


 |
 |
 |
 |
 |
 |
 |
 |
Where Should the Implant be Placed?
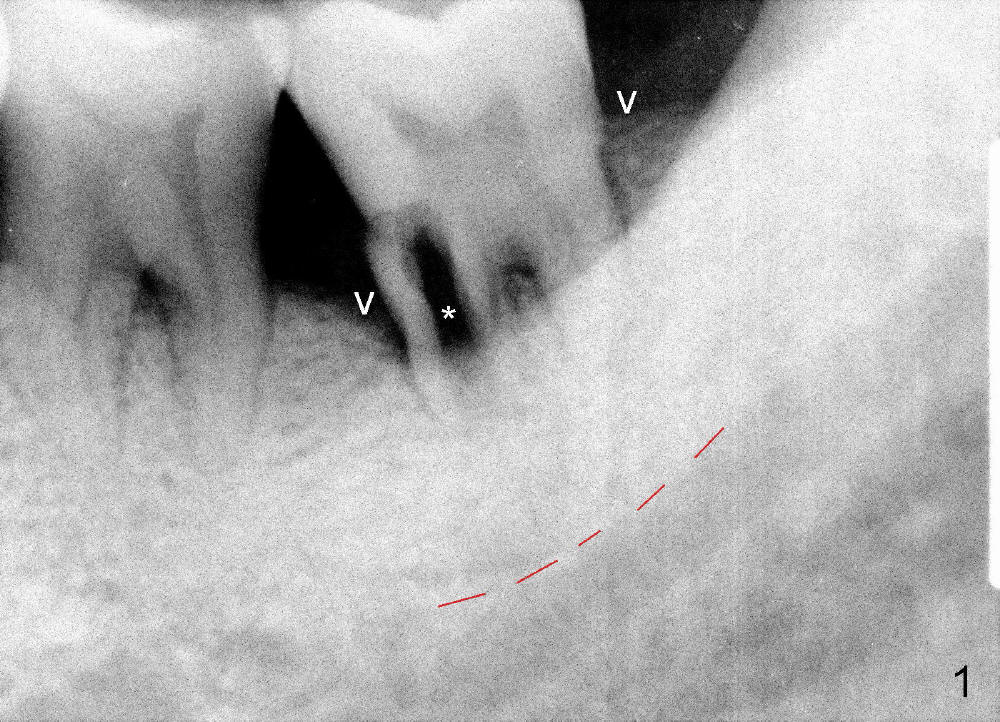
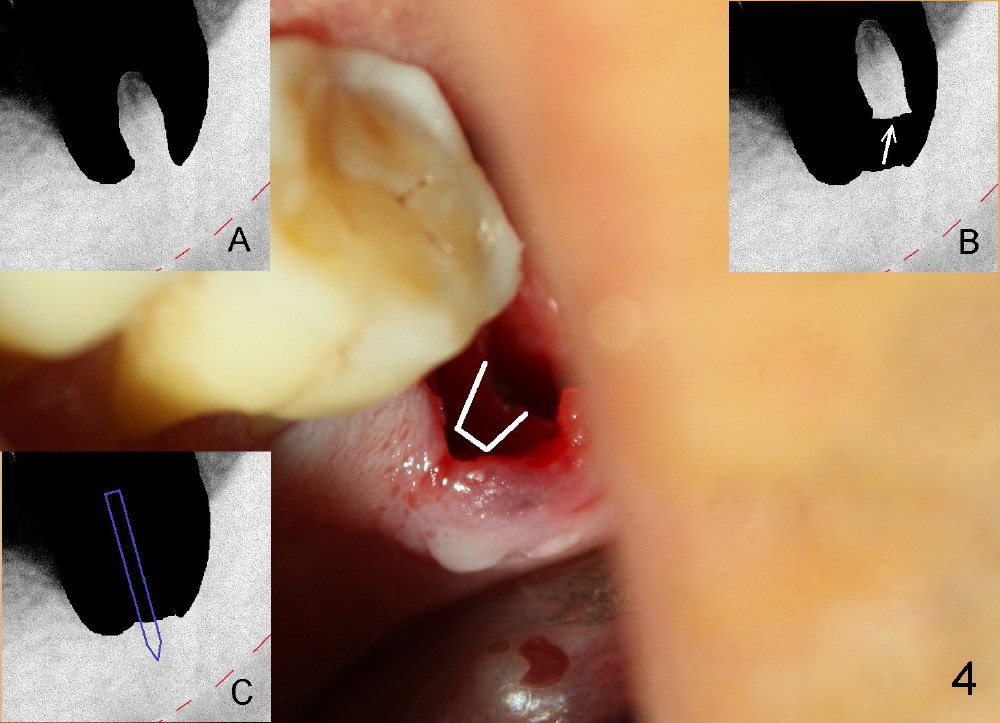
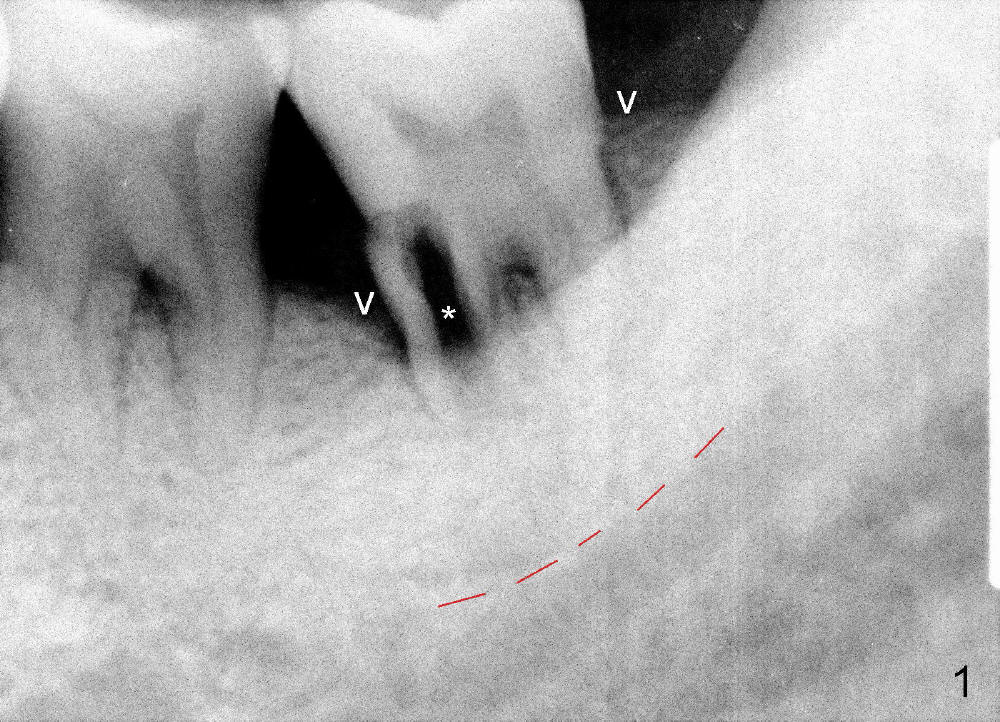
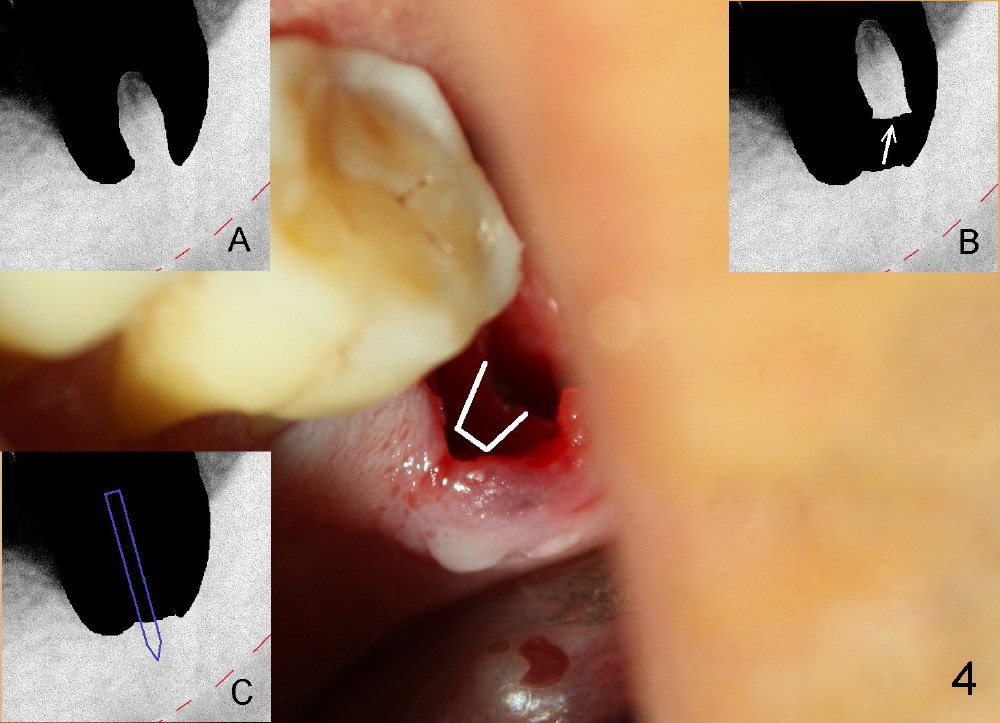
A 51-year-old man has generalized chronic periodontitis. The mesial root of #18 has vertical fracture (Fig.1*) with infection. The patient agrees extraction (Fig.2) and immediate implant. The septum is thin. The pilot drill drops into either the mesial (Fig.3) or distal sockets. Furthermore it is difficult to control pain probably due to severe infection (Fig.2 >: mesiobuccal erythema and edema). Repeated local infiltration does not alleviate pain associated with drilling. Block anesthesia has to be administered (one carpule of 2% Lidocaine with 1:100,000 Epinephrine). Damage to the inferior alveolar nerve (Fig.1 red dashed line) increases. On the other hand, osteotomy through the socket of the tooth with periodontits is easier because of shallow socket. Retraction of the buccal gingiva can reveal the bottom of the socket. We will increase the depth slowly until a tap obtains initial stability. The worst scenario is that active hemorrhage from the socket bottom is encountered initially. The nerve injury can be reduced minimally.
Now where to initiate osteotomy? Since the mesial crest is much lower than the distal (compare arrowheads in Fig.1), placement of an implant in the mesial socket is a good approach, whereas placement in the distal socket is not good for restoration (cantilever). The thin septum is slippery to drill penetration. What should we do?
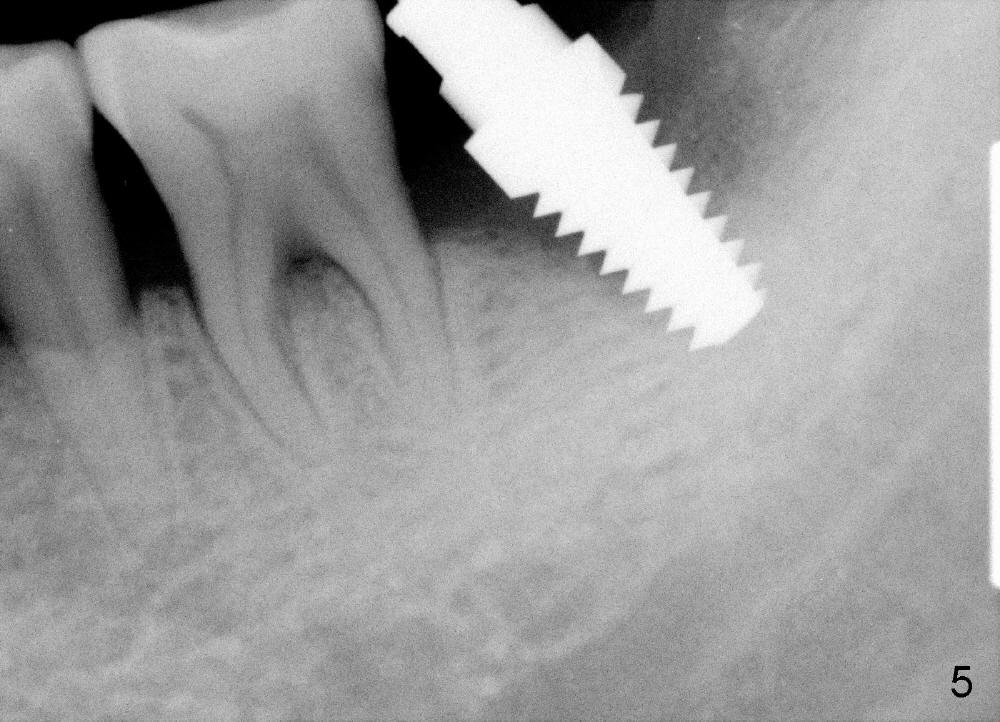
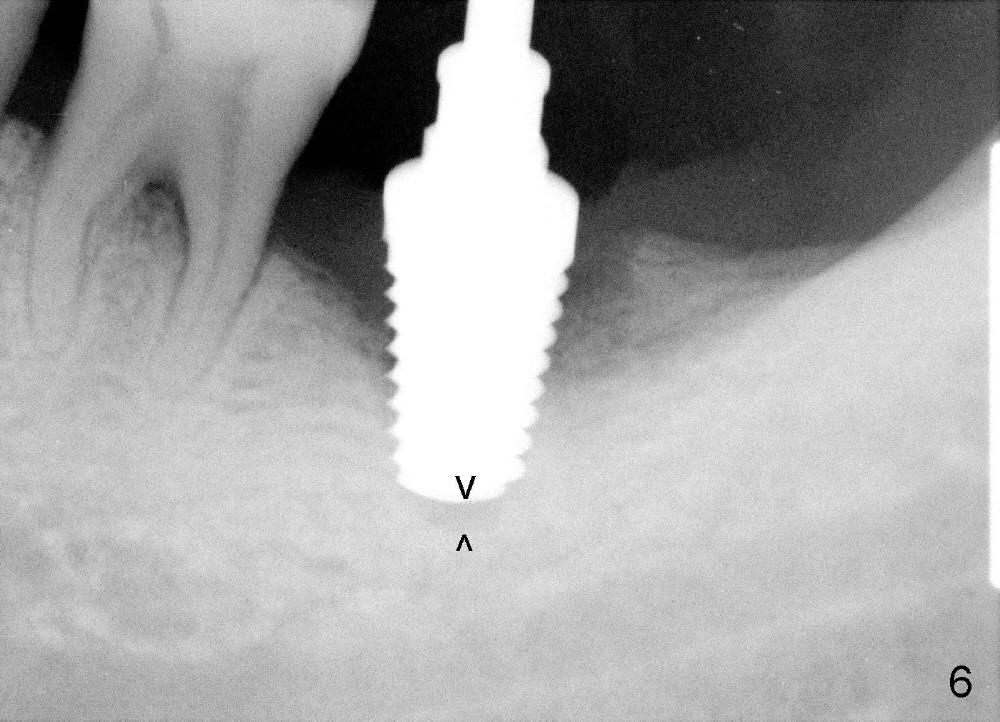
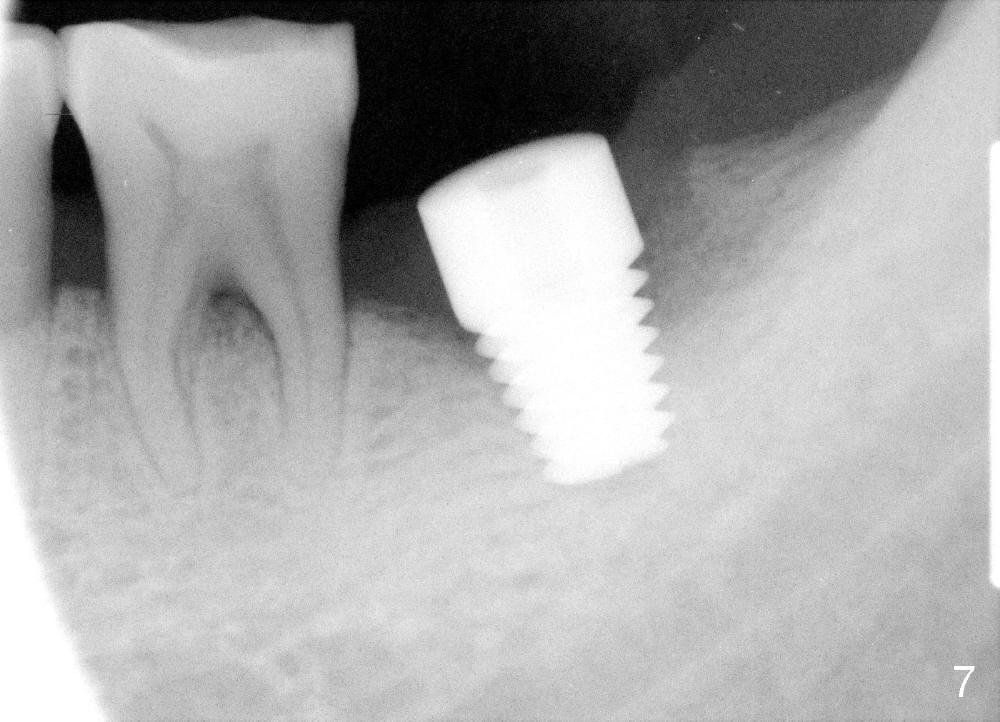
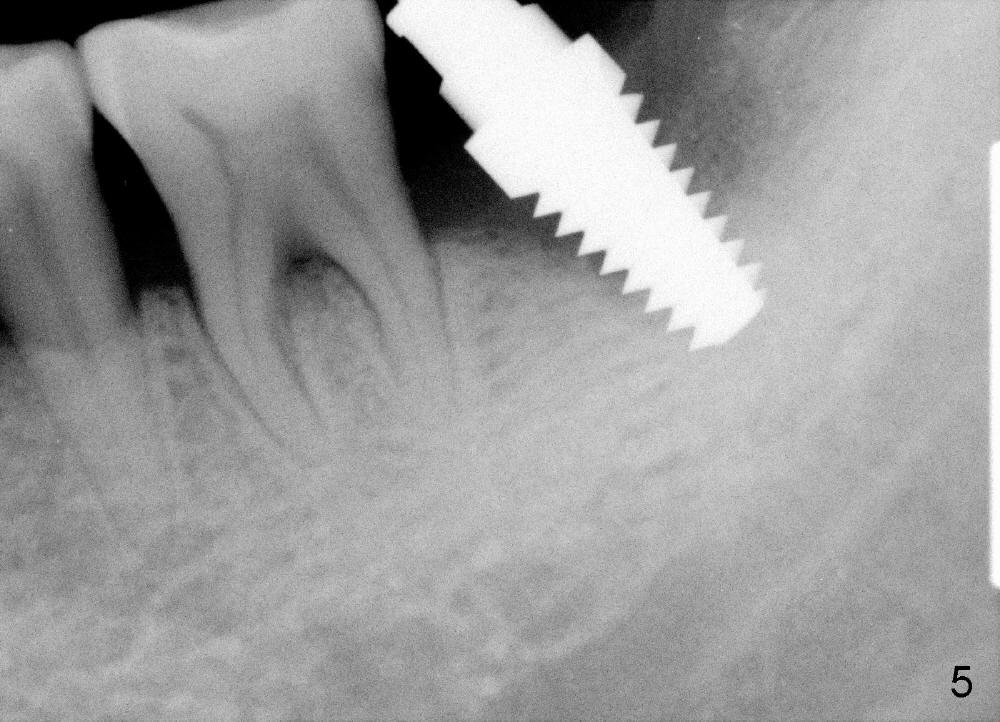
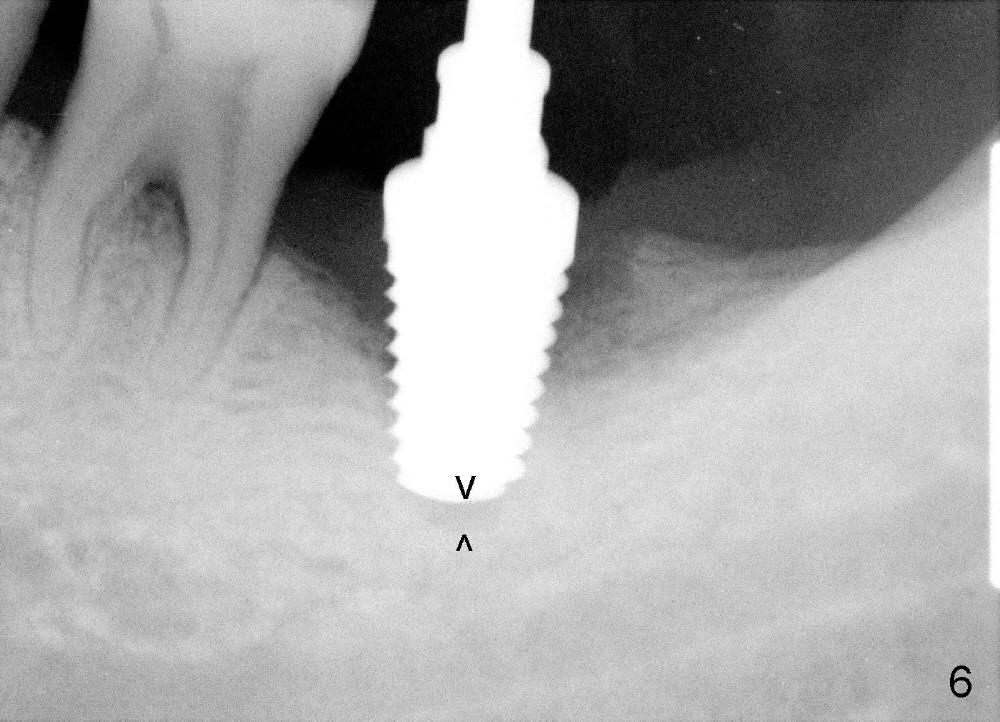
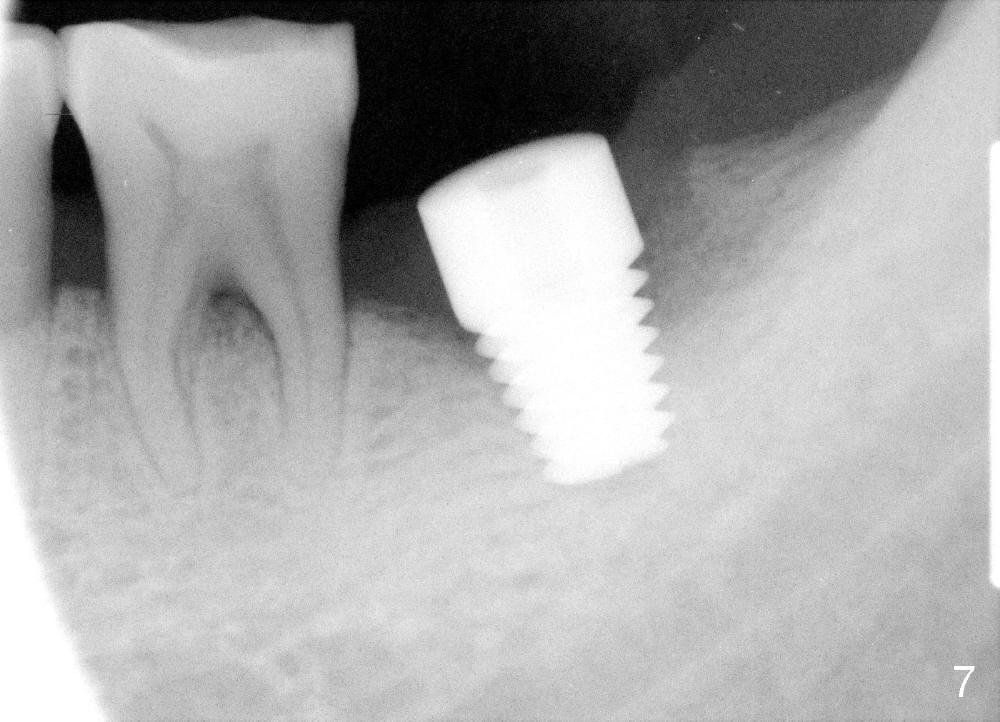
How about flatten the septum (Fig.4 white lines; from inset A (post extraction) to B)? When the septum is level with the mesial and distal sockets, a drill easily penetrates the middle of the socket (Fig.3 inset C). With strict control of depth, the osteotomy increases until a 6x14 mm tap gets initial binding to the socket (Fig.5: depth 11 mm). After increase in the depth by 1-2 mm, PA is taken with a 7x14 mm tap (Fig.6). There is a gap that the tap or the corresponding implant can engage further (between arrowheads). After increase in the diameter in the bottom of the osteotomy, a 7x11 mm implant is placed with insertion torque between 45 and 50 Ncm; the threads of the implant have tight contact with the bone (Fig.7). With the large diameter implant, the socket opening is closed without too much tension (Fig.8). The wound is protected with perio dressing. Postop there is no paresthesia. Pain is controlled by Hydrocodon/Acetaminophen. A long acting local anesthetic (Marcaine) should have been used immediately postop. Next morning, the patient is pain free. A short implant should be used in a critical area such as the lower 2nd molar where the inferior alveolar nerve is nearby. However, the implant is found unstable 1 month postop.
Xin Wei, DDS, PhD, MS 1st edition 02/12/2014, last revision 02/16/2018