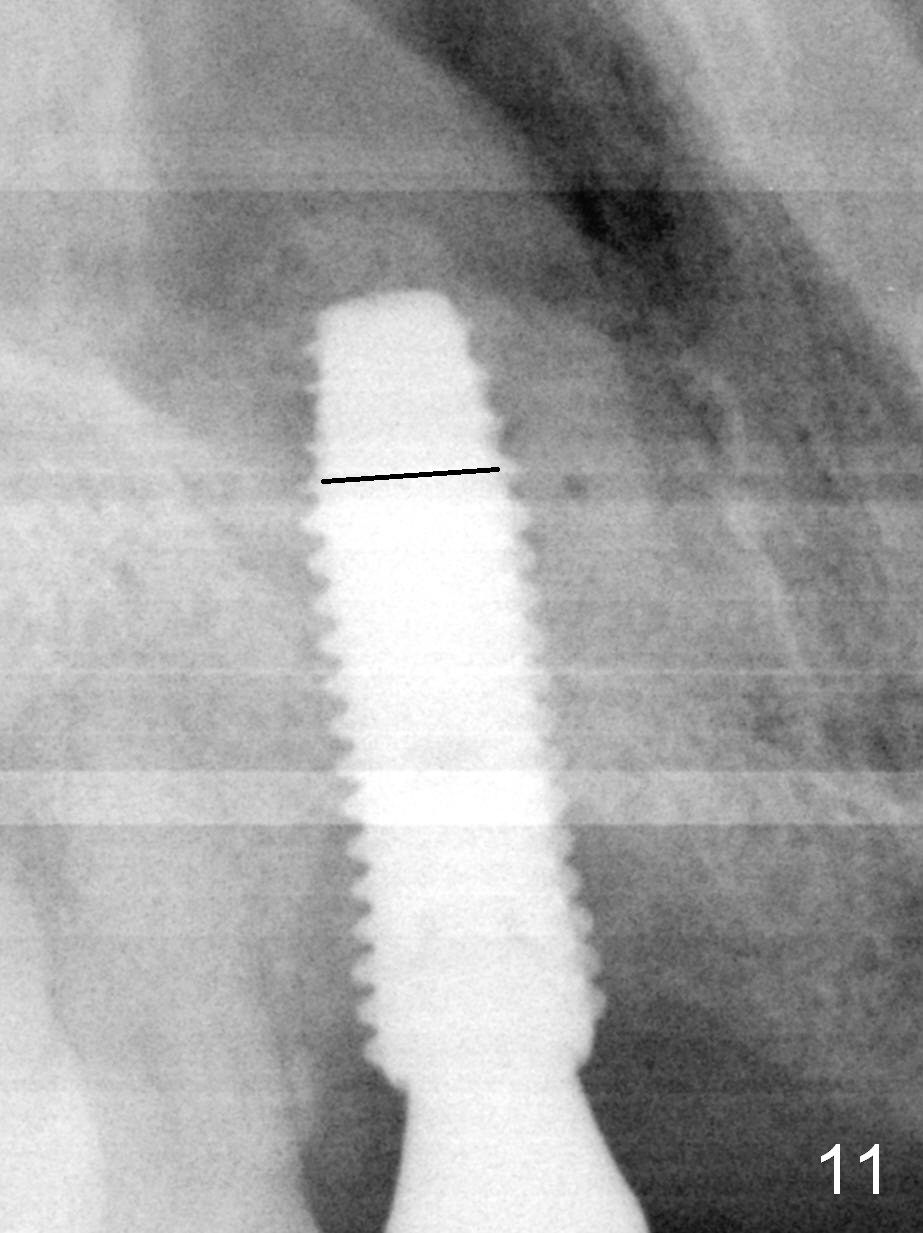
Four months postop, the immediate provisional (Fig.1 P) appears to have shifted mesial (arrow). There is radiolucency around the implant (Fig.2 *). It is painful to remove the provisional. After local anesthesia, the implant is removed with the provisional. Fortunately the osteotomy wall is intact. After Metronidazole treatment, a 5x20 mm tap is placed with stability (Fig.3). After placement of allograft for nasal floor lift (Fig.4 *), a 5x16 mm bone-level implant is placed with insertion torque ~ 35 Ncm. The implant is placed deeper by 2 mm (Fig.5 arrow), followed by placement of a 5.5x7(4) mm healing abutment (H, Fig.6). The loss of the implant is probably due to mobility of the partial denture against the immediate provisional. Enough clearance is provided between the healing abutment and the partial denture (Fig.7 arrowheads). Immediate postop complaint is watery discharge from the right nostril, probably related to the long implant, displacing the Inferior Turbinate (Fig.8 (panoramus taken 8 days postop) IT) and blocking the opening of the nasolacrimal duct (Fig.9). There is a limited empty space in the nasal cavity (Fig.10 *, as compared to the maxillary sinus (S)). The discharge relapses. It appears that the apex of the implant should be truncated for 3-5 threads (Fig.11 black line). Soak a piece of 2x2 gauze in Metronidazole; it will be used to hold the implant outside the mouth for sectioning. Do not prepare bone graft, which in fact should be removed from the nasal cavity (below the nasal floor mucosa (Fig.4,8 *)). Prescribe Medrol dose pak to reduce postop edema.
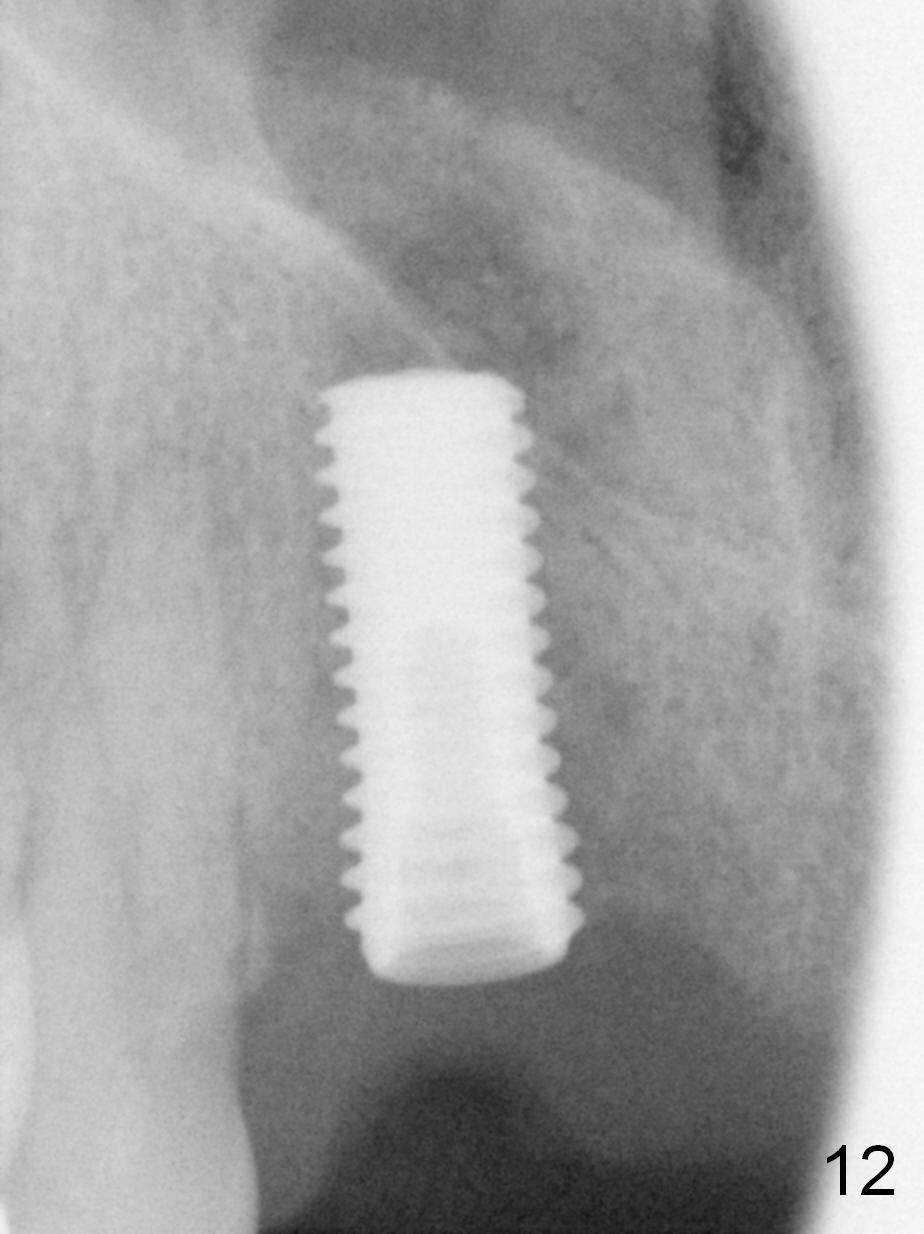
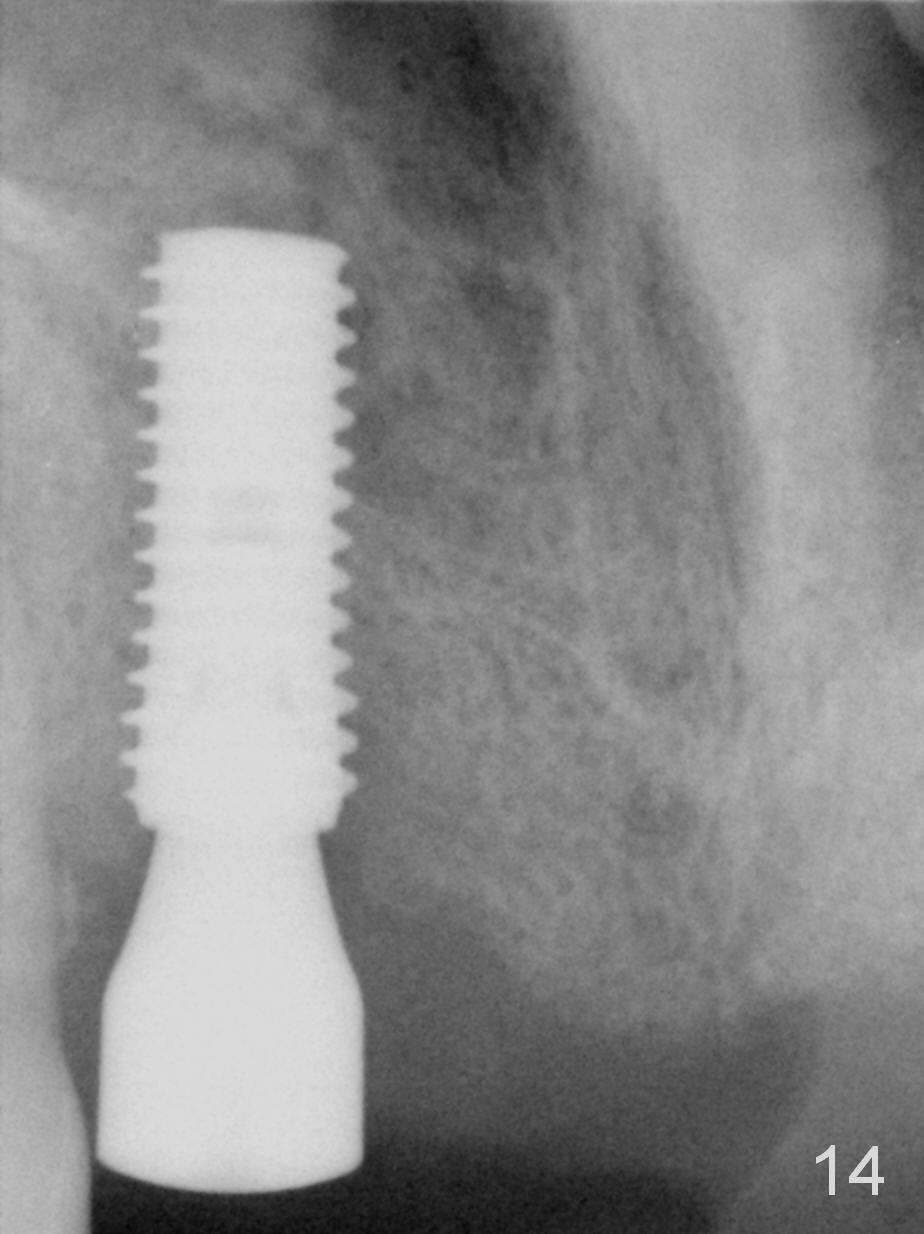
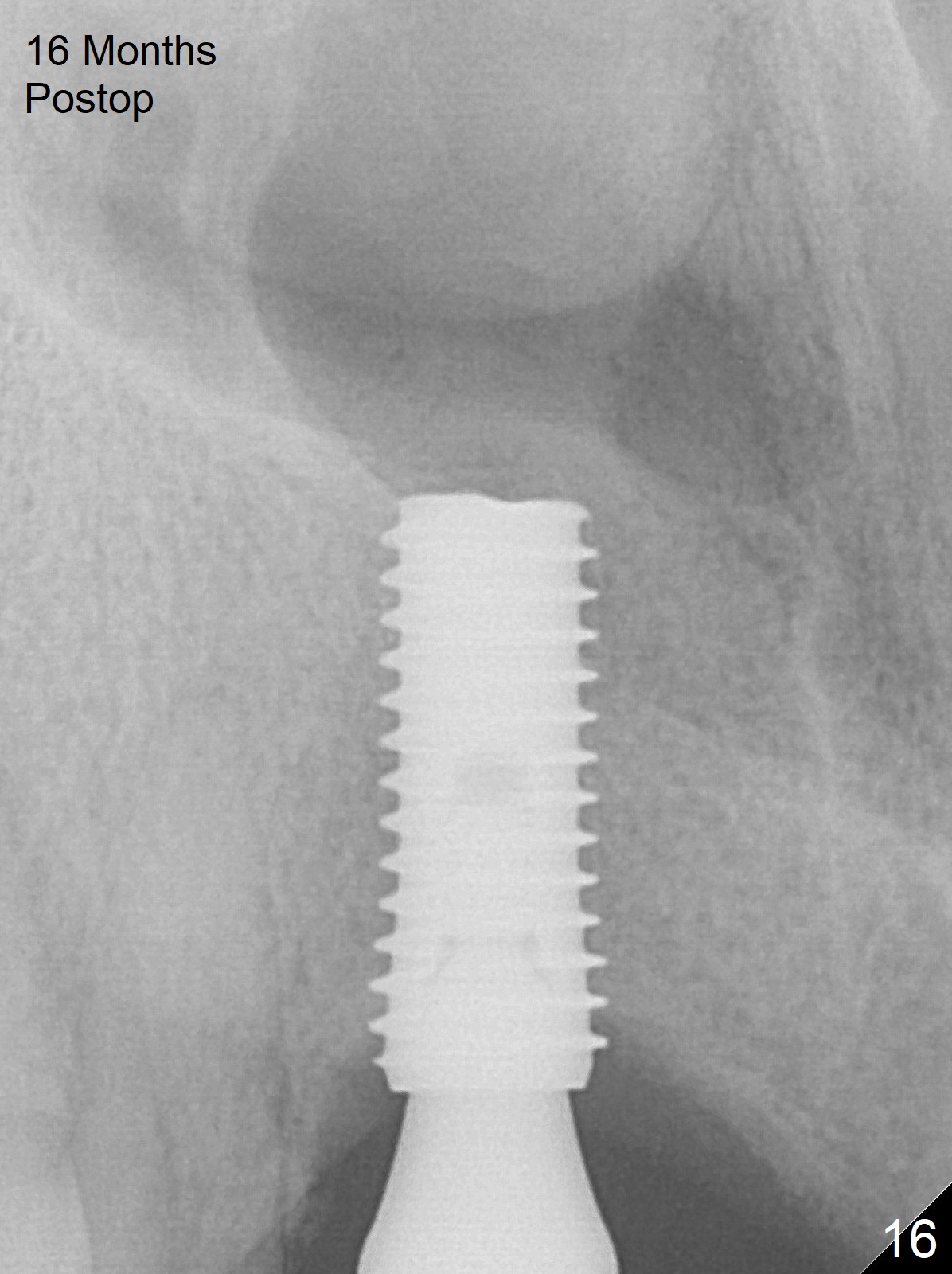
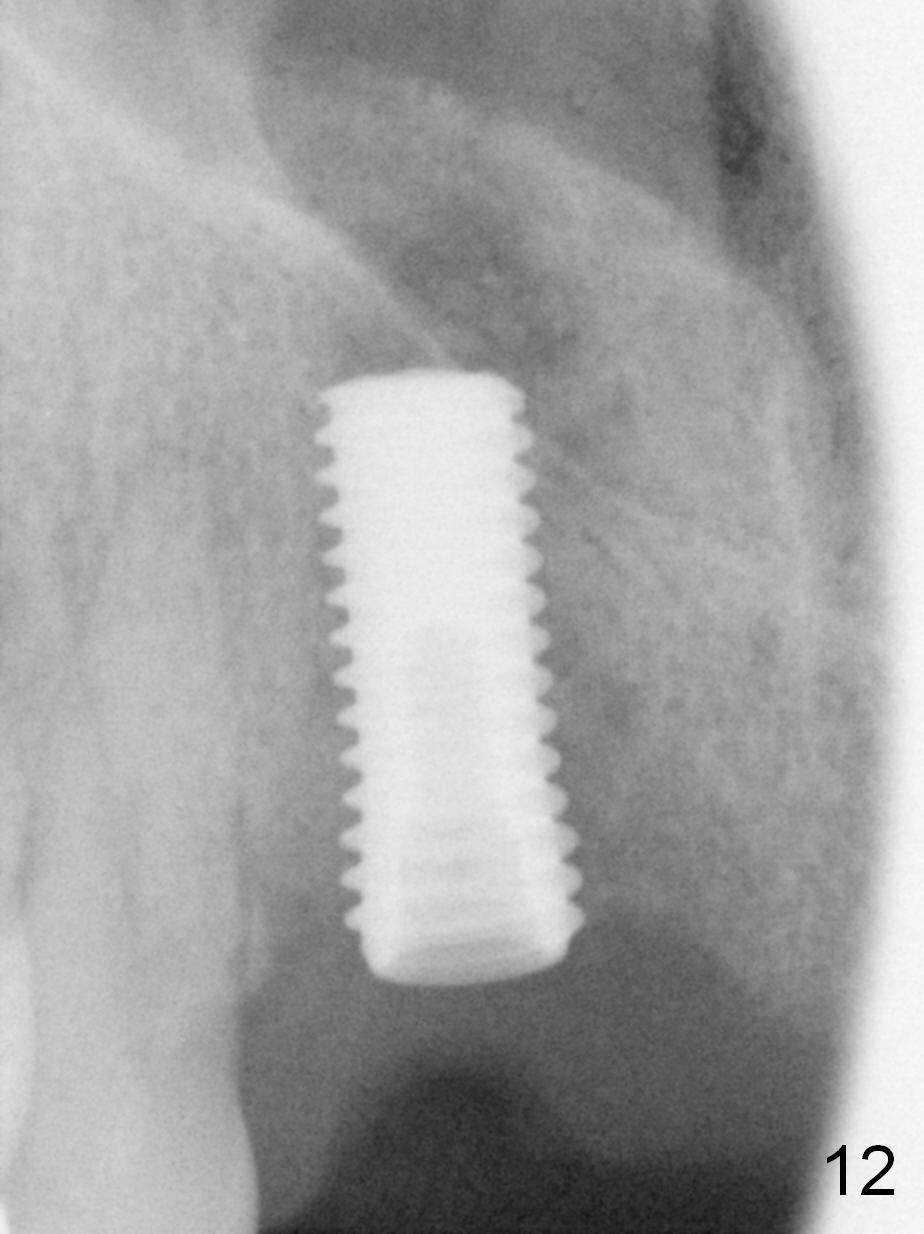
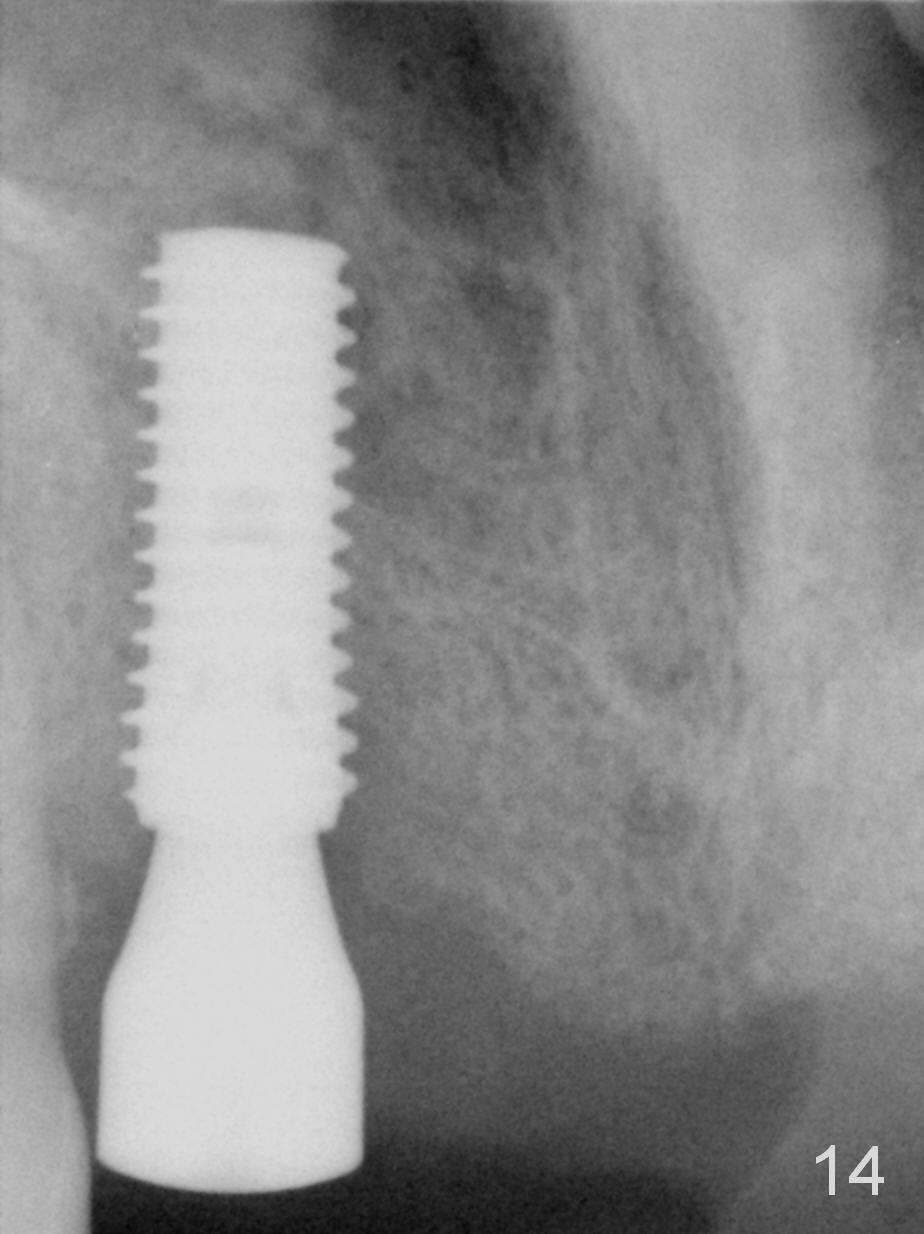
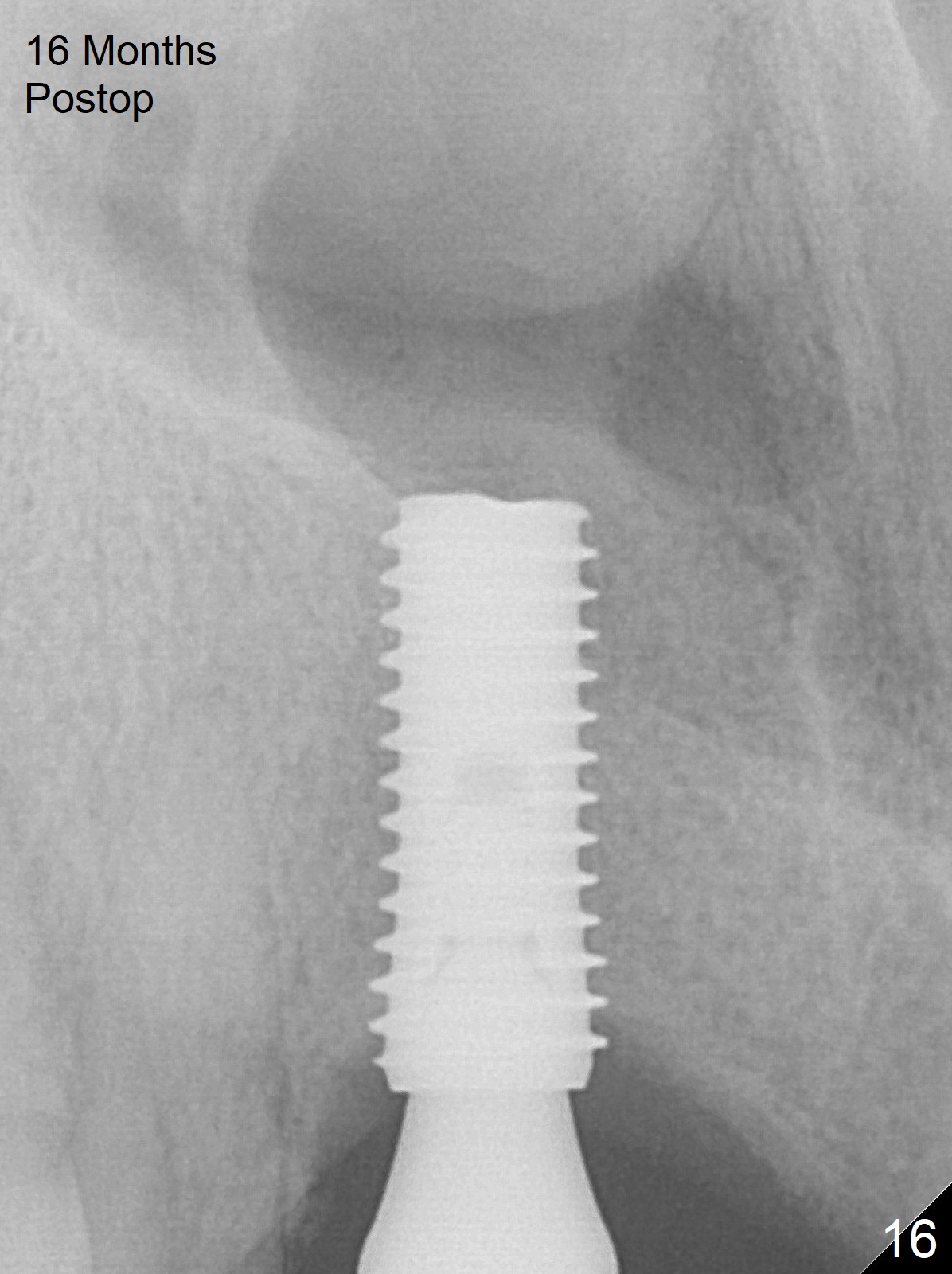
While the implant is being truncated between the apical 3rd and 4th threads, a question is being asked whether the implant will be engaged to the osteotomy once the apical tapered portion is removed. In fact there is no problem (Fig.12). To prevent coronal thread exposure and subsequent periimplantitis, the implant is placed deeper (Fig.13). Then it is placed more coronal (Fig.14,15). No attempt is tried to bring out bone graft. The patient returns 16 months postop (Fig.16). The healing abutment is loose. When the latter is retightened, the underlying implant seems to be stable.
There is gingival recession (Fig.17 *); please use pink porcelain. Tooth shade is A3. Either trim the gingiva of the denture tooth #8 in the model (Fig.18 white curved line) or leave a space incisally (between arrowheads); otherwise the denture cannot be seated due to the presence of the undercut.
Although the patient does not like the open bite associated with the implant crown at #7 (Fig.19; 1.5 months post cementation), the apparently non-keratinized gingiva remains healthy apical to the gold-coated abutment (Fig.20).
Return to Upper Incisor Immediate Implant
Xin Wei, DDS, PhD, MS 1st edition 03/04/2016, last revision 01/19/2018