

.jpg)

 |
 |
 |
 |
 |
.jpg) |
 |
 |
  |
Severe Bone Loss Involving Neighboring Tooth
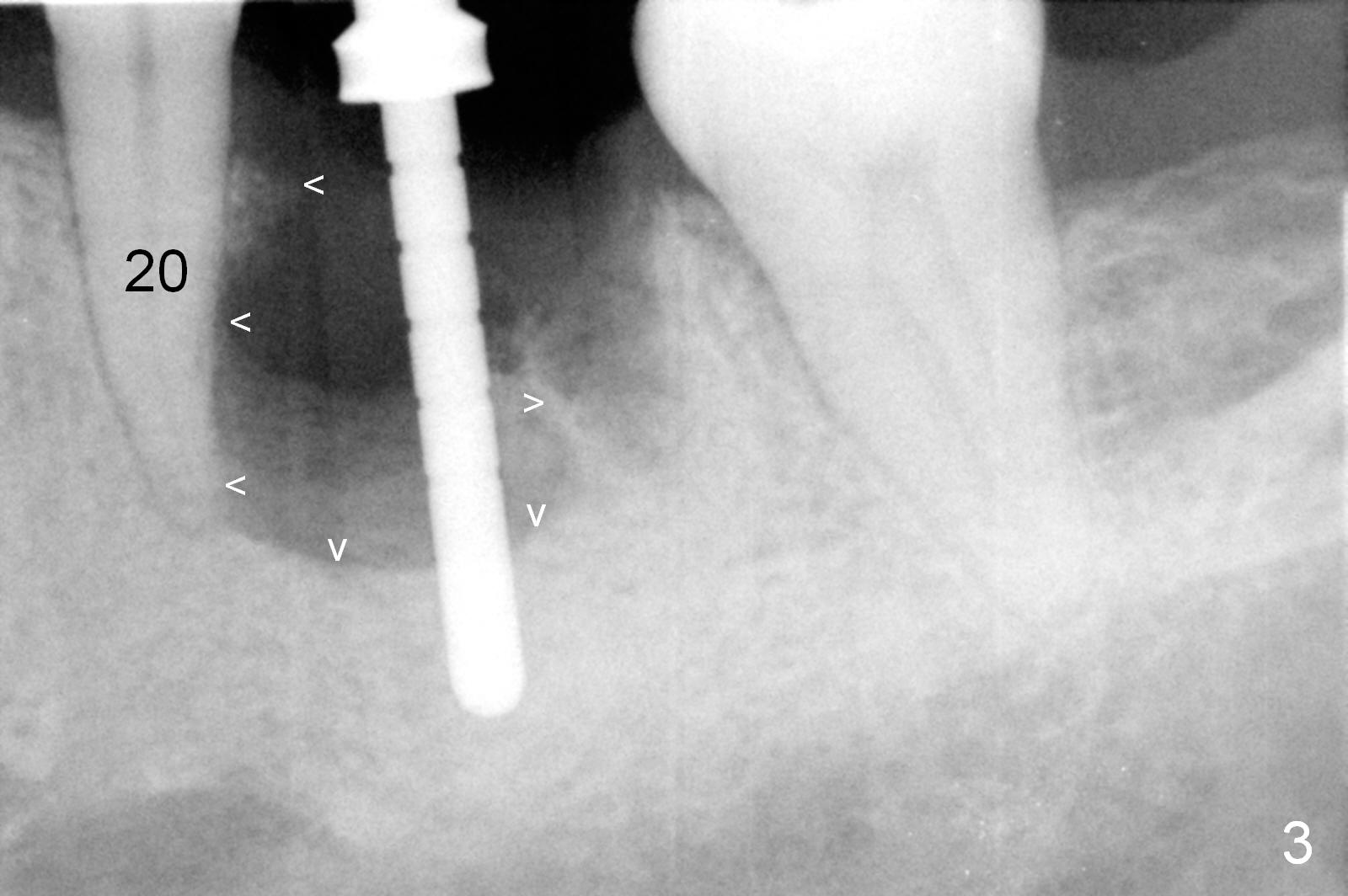
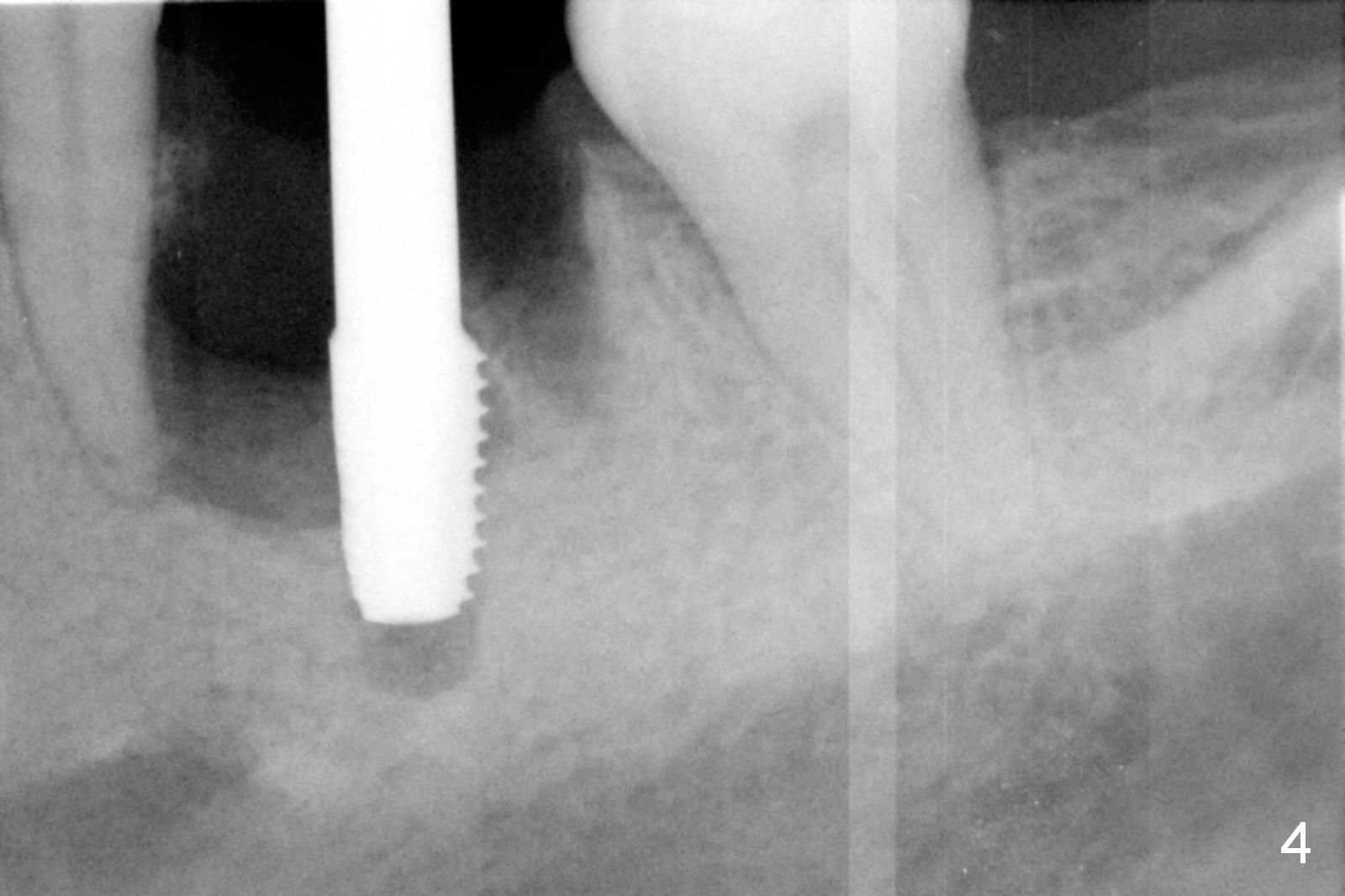
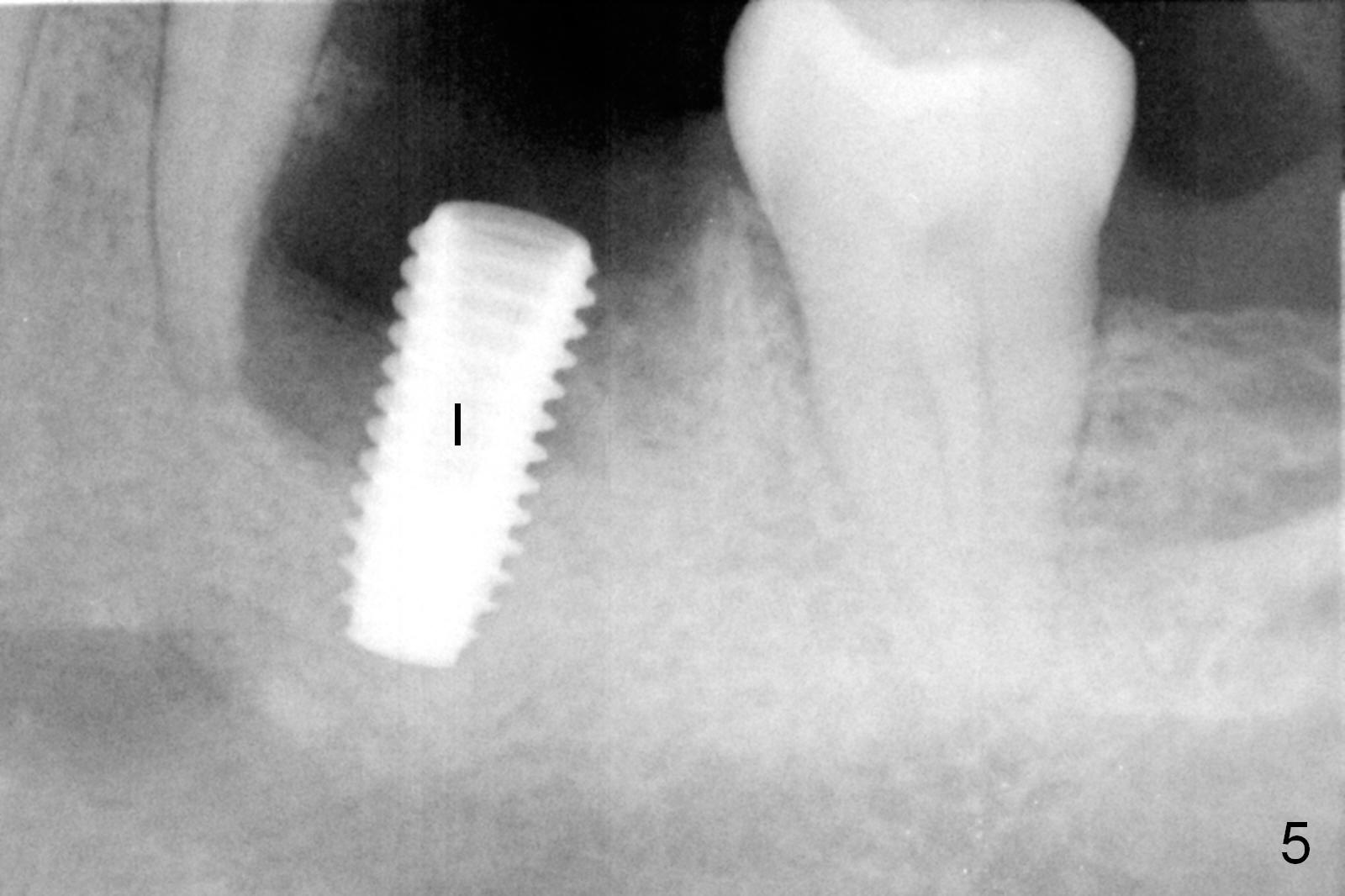
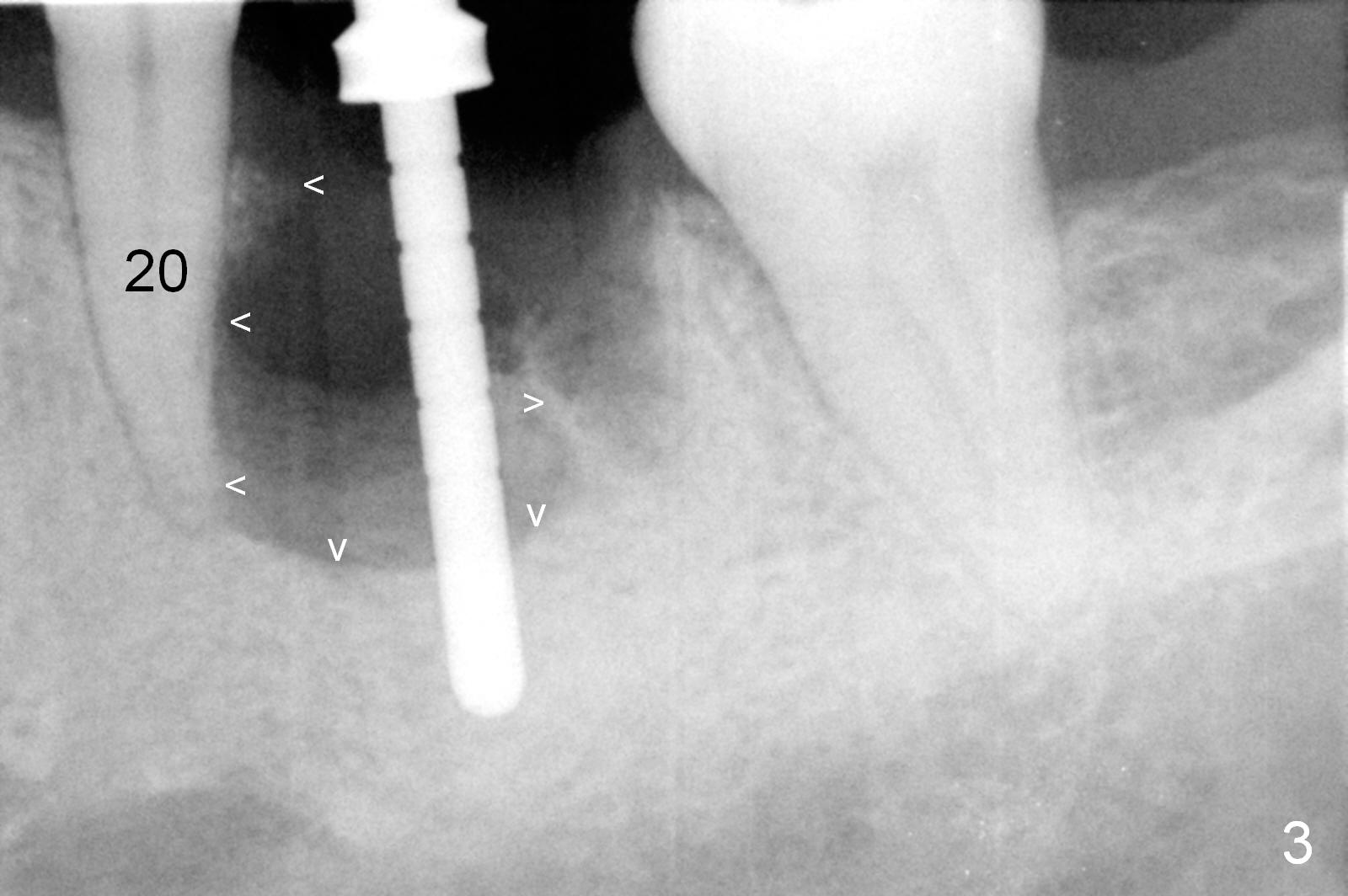
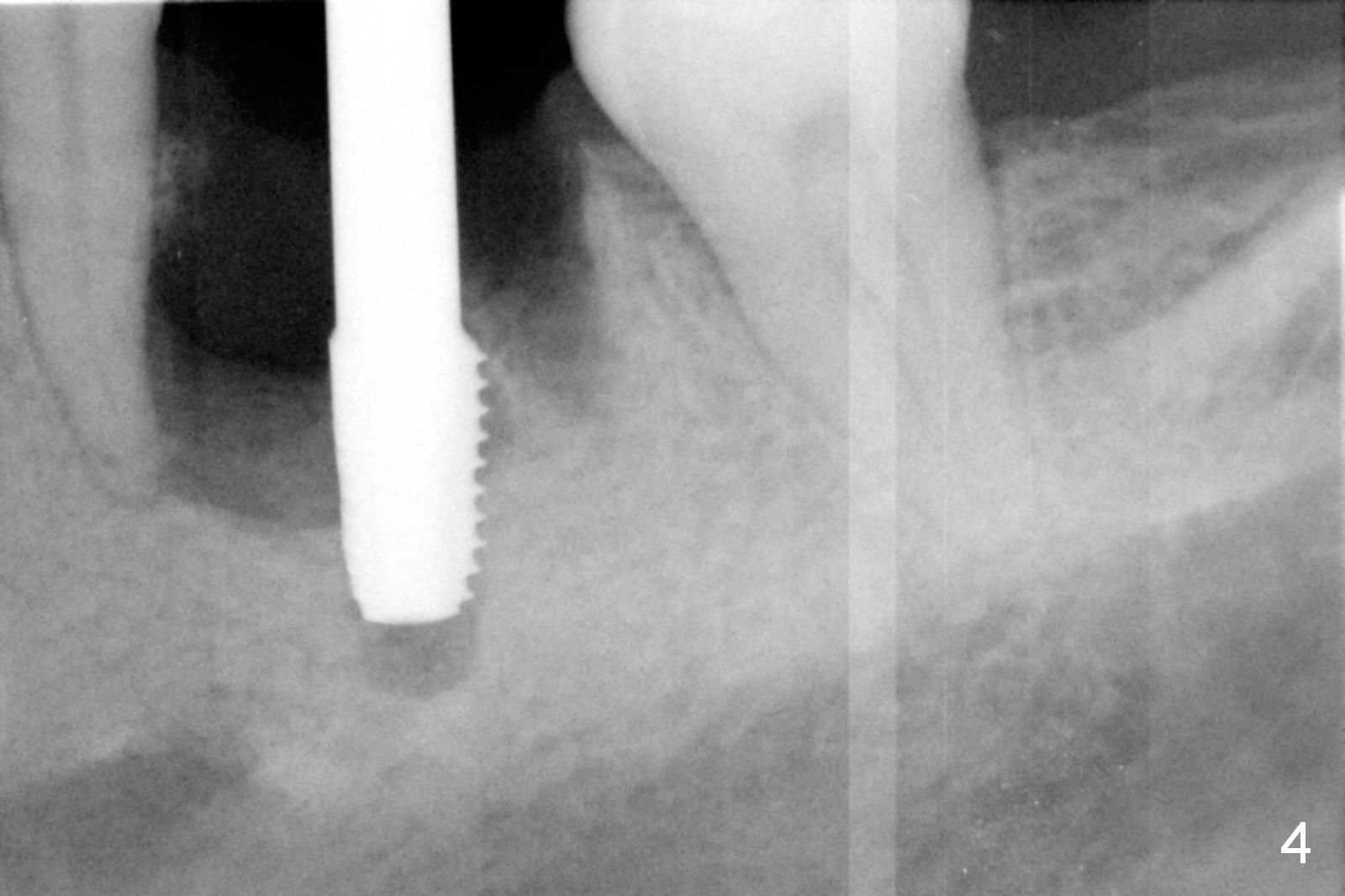
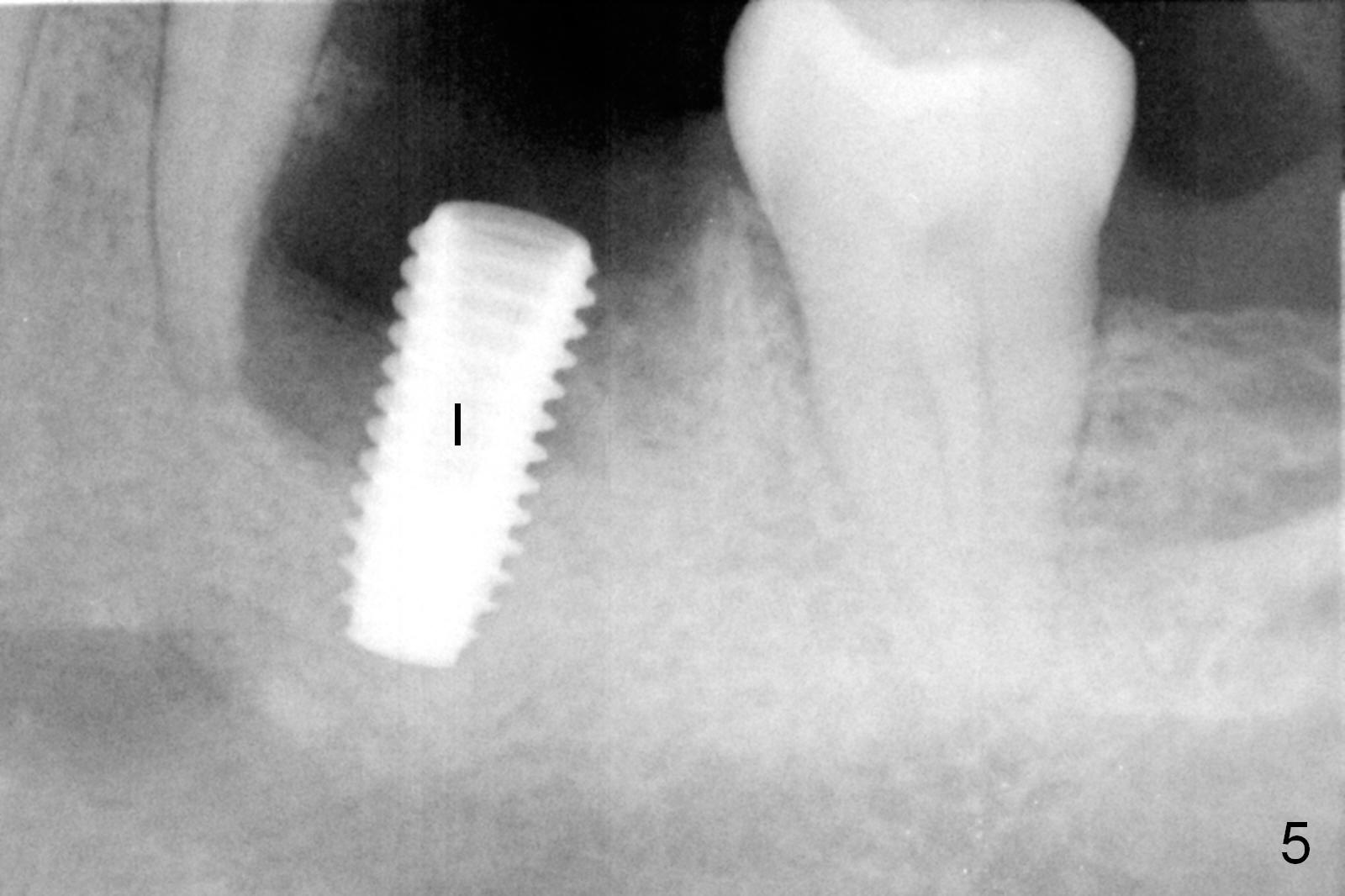
A large periapical radiolucent lesion was detected associated with the mesial root of the tooth #19 10 years ago (Fig.1 arrowheads). Recently severe pain forces the patient to take Amoxicillin for 2 weeks and accepts treatment. There is mild tenderness in the mesiobuccal root area (Fig.2). When the tooth is extracted, the socket debrided and osteotomy is initiated, bone loss is much more severe (Fig.3) than that in Fig.1. The mesiobuccal plate is completely destroyed. There is almost no bone distal to the tooth #20 clinically when the tooth #19 is removed. Pain control is poor with infiltration anesthesia (multiple injections) and incomplete insertion of a 4.5 mm tap (Fig.4). After block anesthesia, osteotomy increases with tight depth control; a 5x11.5 mm implant is placed with 50 Ncm (Fig.5 I). Mixture of autogenous bone and allograft (.5-2 mm, Fig.6 *) is placed in the remaining bony defects before and after placement of a 7.5x4(4) mm abutment (A). An immediate provisional is fabricated to contain the graft in place.
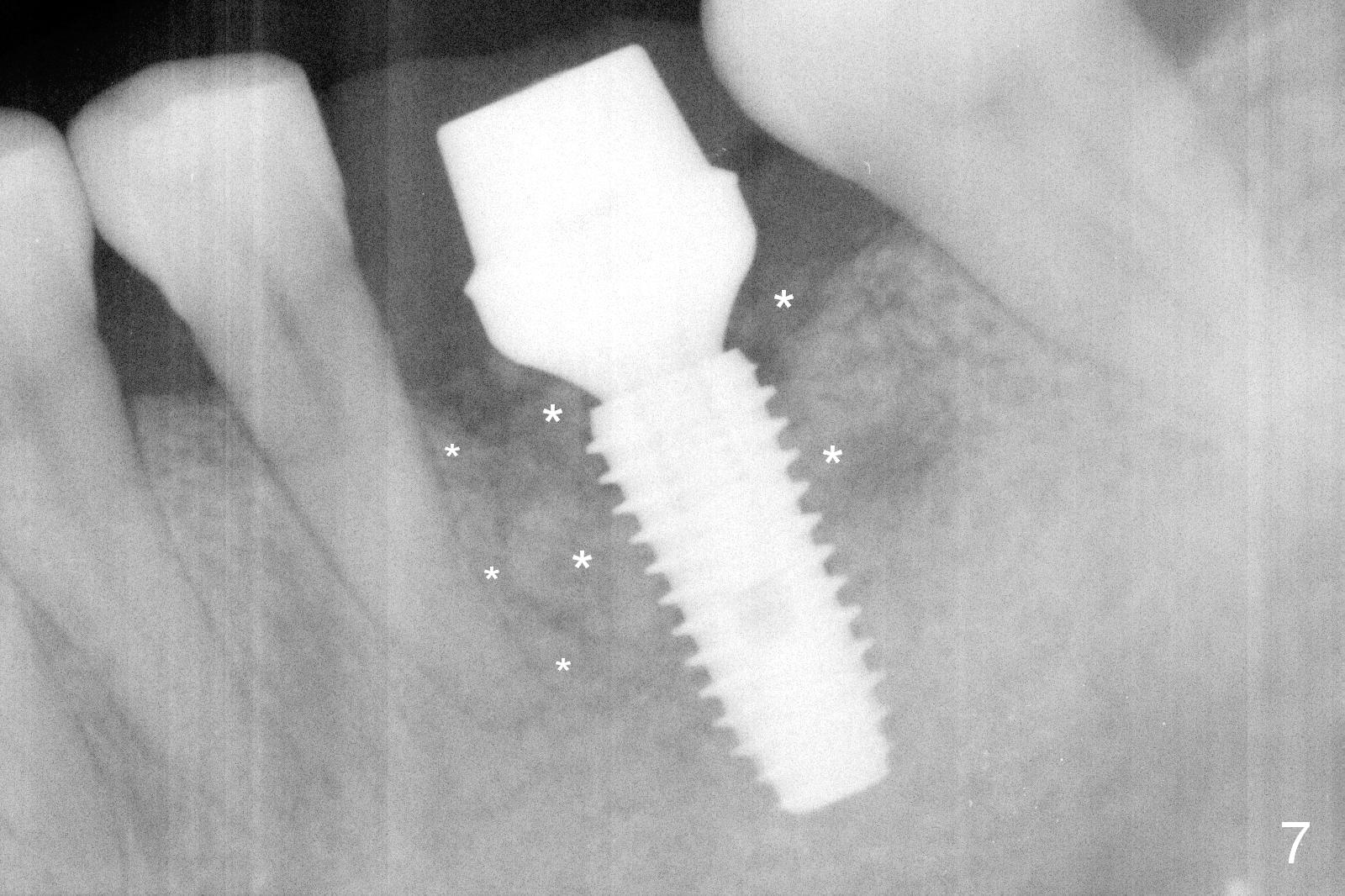
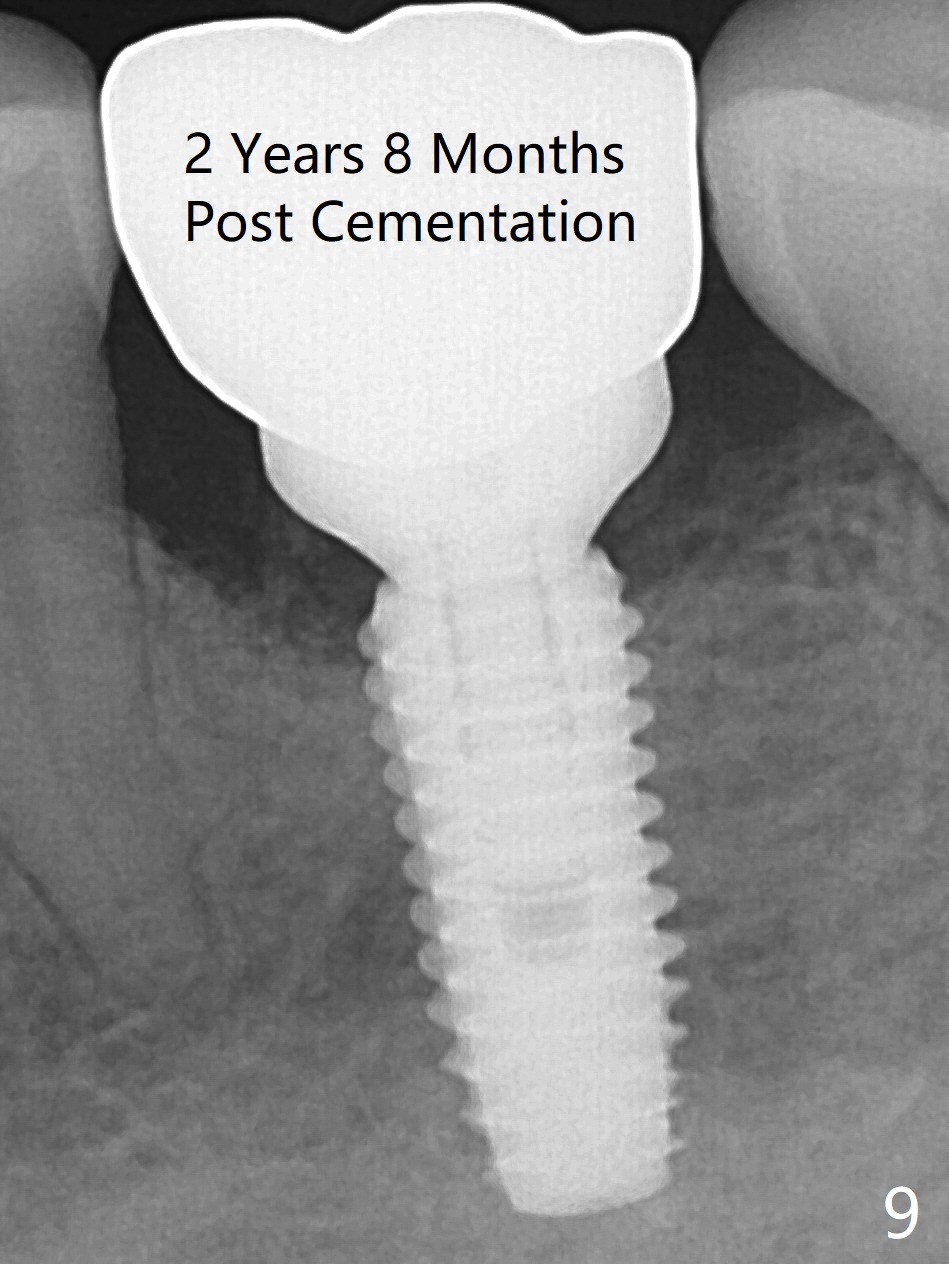
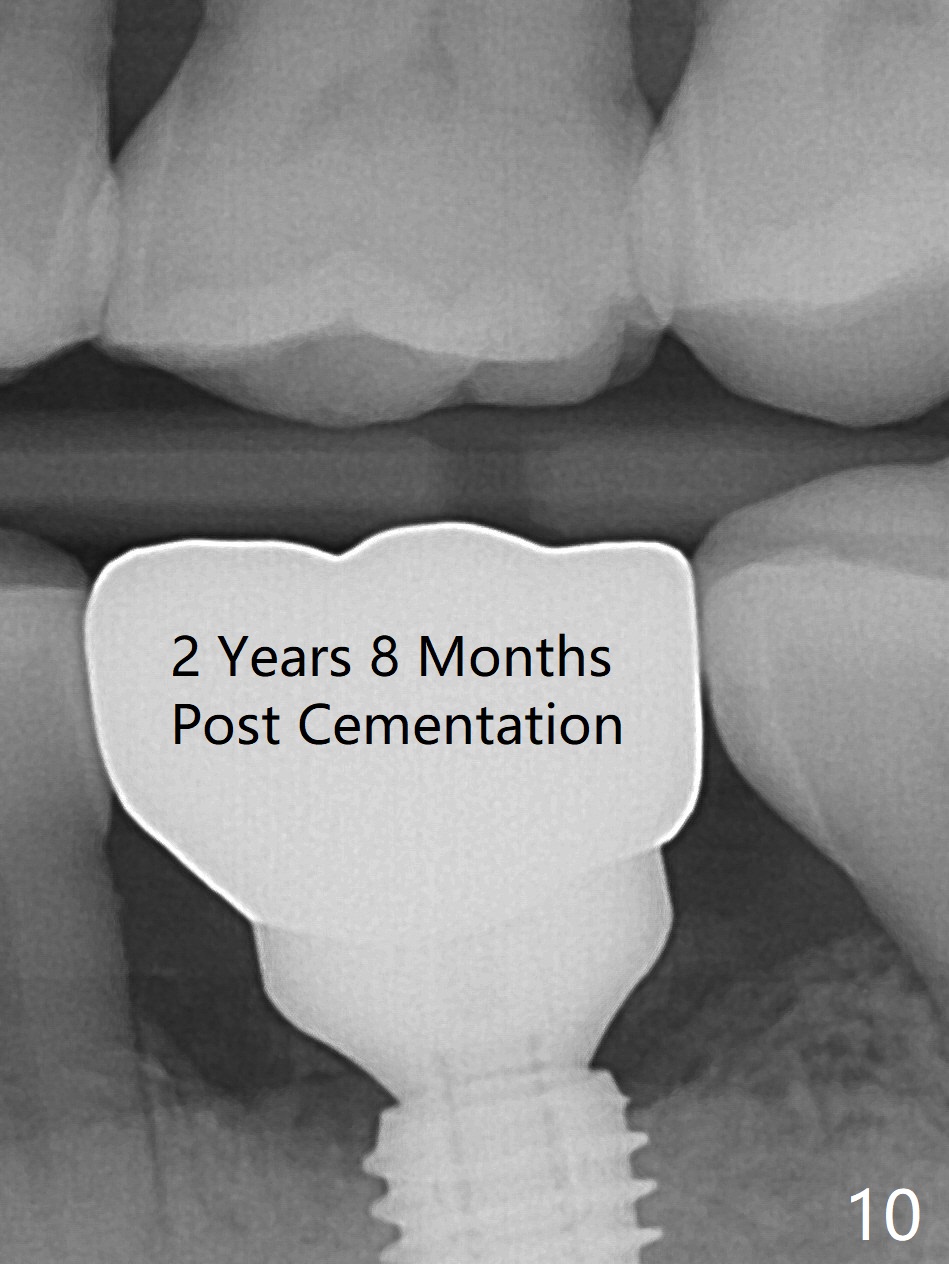
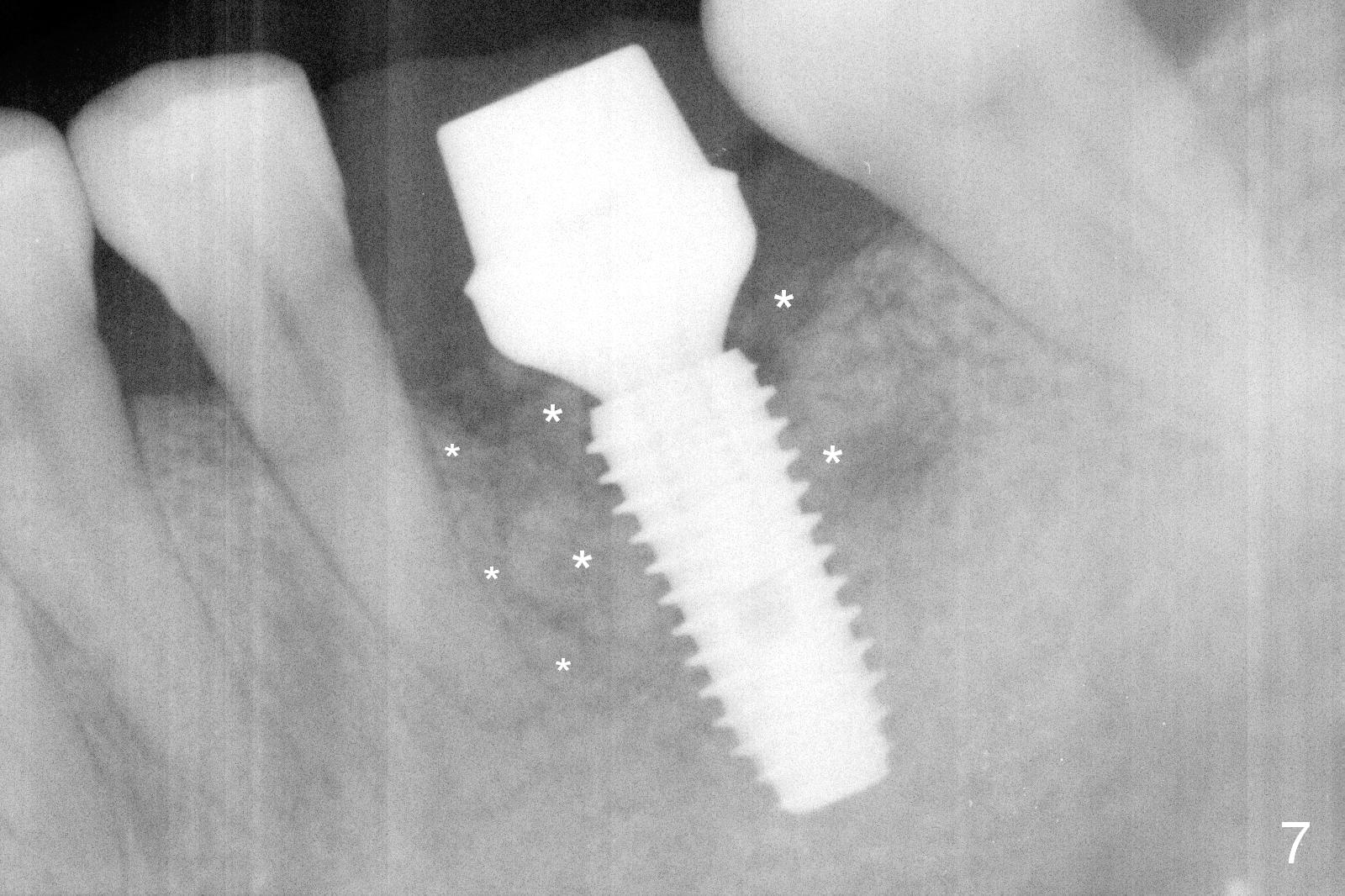
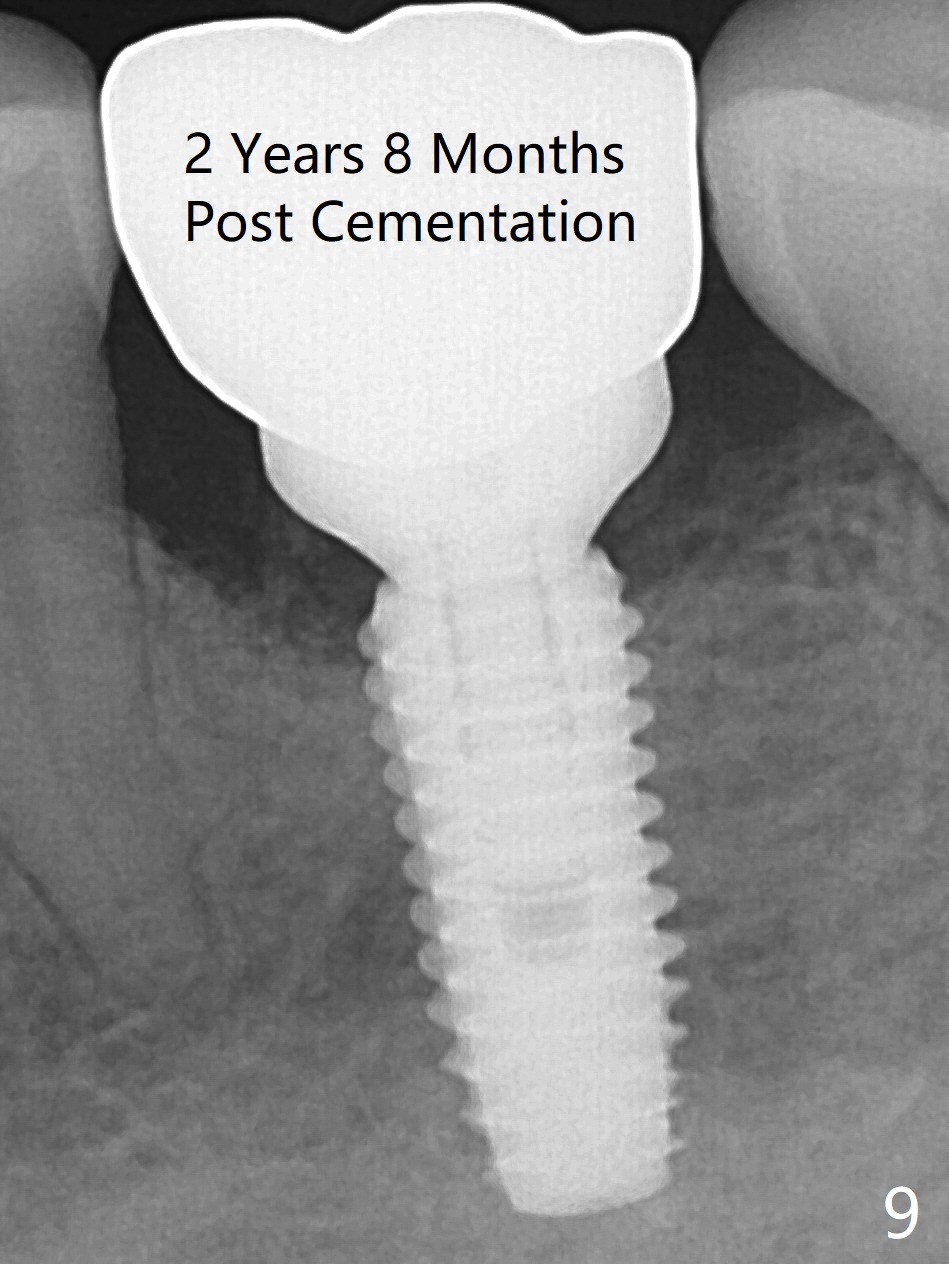
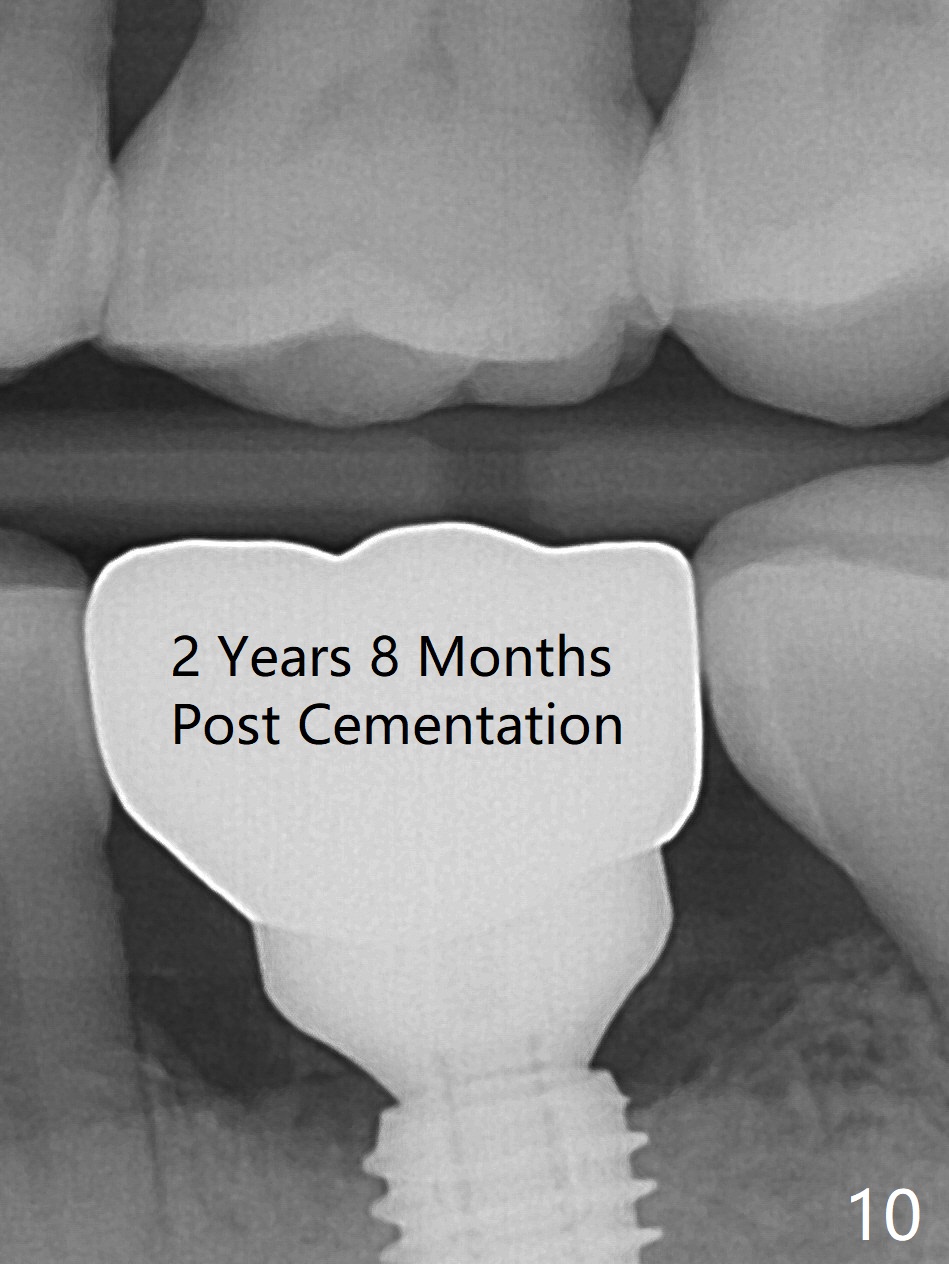
The bone graft (Fig.7 large *) remains in place 4.5 months postop. More amazing is that there is formation of new bone distal to the tooth #20 (small *). The patient does not complain of tenderness of this premolar any more. Bone density around the implant increases 8 months postop (3.5 months post cementation, Fig.8 *), although there is tenderness buccal to #19. Amoxicillin is prescribed. In fact the implant should have been placed deeper, equicrestal or slightly subcrestal distal (Fig.9,10).
Lower Molar Immediate Implant, Prevent Molar Periimplantitis (Protocols, Table), Improvement Xin Wei, DDS, PhD, MS 1st edition 07/18/2016, last revision 12/05/2019