










 |
 |
 |
 |
 |
|
 |
 |
 |
 |
||
 |
 |
 |
|||
Which First, Bone Graft or Immediate Implant?
A 84-year-old man has severe pain distal to #18 (Fig.1). The affected tooth is planned to be restored by a 7x17 mm implant (Fig.2).
When the tooth is extracted, the socket is extremely large. The largest tapered tap (8x17 mm) basically drops into the socket; it is not stable in the socket (Fig.3). It appears necessary to engage into the nascent bone, which is 8.37 mm long.
The initial trajectory using 2 mm pilot drill is off (Fig.4), whereas the 2nd one is good (Fig.5).
When a 7x17mm tap is inserted, it is stable. There is distance to the inferior alveolar nerve (Fig.6: dashed line).
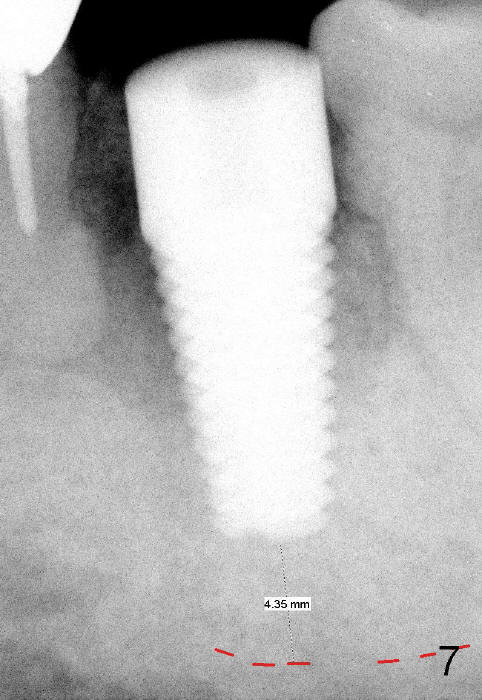
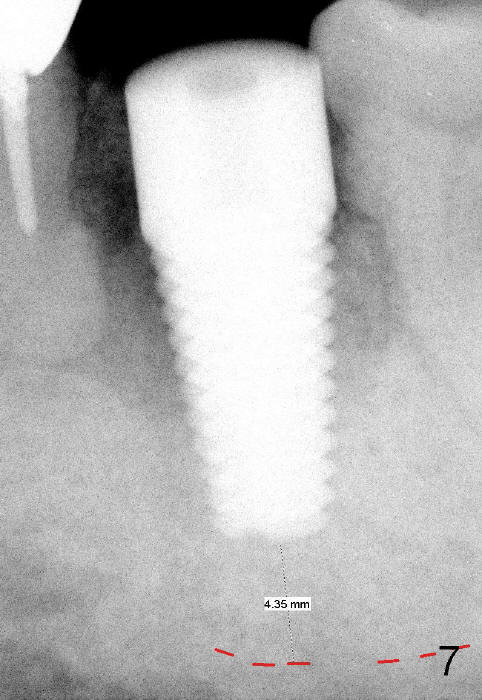
Prior to implant placement (Fig.7,9: 7x17 mm with insertion torque 40 Ncm), a mixture of autogenous bone (Fig.8 red particles) and demineralized cortical allograft (white granules) is packed against defective socket walls, particularly apically. It leaves a space in the middle of the socket for implant insertion later on. In this case, the buccal wall around the apex, corresponding to the fistula (Fig.9 >) is severely destroyed, whereas the crestal portion is more or less intact. Three months later, the implant appears yet to osteointegrate (Fig.10), while the fistula disappears (Fig.11). The large implant does not look too overengineered over the alveolus (Fig.12 (lingual view). In fact, the implant has mild mobility. How to fix it?
It is much more difficult to do bone grafting following implant placement due to limited space. Initially it is felt bone grafting first may interfere with implant placement due to blockage. If the graft is placed tightly against the defective wall, leave a space for implant, the placement is not so hard. Either way, membrane is not necessary.
Incision for bone grafting is not recommended. It compromises blood supply. There is a tendency to place too much bone graft once the wound is open. It may be difficult to close the wound because of tension.
Xin Wei, DDS, PhD, MS 1st edition 01/21/2014, last revision 01/19/2018