.jpg)






 |
 |
.jpg) |
 |
 |
 |
 |
|
 |
 |
 |
|
 |
 |
||
PRF and Sticky Bone Repair Buccal Soft and Hard Tissue
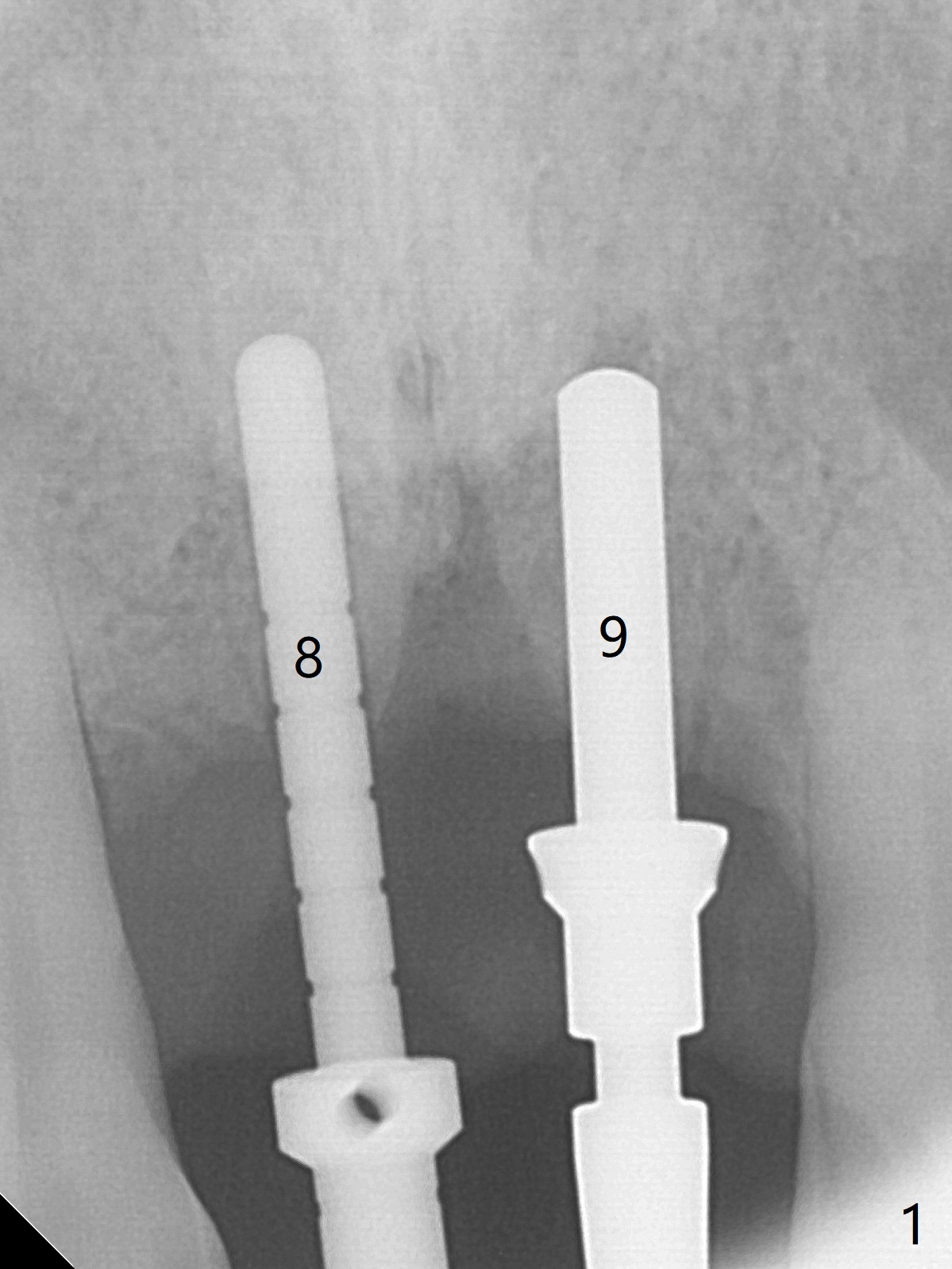
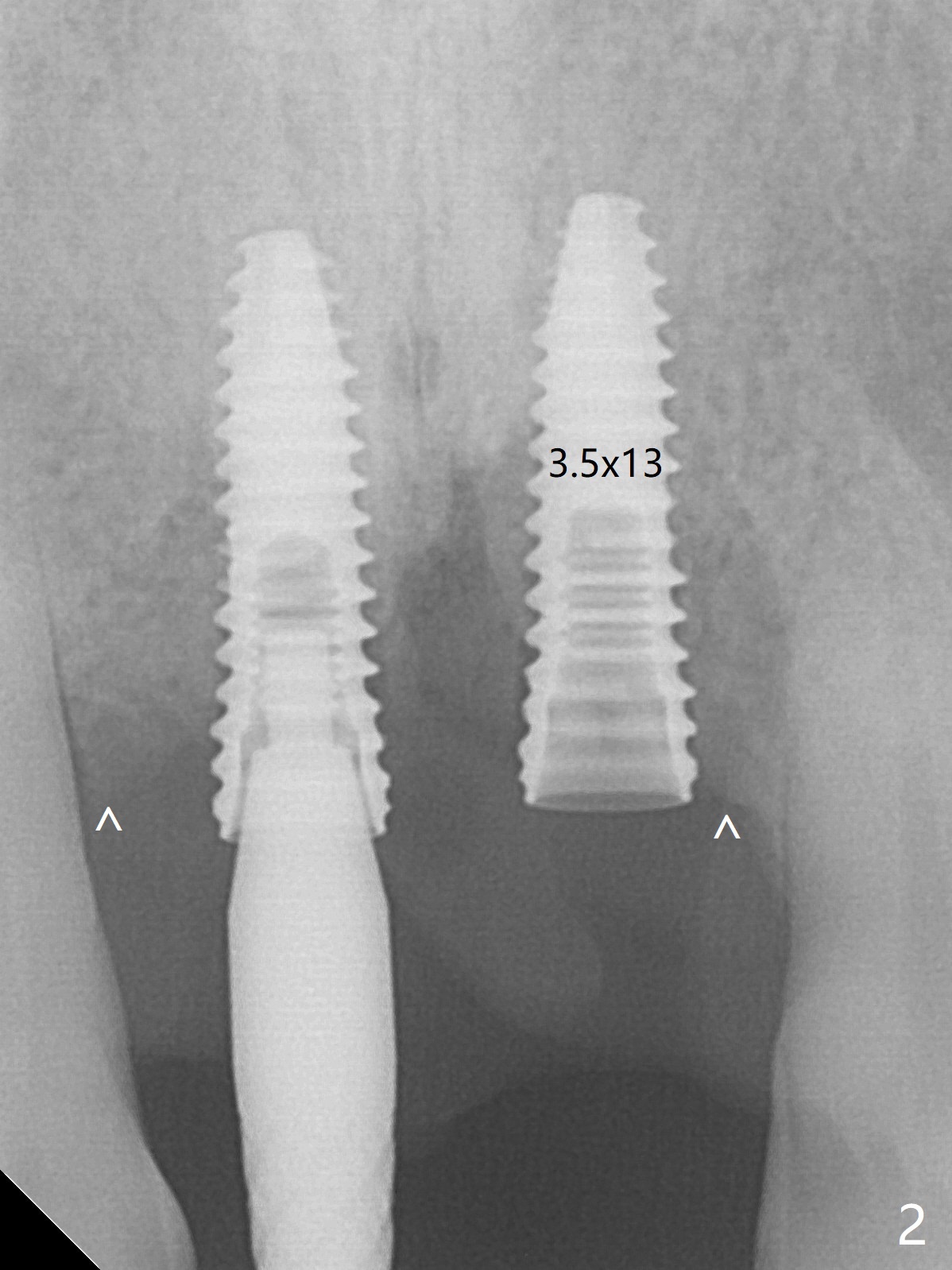
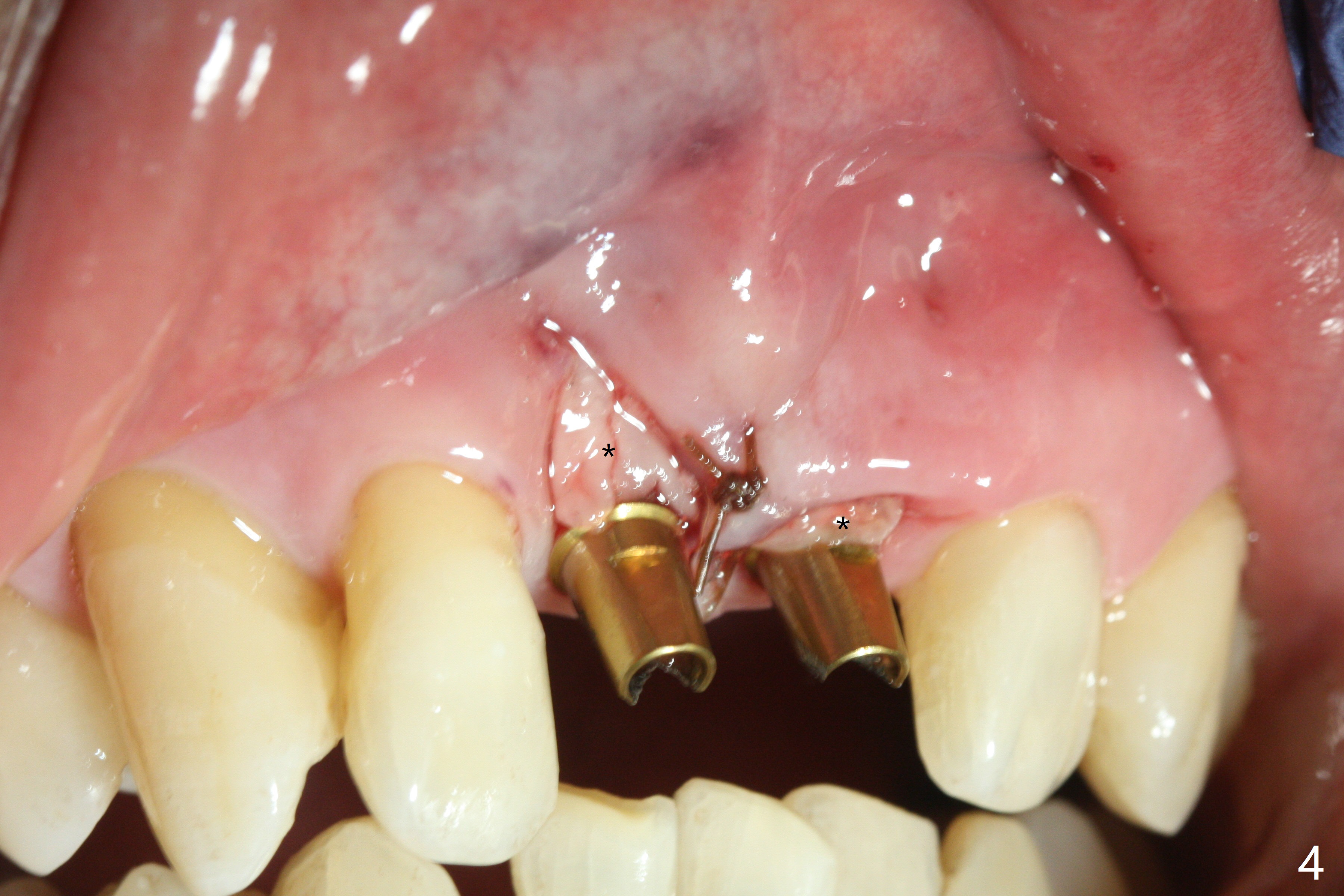
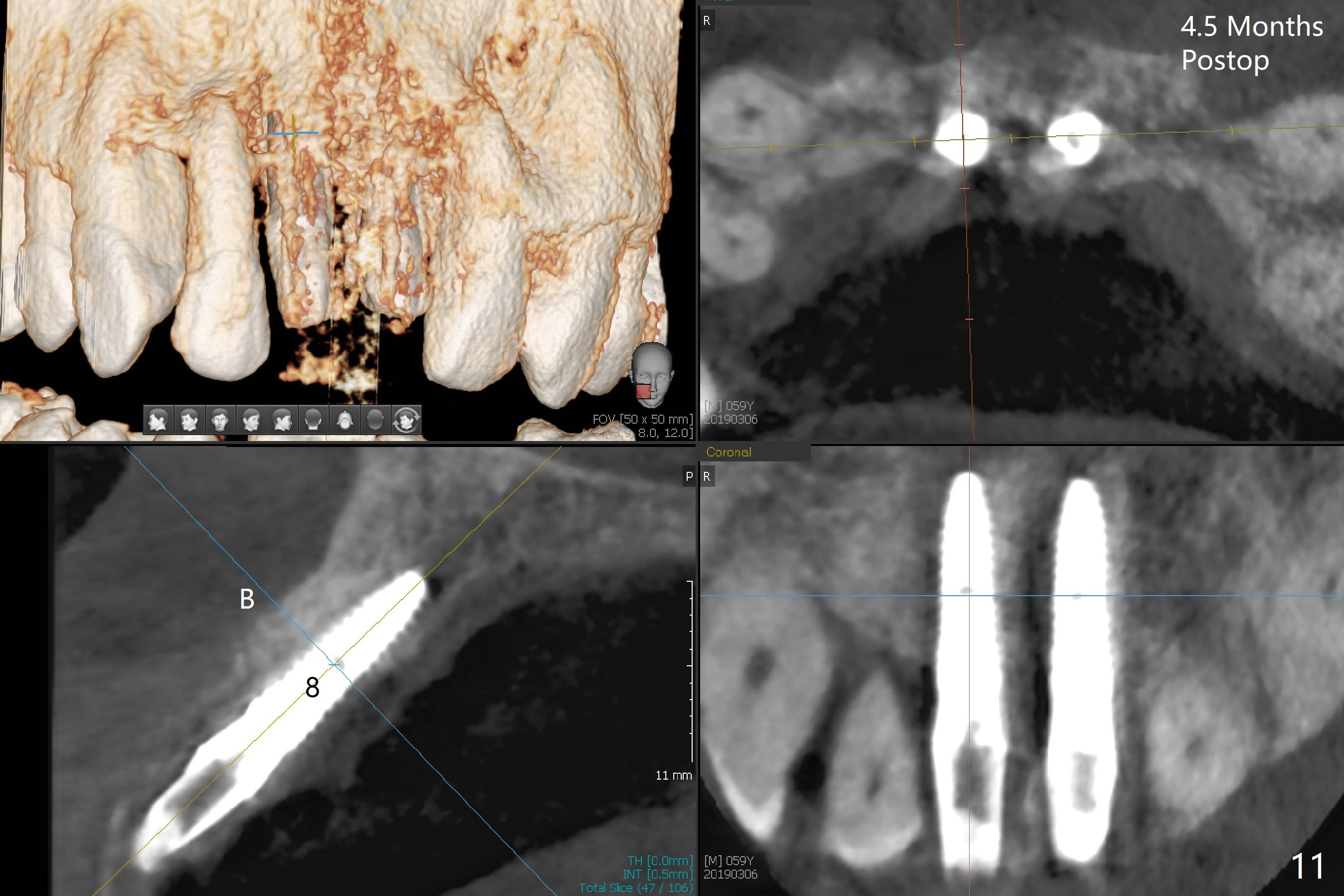
Defects with Immediate Implants
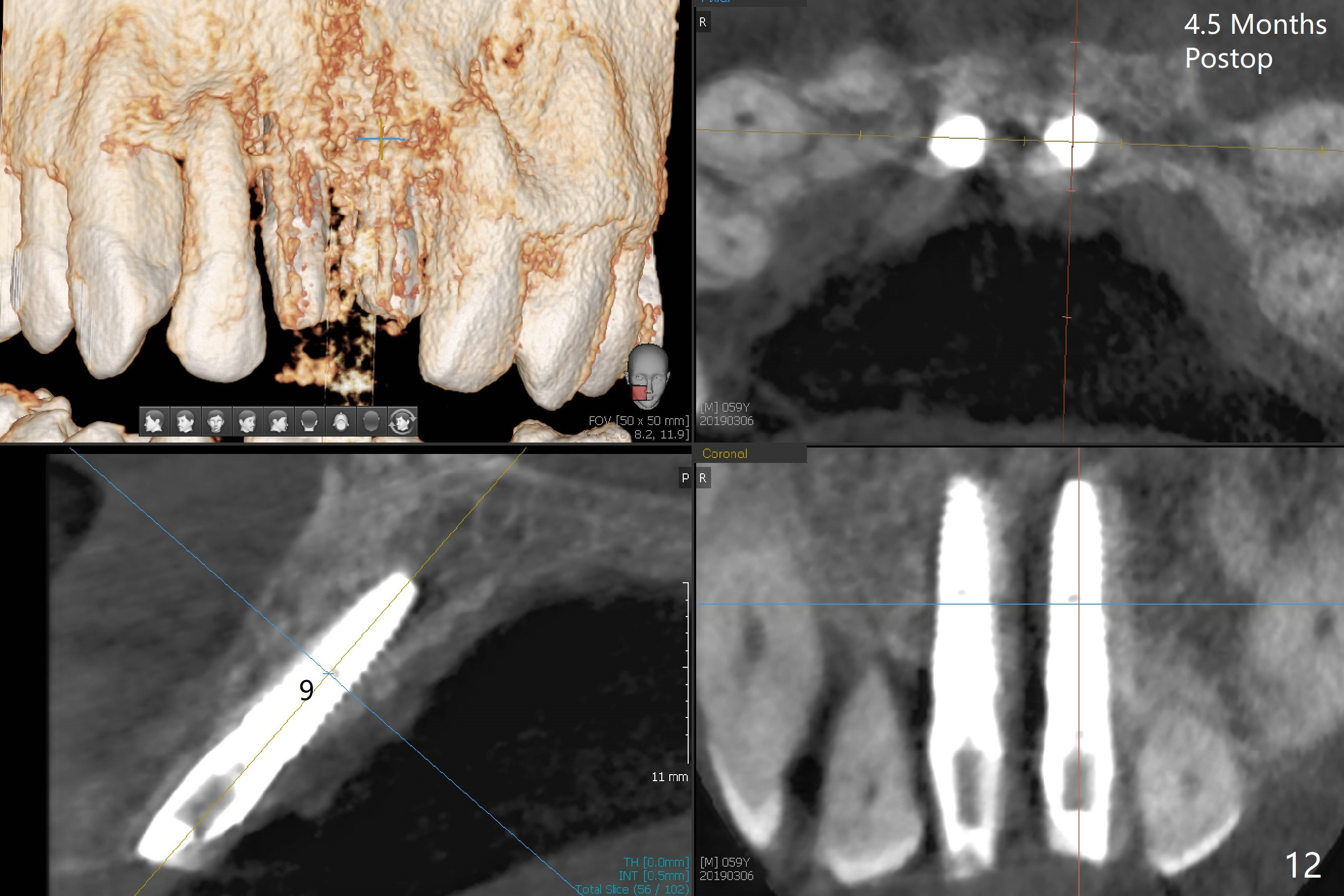
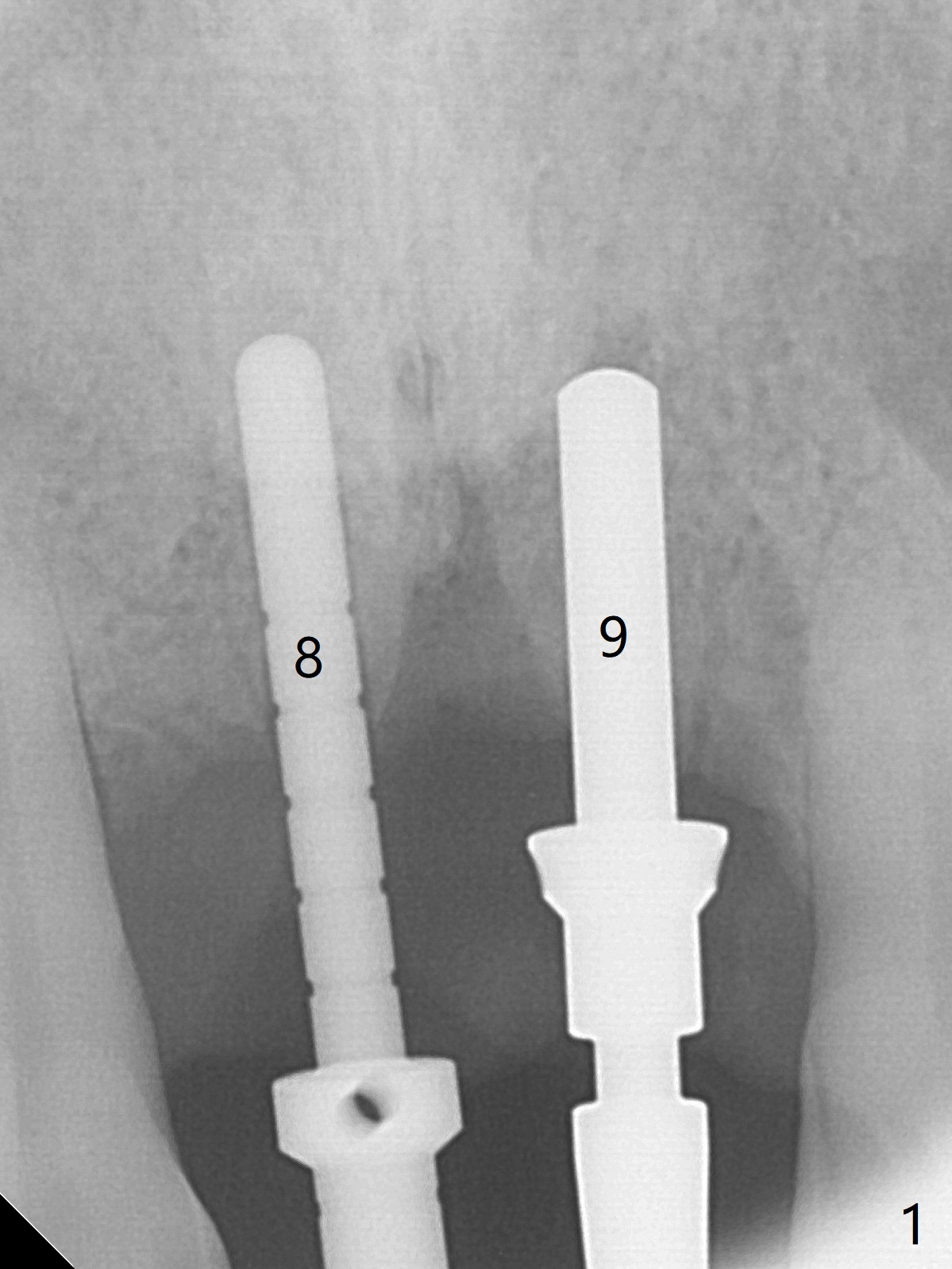
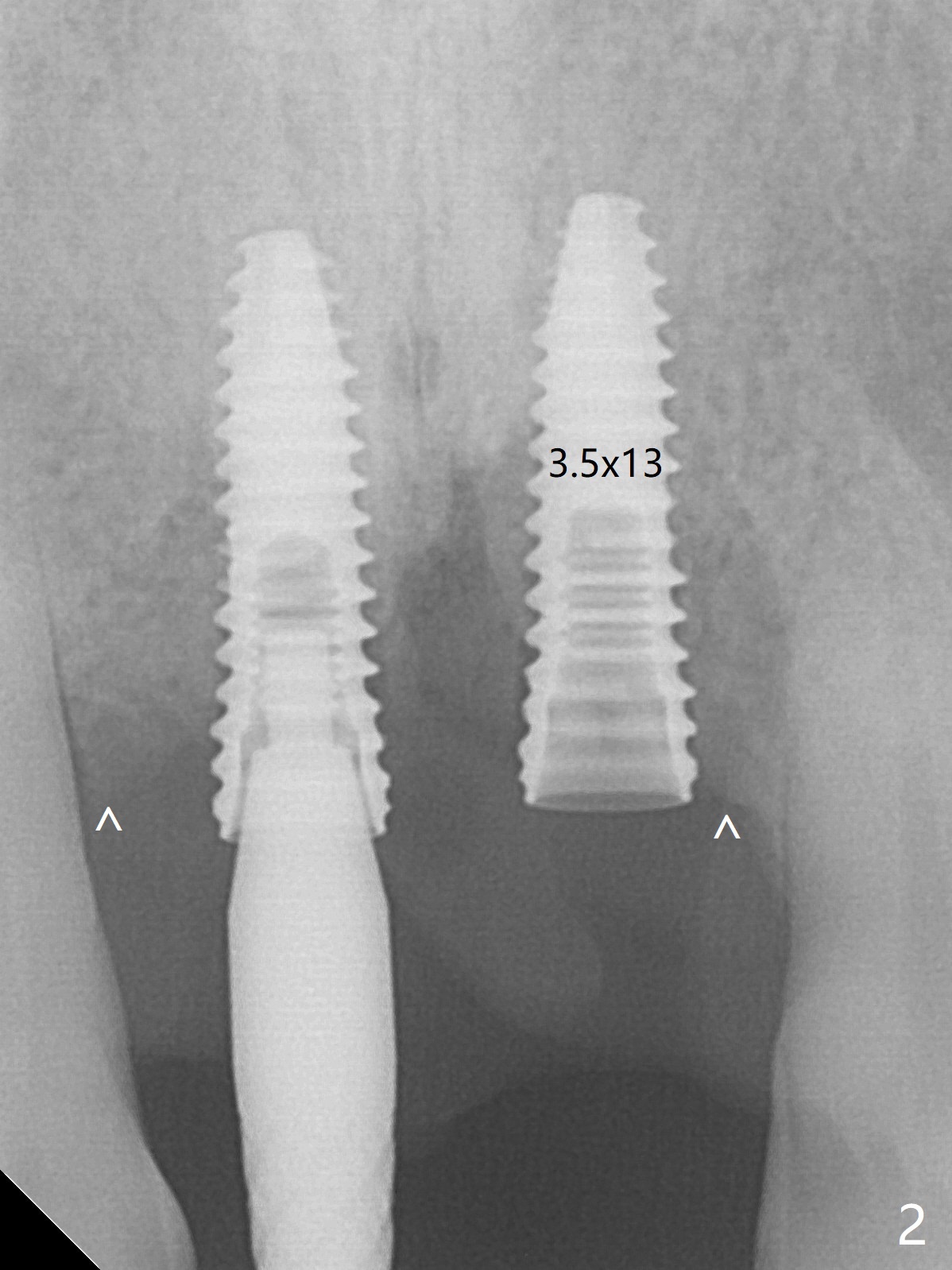
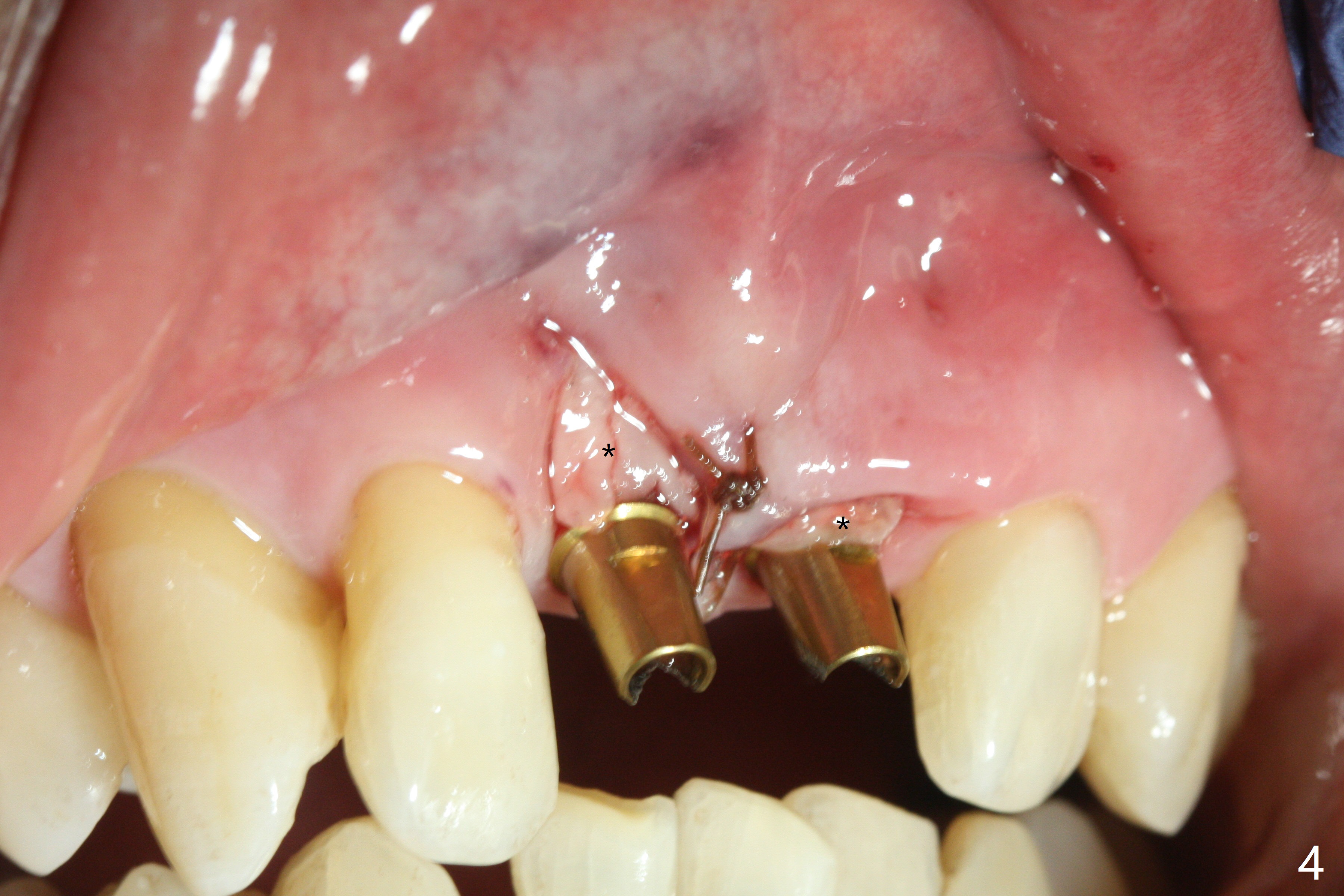
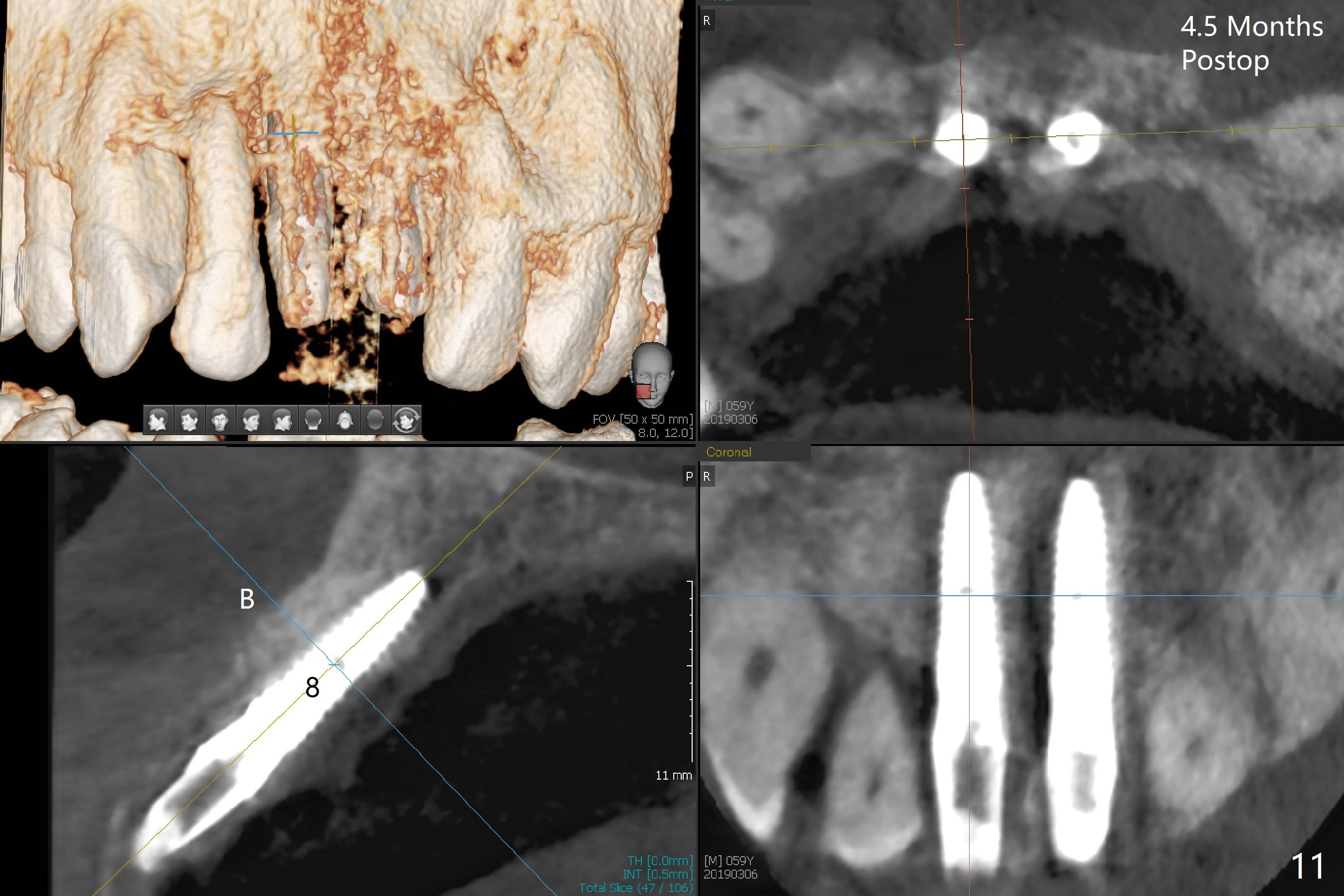
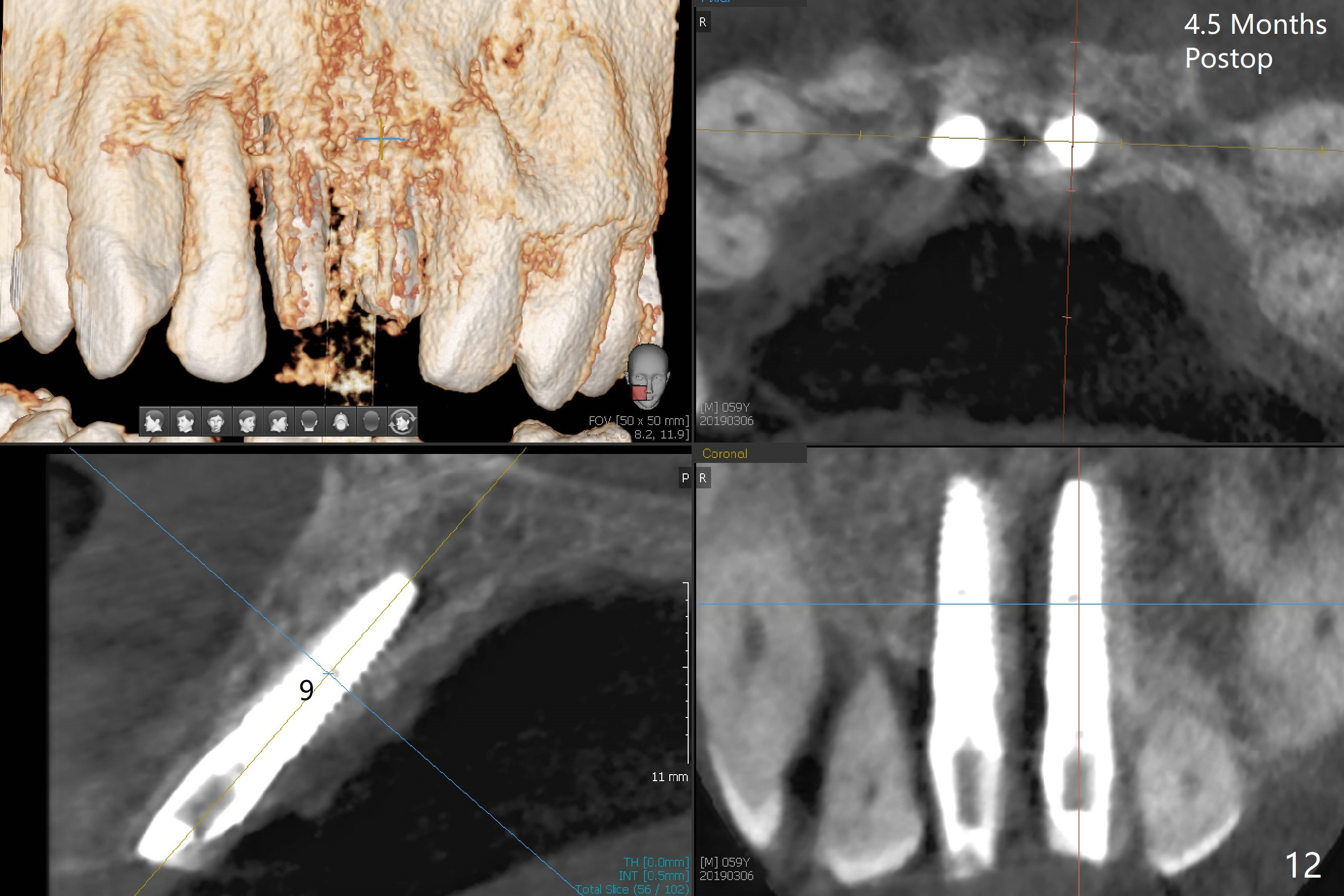
There is no buccal plate at #8 or 9 when the teeth are extracted as well as severe soft tissue defect at #8. Osteotomy is initiated as palatal as possible (Fig.1). When 3.5x13 mm implants are placed initially, the one at #8 is supracrestal (Fig.2 ^). To reduce the chance of peri-implantitis, the implant is placed deeper (Fig.3 (~2 mm implant threads exposed buccally)) with placement of sticky bone around the implants and 4.5x5.5(4) mm abutments (Fig.3 *). The buccal soft tissue defect #8 is repaired with a piece of PRF membrane (Fig.4 *), followed by periodontal dressing. Smaller 2-piece implants (3 mm, IBS) with smaller abutments (4 mm) may further reduce chance of periimplantitis and easy buccopalatal reduction of the abutments for restoration. The periodontal dressing remains stable 7 days postop (Fig.5) because it wraps around the abutments (Fig.6 A). By the time the periodontal dressing gets loose, #8 buccal soft tissue defect should be healing. When breaking-down periodontal dressing is removed 17 days postop, the coronal abutments and bone graft are exposed; after fabrication of provisional crowns (Fig.7), periodontal dressing is re-applied buccally. When the second dressing dislodges 5 weeks postop, the buccal soft tissue appears to reduce (Fig.8). Raising flaps may be less traumatic. A piece of bone graft is being extruded 4 months postop (Fig.9 >). After the abutments change from 4.5x5.5(4) to 4.5x7(3) mm, new temporary crowns are fabricated (Fig.10 (4.5 months postop)). CT shows apparent buccal bone at #8 and 9 (Fig.11,12). How to improve cosmetic?
Return to Upper Incisor Immediate Implant, Trajectory Xin Wei, DDS, PhD, MS 1st edition 10/26/2018, last revision 04/25/2019