




 |
 |
 |
||
 |
 |
 |
||
 |
 |
 |
 |
|
 |
 |
 |
 |
|
 |
 |
|||
Provisional Without Prep
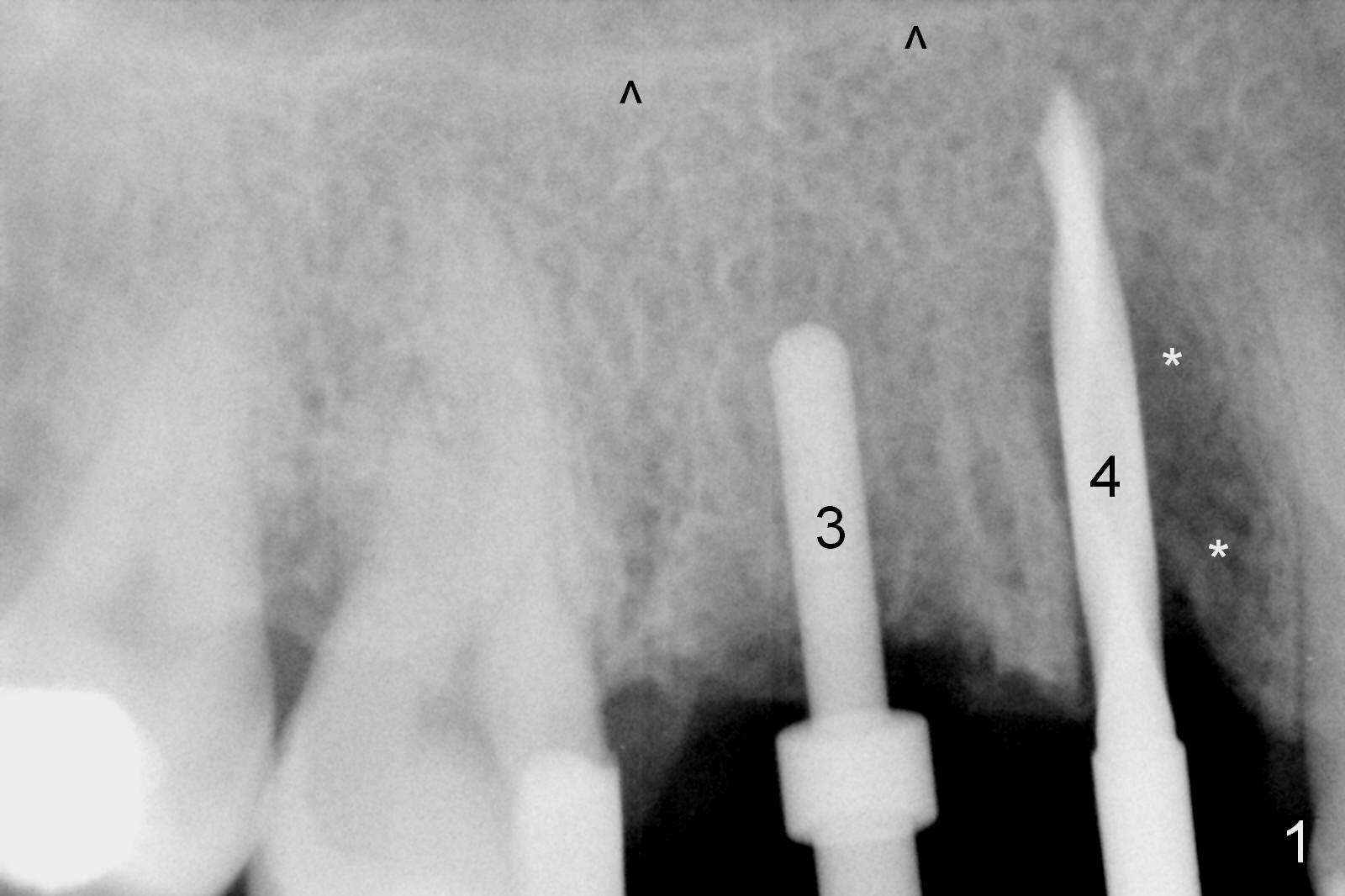
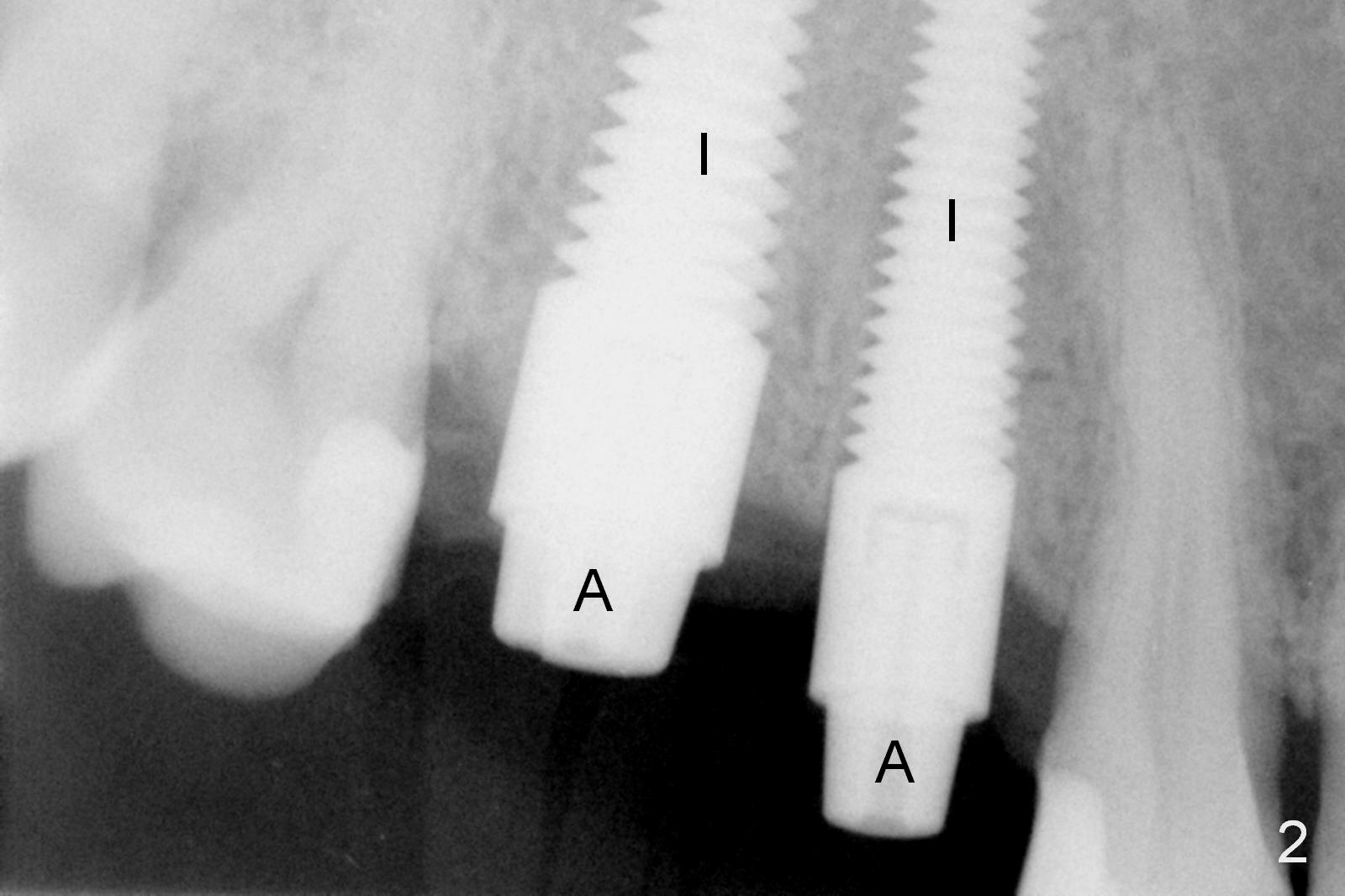
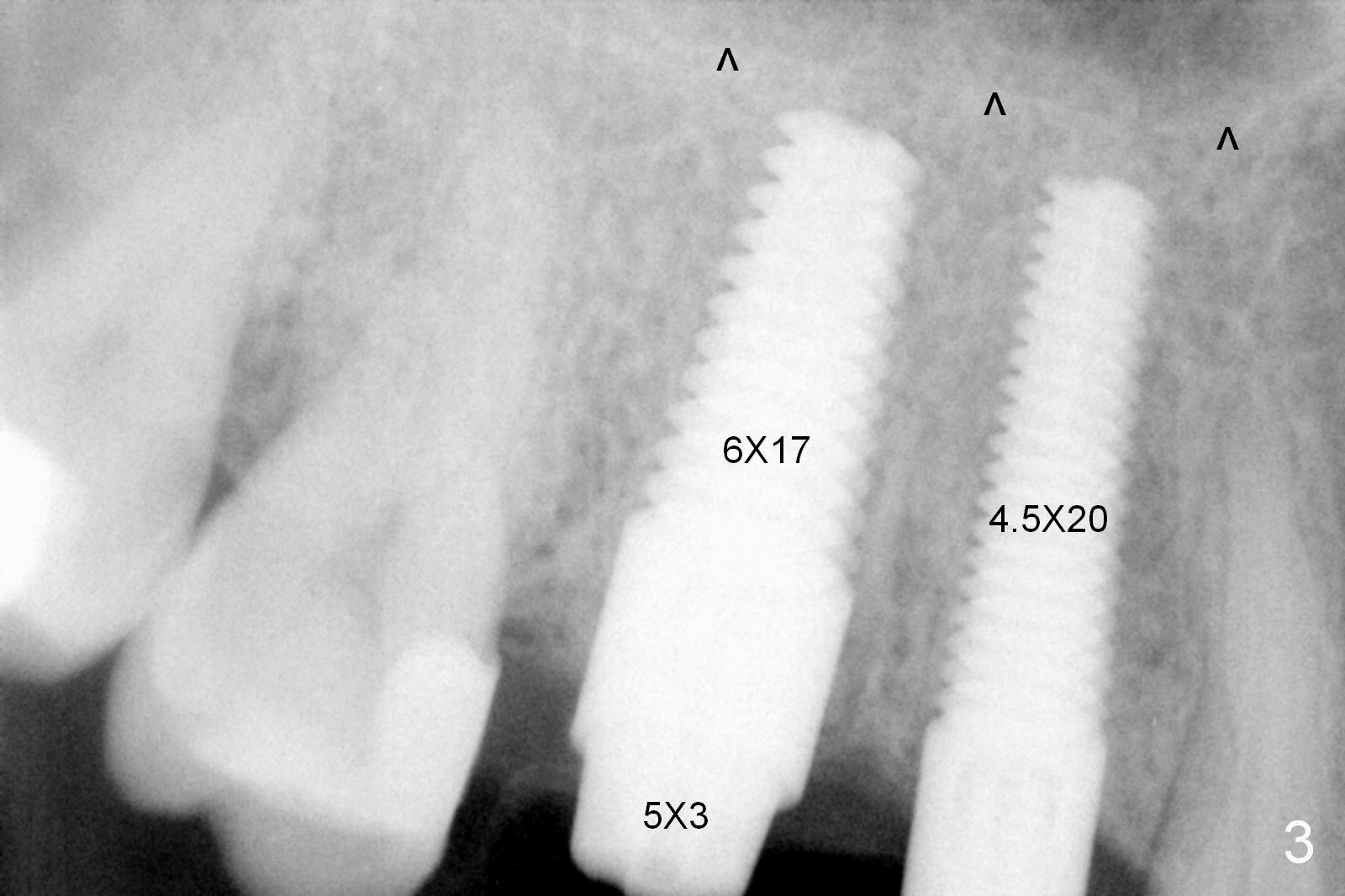
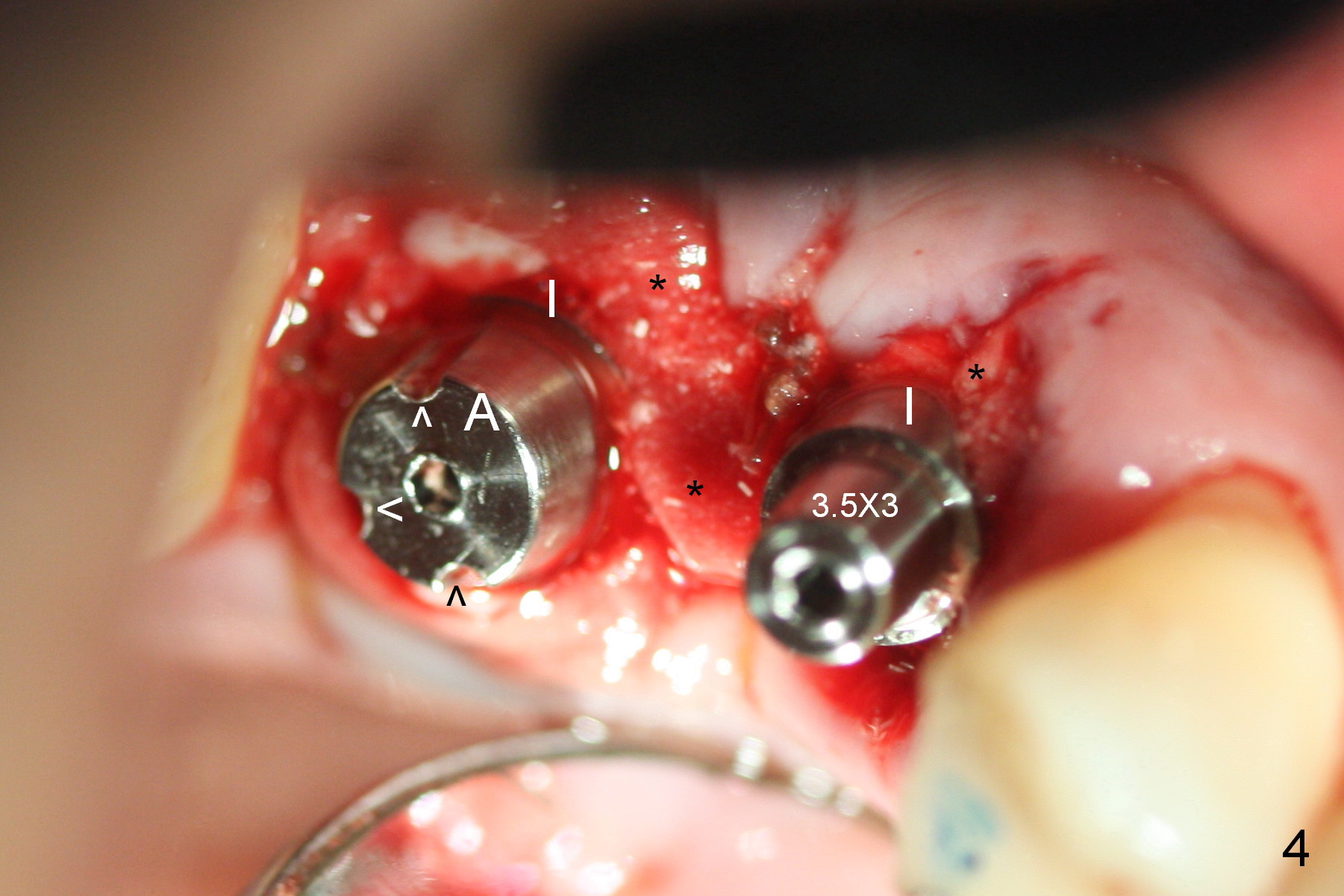
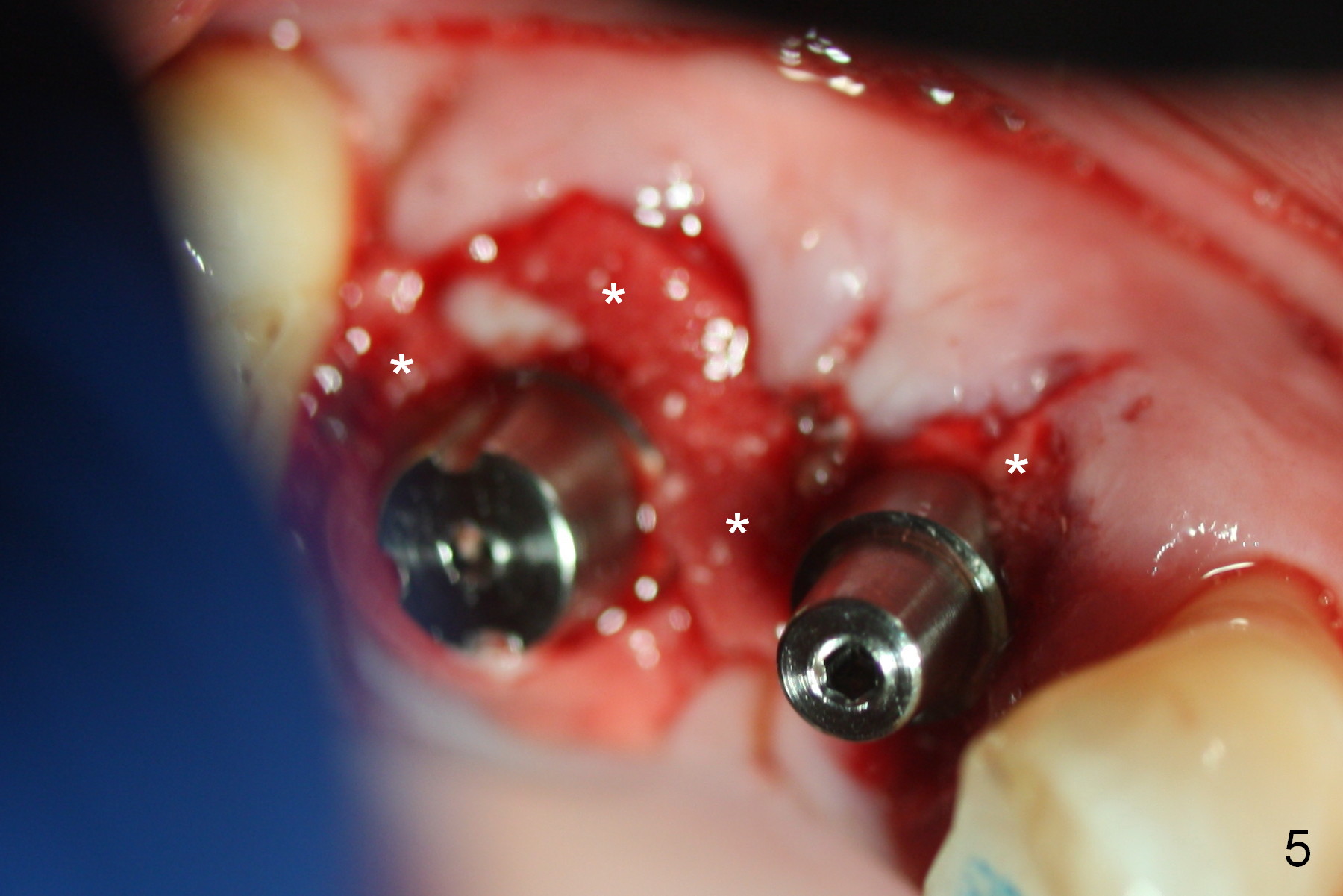
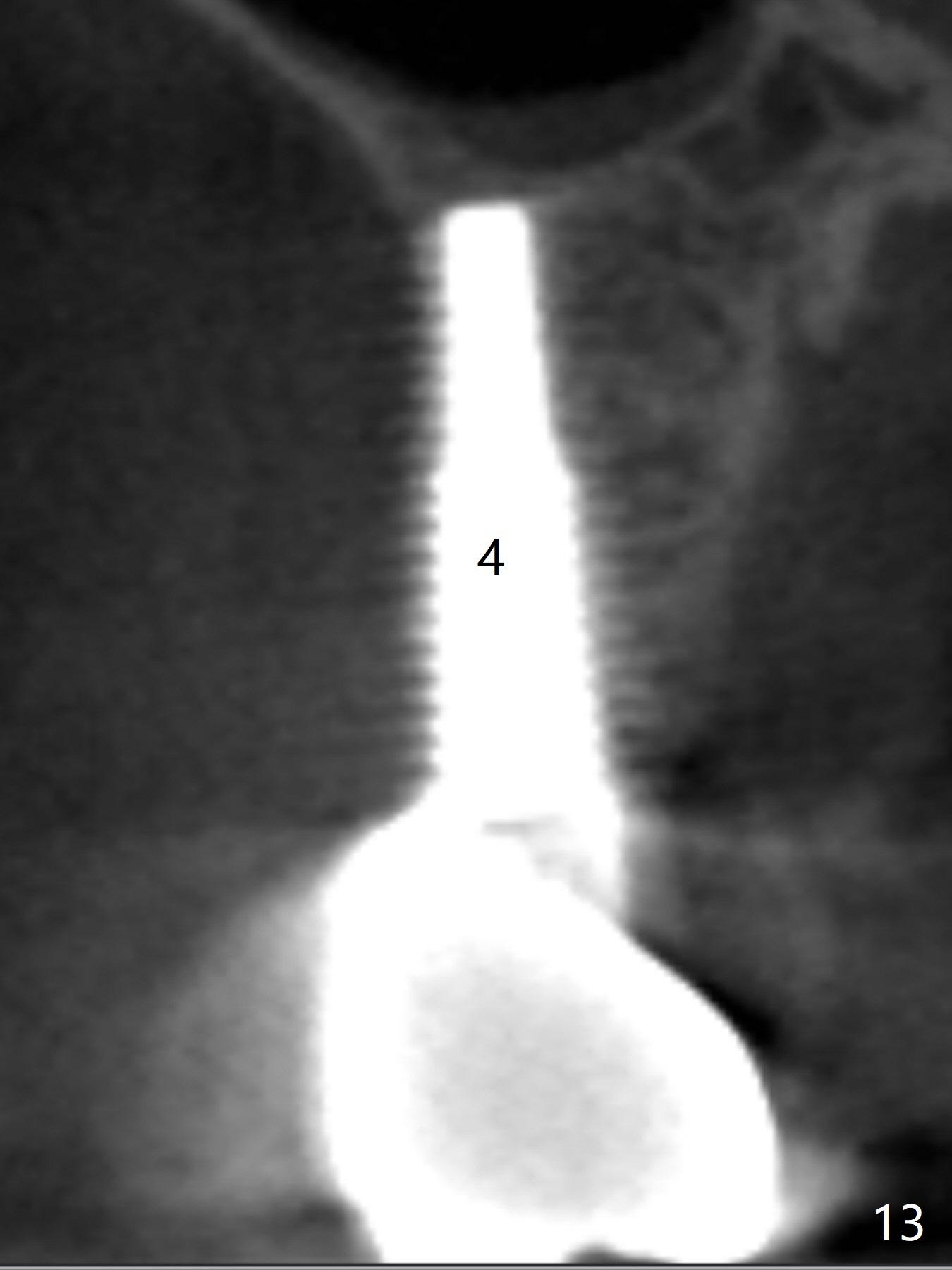
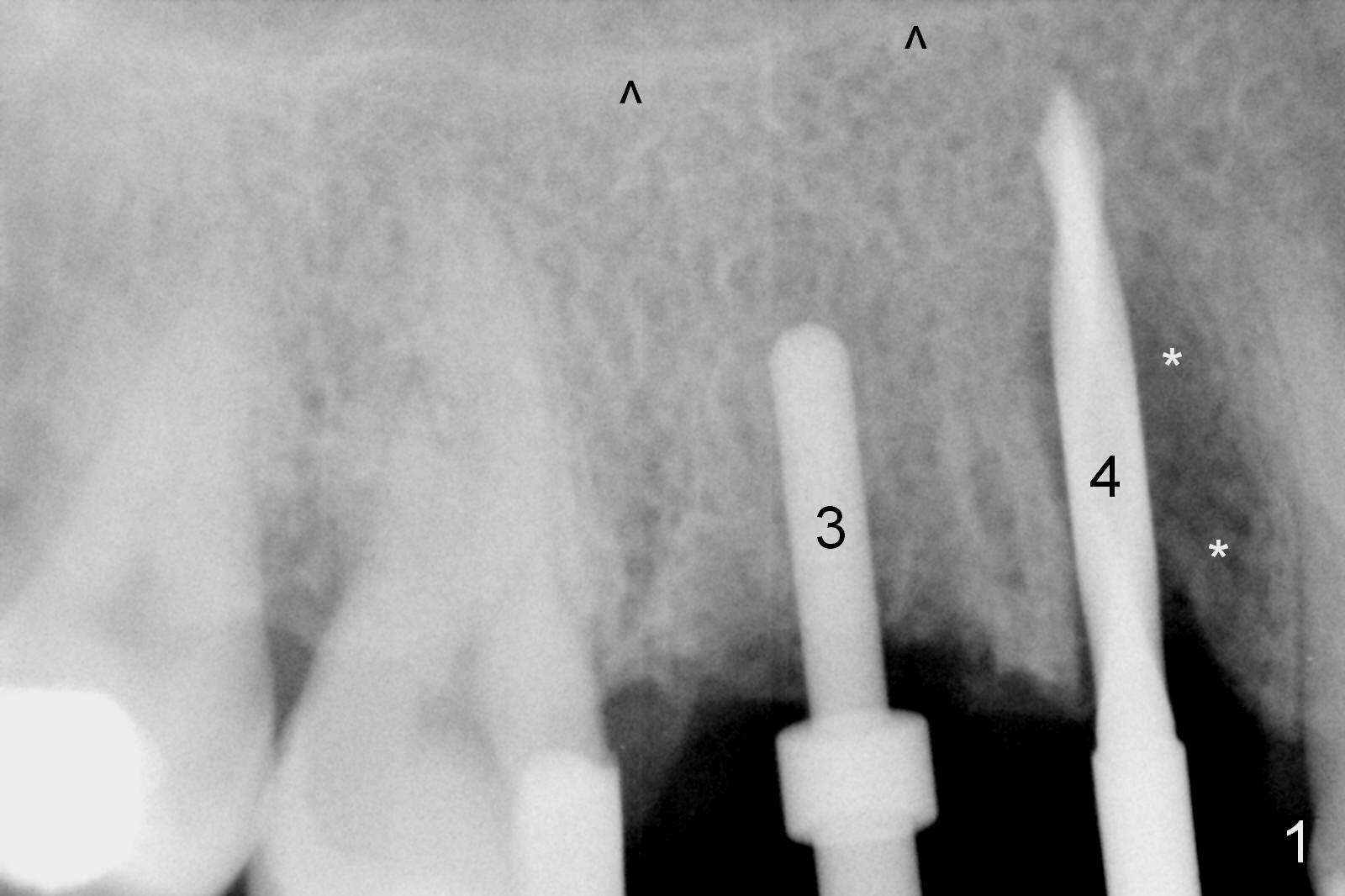
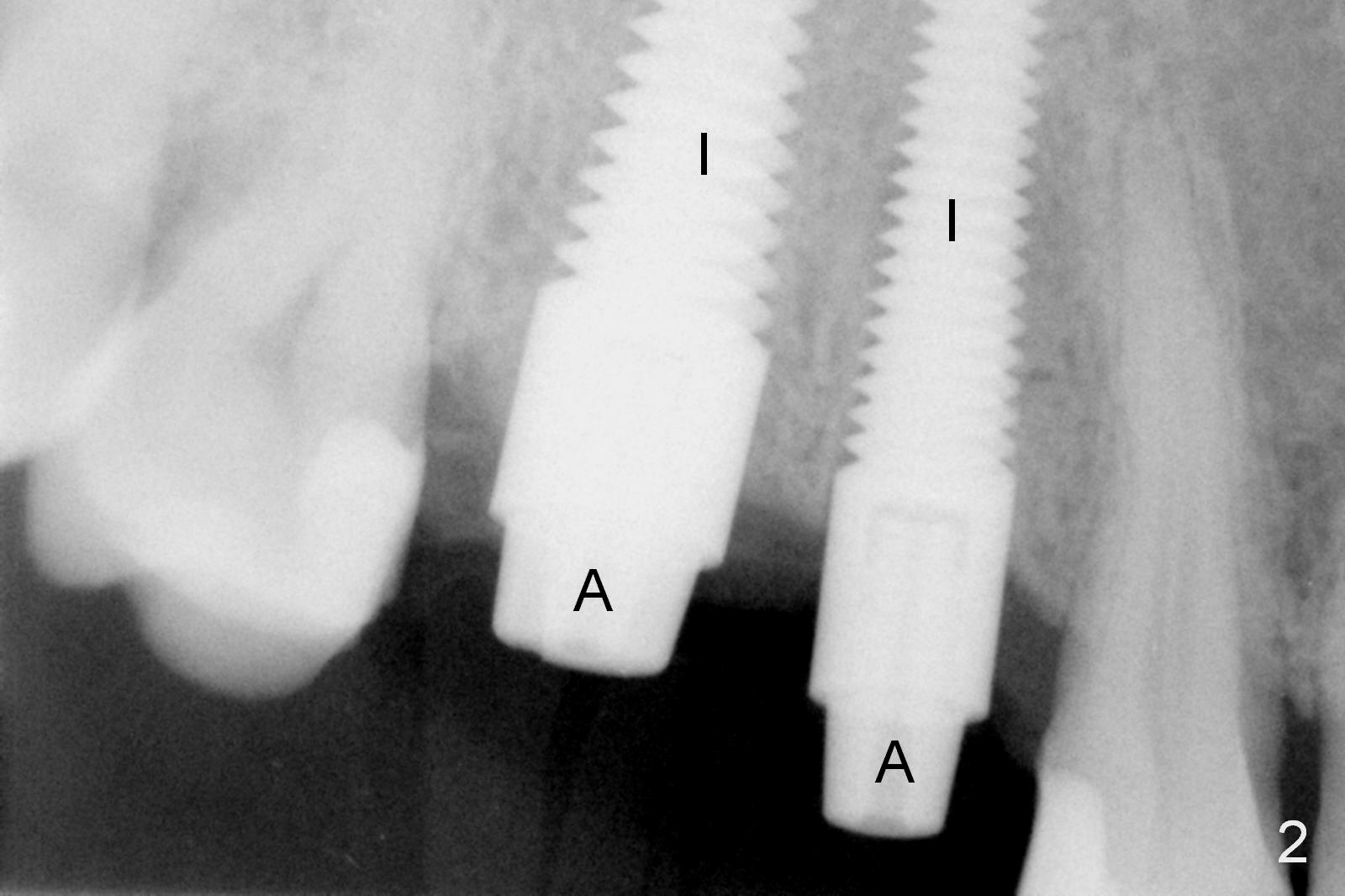
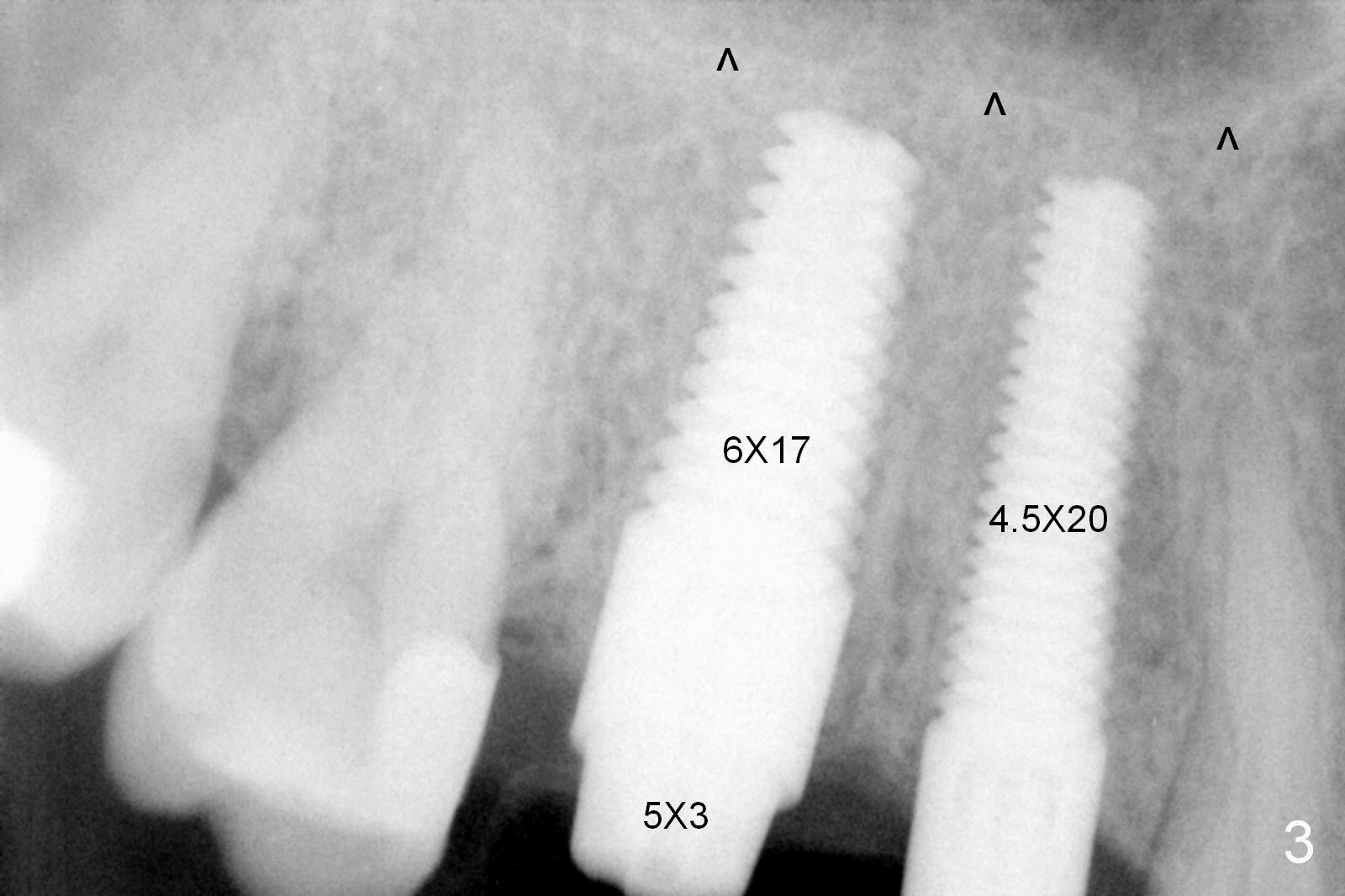
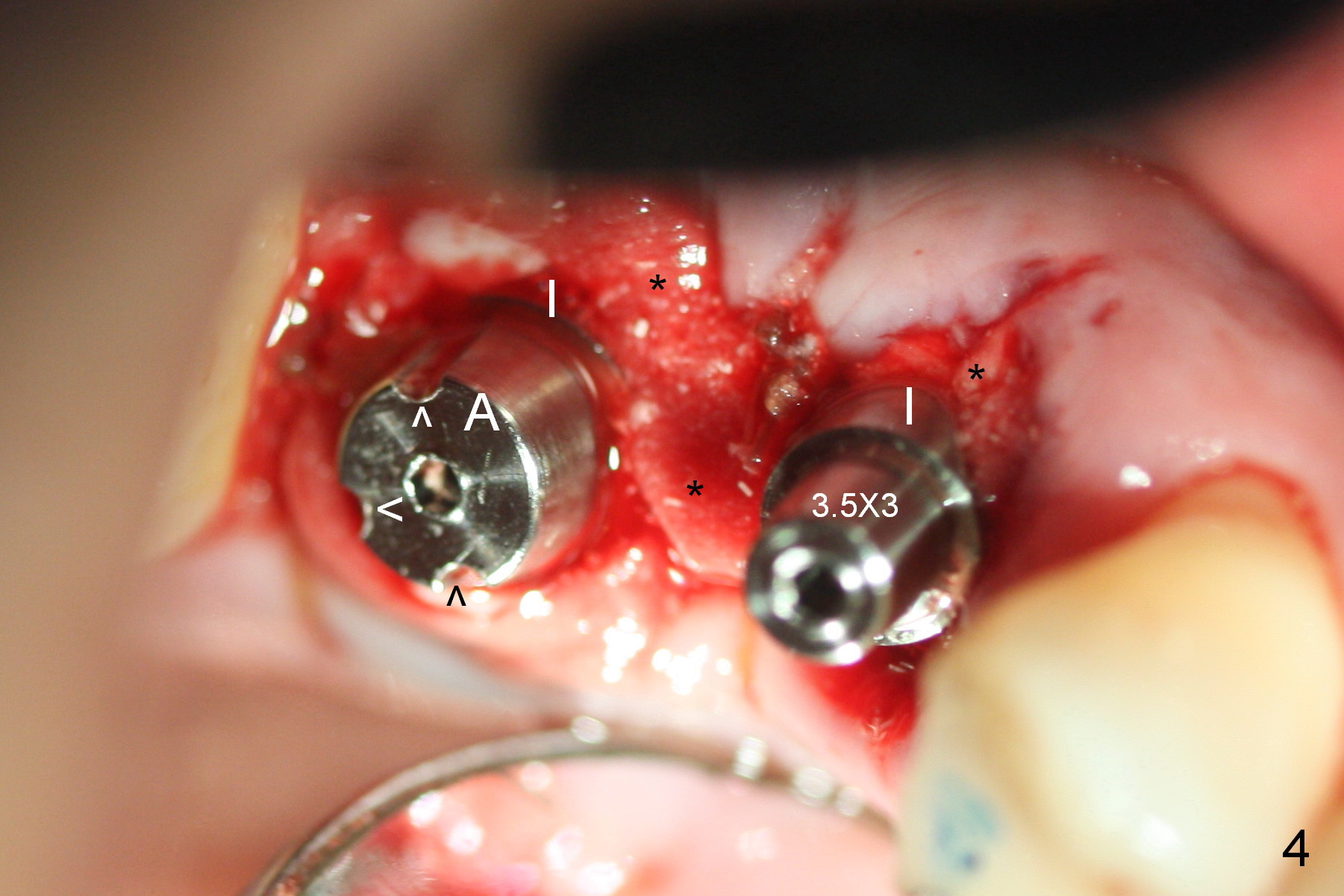
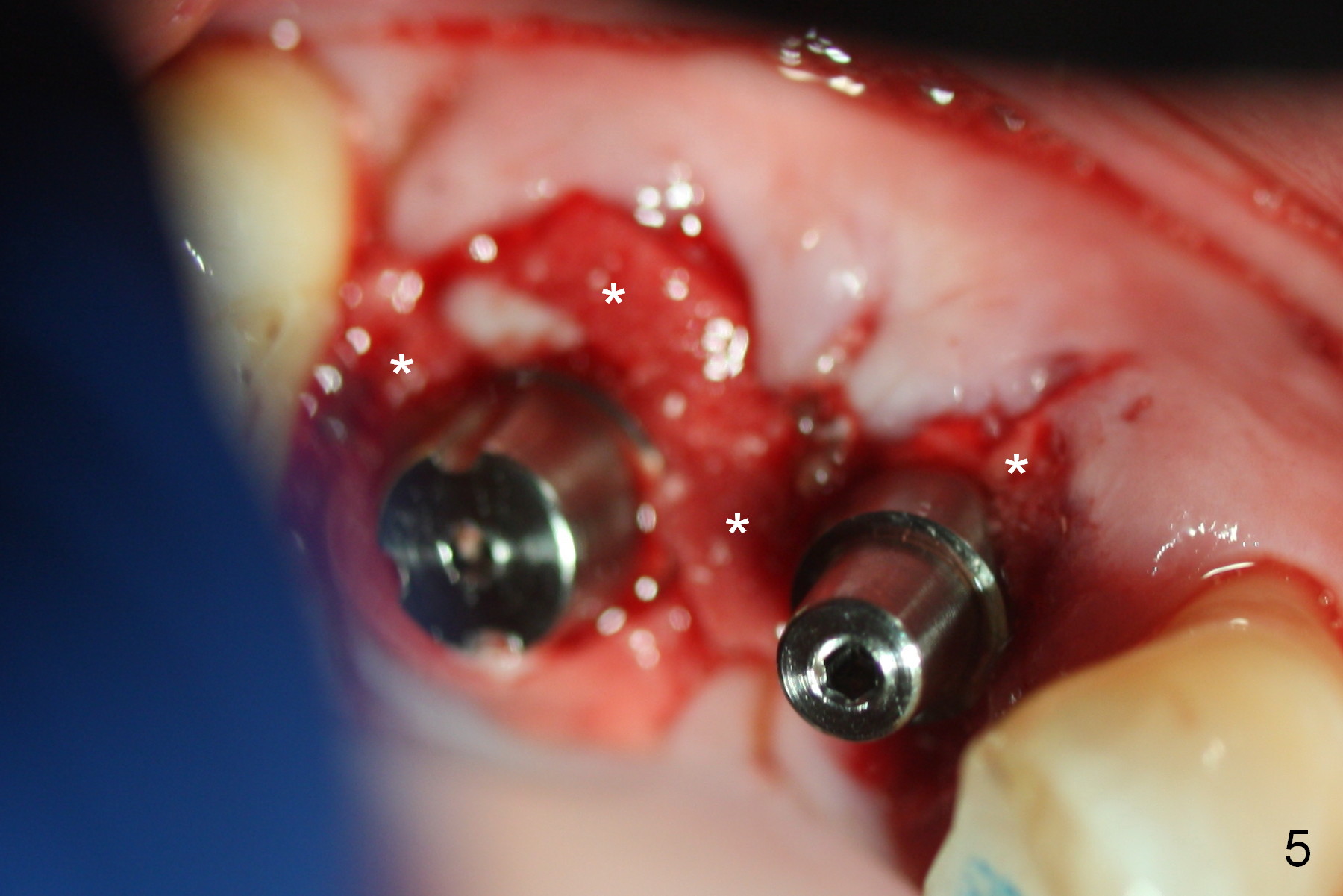
Initial osteotomies at the sites of #3 and 4 are parallel immediately post extraction (Fig.1); the buccal plate of the #4 socket is absent (*). The immediate implants (I: 6x17 and 4.5x20 mm) obtain insertion torque > 60 Ncm (Fig.2,3). Abutments (Fig.2 A) are placed (5x3 and 3.5x3 mm, Fig.3,4). The remaining sockets are filled with Osteoplug, autogenous bone and Osteogen, followed by Collagen Dressing. Since the wound is large (Fig.4,5 *), no prep is done intraorally to avoid contamination of Titanium shaving. The 3 retention grooves on the abutment at #3 are made extraorally (Fig.4 arrowheads). A splinted provisional, fabricated to cover the sockets, is retentive after reline. Periodontal dressing is applied.
Eighteen days postop, the provisional is loose because of the abutment at #3 is loose. After tightening it, the implant/abutment complex are prep with addition of retention grooves. The provisional is relined.
The provisional is dislodged 3 months postop because of mobility and extrusion of the implant at #4 (Fig.6 with increased peri-implant space: *). There is no buccal concavity at #4. After local anesthesia, the implant is retightened until 20 Ncm. The provisional is recemented.
There is tendency of loosening of immediate implant at the premolar. One of reasons is that the socket is oval while the implant is rounded. To compensate the shape discrepancy, a D-implant should be used more often. A longer or large implant is used especially in the presence of infection or loss of the buccal plate (Fig.1 *).
When the patient returns 3 months post #4 implant retightening, the implant is stable with apparent osteointegration mesially radiographically (Fig.7). The most coronal distal threads appear not covered by bone (Fig.7 *). There is buccal plate collapse and gingival recession (Fig.8 *), probably related to buccal placement (buccal plate loss). Arrowheads in Fig.'8 indicate the future buccal margin of the crown at #4.
In brief, when the buccal plate is lost, place an implant as palatal and apical as possible to reduce chance of thread exposure.
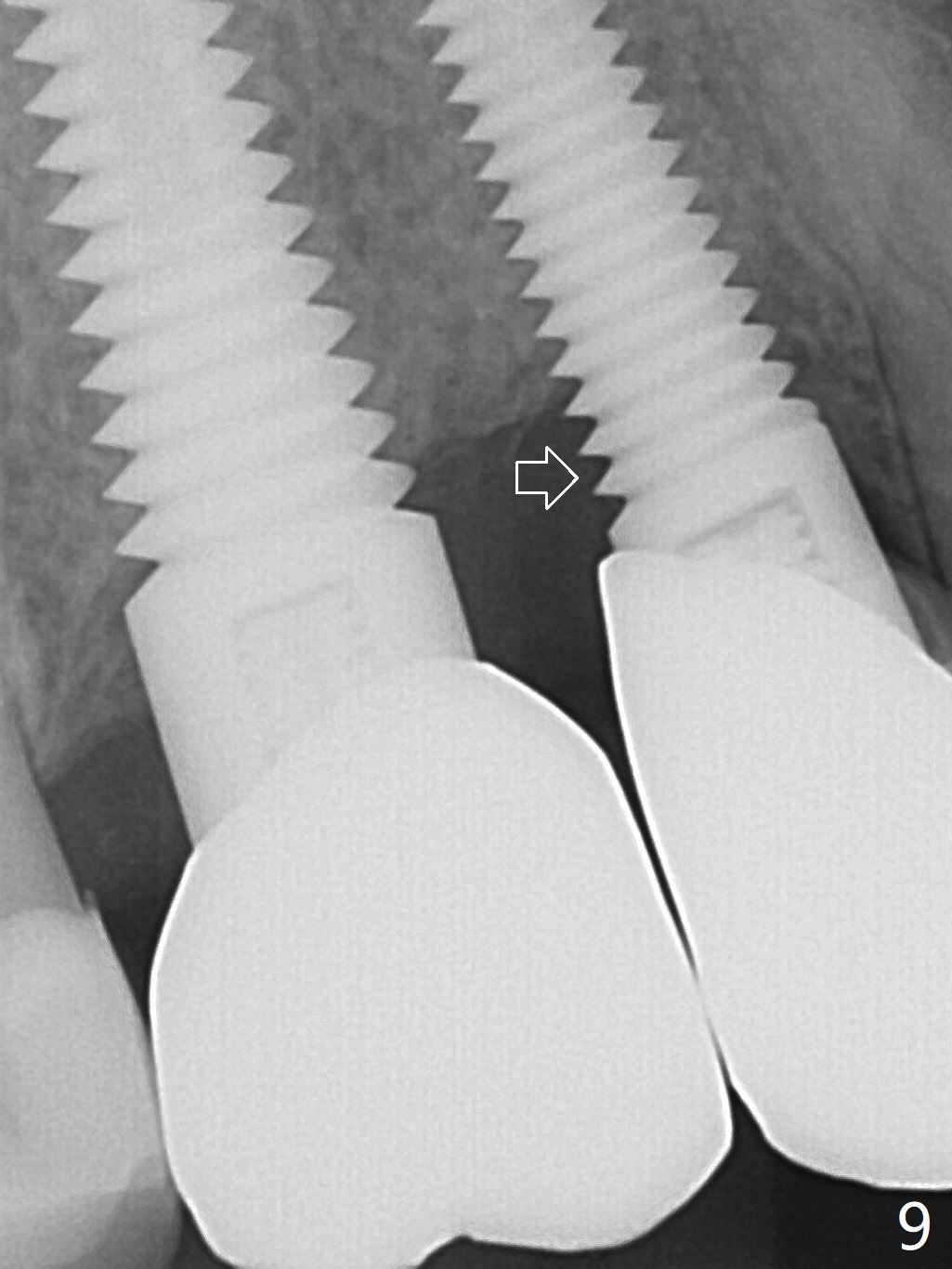
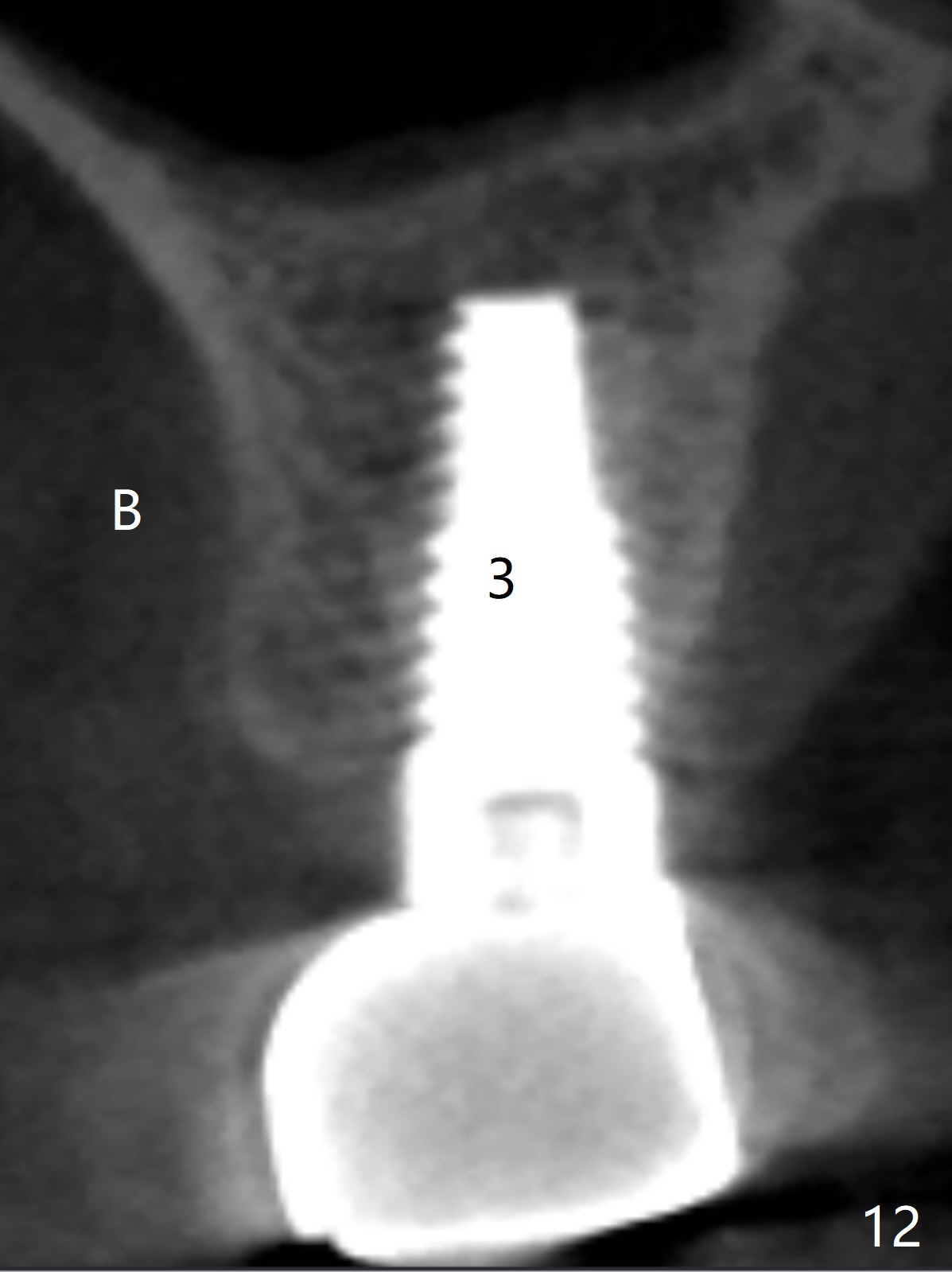
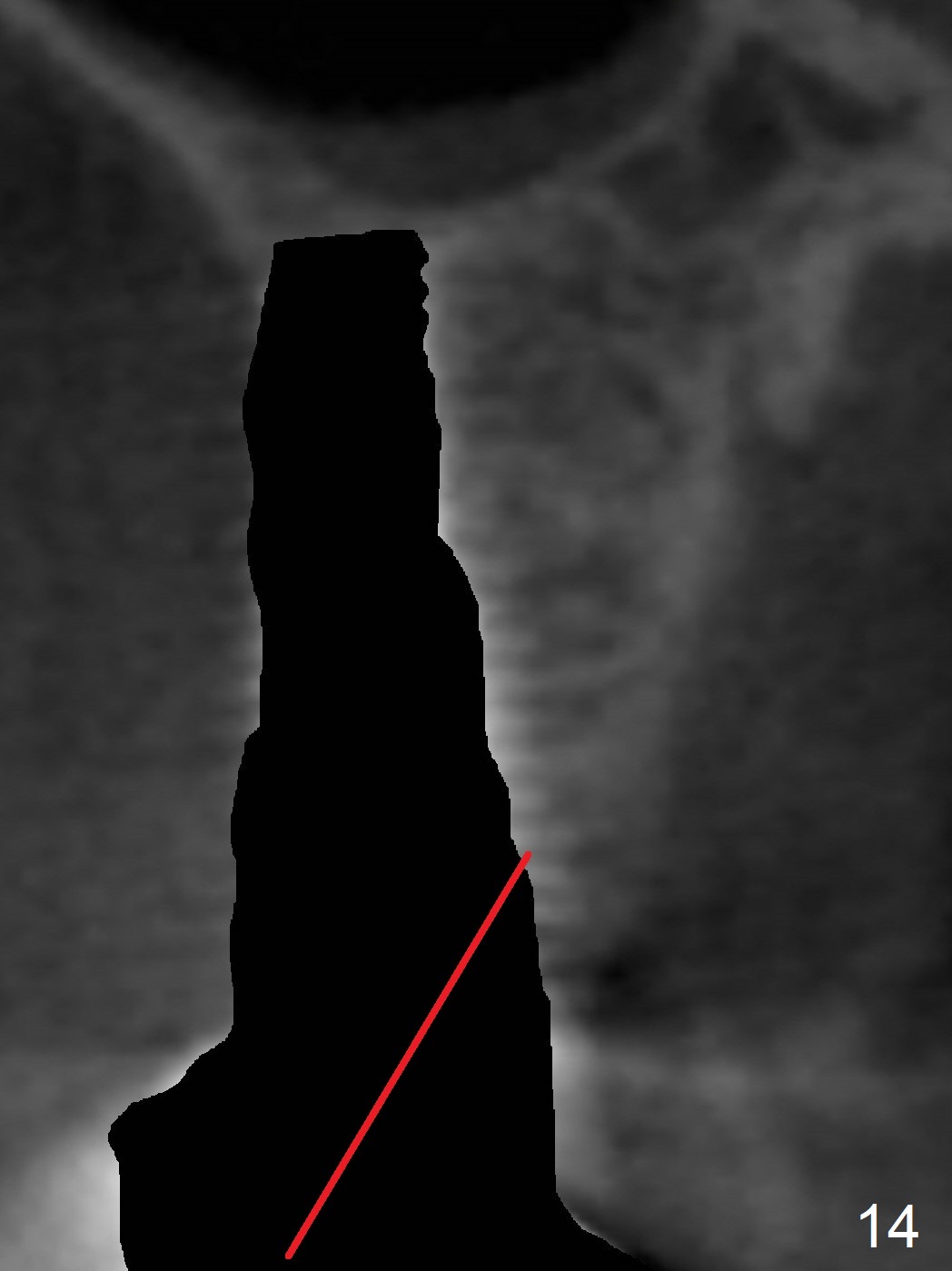
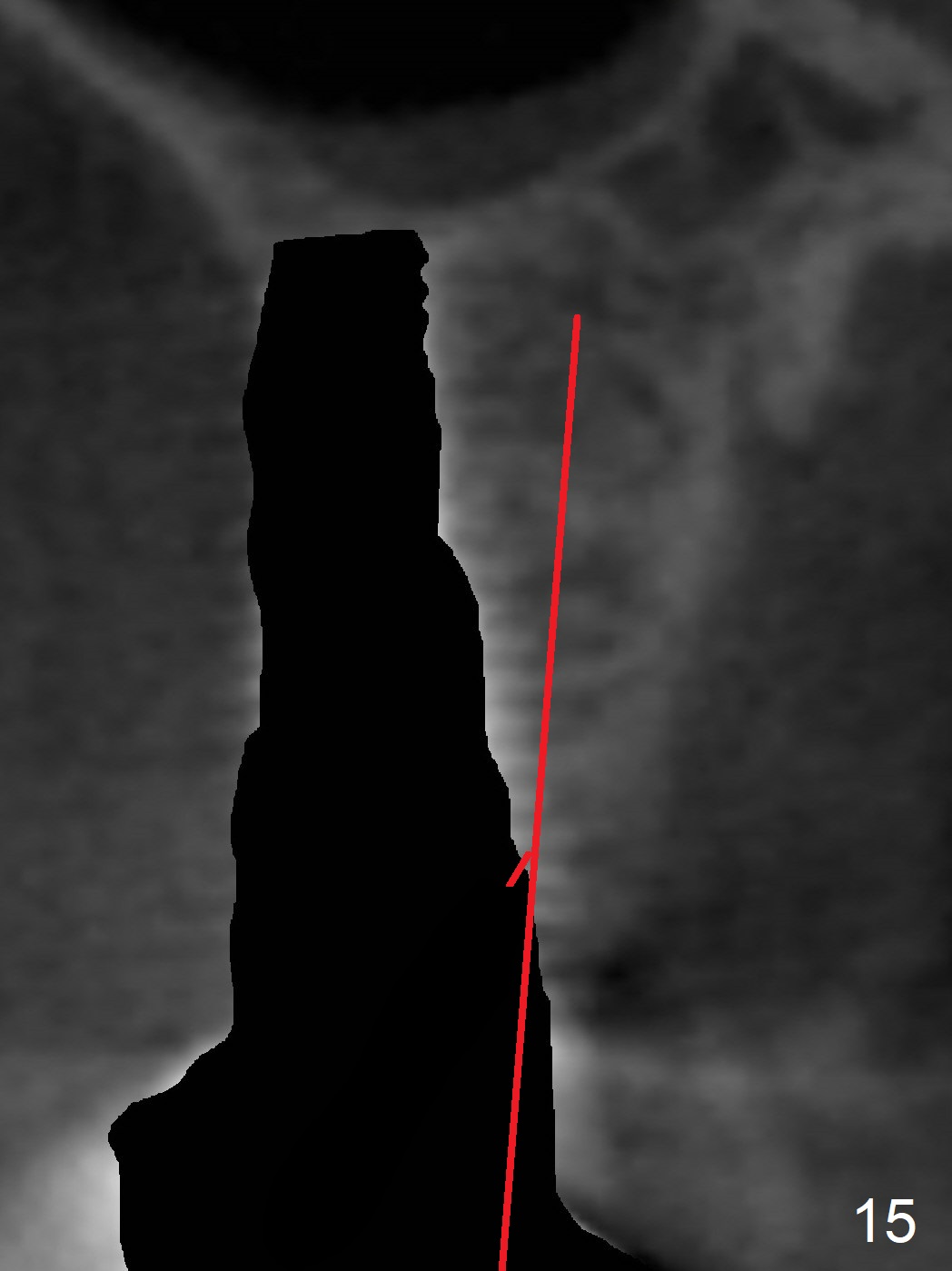
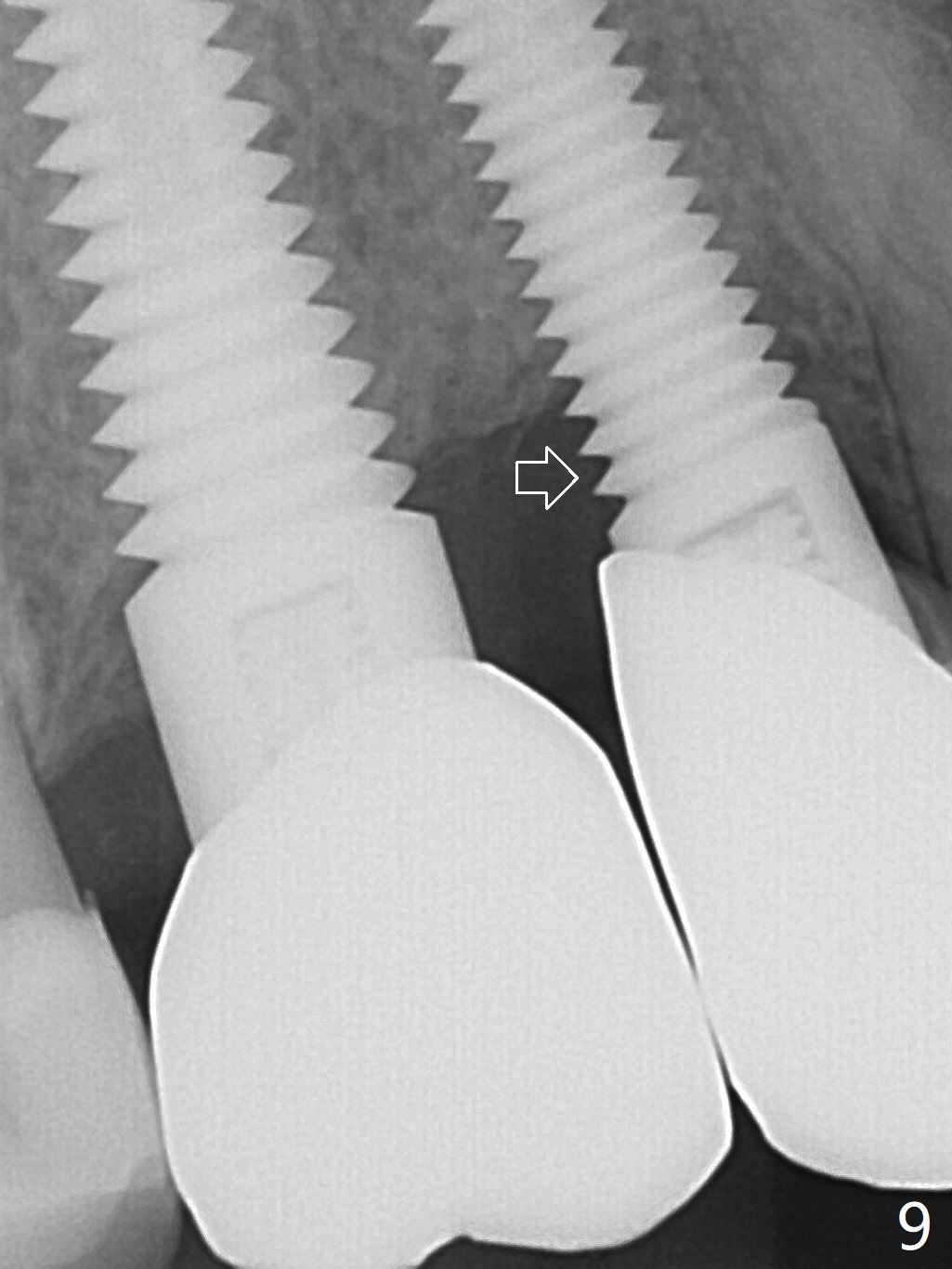
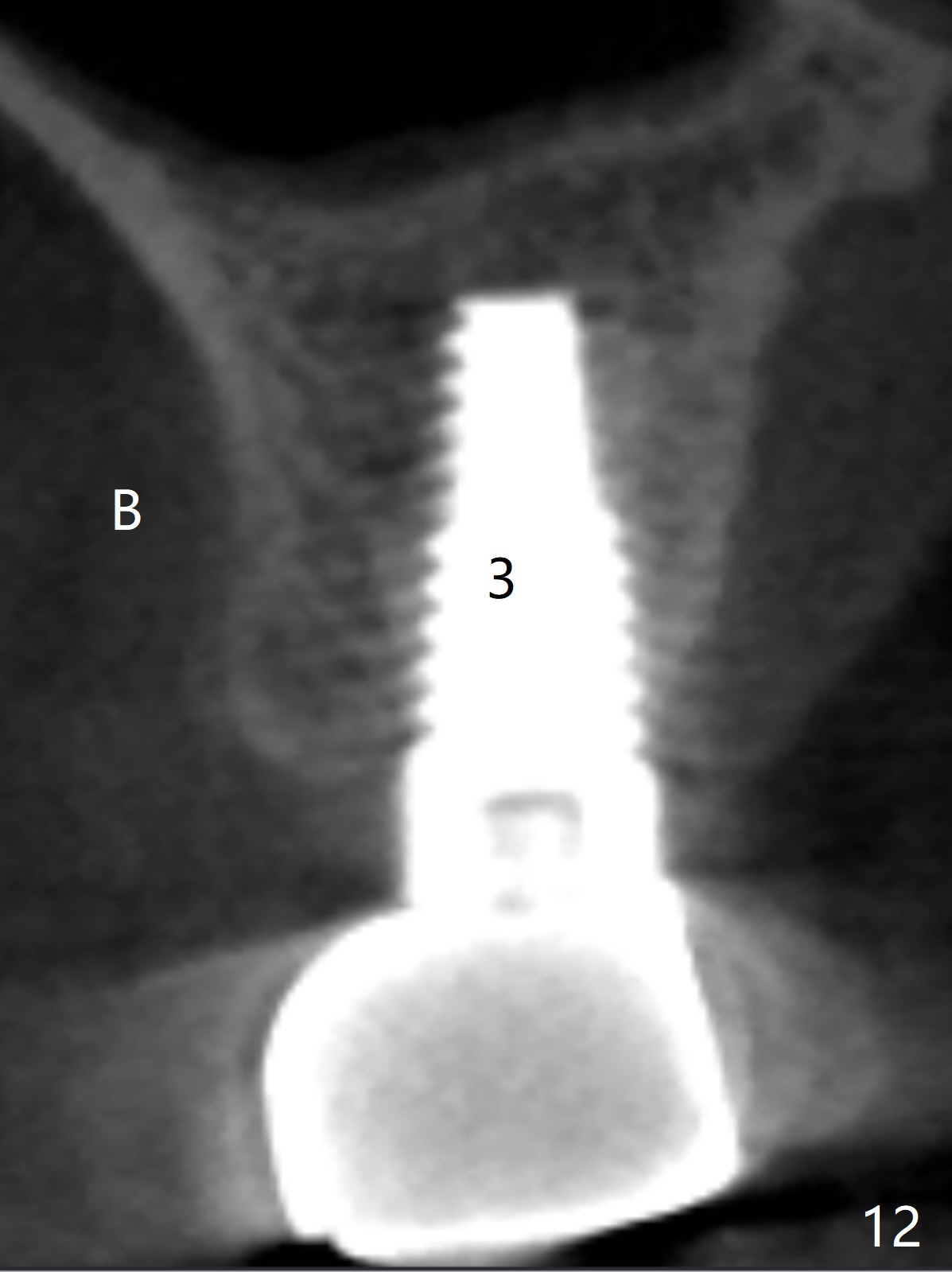
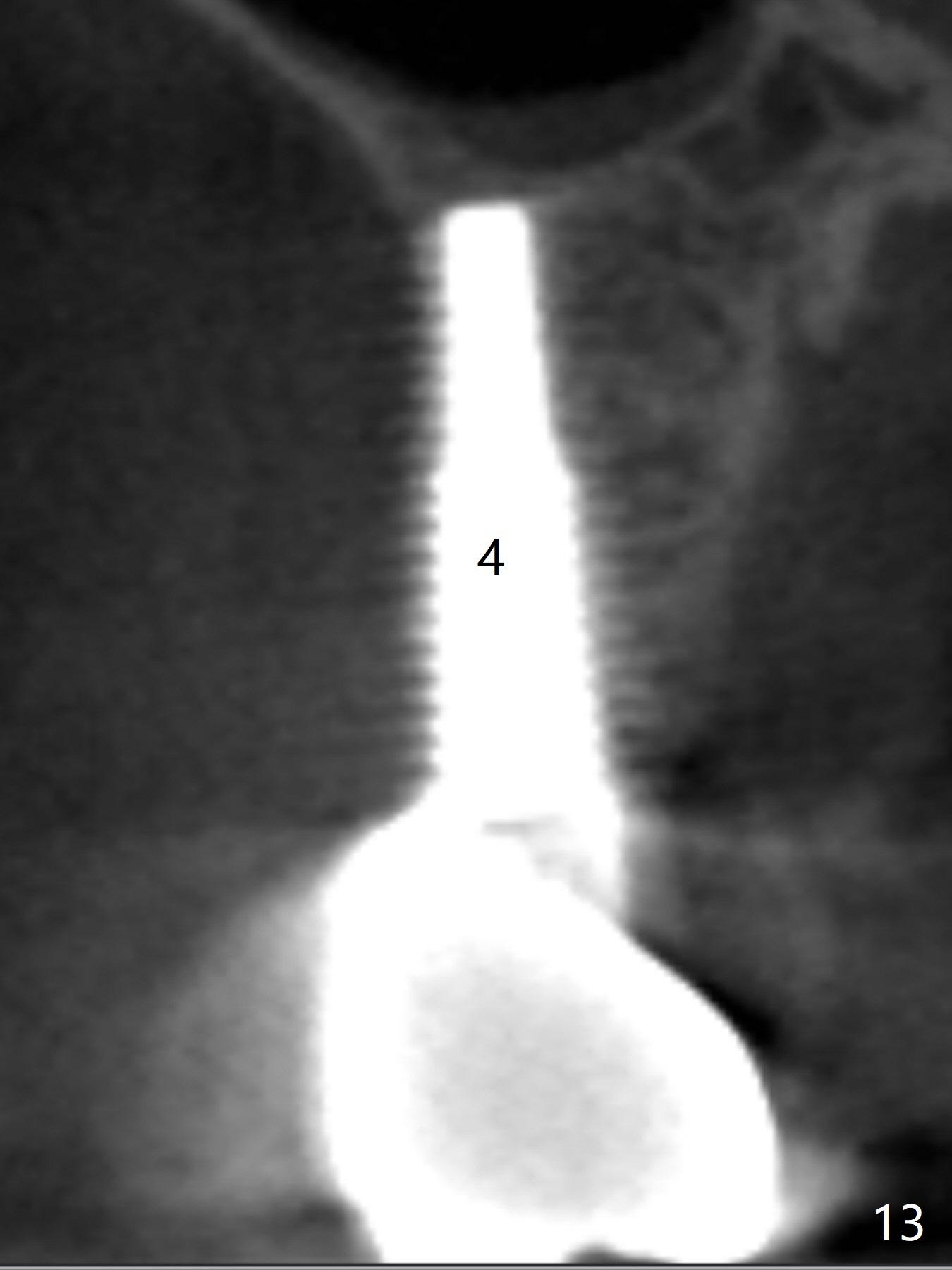
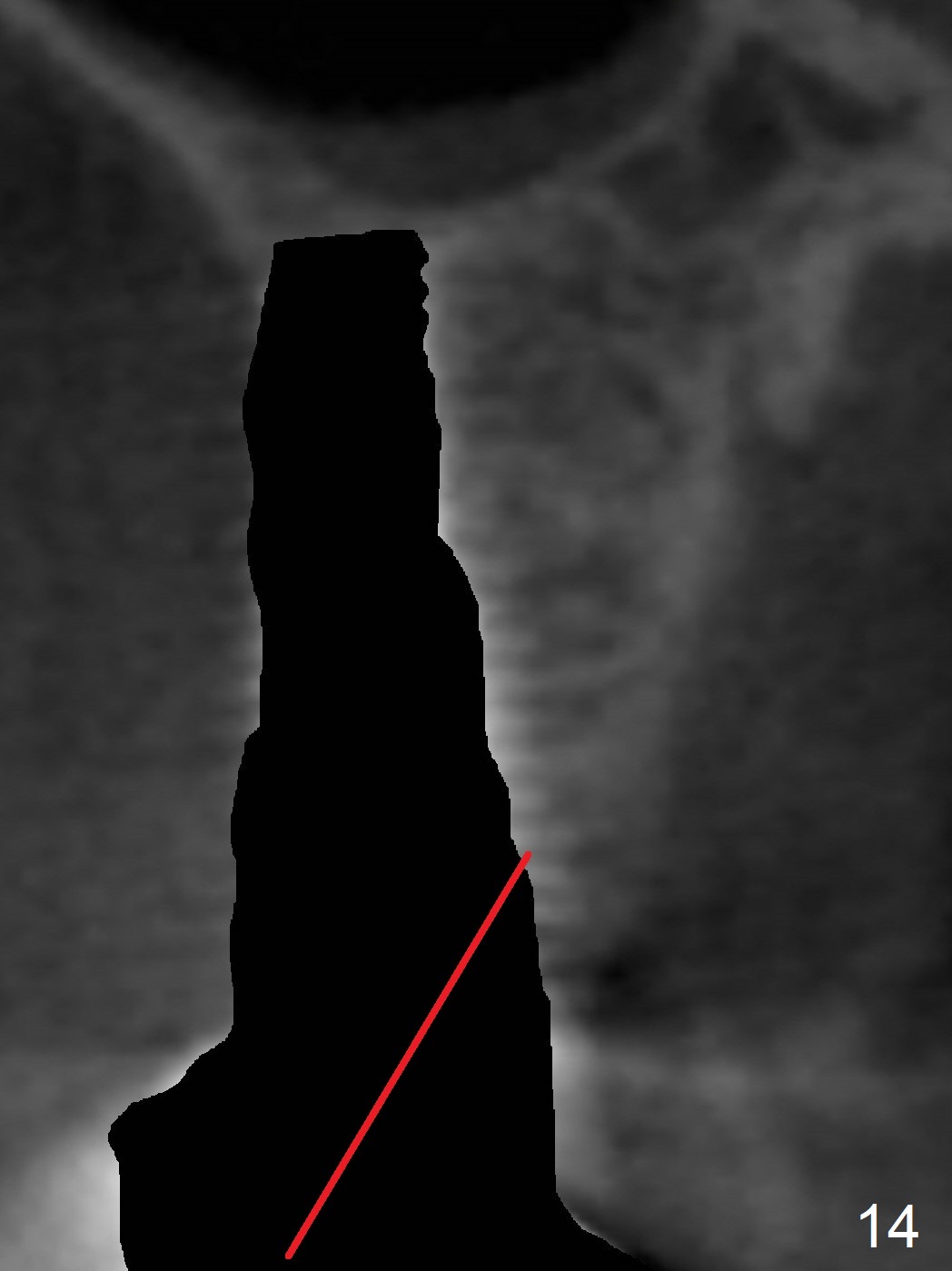
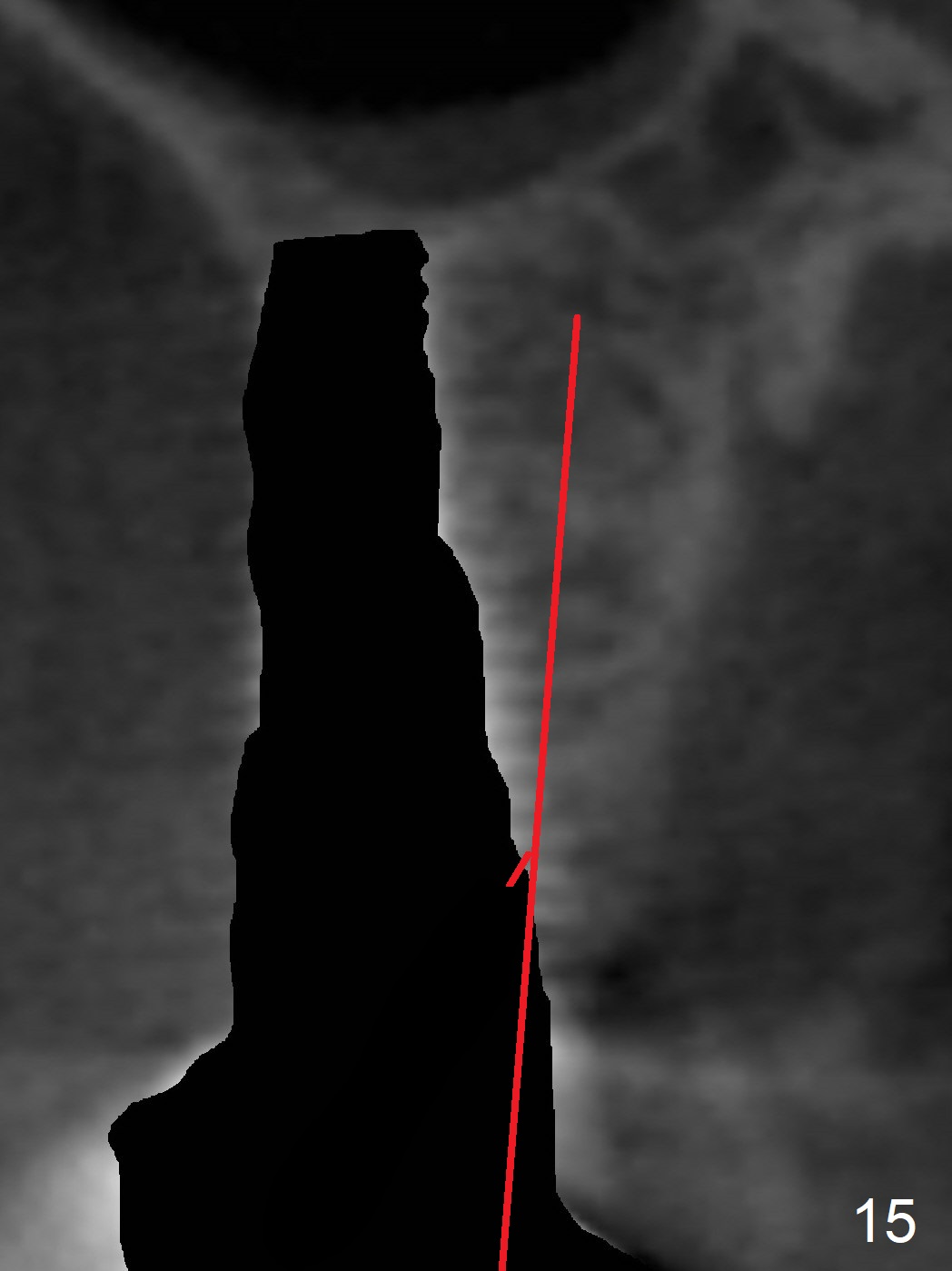
Implant thread exposure (Fig.9 arrow) and gingival recession (Fig.10 arrow) become worse 17 months post cementation. CBCT confirms thread exposure at #4 (Fig.11-13). After use of water pik, there is no symptom of periimplantits at #4. If the latter recurs, it will be removed (Fig.14 black area). Osteotomy will be initiated as palatal as possible obliquely (Fig.14 red line). Once penetrated, the initial drill will change the trajectory (Fig.15).
Return to Upper Premolar,
Molar Immediate Implant,
Posterior Immediate Provisional,
Immediate Implant
Complications,
Technicians
Xin Wei, DDS, PhD, MS 1st edition 09/18/2015, last revision 05/20/2018