

 |
 |
 |
 |
|
 |
 |
 |
||
 |
 |
|||
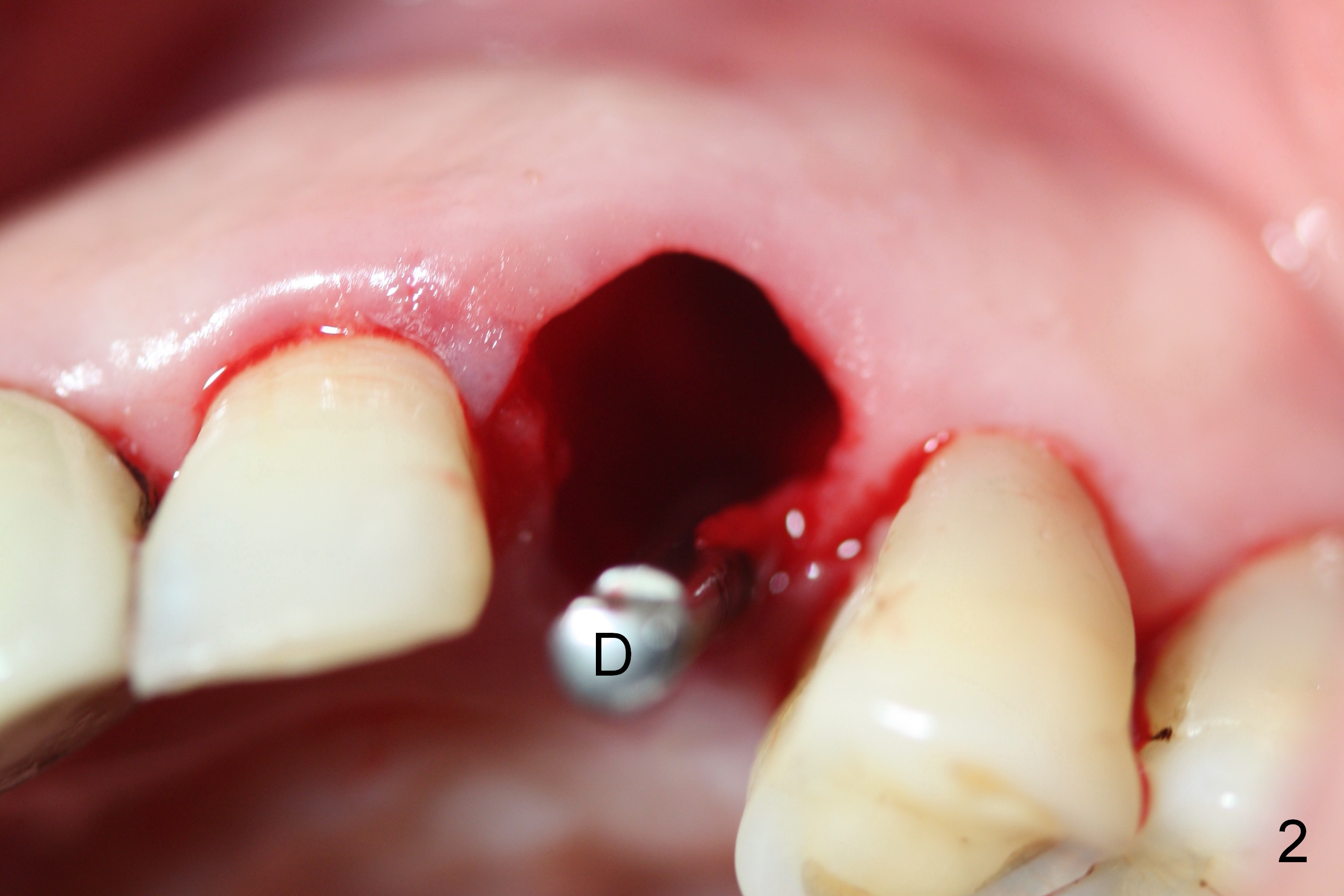
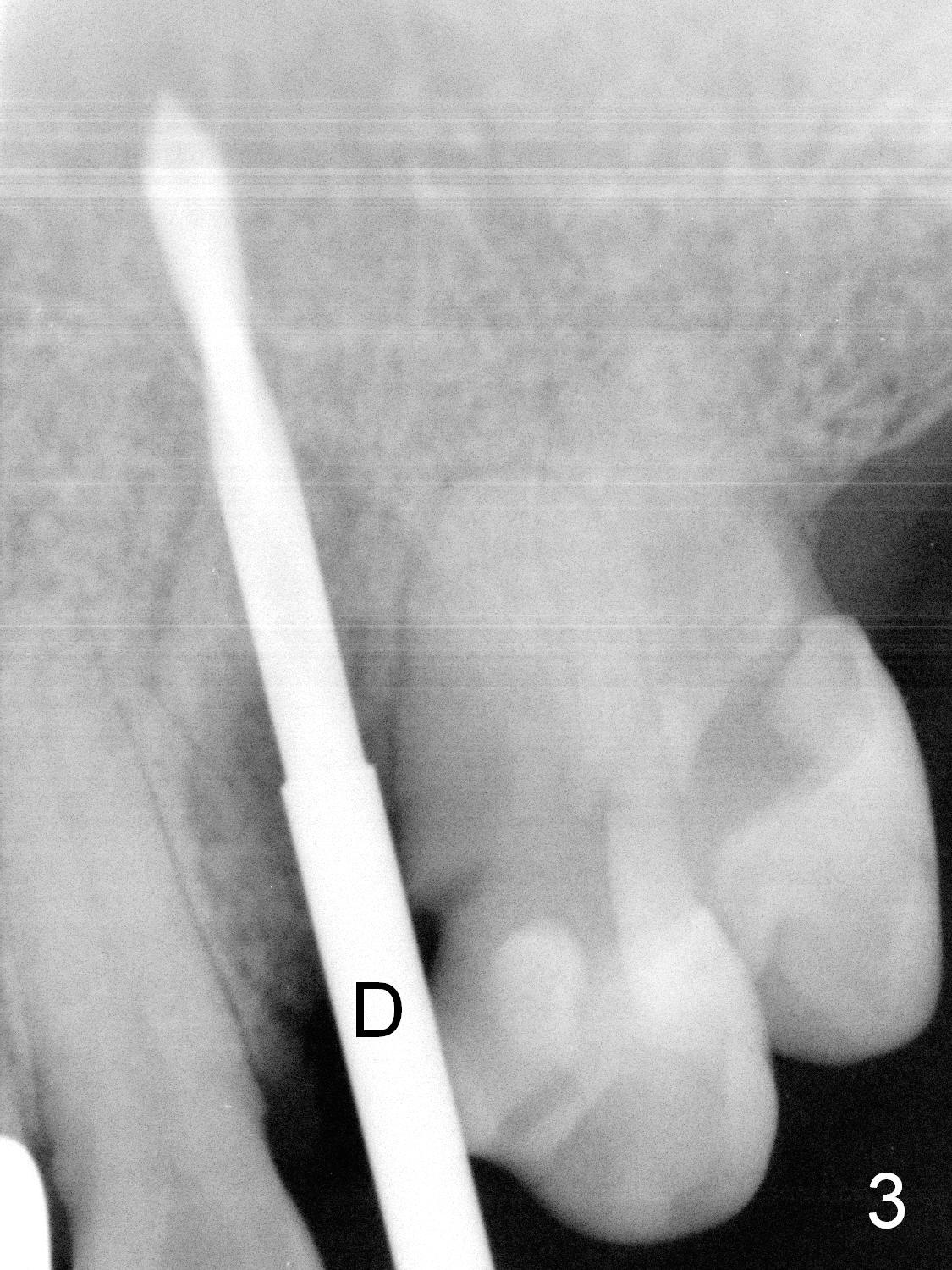
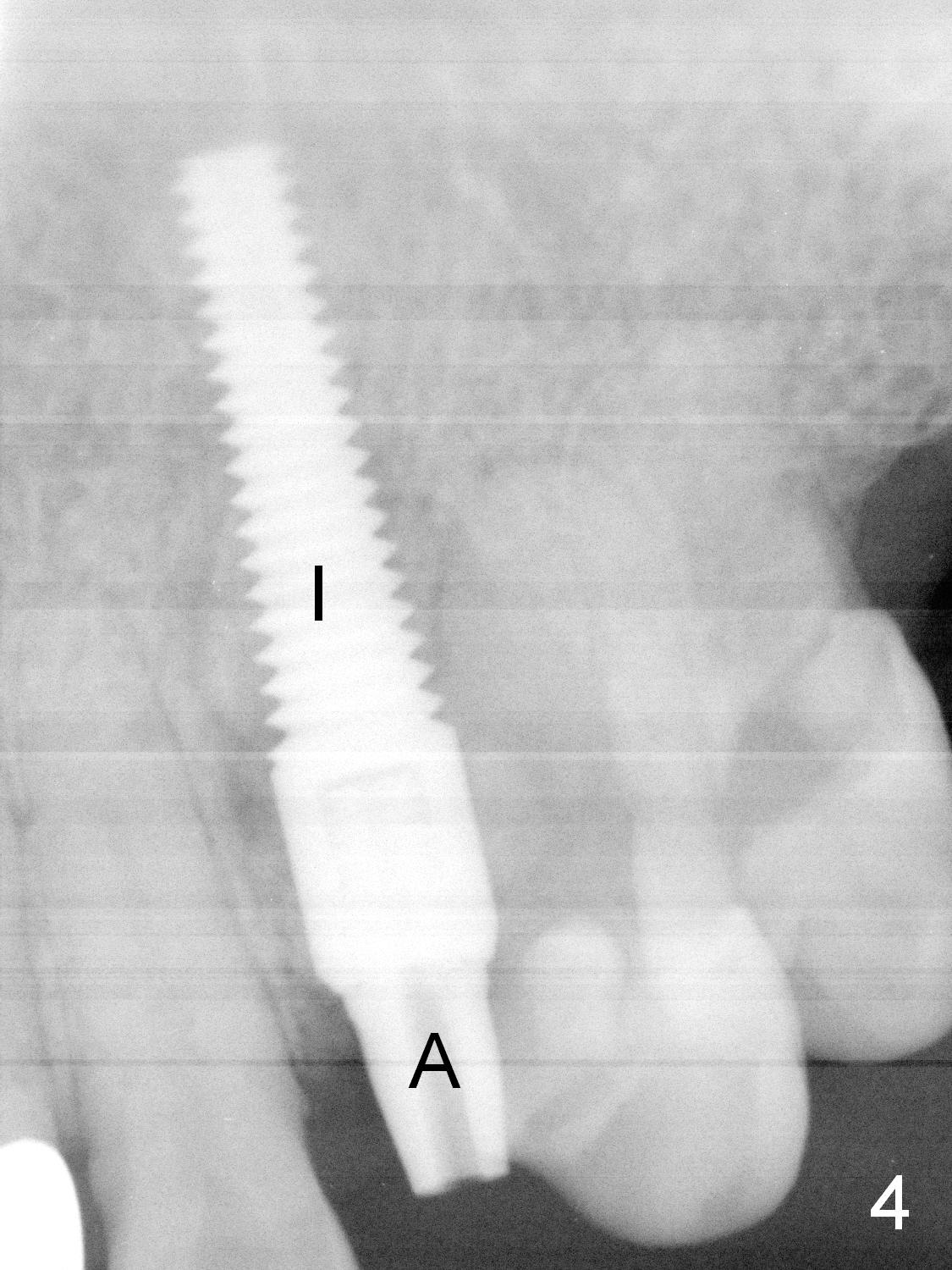
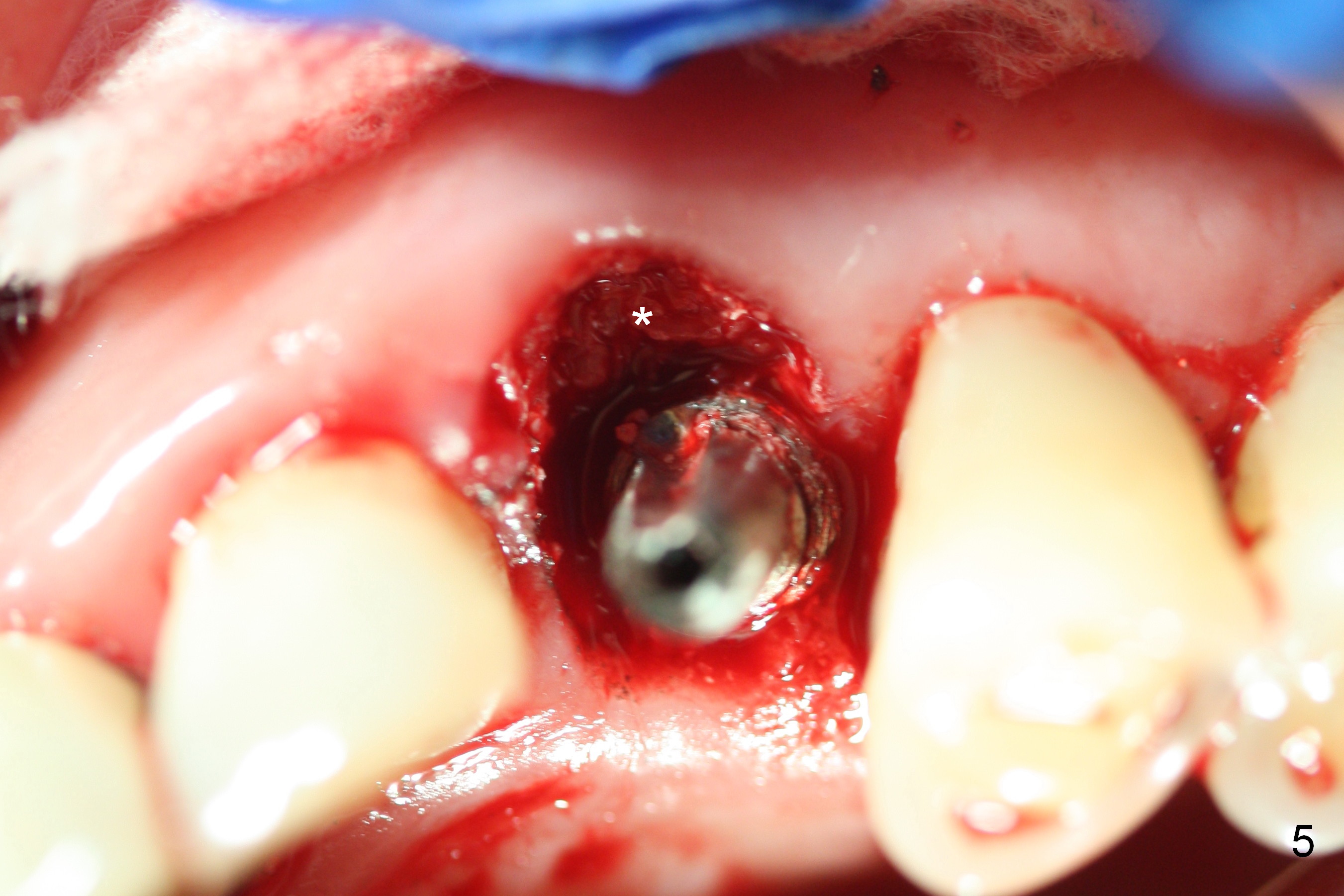
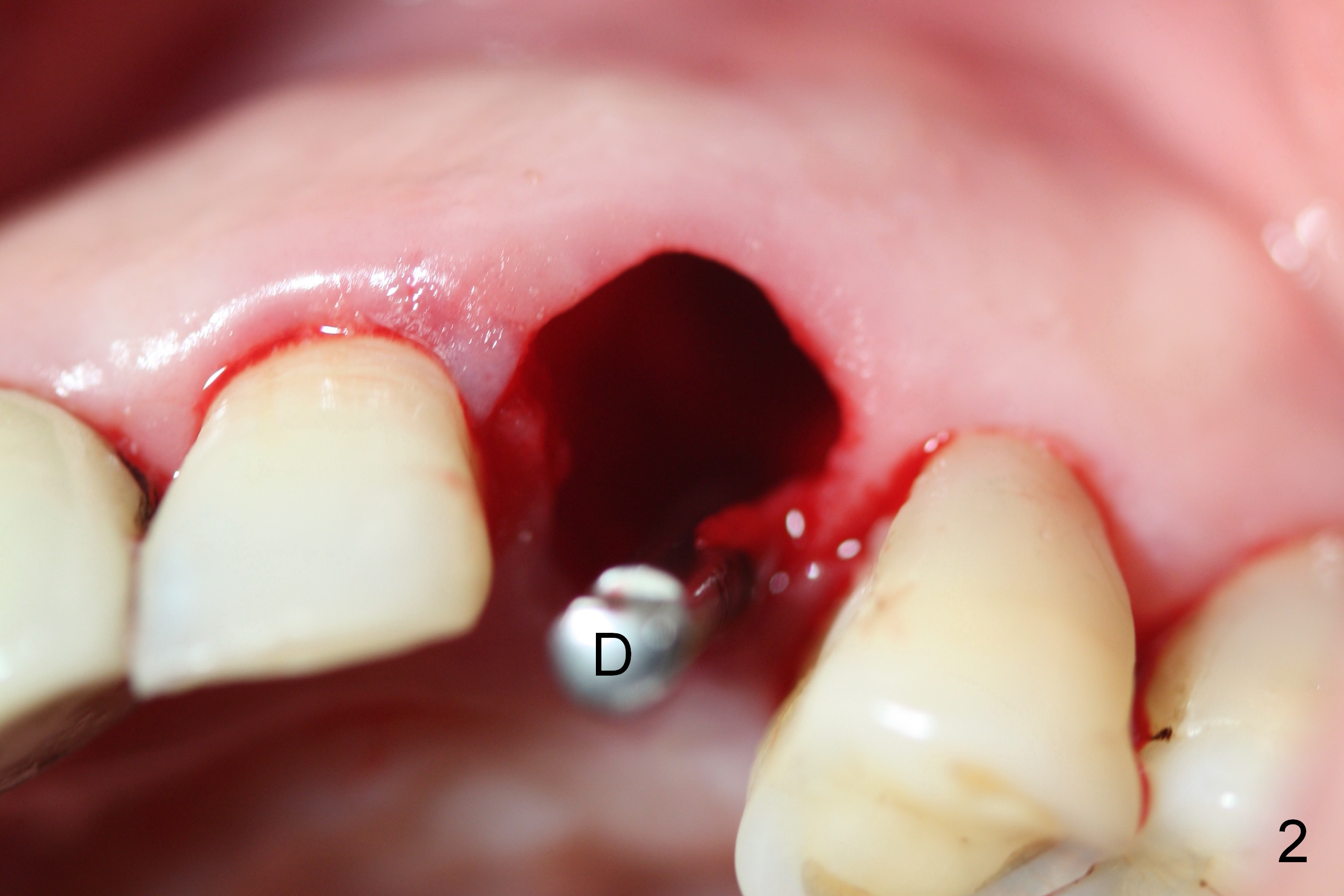
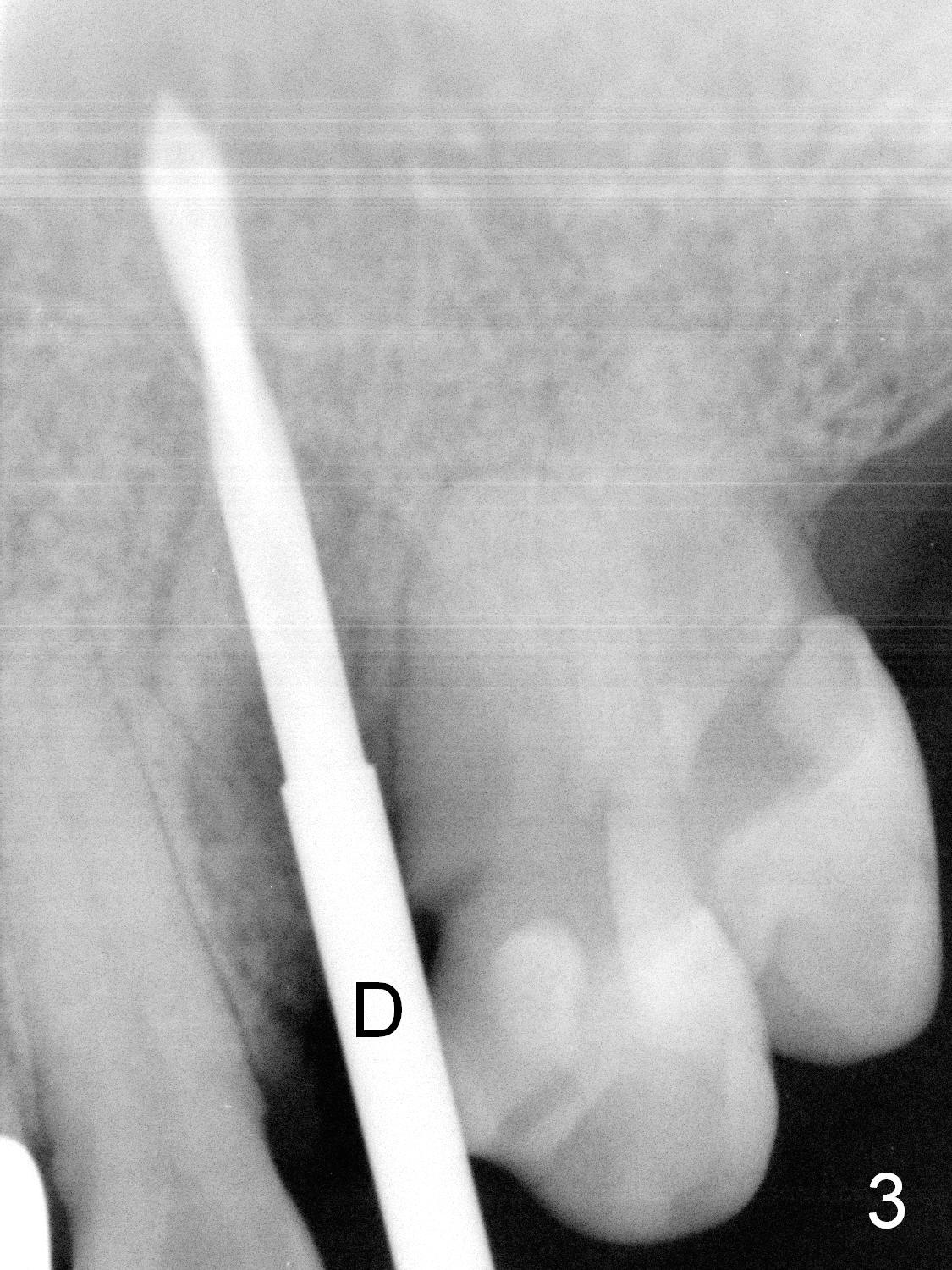
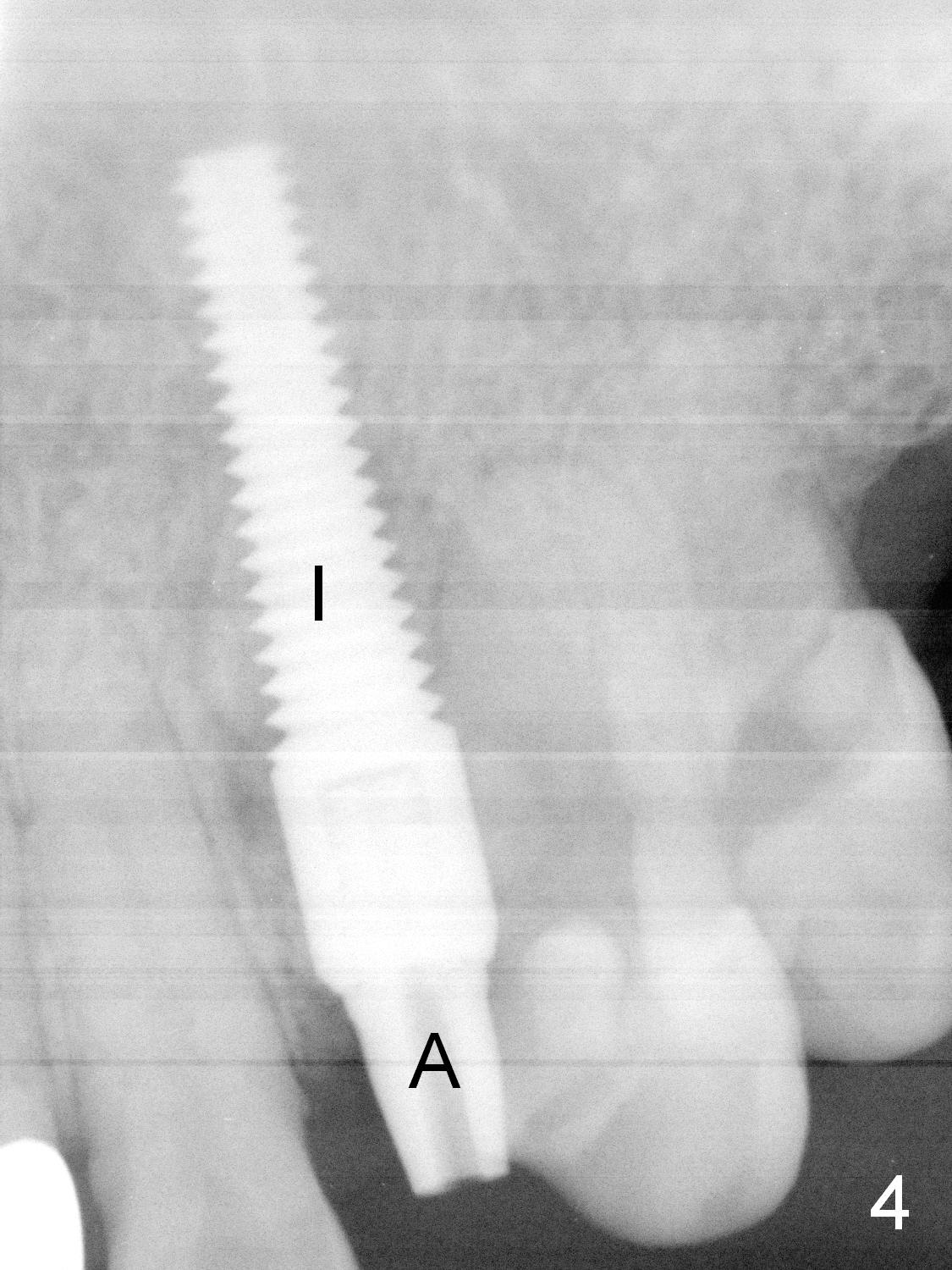
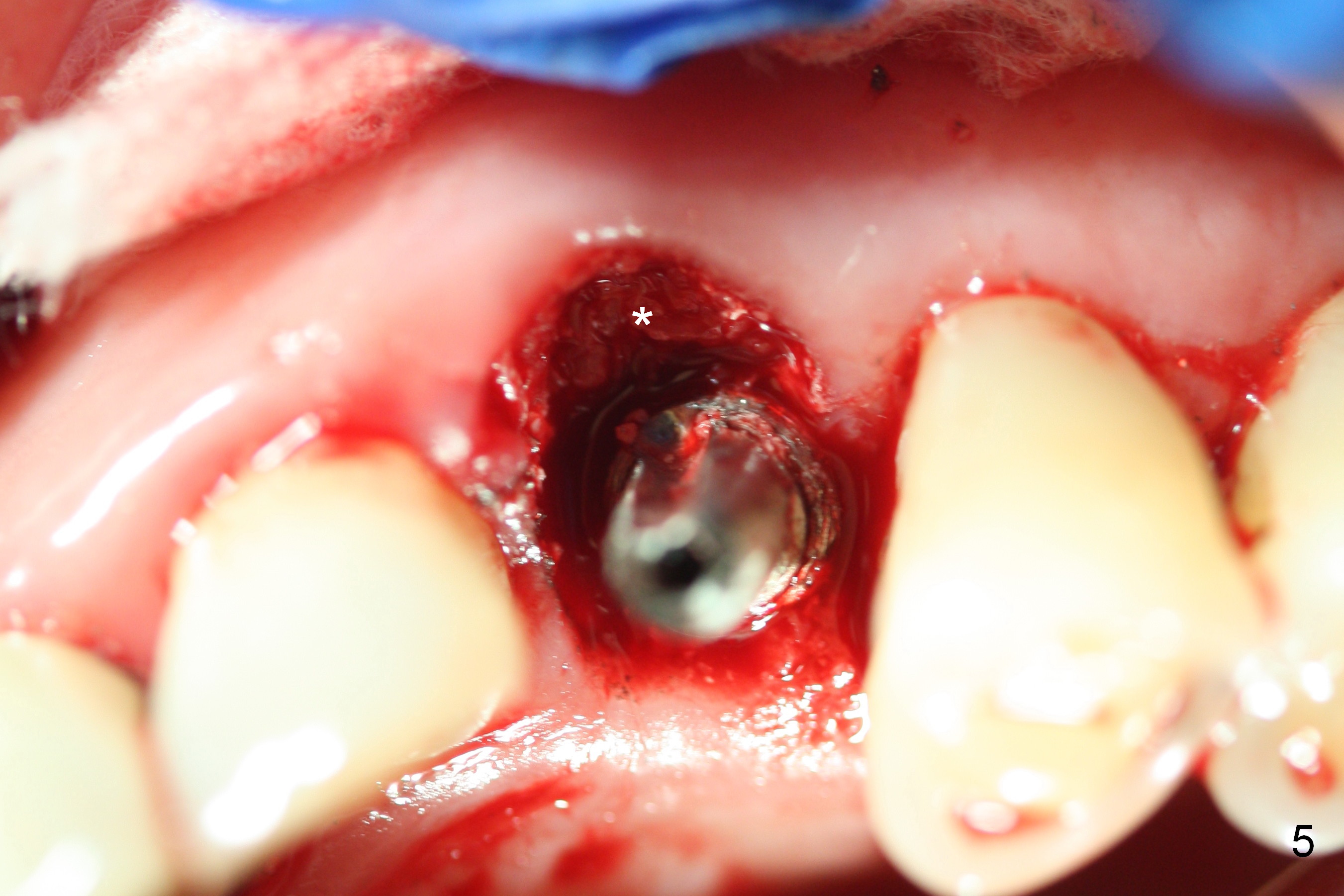
Preop exam shows mild pus (Fig.1 *) in the distal sulcus of the residual root of #11 with deep pocket (without pain). The extraction is easy and finished with a proximator (periotome). Debridement of the socket is intensive. Osteotomy is initiated in the palatal wall with a 2 mm pilot drill (Fig.2,3). There is buccal apical plate perforation. Osteotape is placed against the defect prior to implant placement. Probably due to low density bone and/or over prep, insertion torque of a 4.5x20 mm implant is between 30/35 Ncm (Fig.4,5). The implant/abutment remains palatal, but slightly distal. The occlusal clearance of the immediate provisional is a little too excessive due to low torque (Fig.6). The provisional closes the buccal gap and keeps bone graft (Fig.5 *) in place.
After surgery, the patient reveals that he has been on diet to control his weight because of family history of stroke. It appears that this 74-year-old man has a type of osteoporosis. Attention should be paid to bone density while osteotomy is being made for every immediate implant, in addition to position and trajectory. If the bone feels soft, the osteotomy should be less deep than expected. Under prep is mandatory.
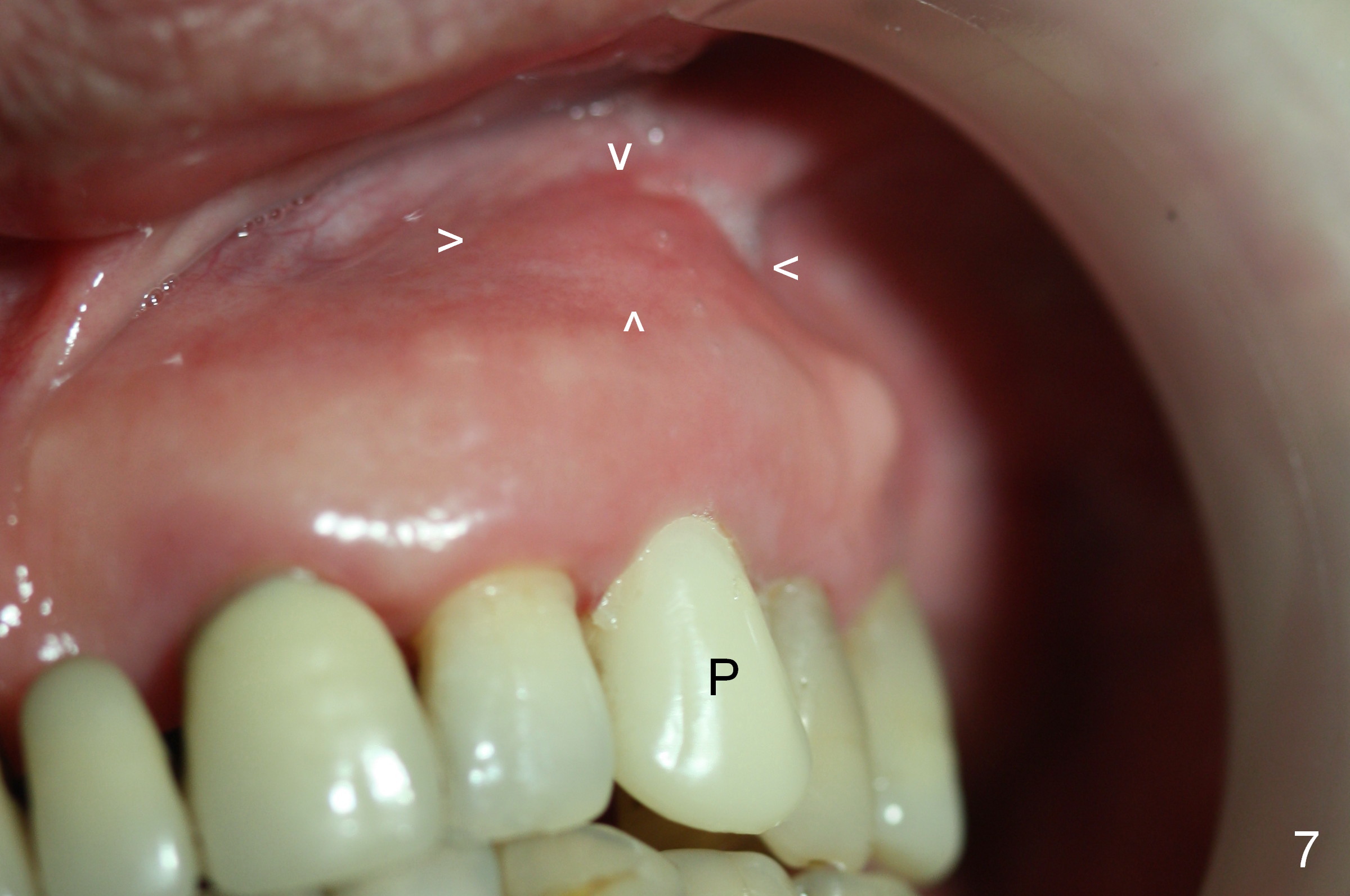
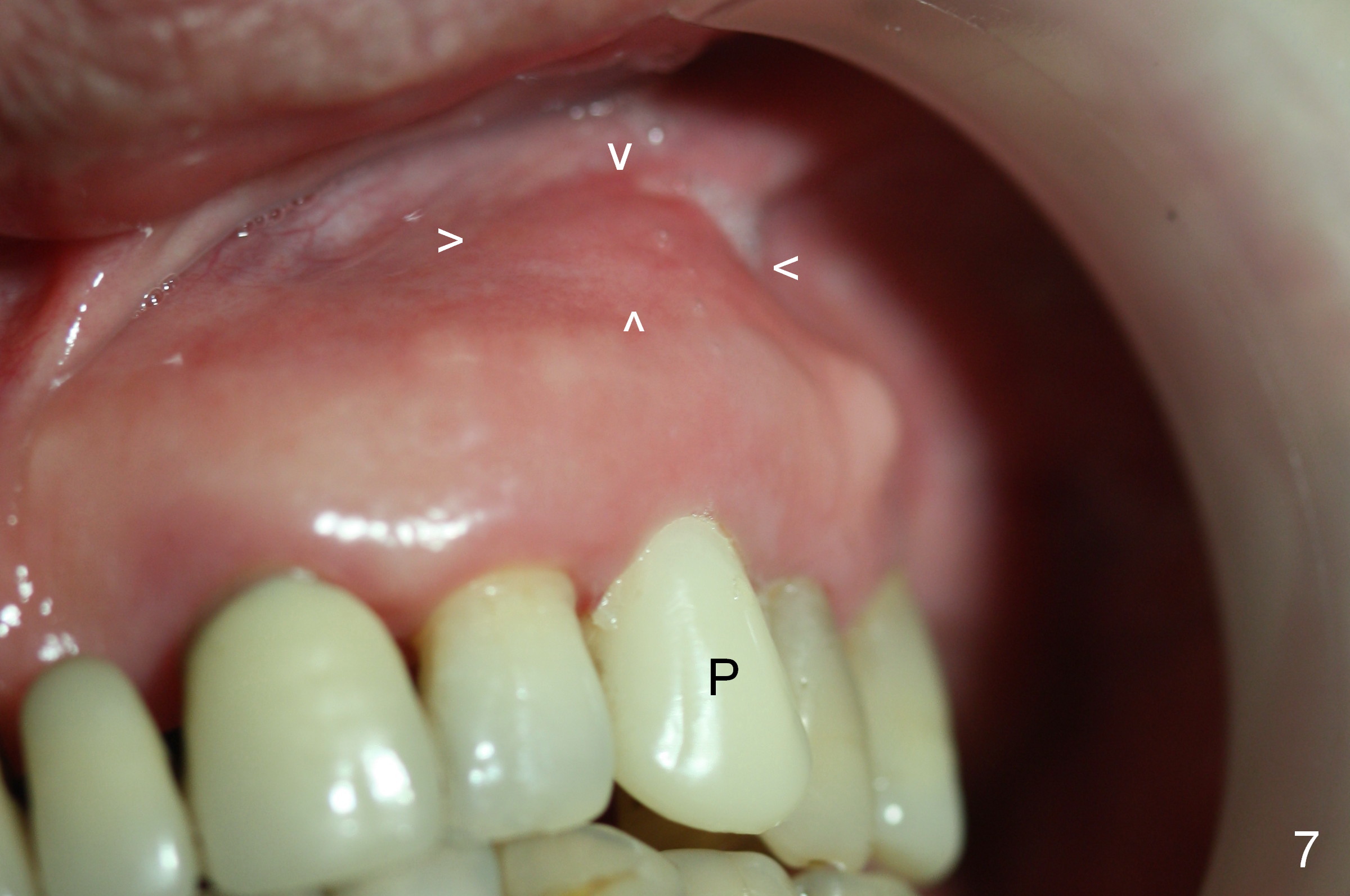
One week later, the gingiva around the provisional (Fig.7 P) looks healthy, while there is an asymptomatic swelling apically (arrowheads), which is not reported again later on.
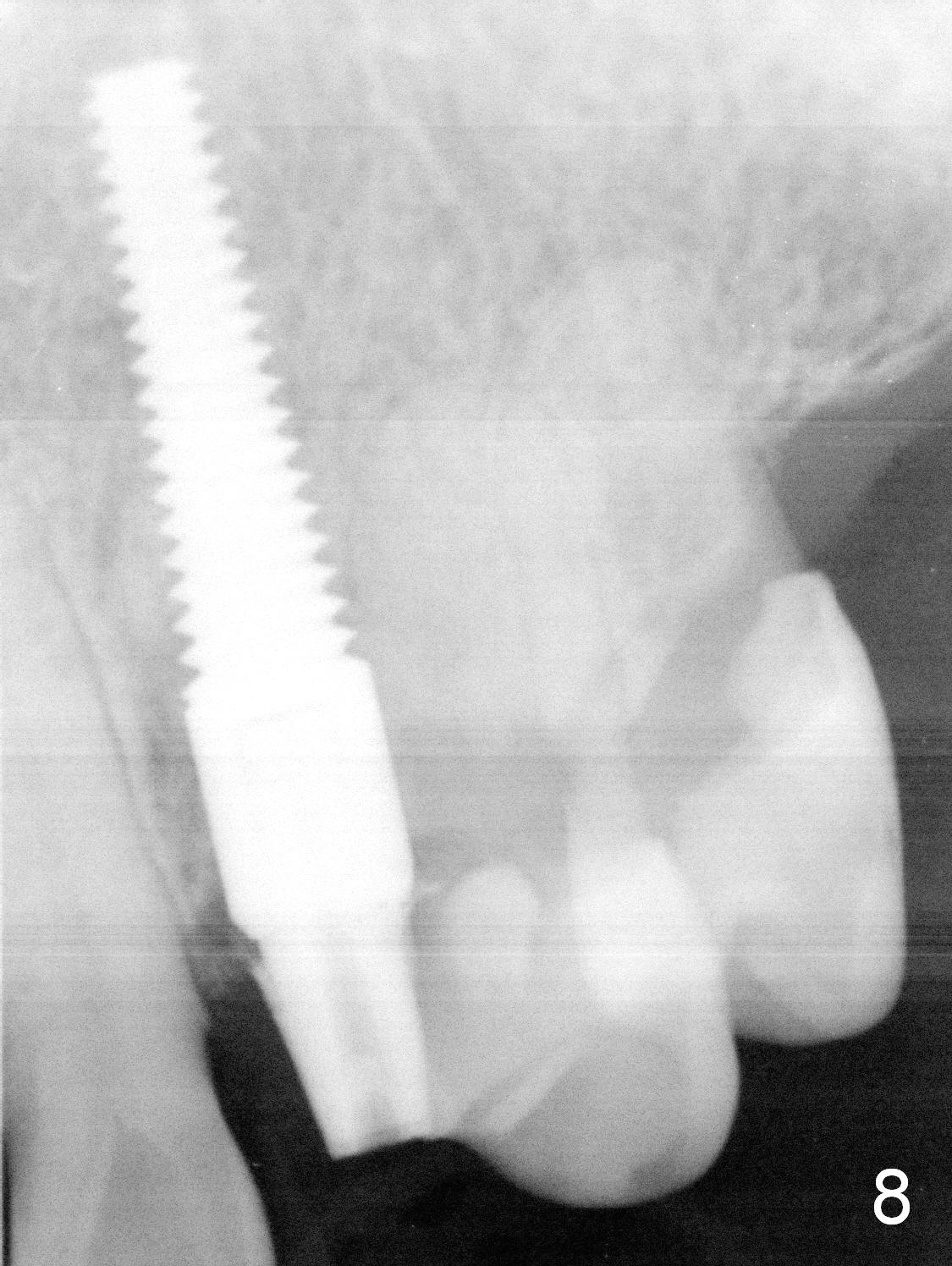
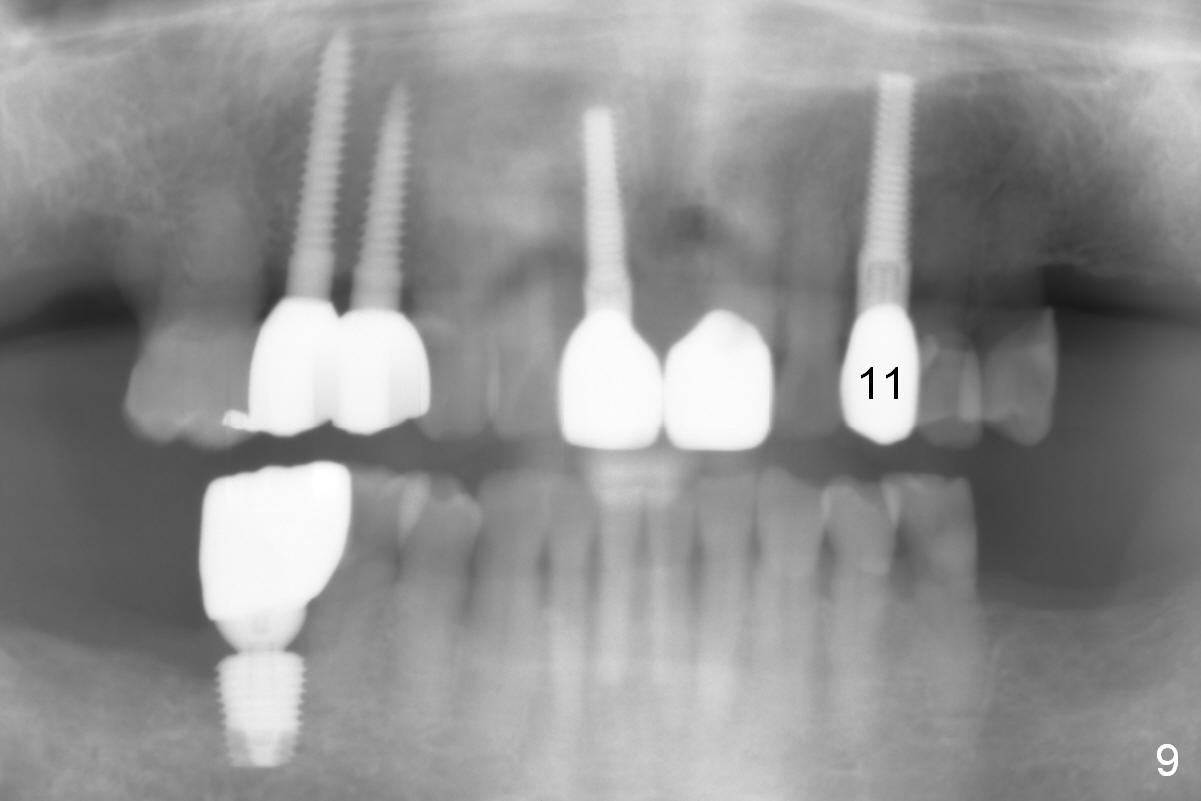
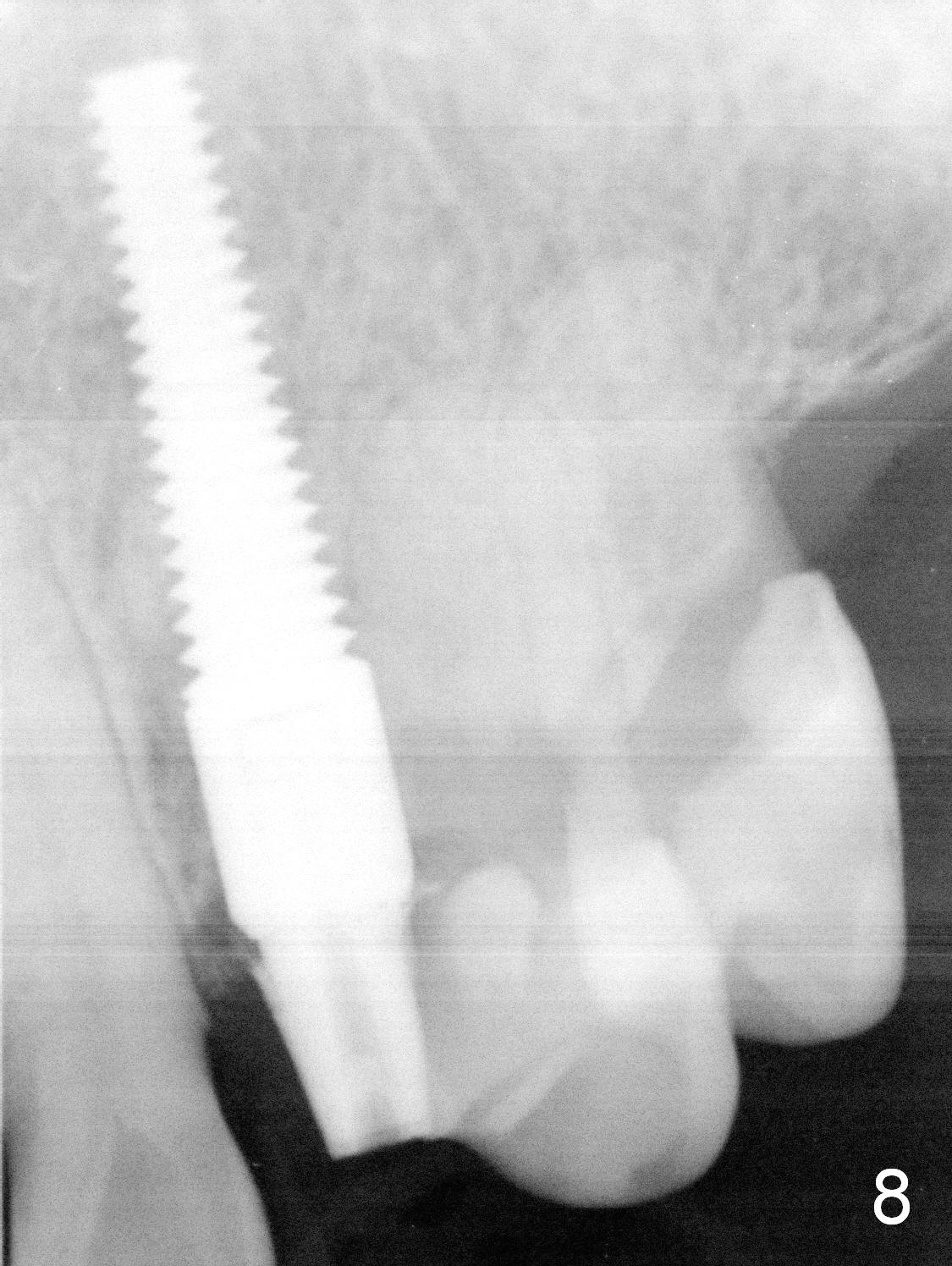
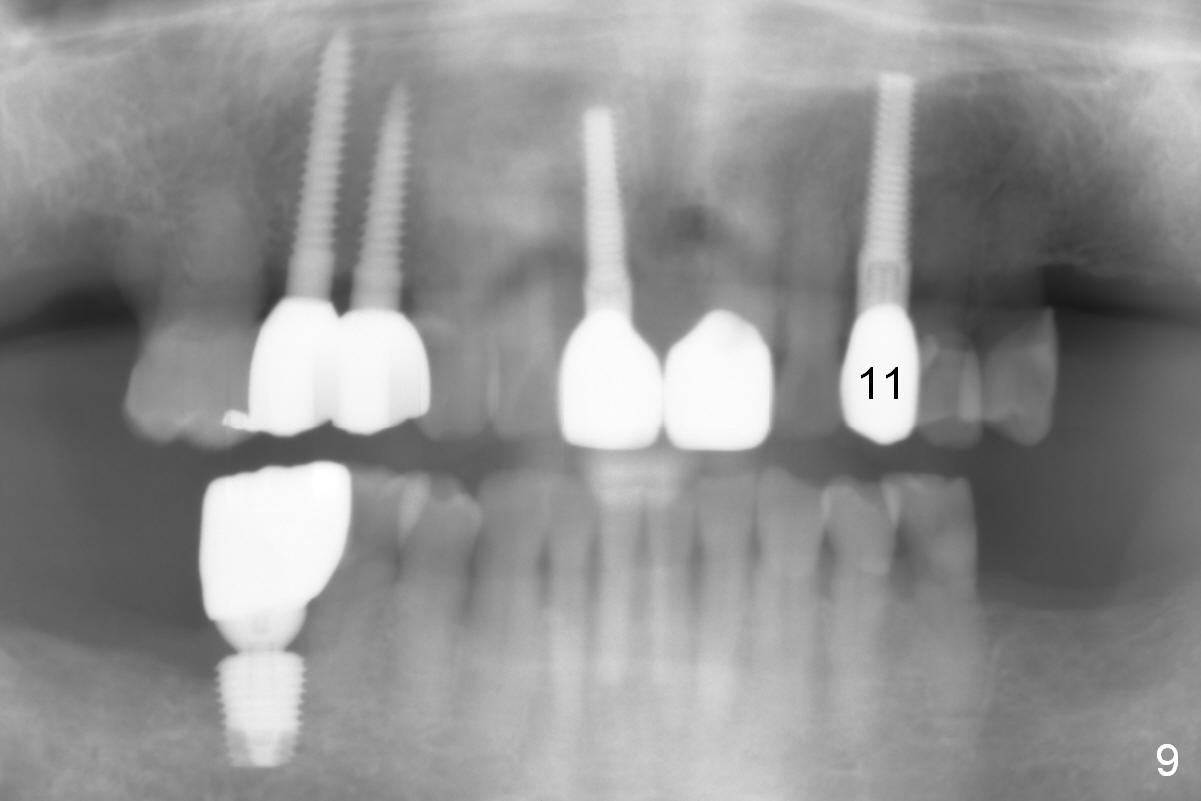
There is no abnormality 3.5 months postop (Fig.8). The patient has started to chew on the left since more implants have been placed on the right (#4,5, 8 and 30). There appears no implant thread exposure 9 months post cementation (Fig.9). Clinically there is no gingival recession.
Return to
Upper
Canine Immediate Implant
Xin Wei, DDS, PhD, MS 1st edition 07/08/2015, last revision 02/03/2019