





.jpg)

 |
 |
 |
 |
||
 |
 |
 |
 |
 |
|
 |
 |
 |
|||
 |
 |
 |
|||
 |
 |
.jpg) |
|||
 |
|||||
Extra Wide Implant
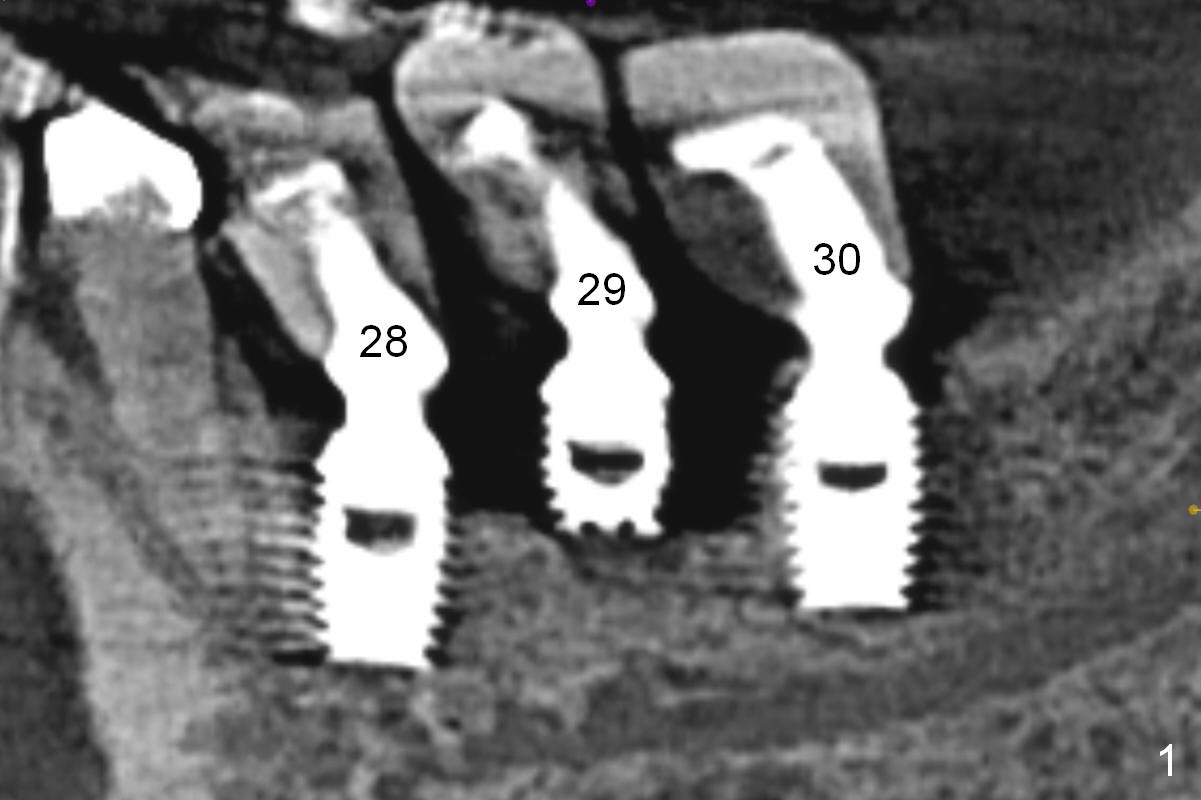
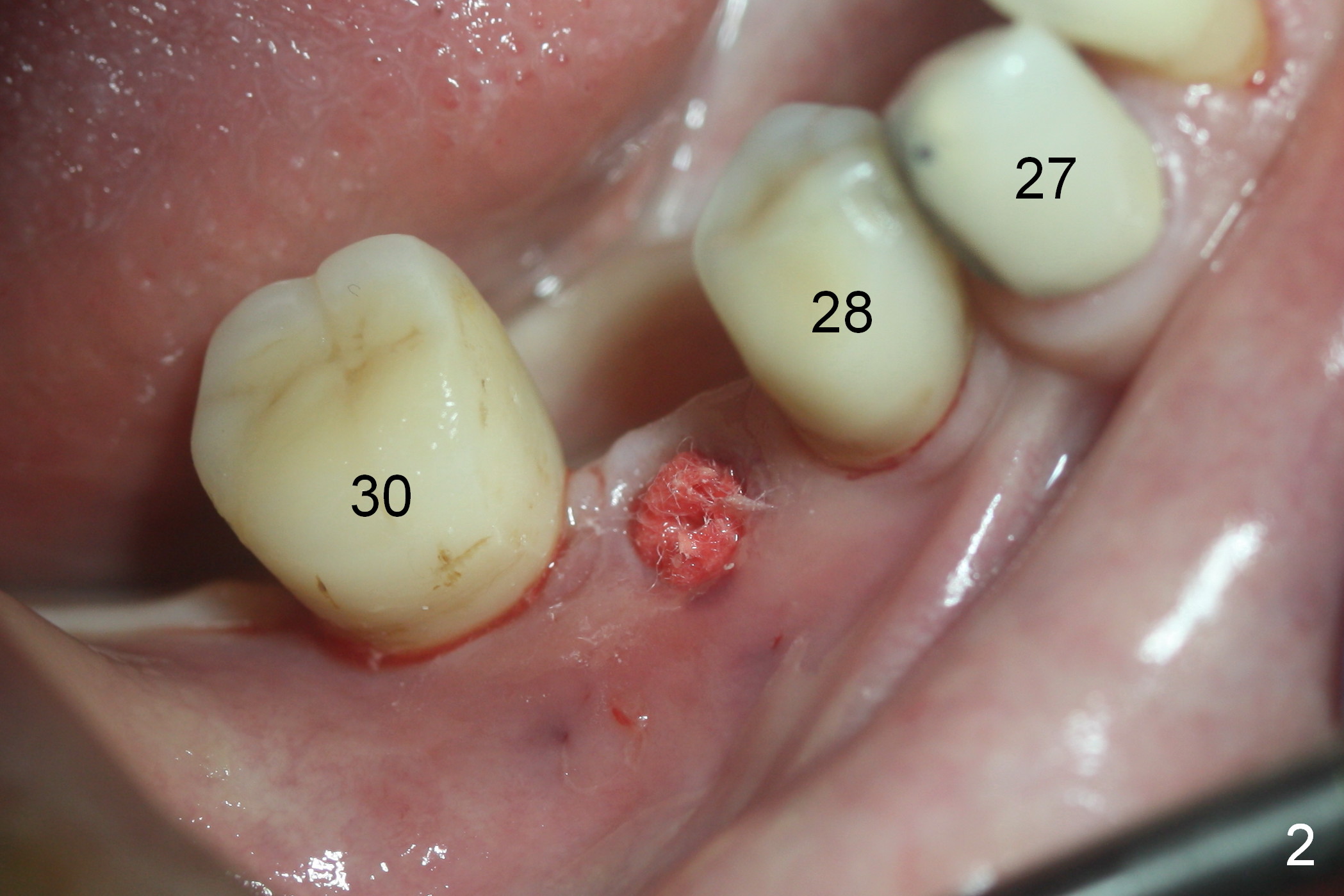
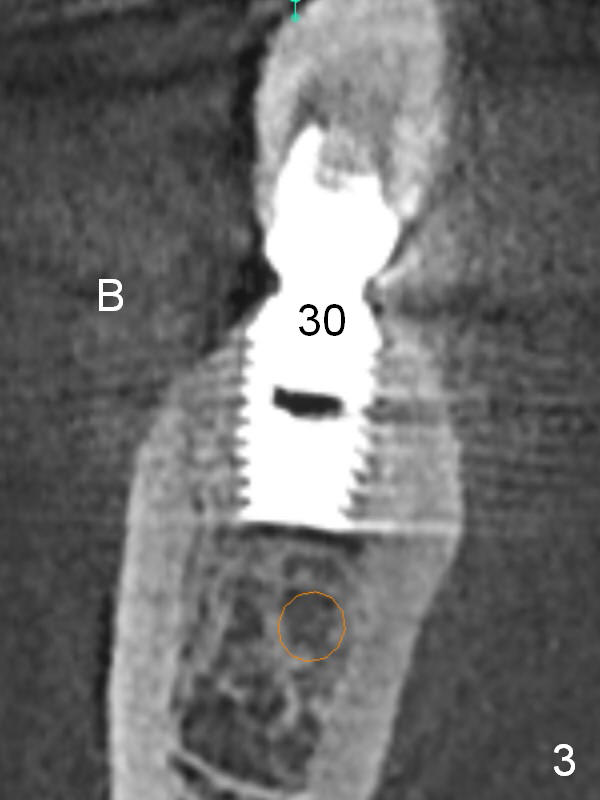
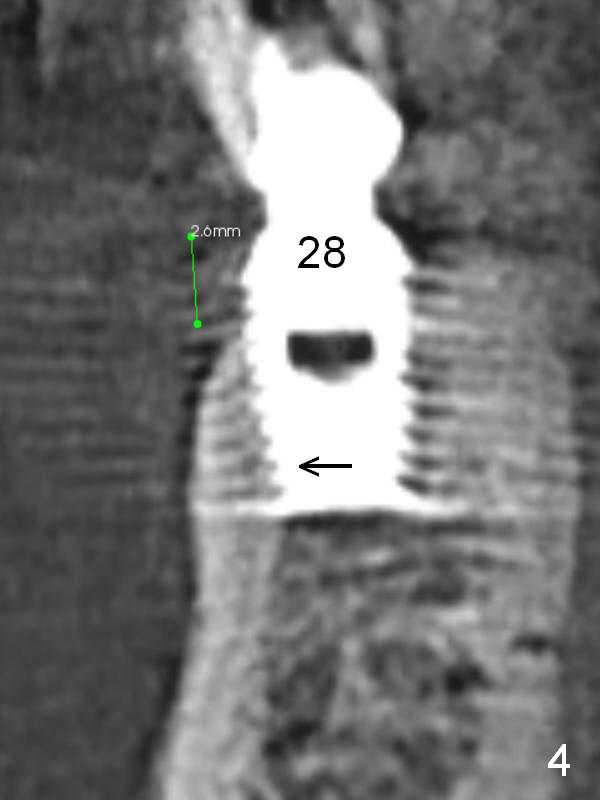
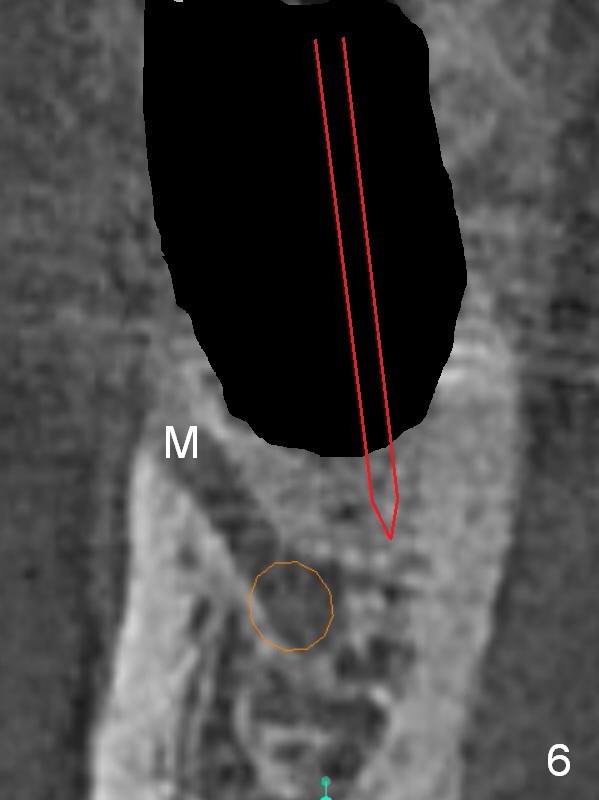
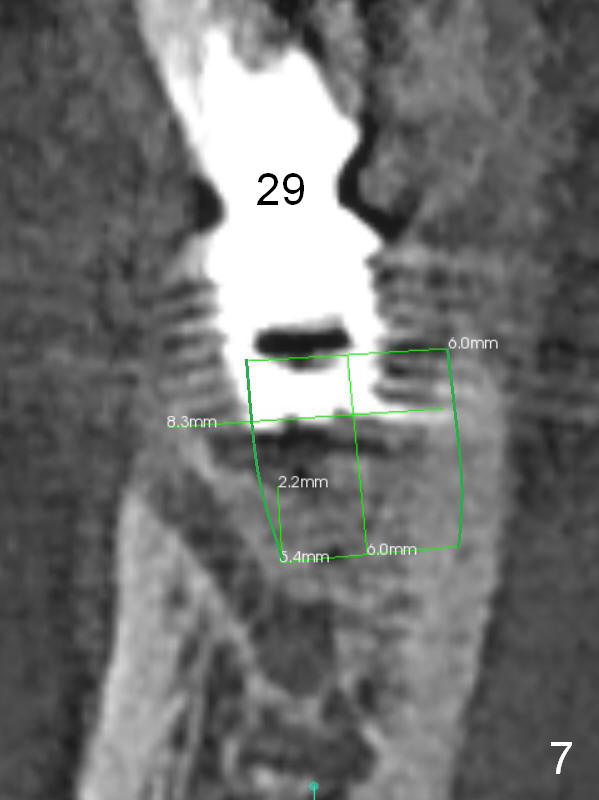
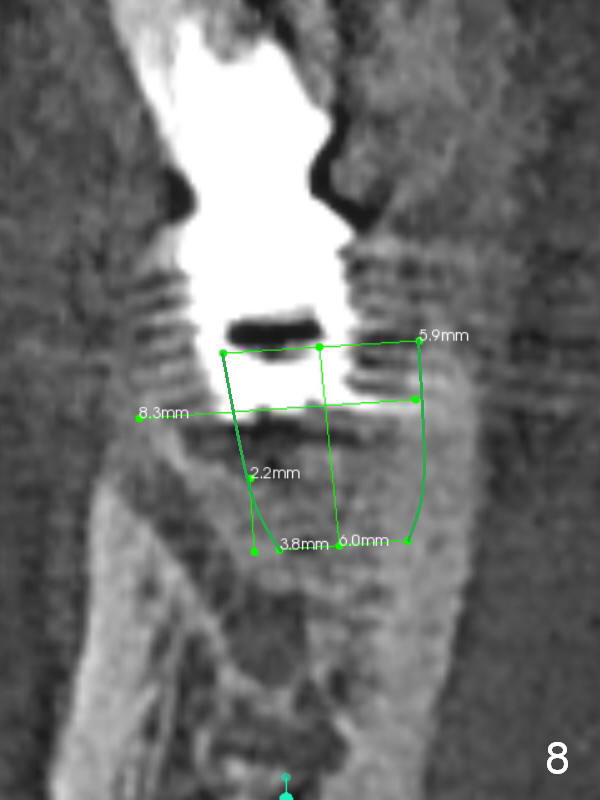
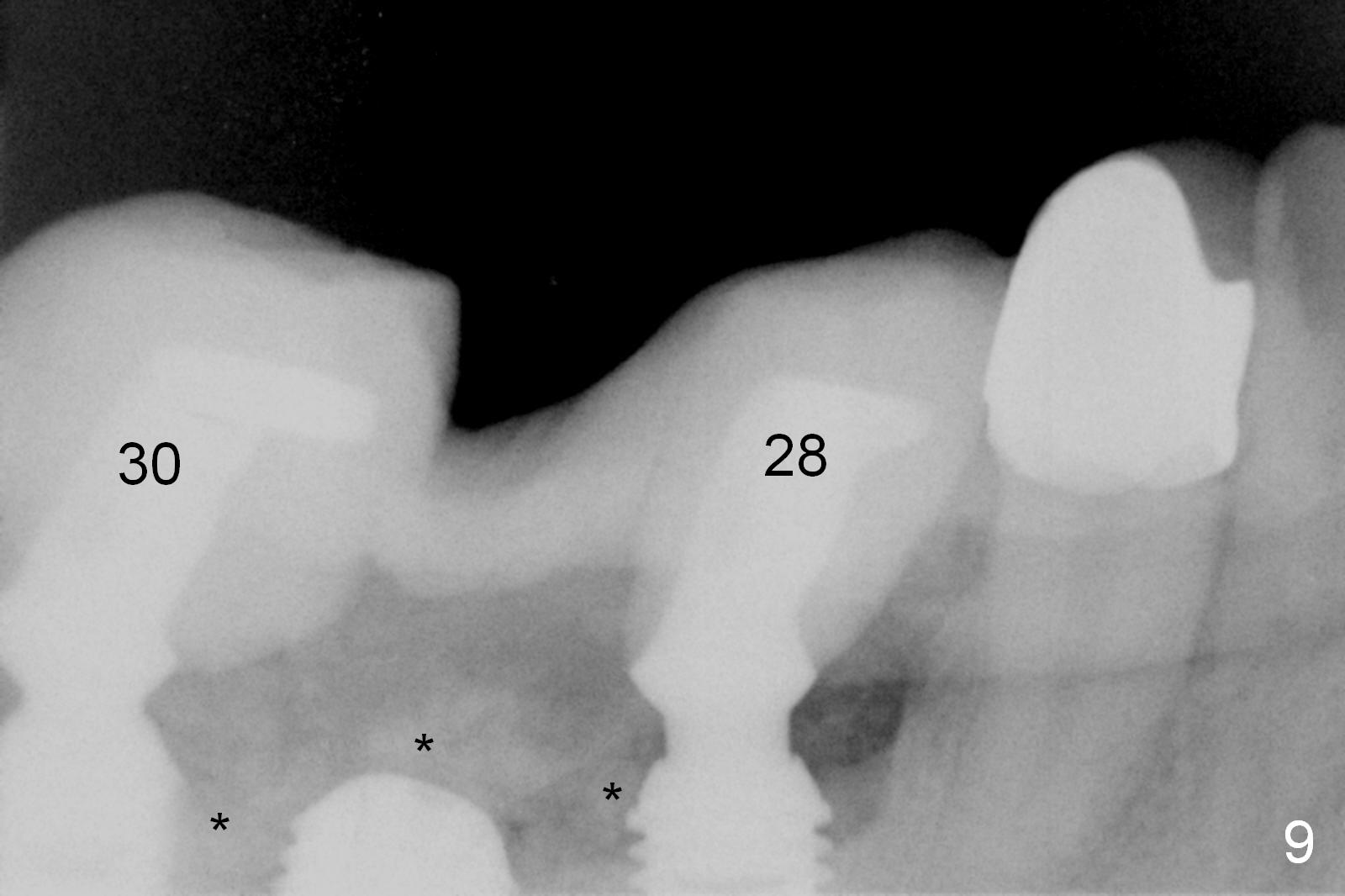
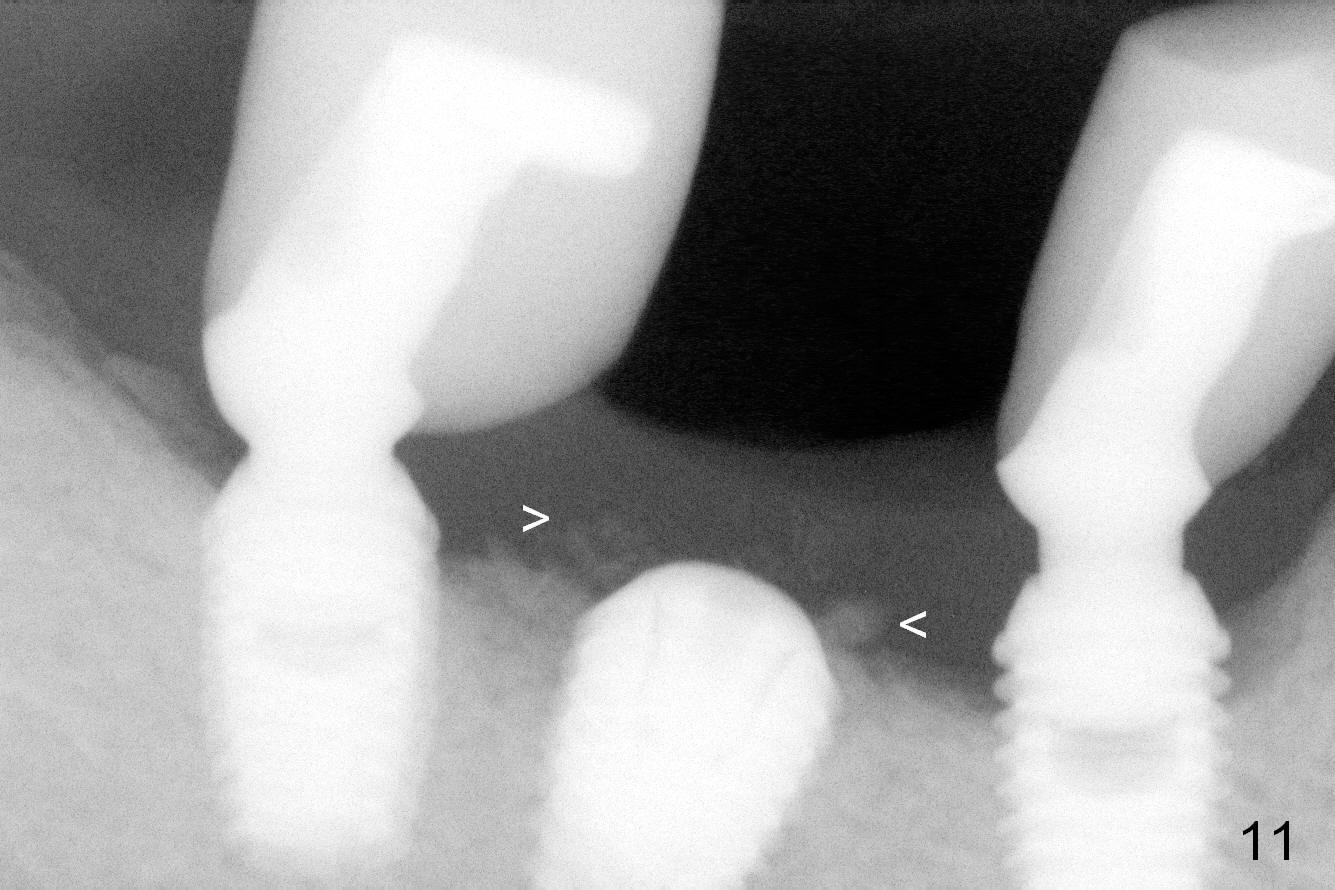
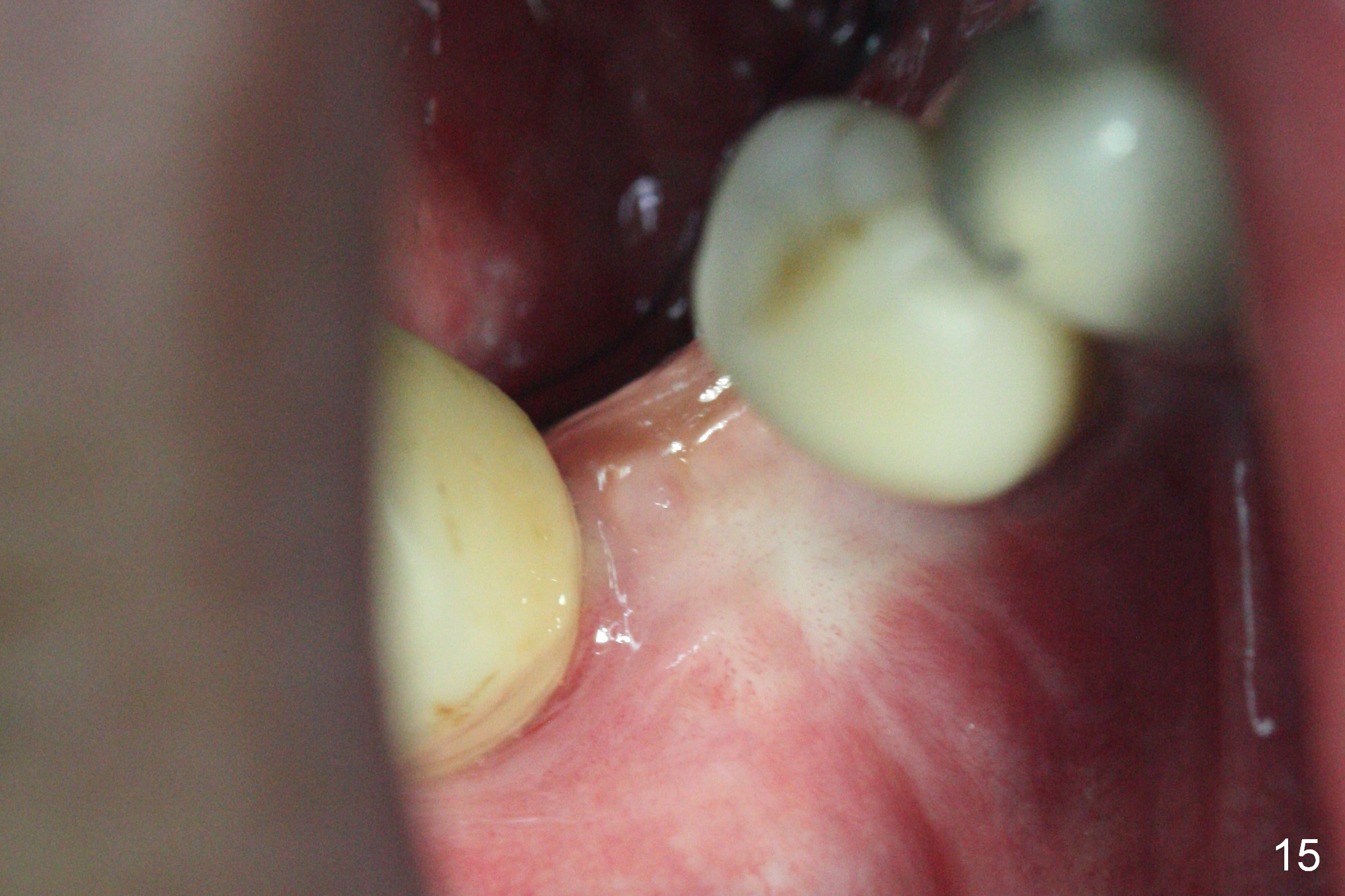
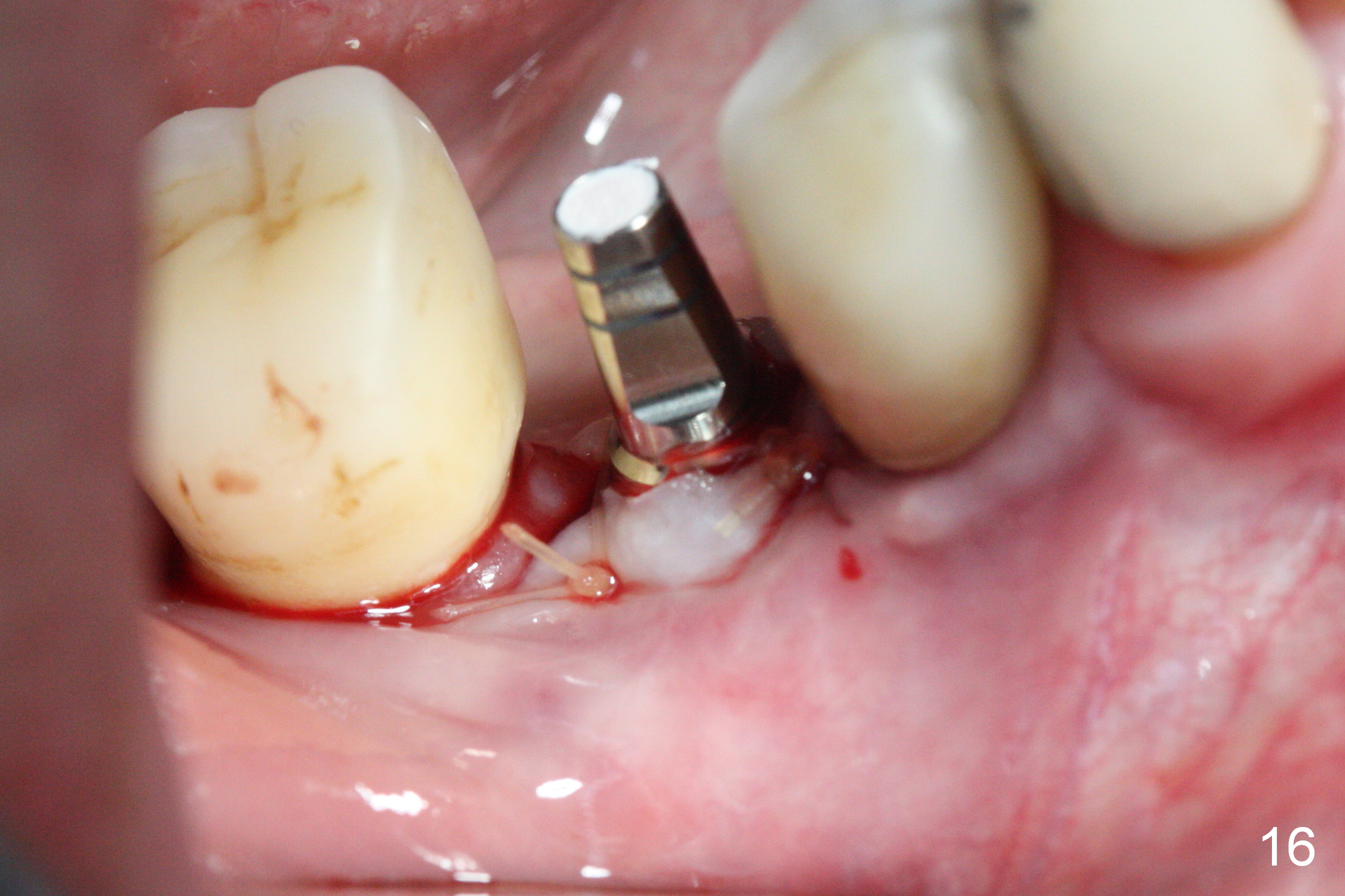
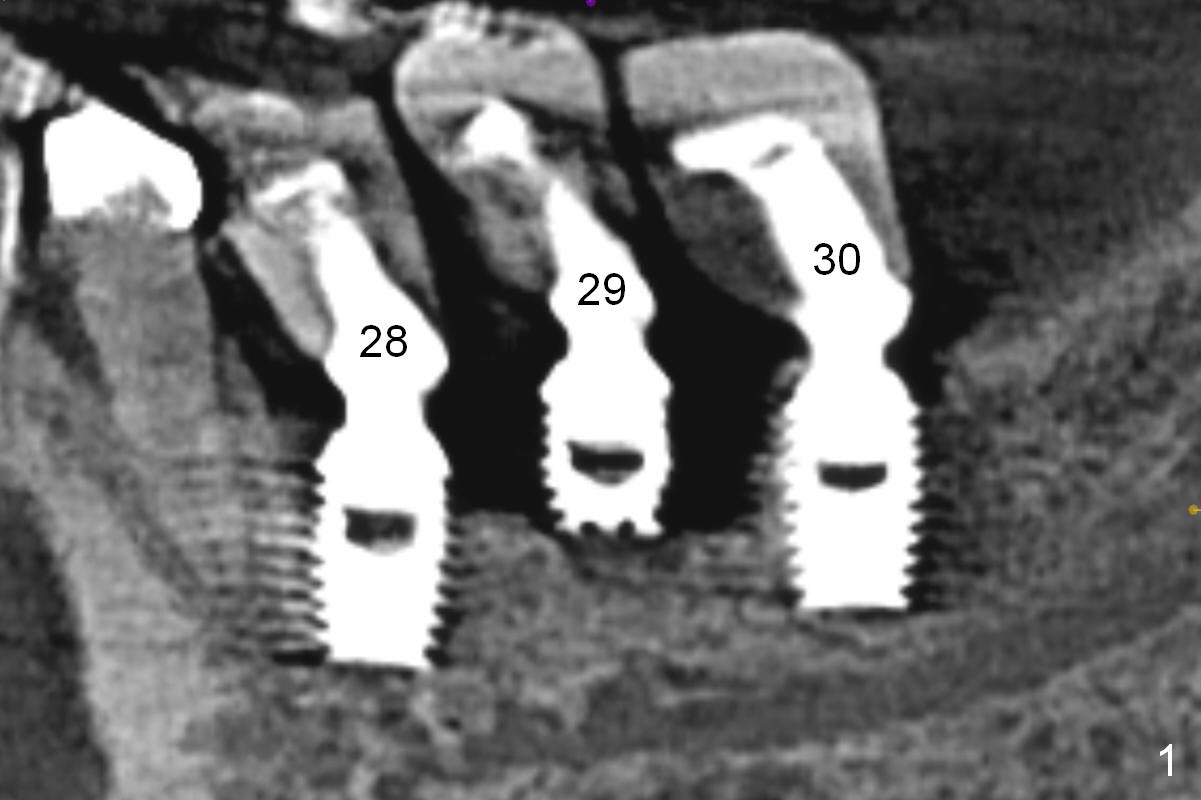
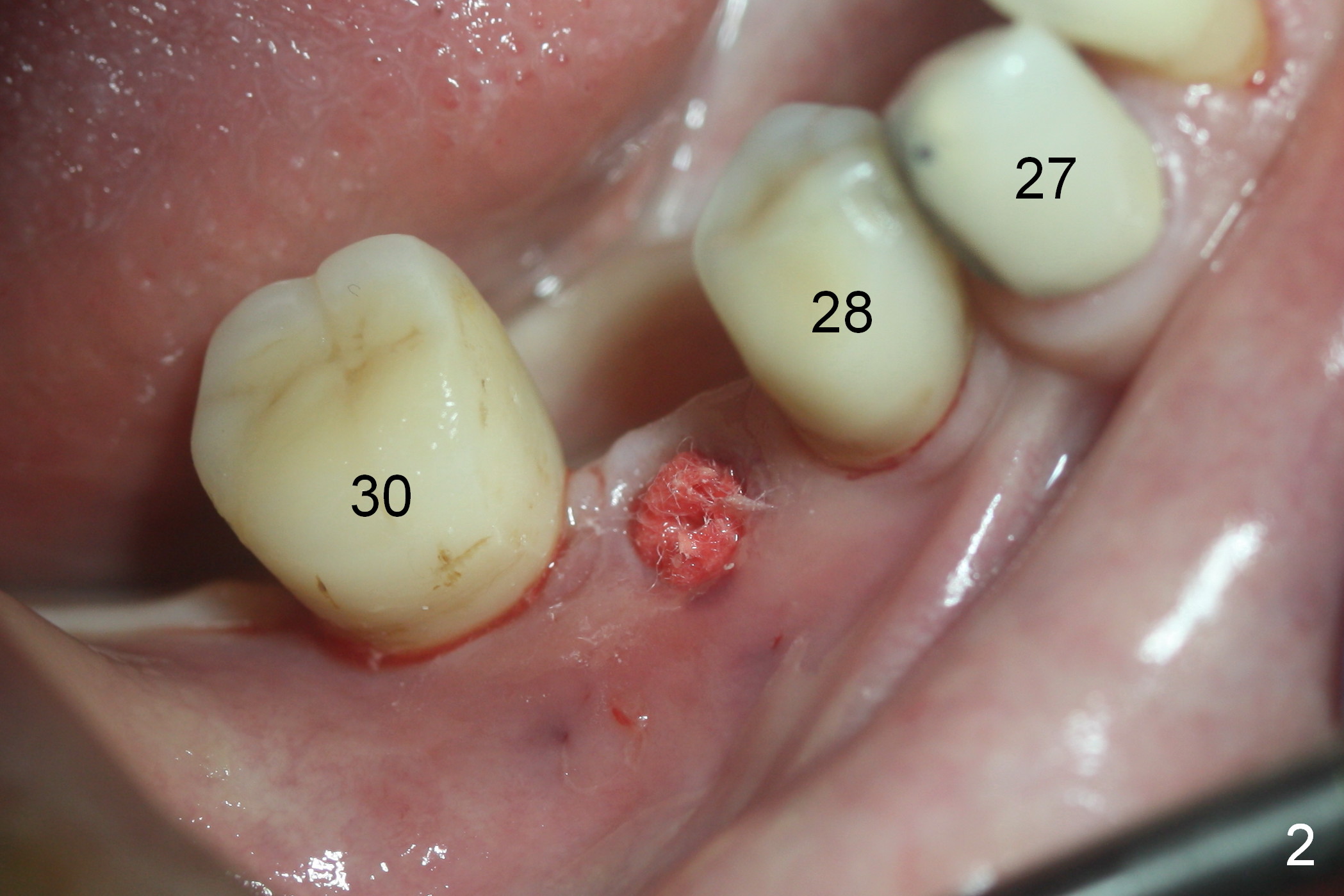
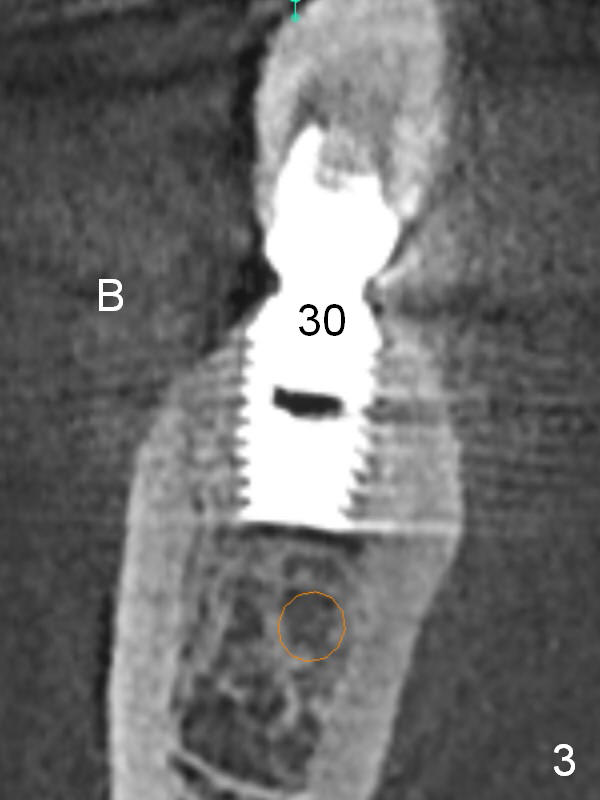
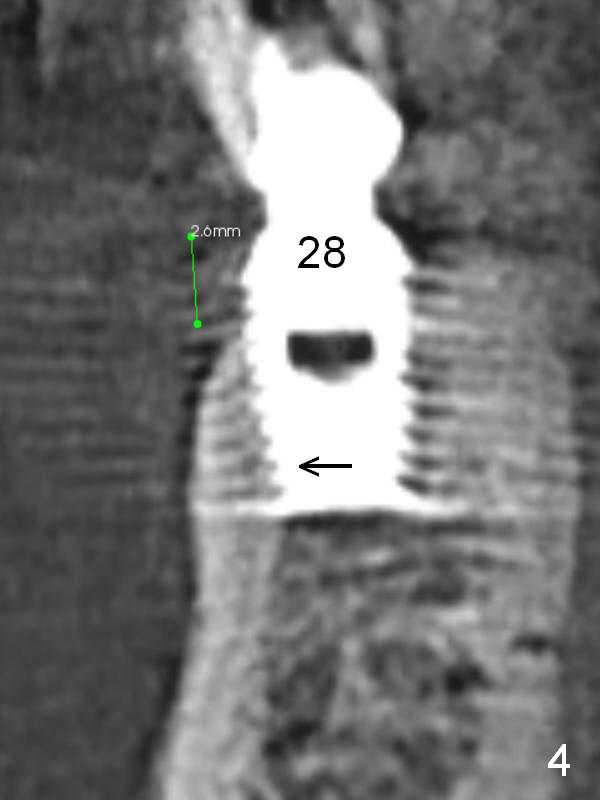
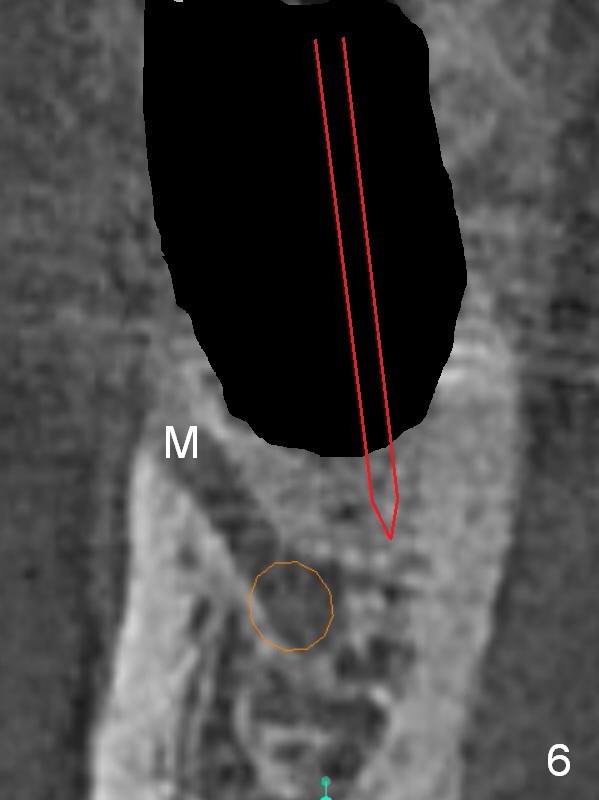
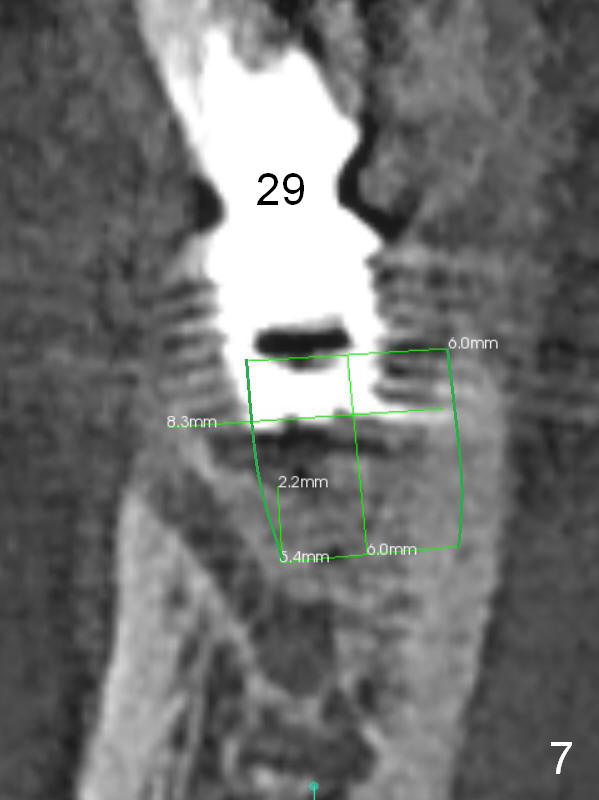
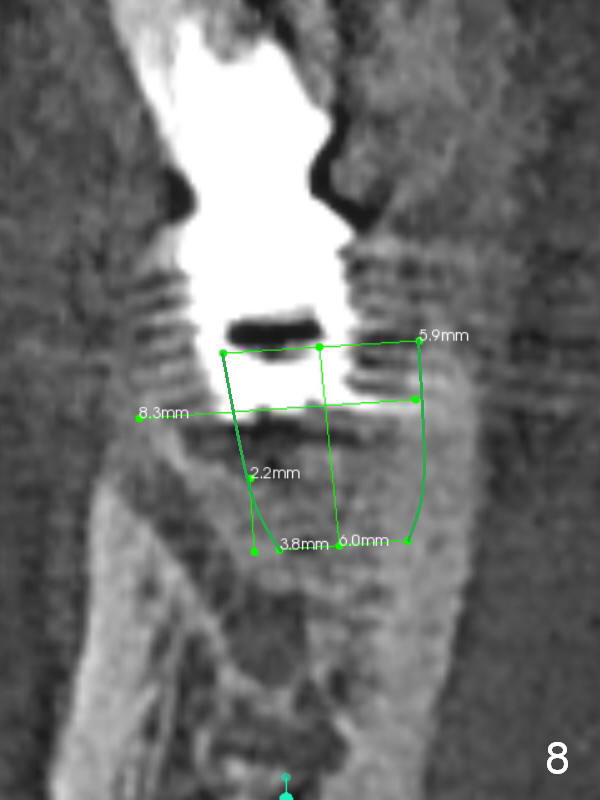
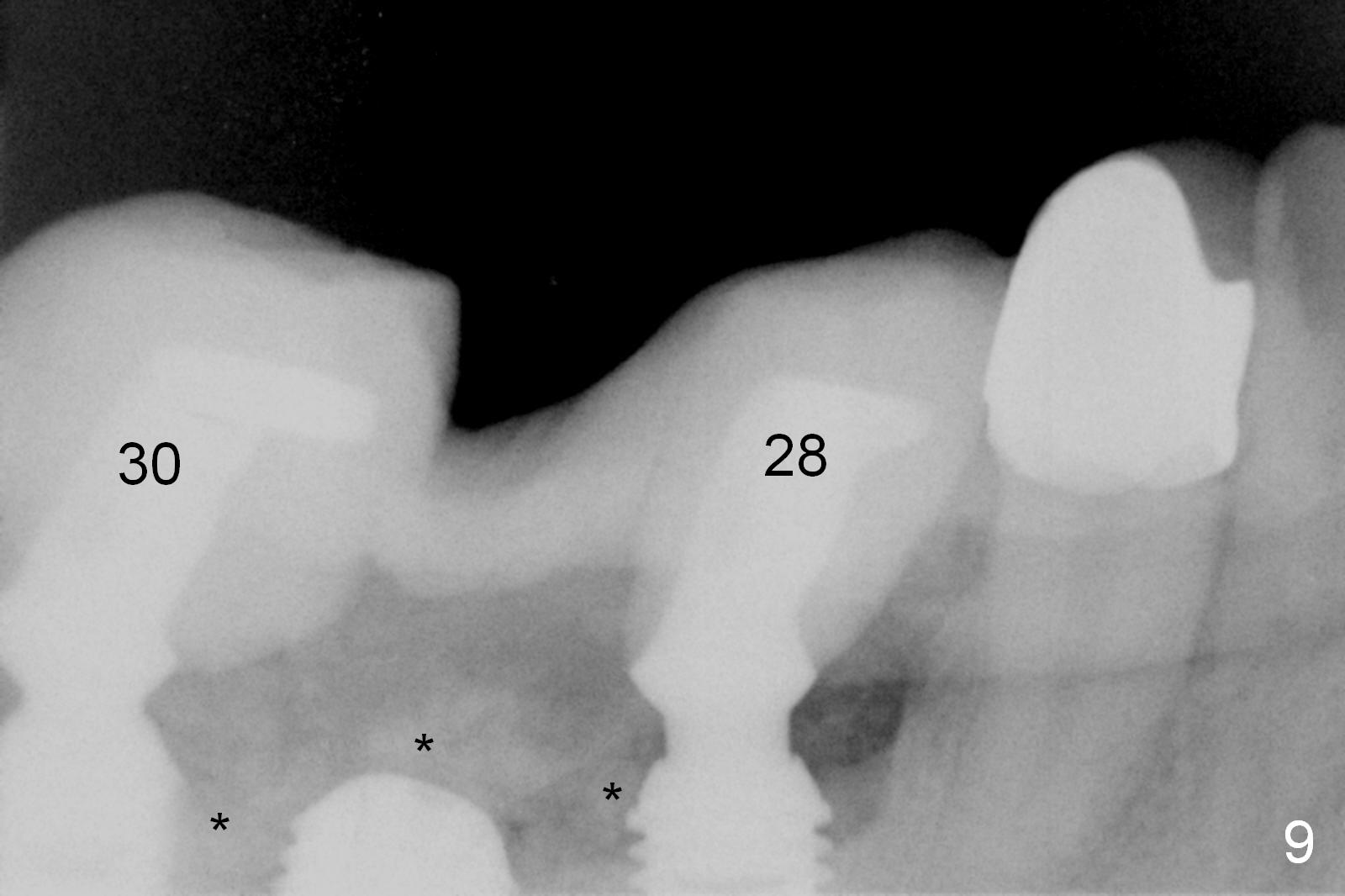
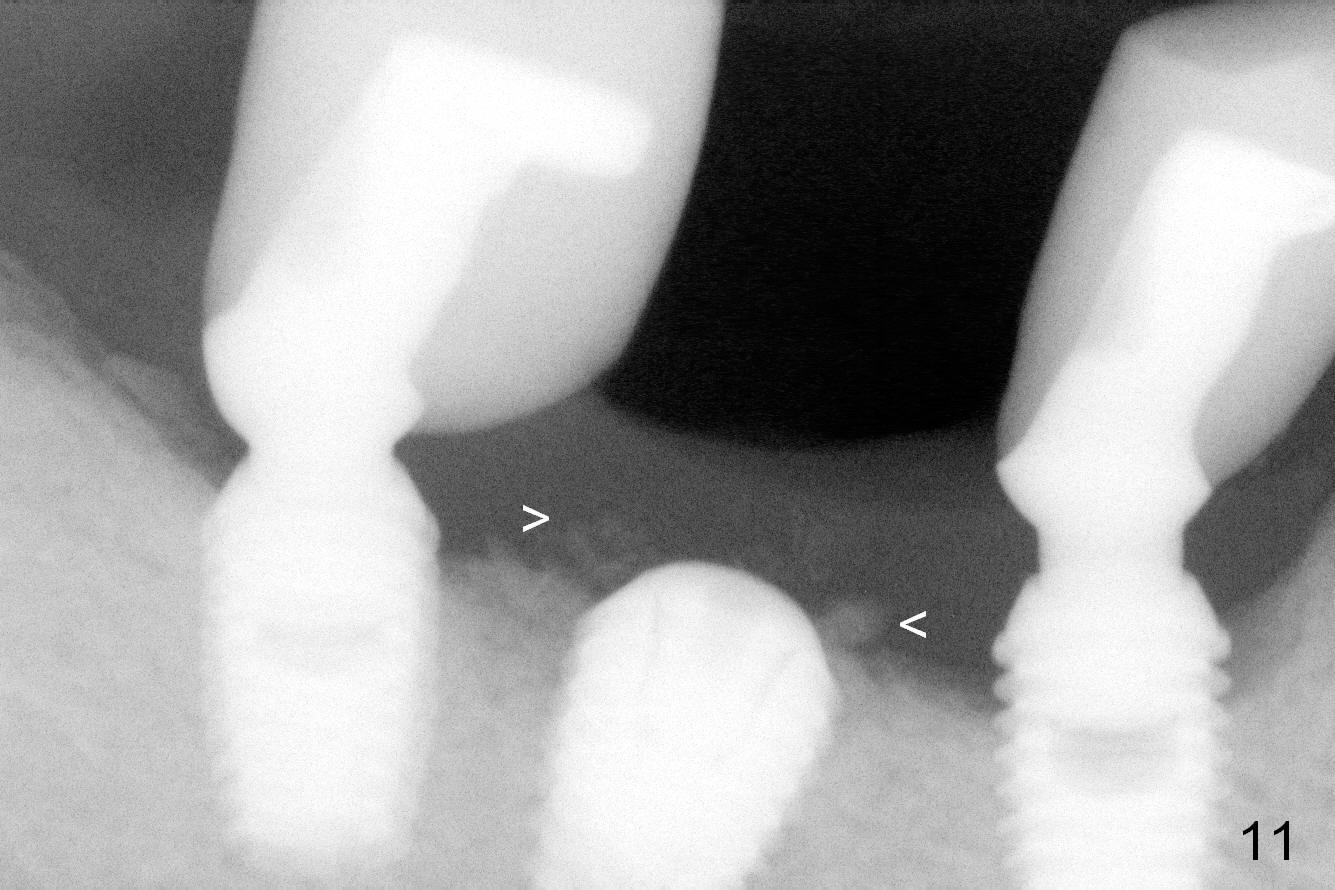
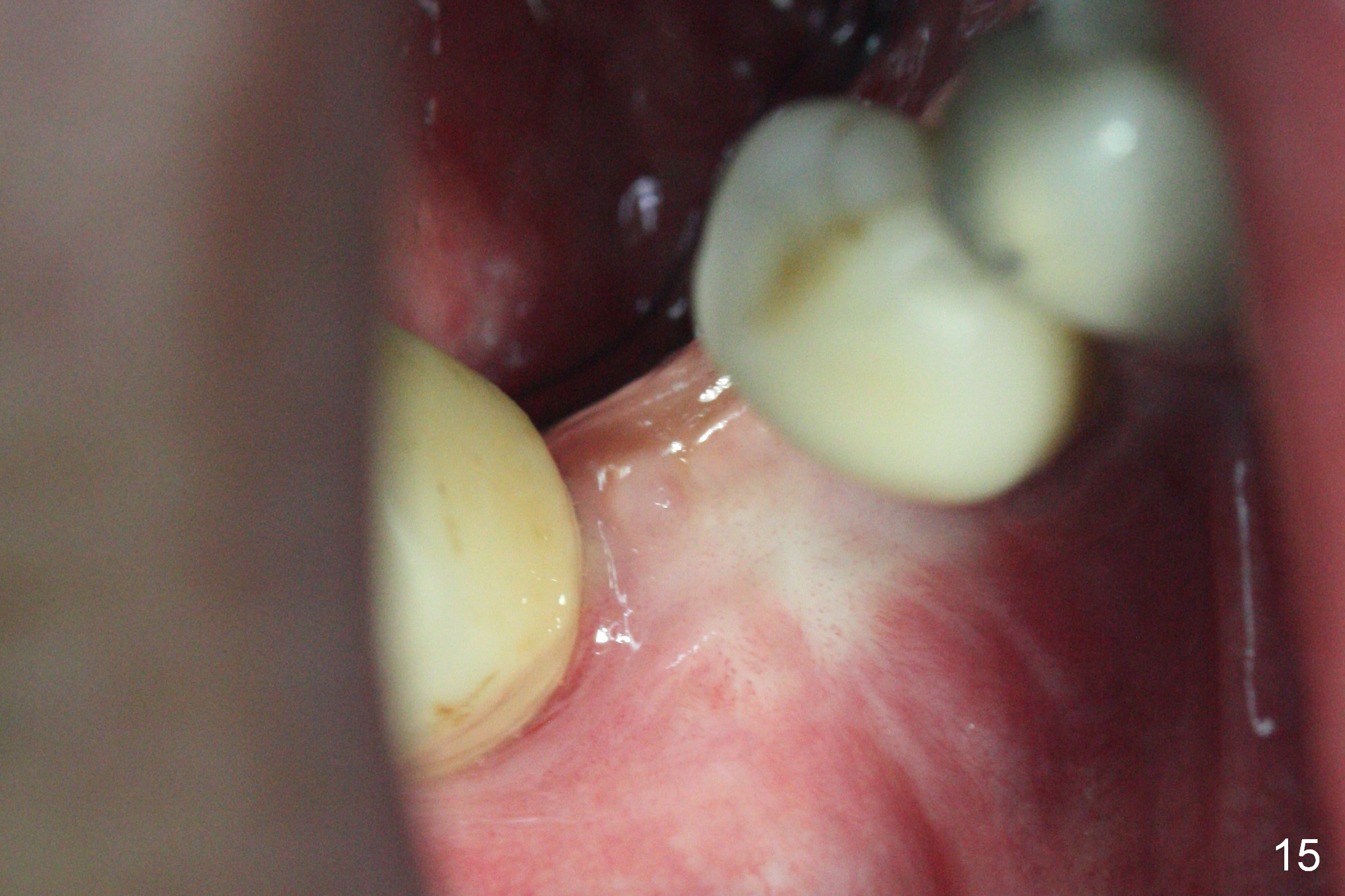
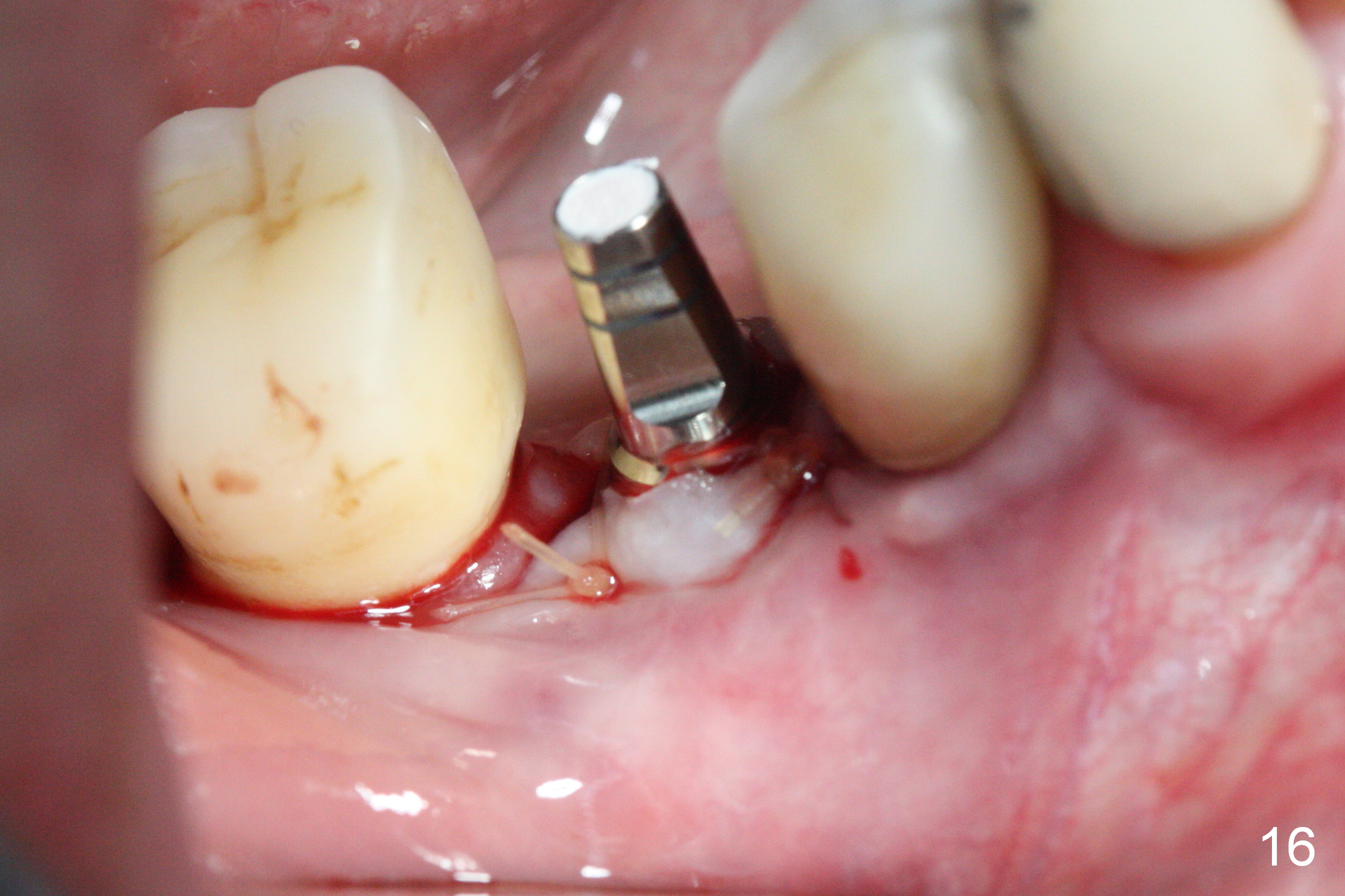
Preop CT confirms severe bone loss around the implant at #29 (Fig.1,7). The remaining implants at #28 and 30 are surrounded by basically non-keratinized gingiva (Fig.2), as compared to that of the tooth #27 (keratinized gingiva). When the buccal gingiva is opened, there is buccal (B) thread exposure of the implants at #28 and 30 with mild periimplantitis (Fig.3,4 (coronal sections). The exposed threads are cleaned with Titanium brush and later covered by allograft. The extraction socket at #29 is saucer-like (Fig.5). Osteotomy is initiated as lingual as possible (Fig.6 red arrow to avoid the Mental Canal (M)); the depth of the osteotomy is 4 mm. There is pain associated with the osteotomy with infiltration anesthesia. Later block anesthesia has to be administered to place a 6x6 mm UF implant with better surface treatment (Fig.7,9,10). The drawback is the larger apical diameter (5.4 mm vs. 3.8 mm of 5.9x6 mm SM implant (Fig.8)). In fact there is brisk hemorrhage from the apicomesiobuccal line angle of the final osteotomy (invasion of the Mental Canal (?)). Gauze has to be packed for hemostasis. Socket preservation is prepared. When the gauze is removed, hemostasis has been achieved. The UF implant is placed, followed by collagen membrane and bone graft (Fig.9,10 *). The wound is closed with some tension, since the Mental neurovascular bundle is close to the incision and it is difficult to dissect. Periodontal dressing is applied. It would be better to place a healing or definitive abutment to reduce suturing tension. In fact the wound dehisces (Fig.13). PRF (Fig.14) is applied twice apparently without success. Finally the wound heals 5 months postop with reduction in bone graft (Fig.11,12). The keratinized tissue is lacking. At the appointment of uncover, harvest gingival graft from the palate and insert PRF membrane in the donor site. In fact there is keratinized gingiva at the site (Fig.15). A 4.5x7(4) mm abutment is placed. Three weeks later, the provisional is lost; the angulation of the abutment is not ideal (Fig.17). When the abutment is changed into 4.5x15° B(4 mm) angled one (Fig.18), the angulation is better (Fig.19).
Return to Lower Premolar Immediate Implant
Xin Wei, DDS, PhD, MS 1st edition 05/24/2016, last revision 01/19/2018