



 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
As Large As Possible
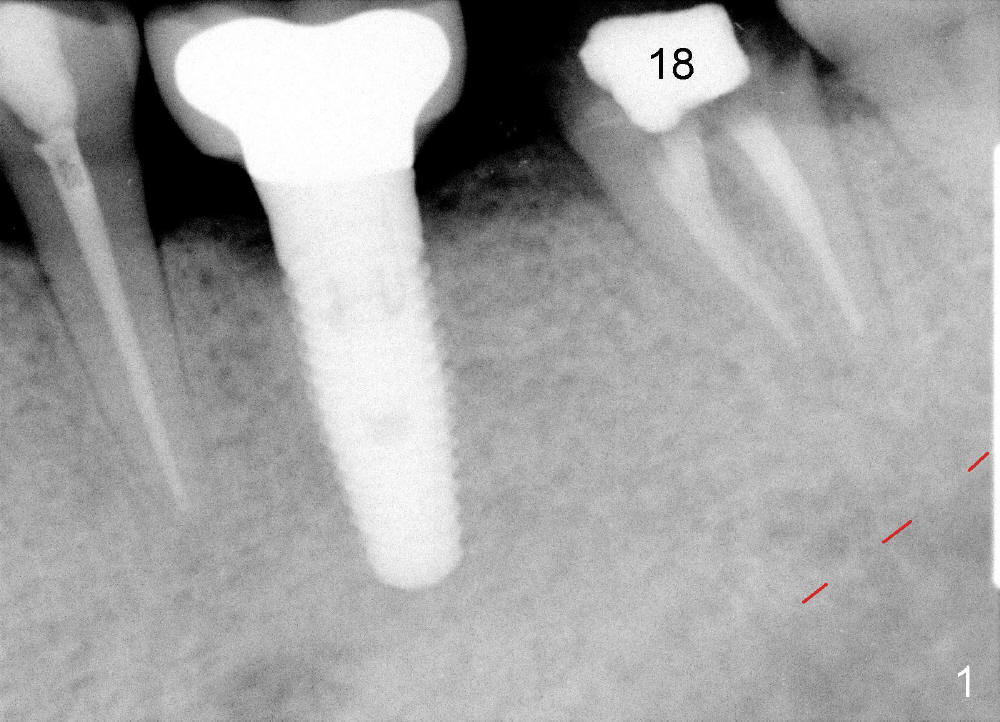
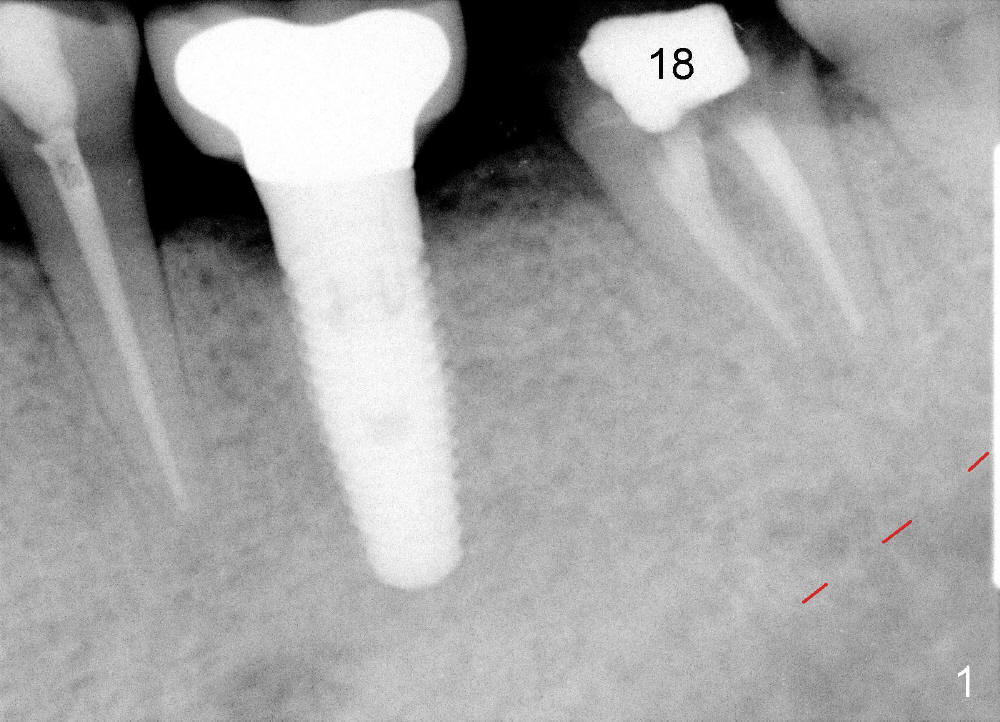
A 63-year-old man has lost a crown from the tooth #18 (Fig.1), which is tender to percussion. The margin is subgingival.
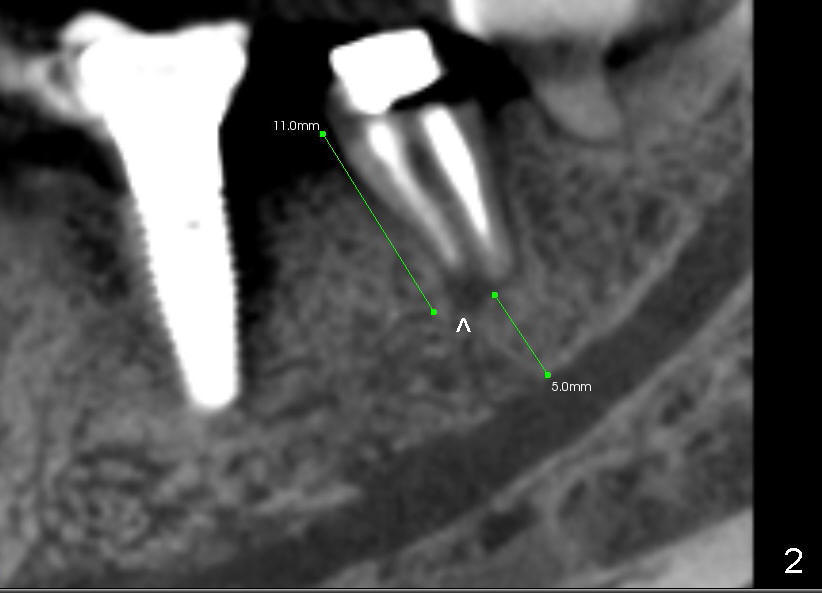
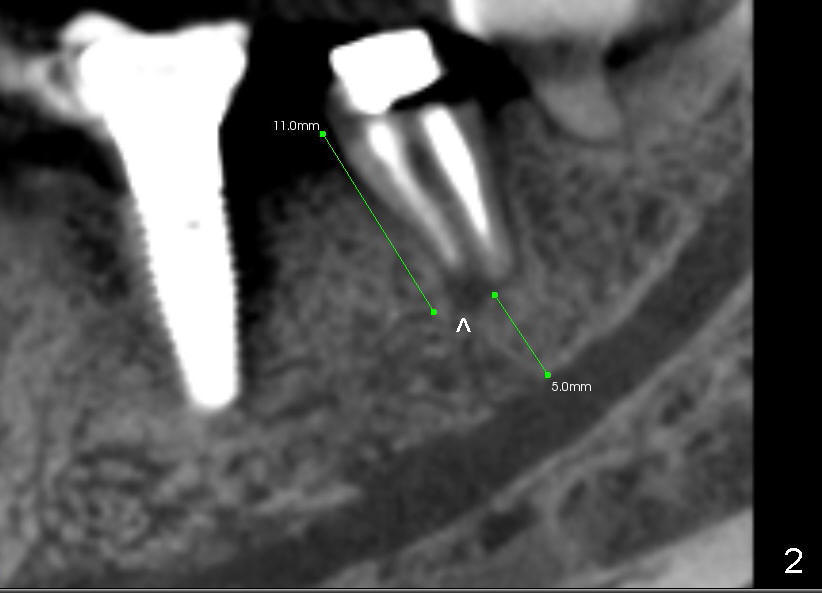
CBCT reveals periapical radiolucency (Fig.2 ^). The tooth appears to be nonsalvageable. The root is 11 mm long. There is 5 mm bone between the fused apex and the inferior alveolar nerve. The prospective implant is going to engage 3 mm out of the 5 mm native bone for primary stability.
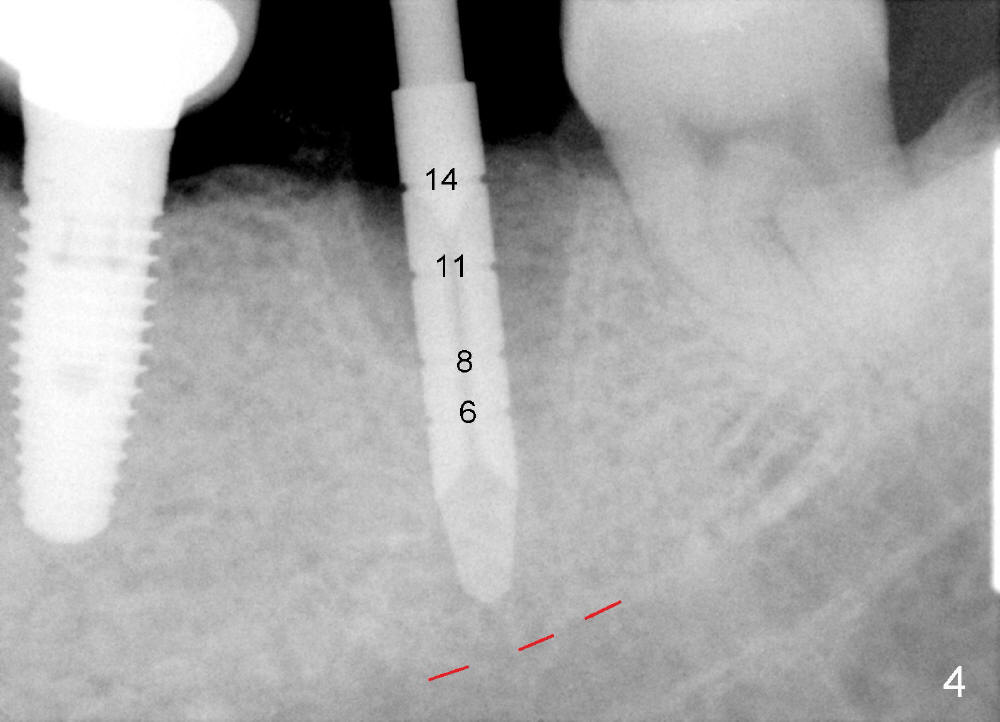
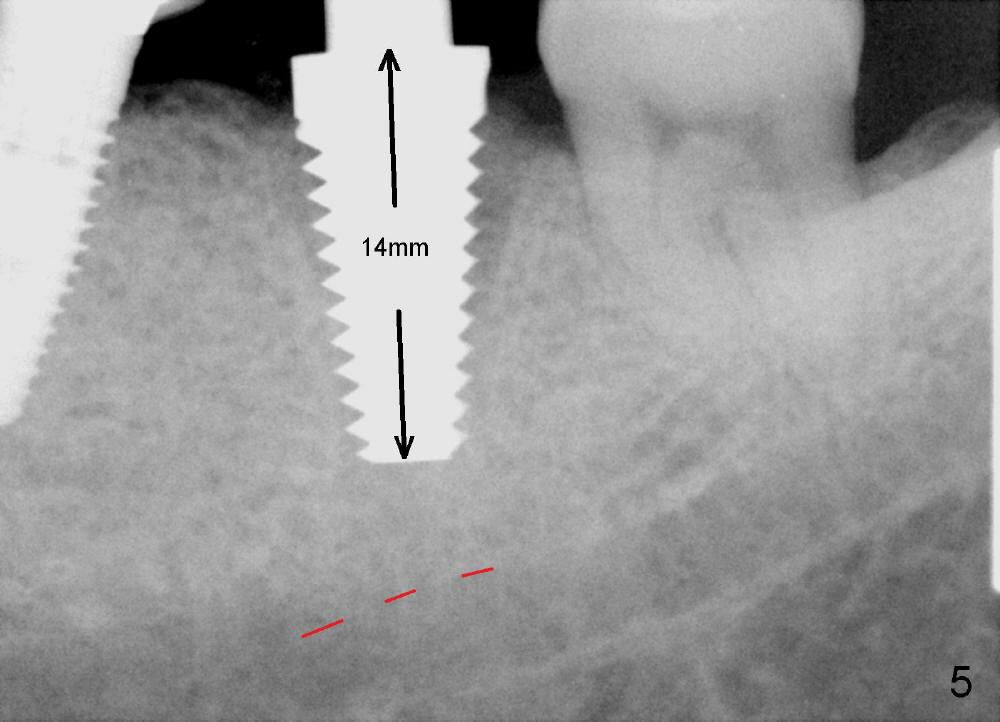
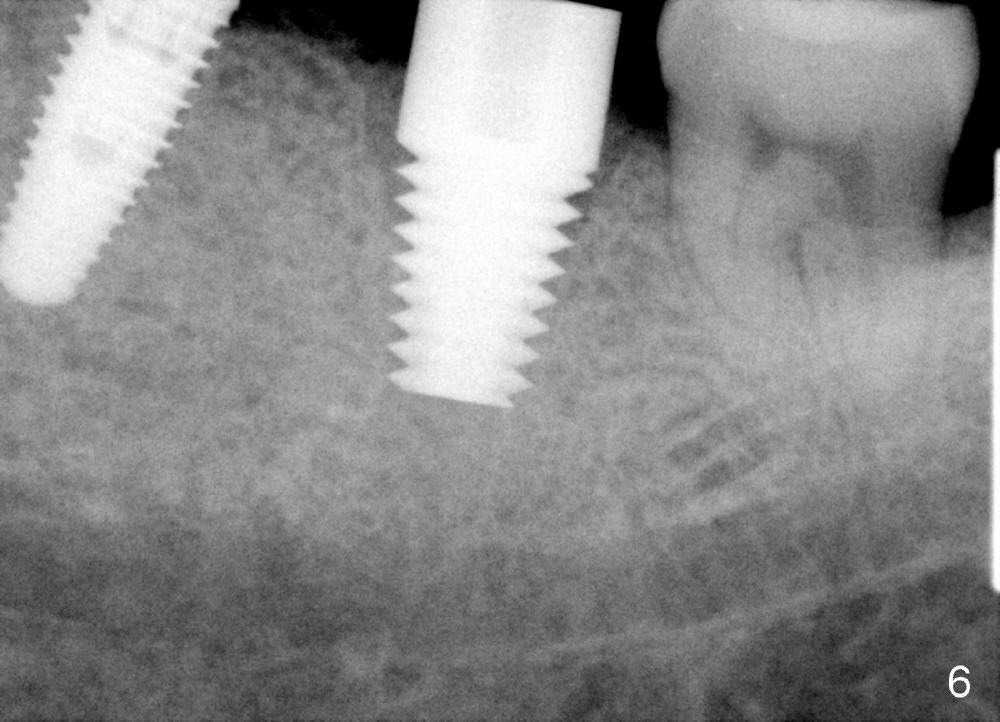
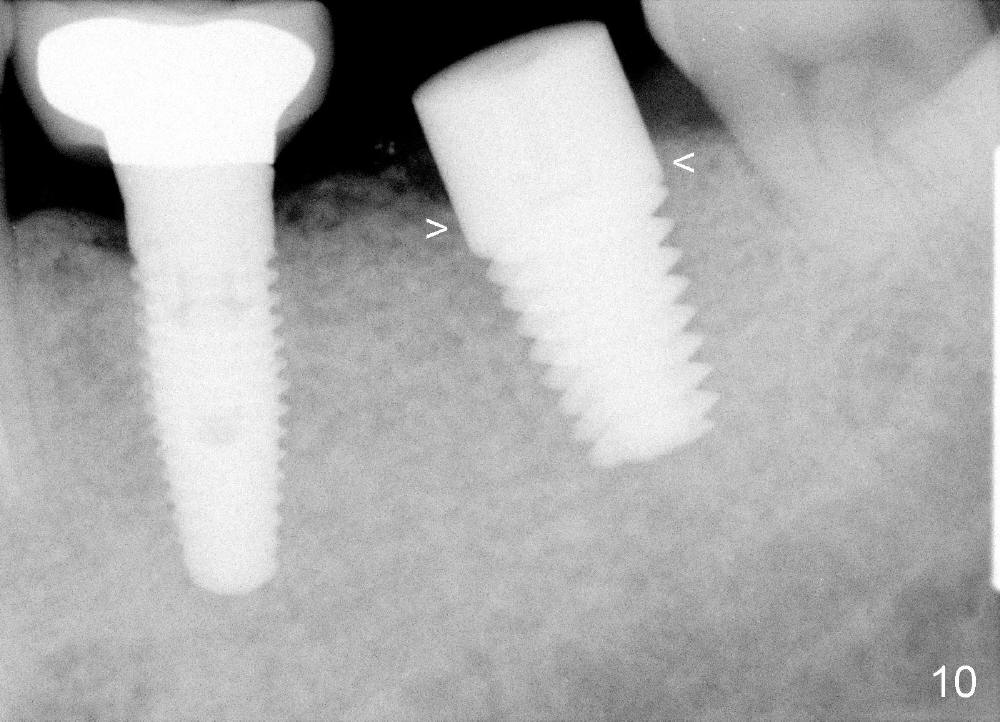
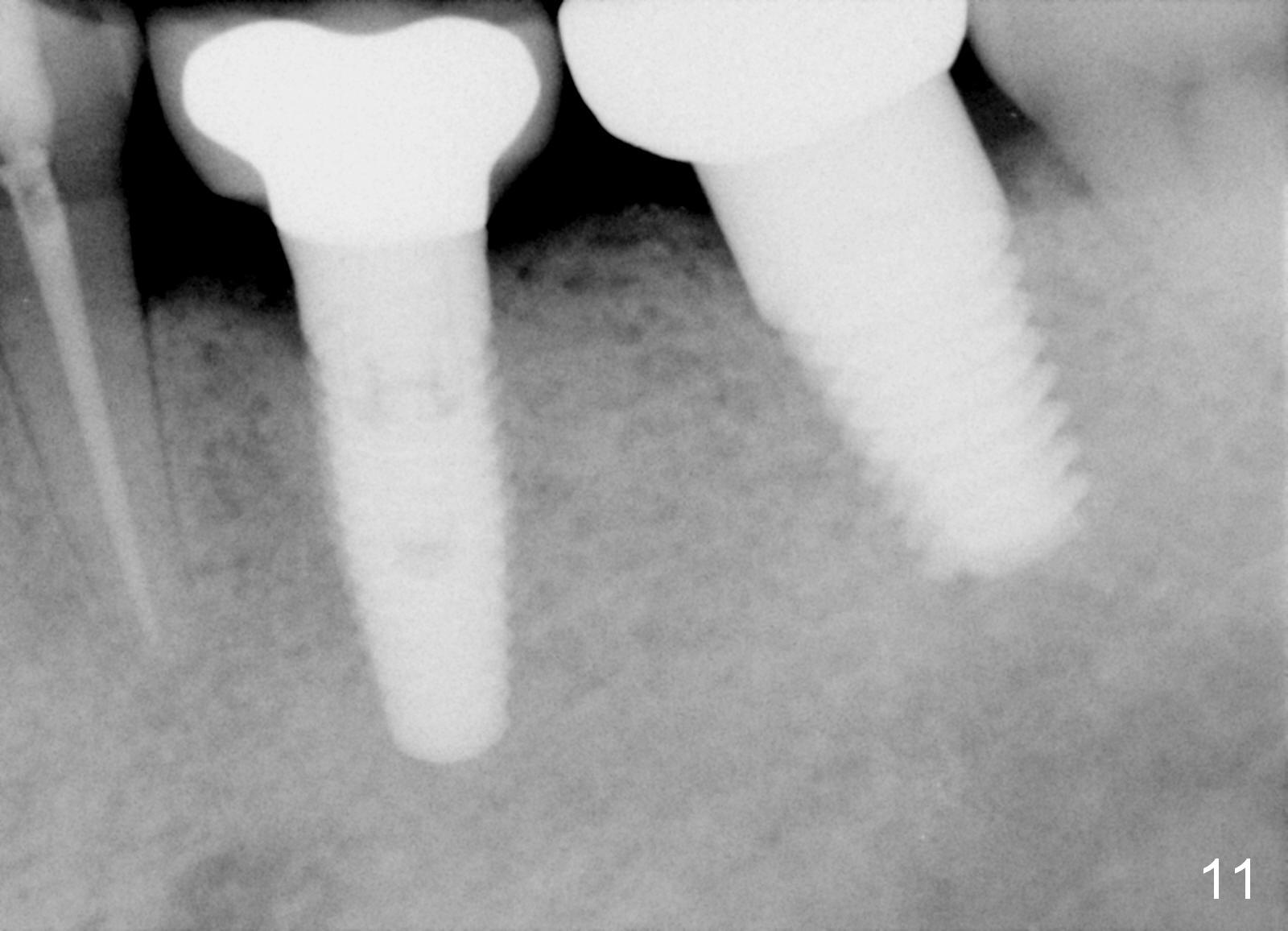
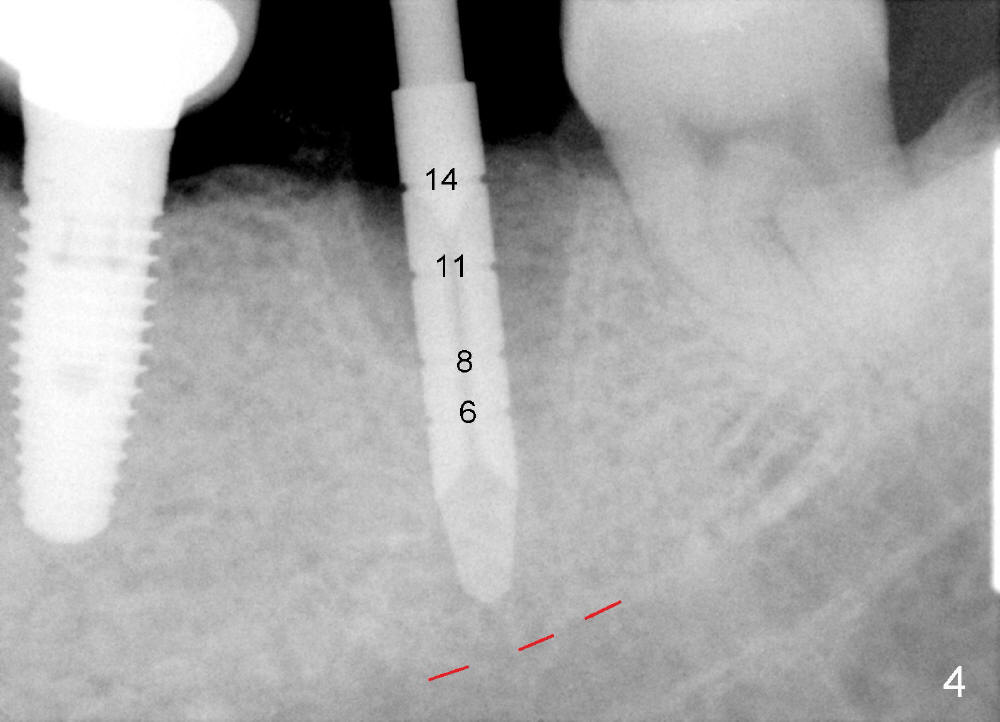
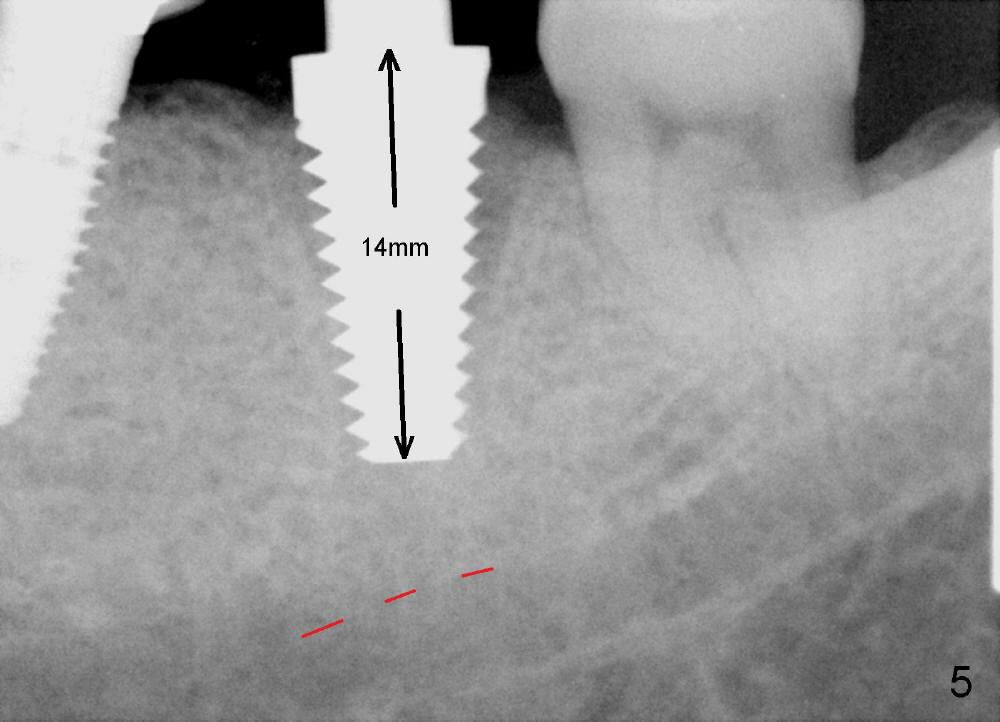
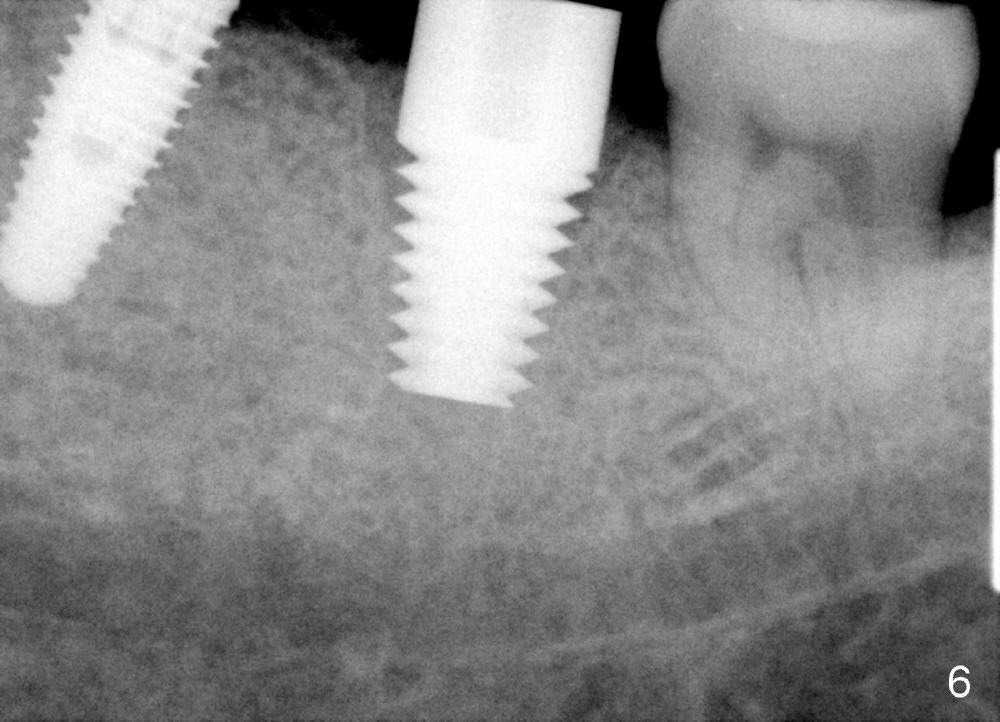
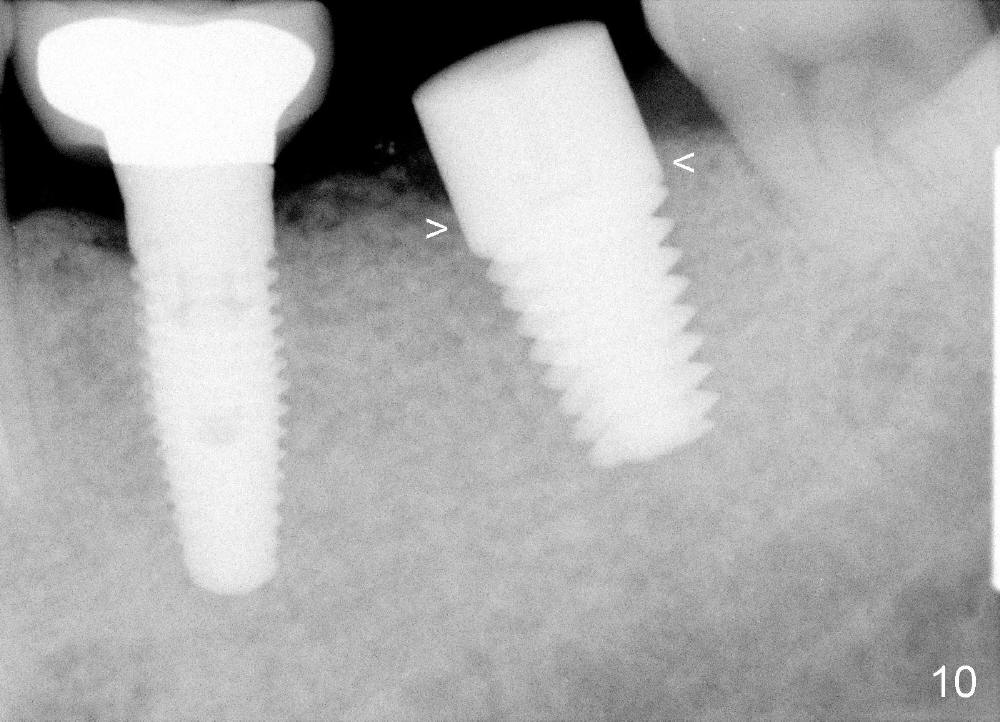
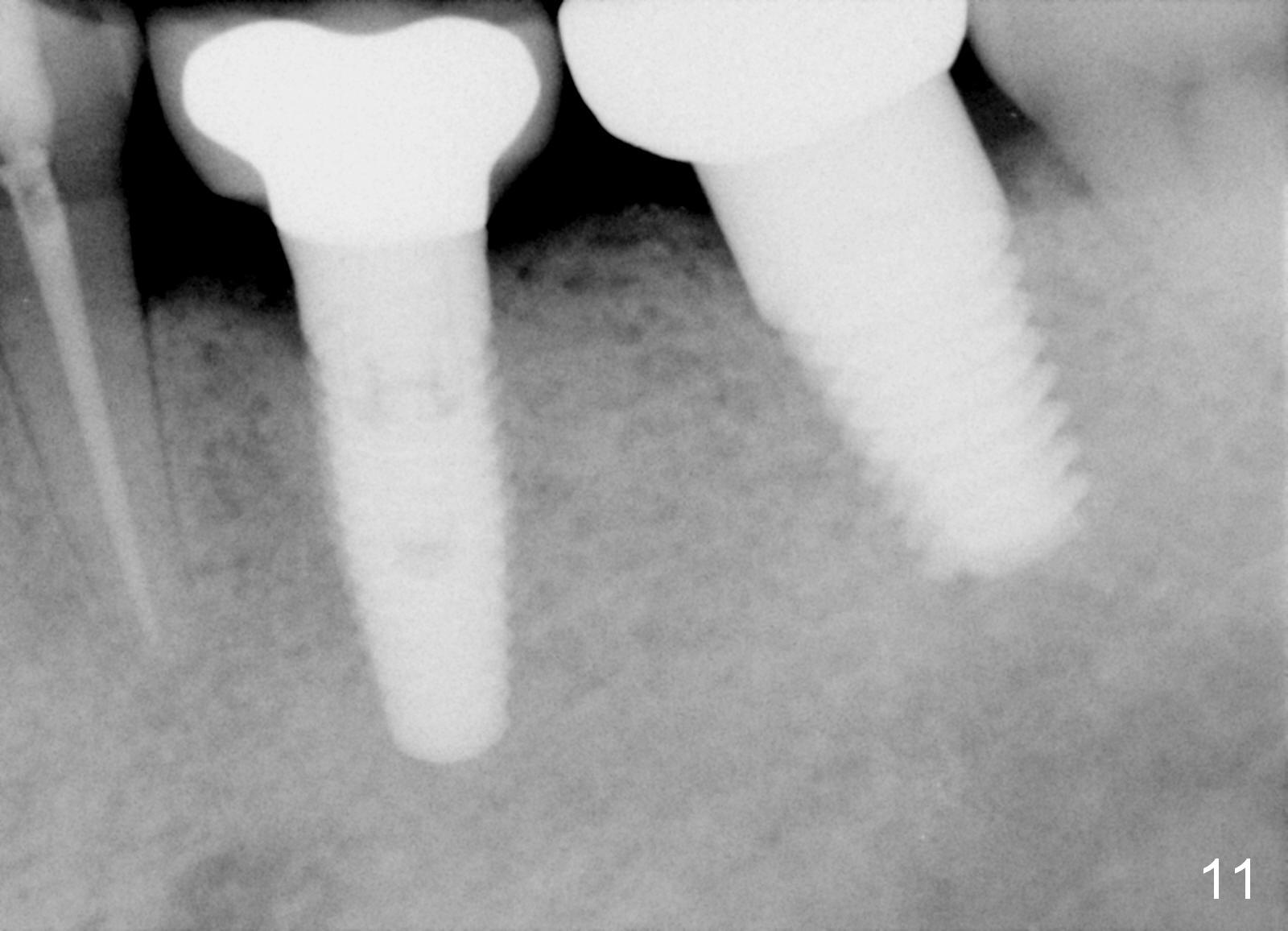
The septum of the socket is thin (Fig.3*), and easily removed, leaving a large socket. Osteotomy is initiated with 2 mm pilot drill in the middle of the socket, slightly mesiolingual, since the buccal and distal bone is low and defective. Reamers (2.5 to 4 mm in diameter) are sequentially used to enlarge osteotomy and harvest autogenous bone (Fig.4 (3 mm reamer in place). When 5 mm tap is placed, there is no stability. Six mm tap gains some stability, but the socket is not closed. Seven mm tap achieves strong stability and is closing the socket (Fig.5). Ultimately a 7x14 mm implant is placed with insertion torque more than 60 Ncm (Fig.6). The implant almost obliterates the socket (Fig.7). The harvested autogenous bone is placed in the buccal and distal aspects of the socket before Chromic gut suture (4-0) is placed distally. Fig.8,9 show the healing socket 6 days and 1.5 months postop, respectively. Osteointegration appears to occur in 2.5 months (Fig.10, compare to Fig.6). Bone level remains the same 1 year post cementation (Fig.11).
In brief, a large implant is placed in a single socket of the lower 2nd molar for primary stability and better restoration. To place an immediate implant in the middle of a lower molar socket requires knowledge of local anatomy. His bone density is high, which also helps implant placement at healed sites.
Return to Lower Molar Immediate Implant
Xin Wei, DDS, PhD, MS 1st edition 01/28/2014, last revision 01/19/2018