


















 |
 |
 |
 |
 |
|
 |
 |
 |
 |
 |
|
 |
 |
 |
|||
 |
 |
 |
|||
 |
 |
 |
 |
||
Tuberosity Bone Graft for Labial Plate
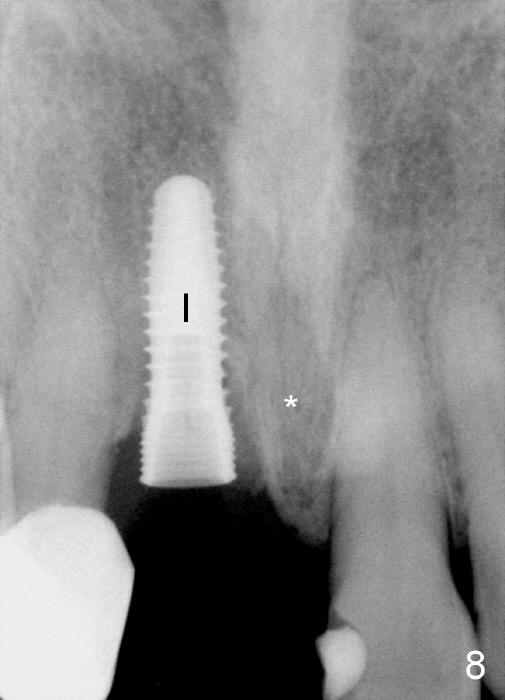
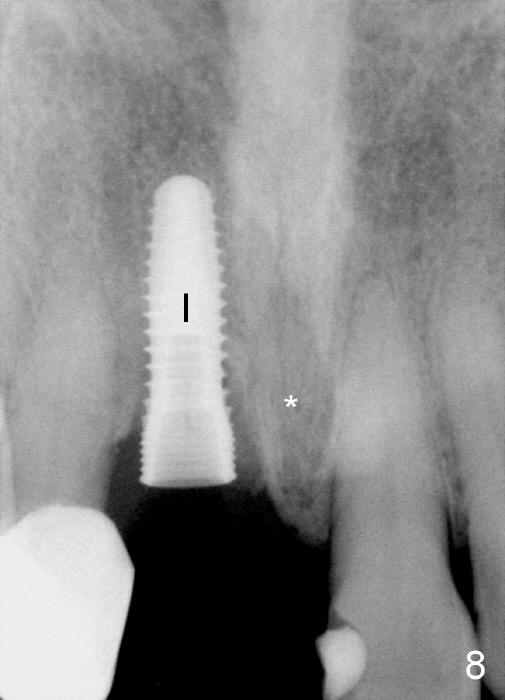
A 64-year-old lady requests replacing #7 and 8 crowns (Fig.1,2). When #8 is extracted, the labial plate is found to be missing (Fig.3). Following 2 mm pilot drill (Fig.4,5 P), 3.8 mm tap drill (Fig.6,7 T) and 4.5x14 mm implant (Fig.8 I) and 4.8 mm abutment (Fig.9 A), corticocancellous bone is harvested from the left tuberosity and placed in the labial gap of the socket (Fig.10 G). Collagen dressing is placed over the bone graft (Fig.11 C). The former is secured in place by an immediate provisional (P).
The autogenous bone graft from the tuberosity is mainly cancellous. It consists of small pieces. They are easily packed into the labial gap. The small portion of the cortical bone provides meshwork and may retard resorption.
The patient returns for follow up 8 days postop and the labial margin of the provisional looks long. The metal crown is changed to a provisional at the visit. Eight days later, the provisional at the site of #8 is removed for labial margin trimming; the labial gingiva heals (Fig.14 *). The labial plate remains slightly convex (Fig.15). The labial margin of the provisional at the site of #8 is at the same level of that of #9.
Four-month follow up shows that bone graft from the tuberosity appears to have healed with the implant microthreads (Fig.17 *); there is a diastema between #8 and 9 (arrowheads). Before removal of the provisionals of #7 and 8 for final impression, new composite is added to the mesial surface of #9 as the first step of closure of the diastema (Fig.18 <).
One year post cementation, there is cortical bone formation mesial to the implant (Fig.19 <). Buccal concavity is minimal (Fig.20).
Return to Upper Incisor Immediate
Implant
Xin Wei, DDS, PhD, MS 1st edition 08/26/2014, last revision 10/16/2015