 |
 |
 |
 |
 |
 |
 |
|
Limited Clearance with Opposing Tooth
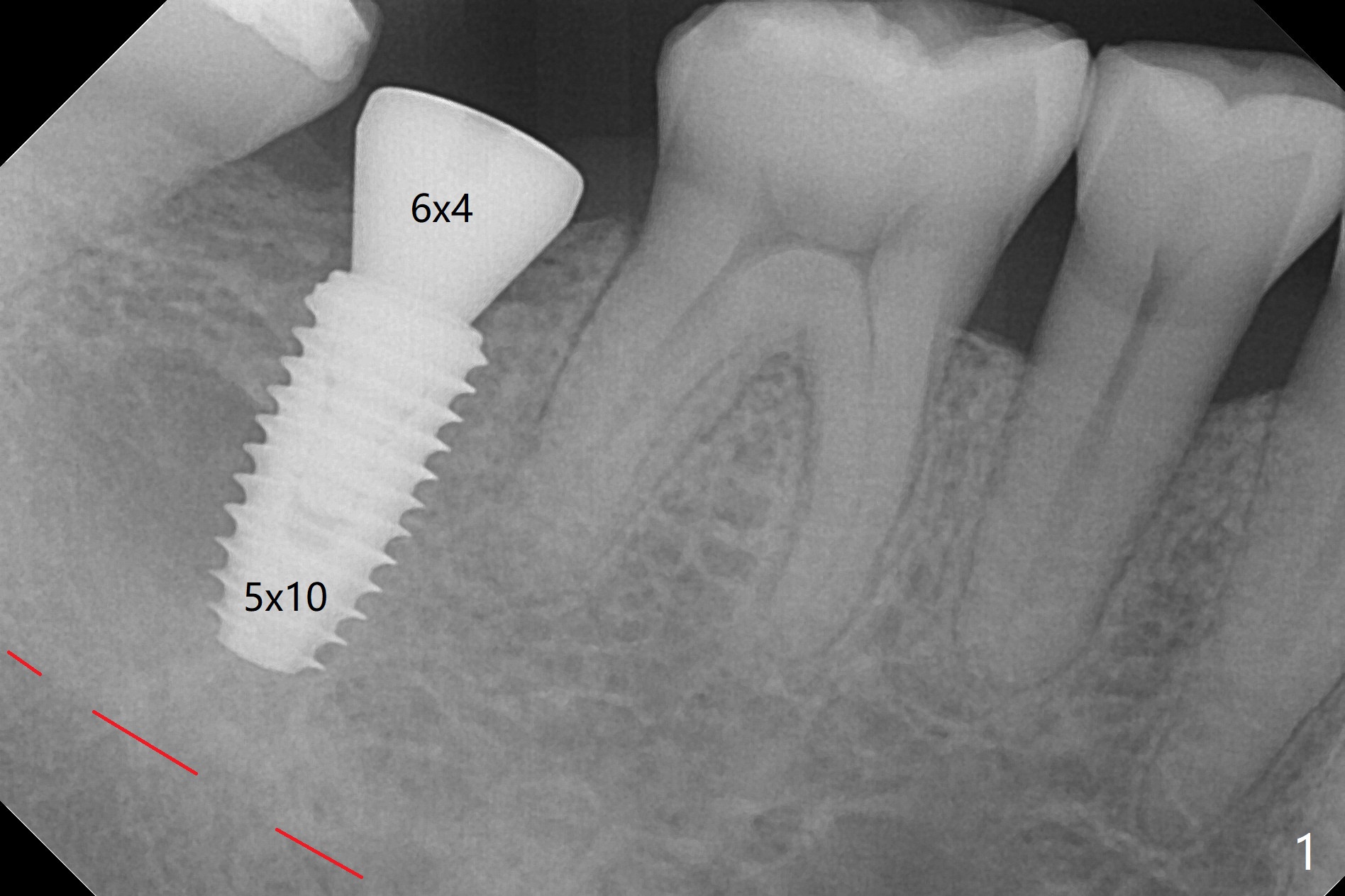
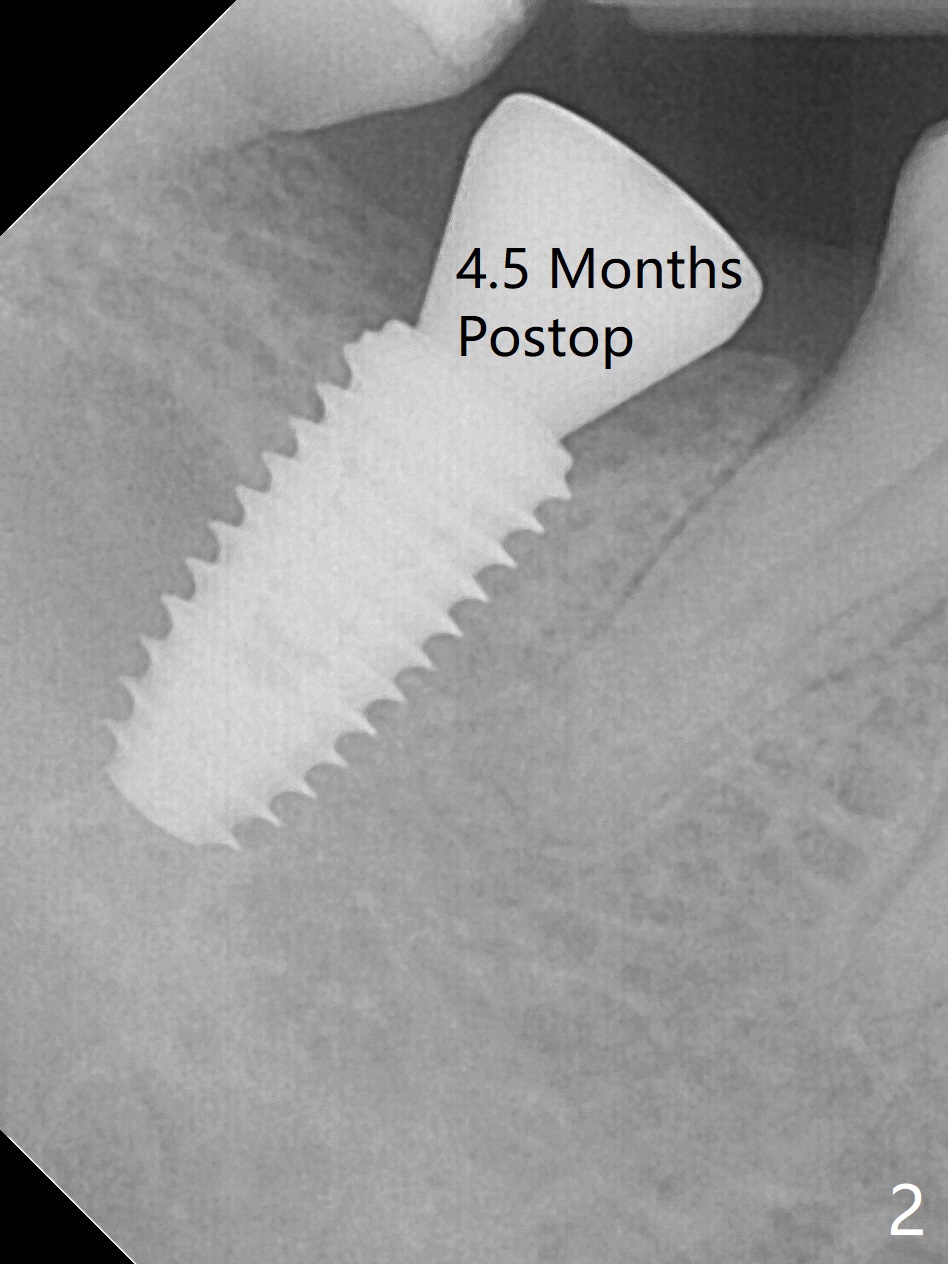
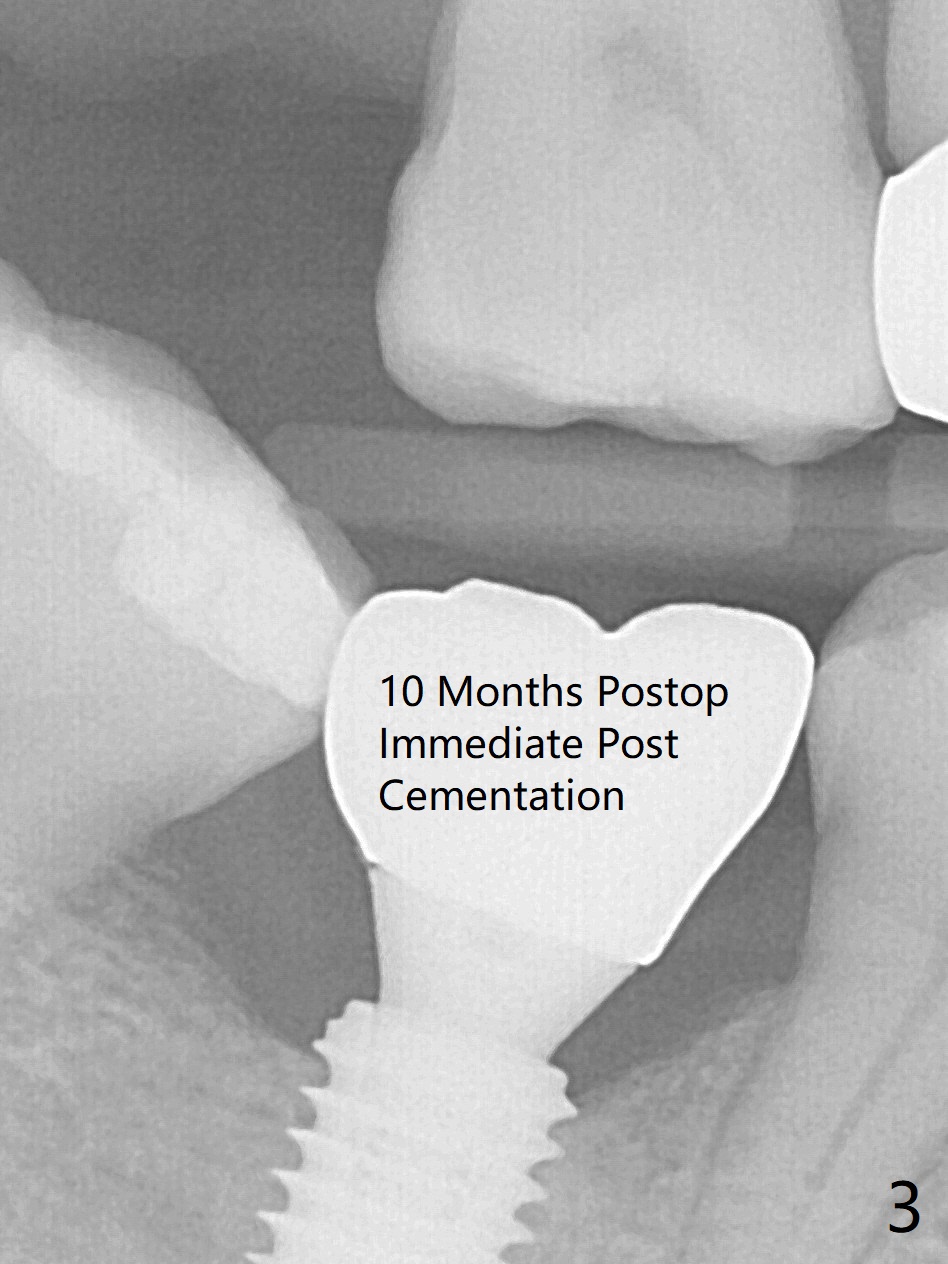
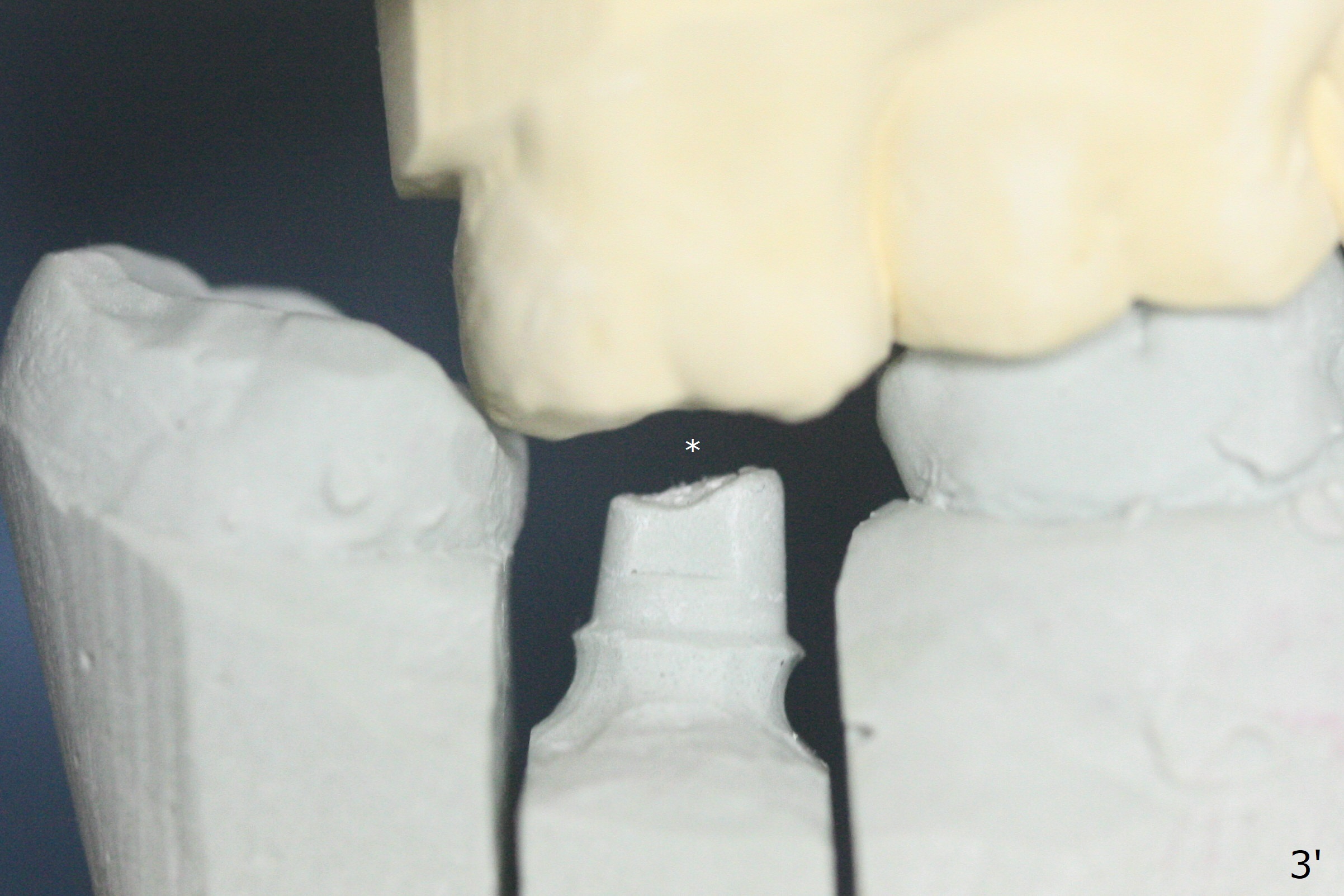
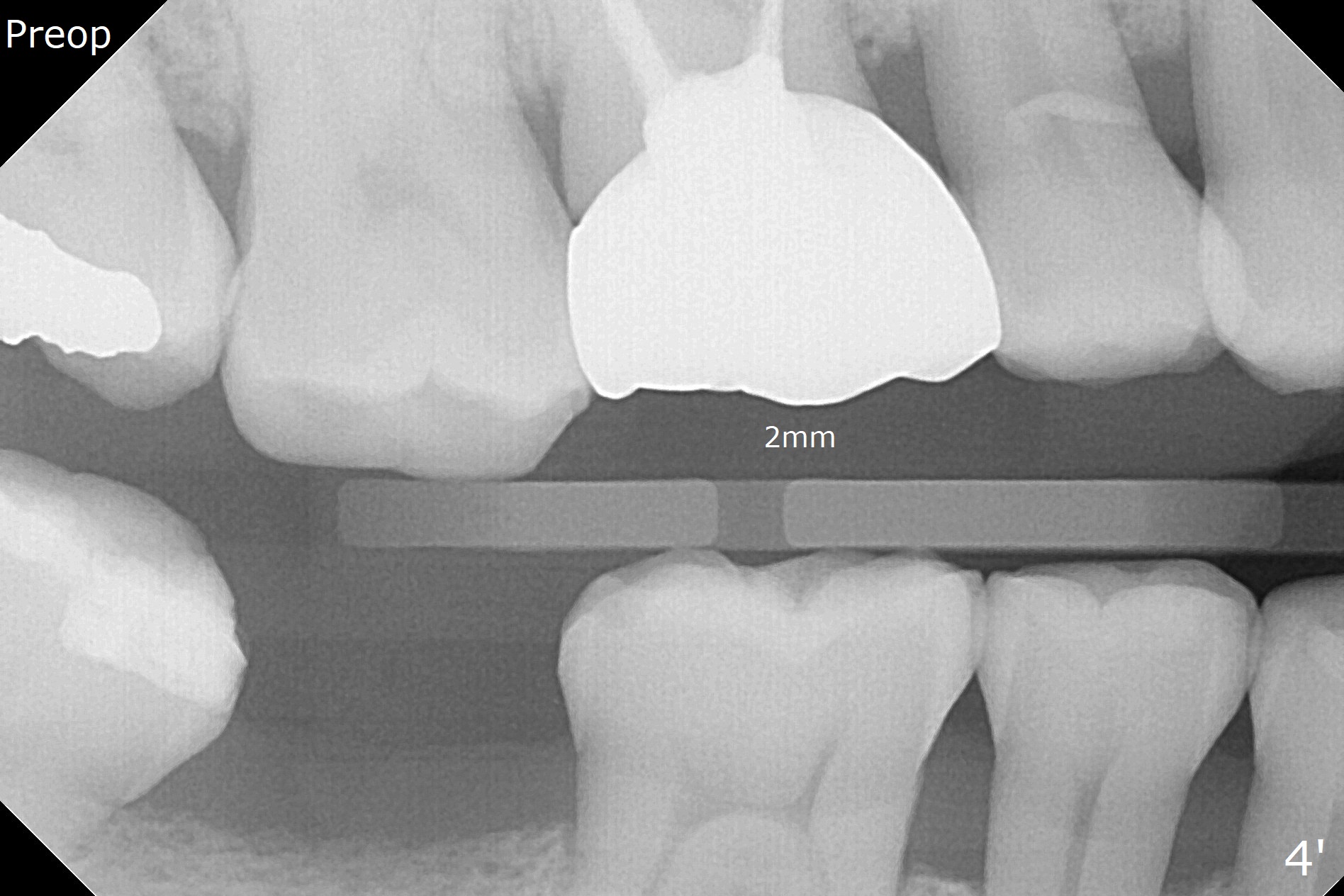
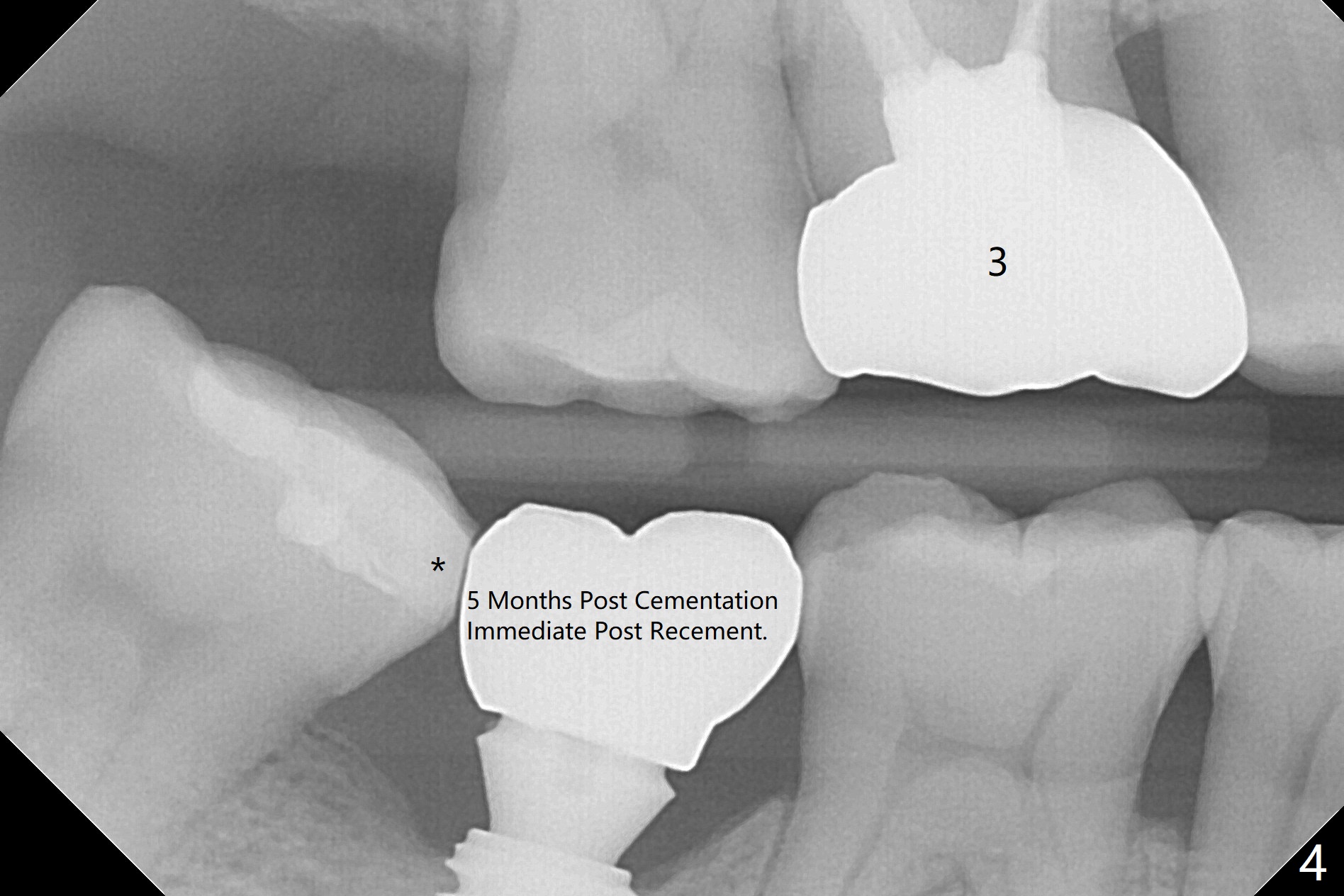
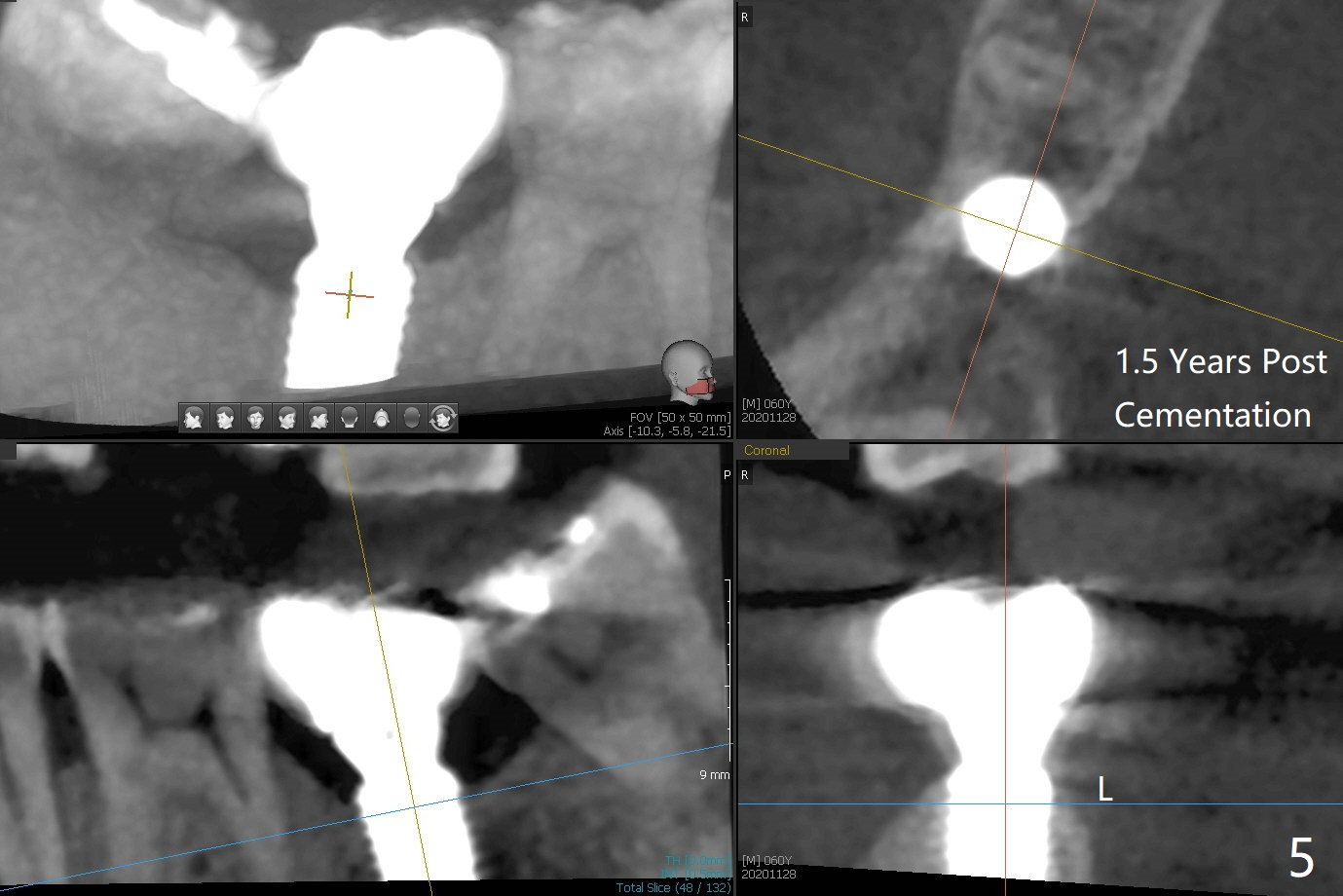
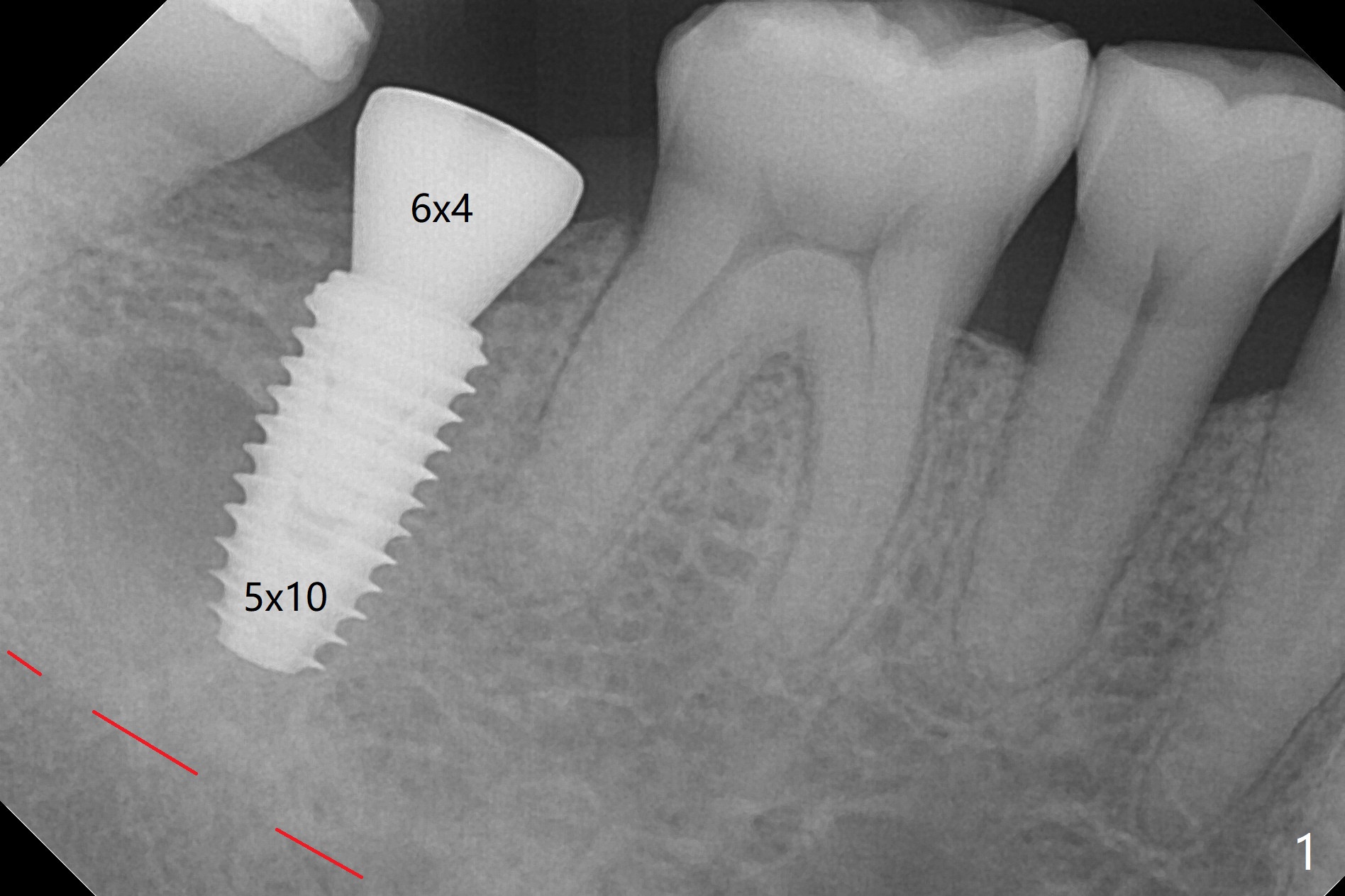
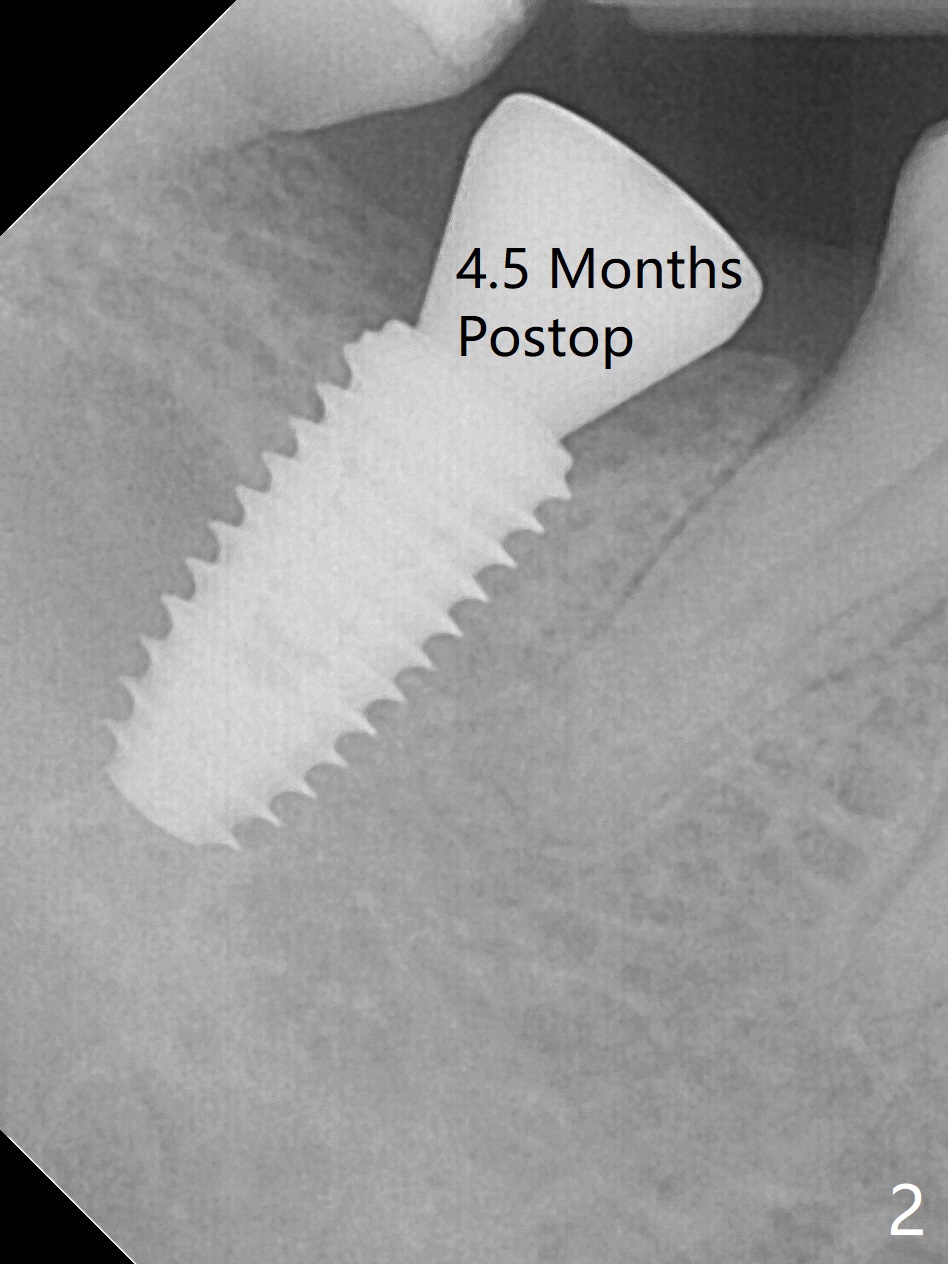
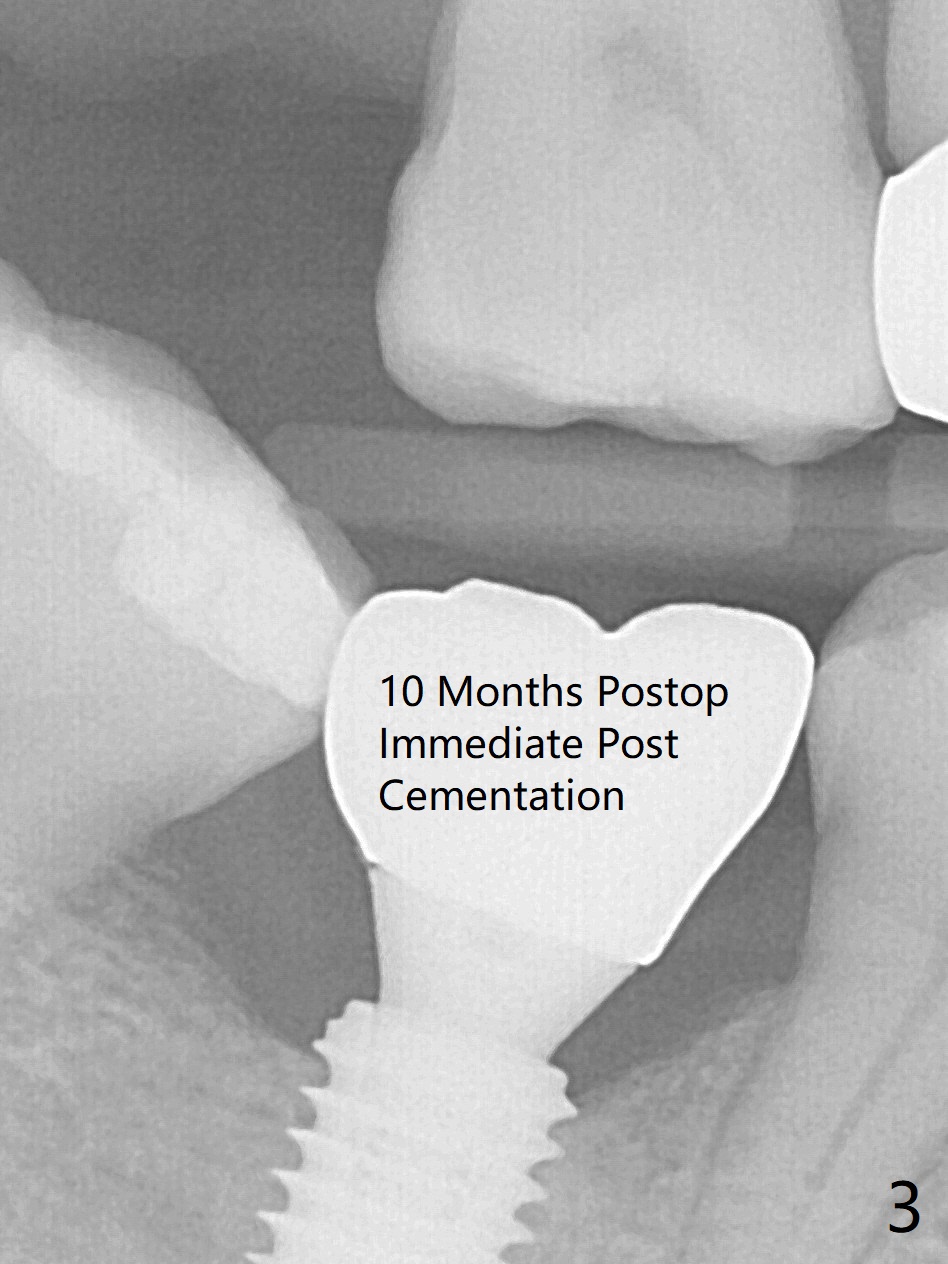
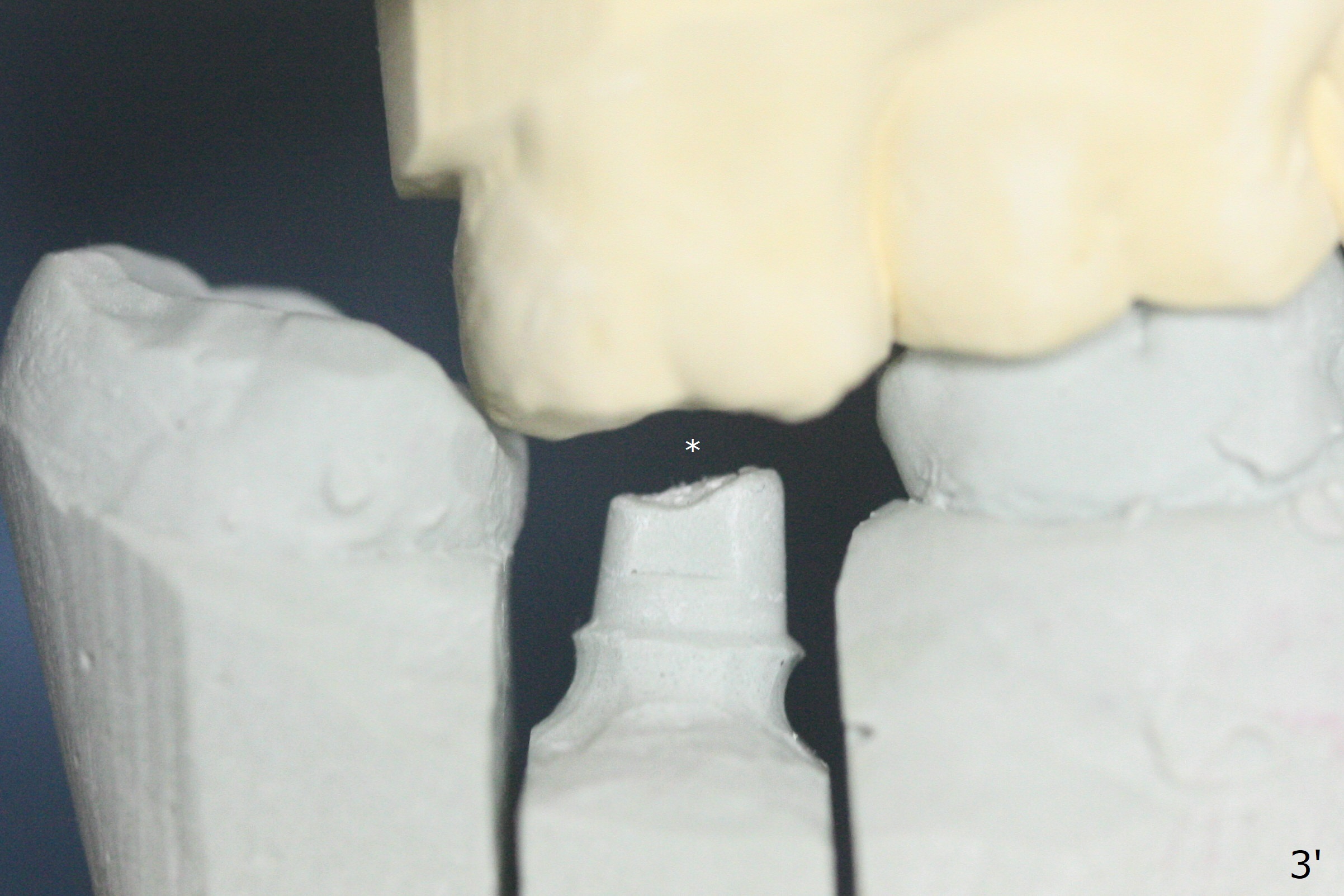
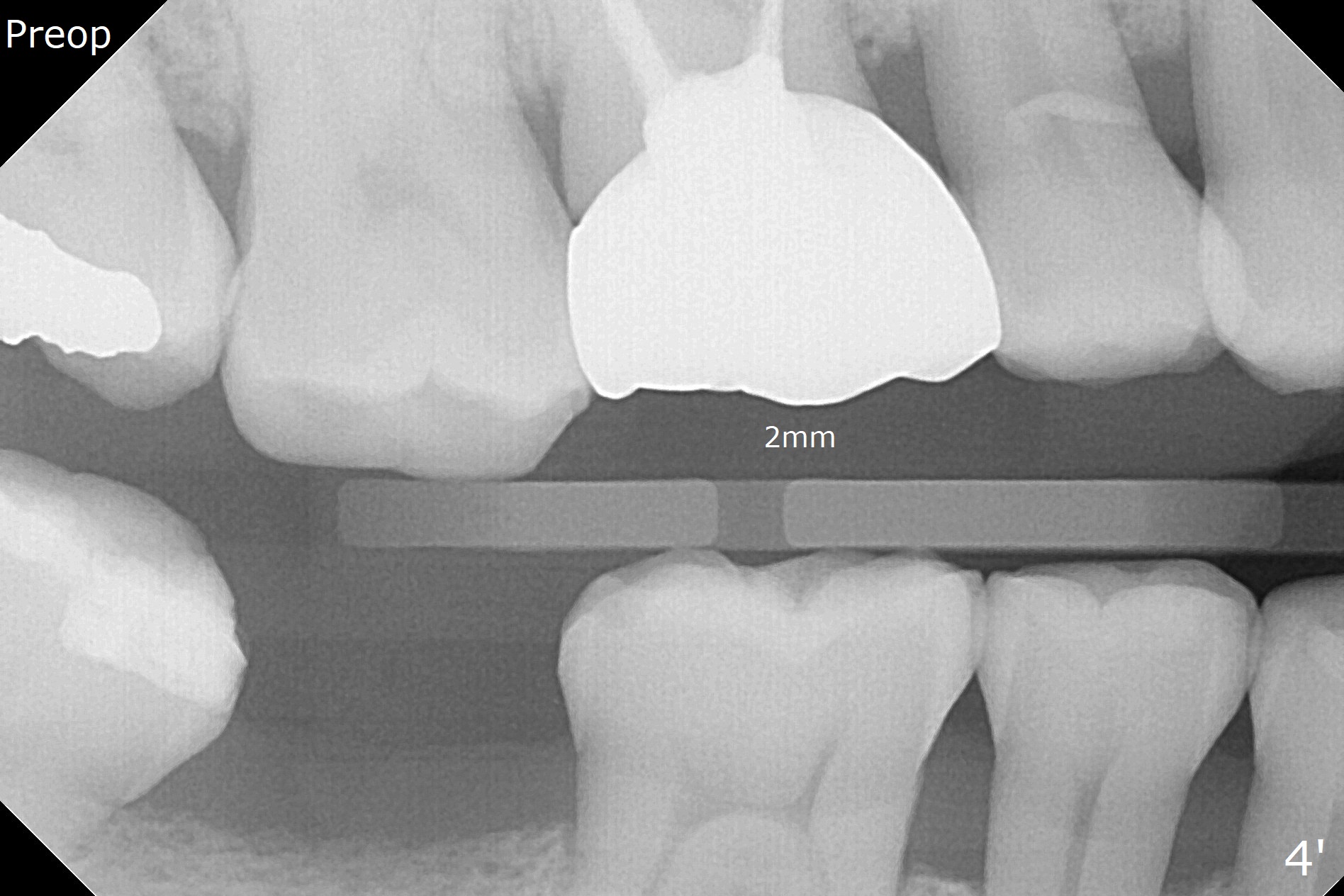
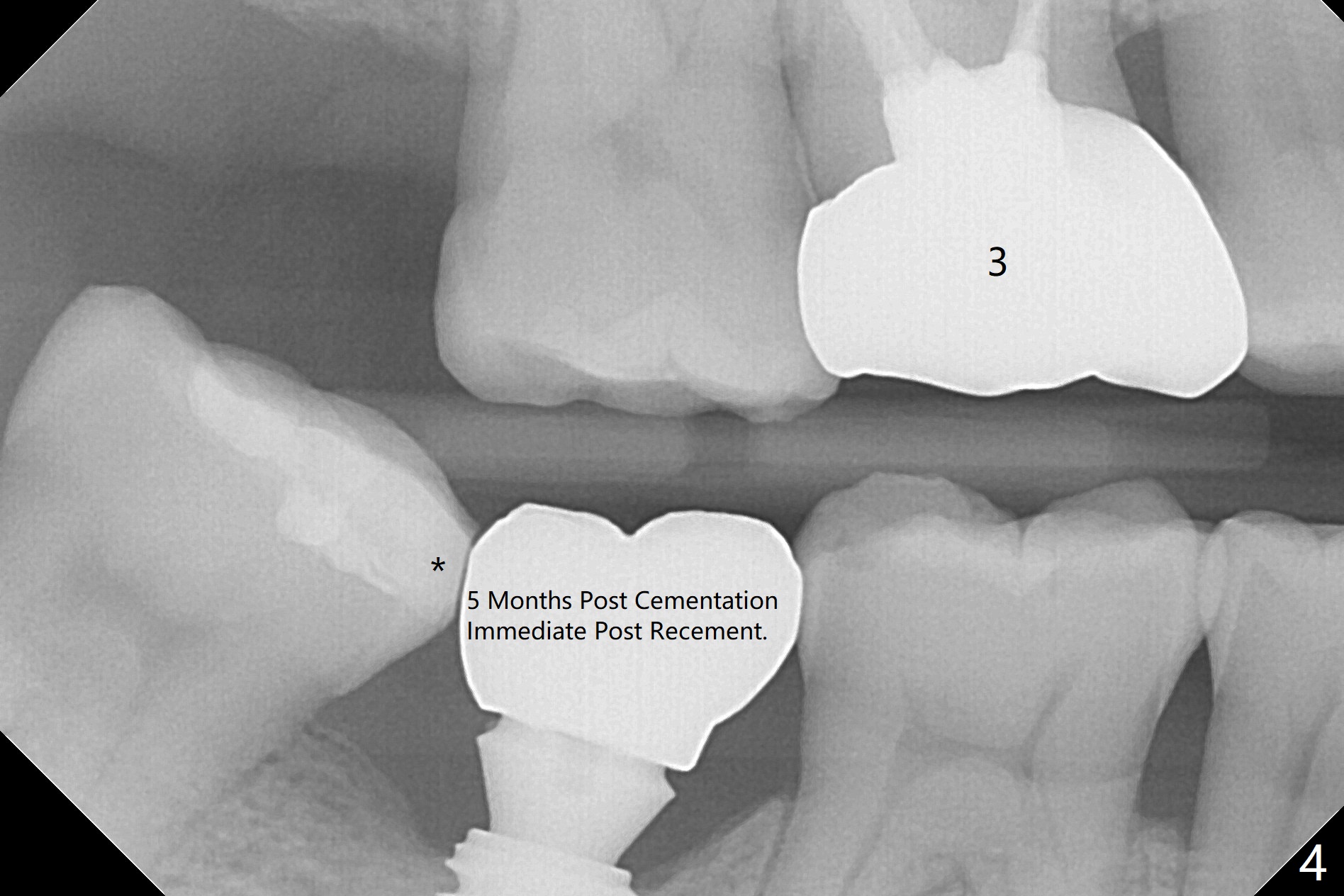
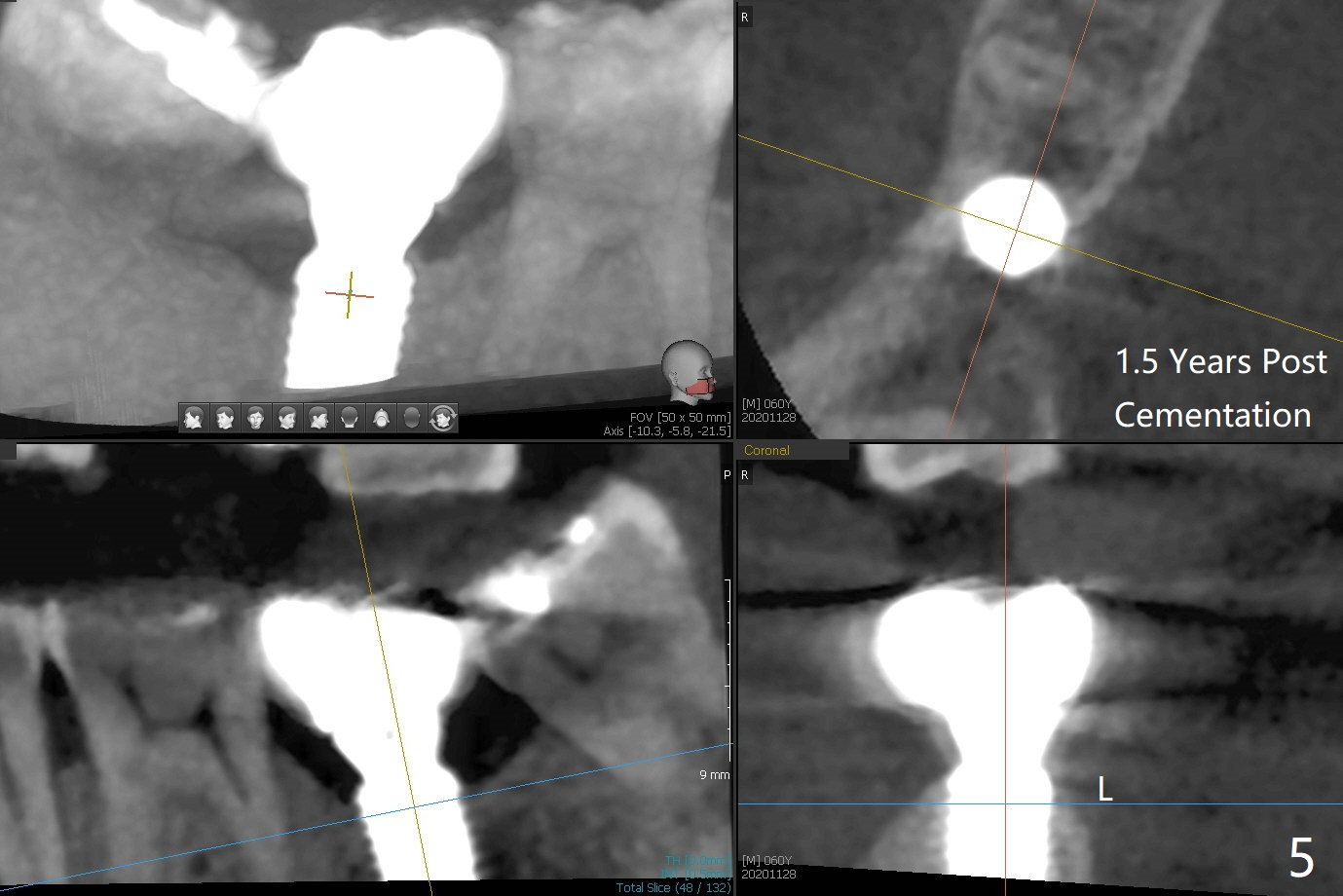
In fact 5x10 mm implant placement with guide requires using 5 mm cortical tap (Fig.1). When a 6x4 mm healing abutment is placed slightly supragingival, the clearance with the opposing supraerupted tooth is ~ 2 mm. It suggests that orthodontic intrusion is required for restoration. In fact the patient is incompliant with orthodontic mini-implant placement and retraction. When the implant at #31 is osteointegrated 4.5 months postop (Fig.2), it is used an anchor with an abutment and a provisional to intrude the opposing tooth. The final crown is cemented 10 months postop (Fig.3) with occlusal clearance (Fig.3' *). The contacts between #2 and 3 and between #31 and 32 are loose with papillary inflammation 5 months post cementation. It is planned to remove #31 crown/abutment for pick up impression/porcelain addition. Instead the crown is removed. After removing #32 MO composite with minor 2nd caries, new composite is placed (Fig.4 *) while the crown is reseated. When the crown is recemented, bitewing shows open margin (Fig.4), but the contact is wide and tight. After occlusal adjustment, occlusal contact at #31 and 32 mesial is heavier than that at #30. #3 crown is recommended. The occlusal table difference betweeen the upper 1st and 2nd molar is ~ 2 mmm preop (Fig.4'), whereas the difference is ~ .6 mm postop (in combination of occlusal equilibrium and intrusion of the upper 2nd molar (Fig.4)). It seems that orthodontic intrusion is not efficient in a male with bruxism. There is mild lingual (L) and distal bone loss 1.5 years post cementation (Fig.5) when CT is taken for #3 immediate implant. Lower Molar Immediate Implant, Armaments Xin Wei, DDS, PhD, MS 1st edition 07/12/2018, last revision 11/28/2020