
,%20Vanilla,%20angled%20abutment%20later.jpg)
.jpg)
%20BW%20sensor%202,%2017m%20post%20cem.jpg)
,%20occl%20reduction,%20palatal%20margin%20reduction,%20sensor%201%20PA.jpg)
,%20(3)%20worn.jpg)
,%20(3).jpg)
 |
 |
,%20Vanilla,%20angled%20abutment%20later.jpg) |
|||
 |
.jpg) |
 |
%20BW%20sensor%202,%2017m%20post%20cem.jpg) |
 |
,%20occl%20reduction,%20palatal%20margin%20reduction,%20sensor%201%20PA.jpg) |
,%20(3)%20worn.jpg) |
,%20(3).jpg) |
||||
Thin Septum: Difficult for Immediate Implant
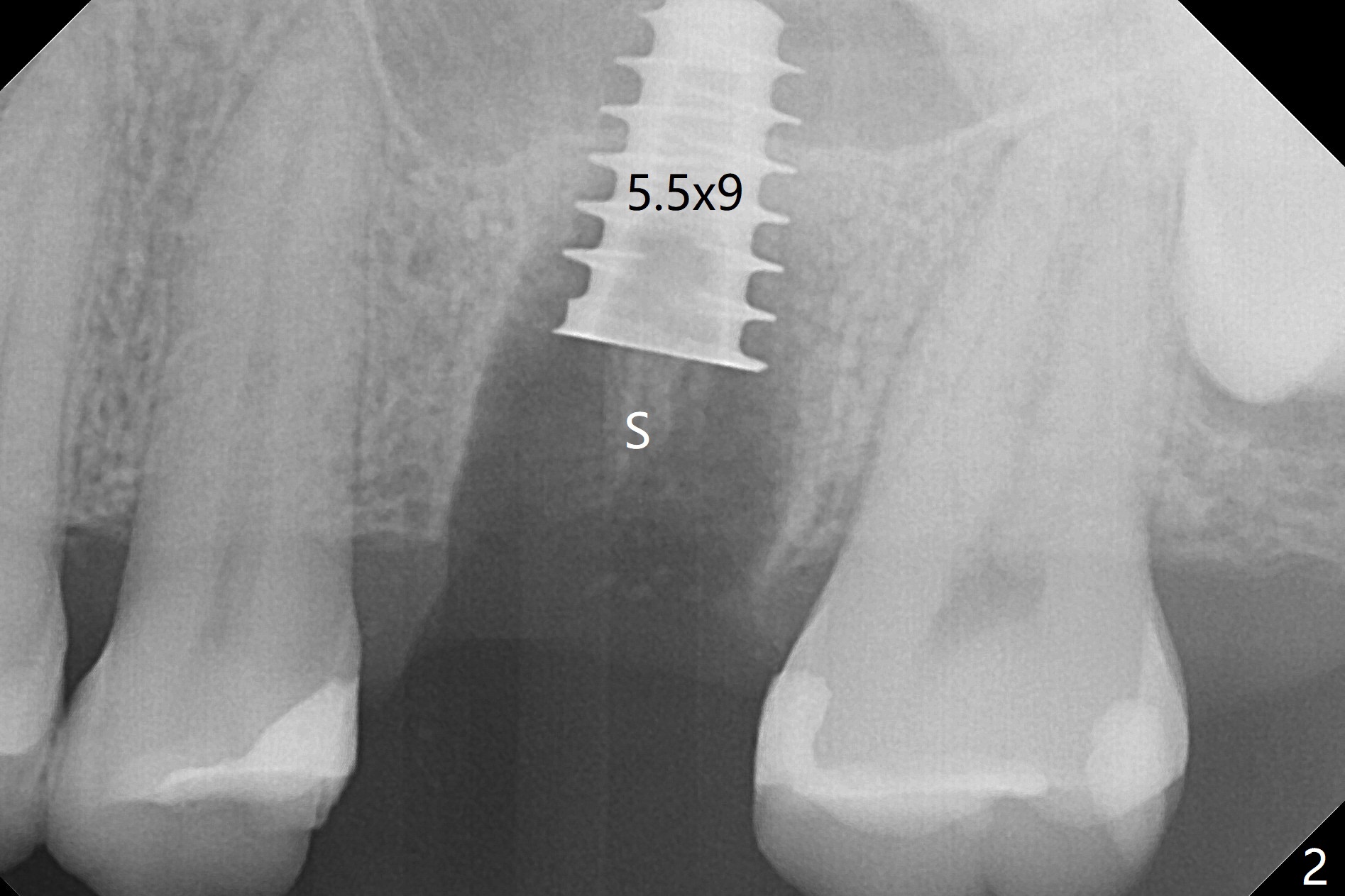
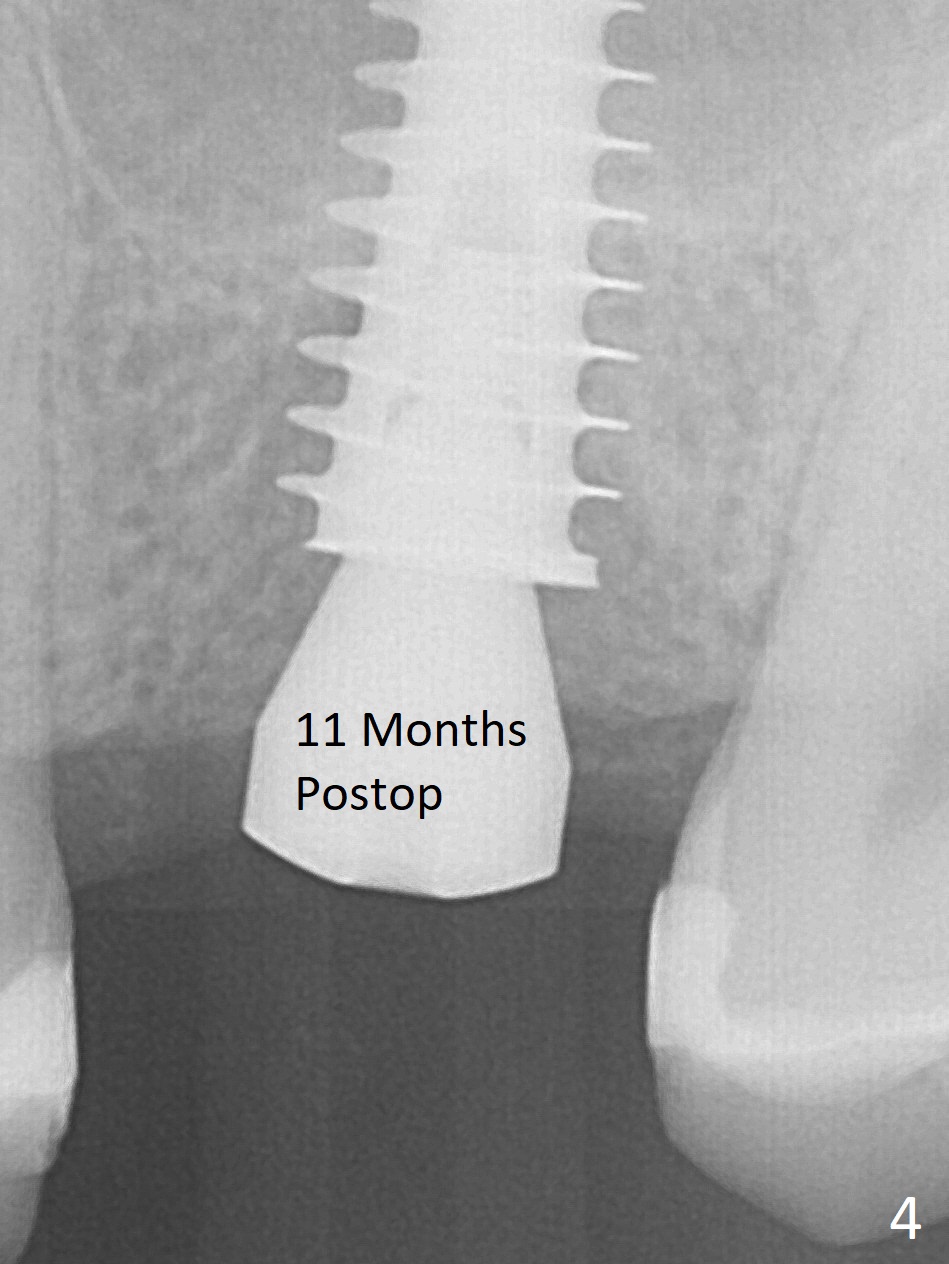
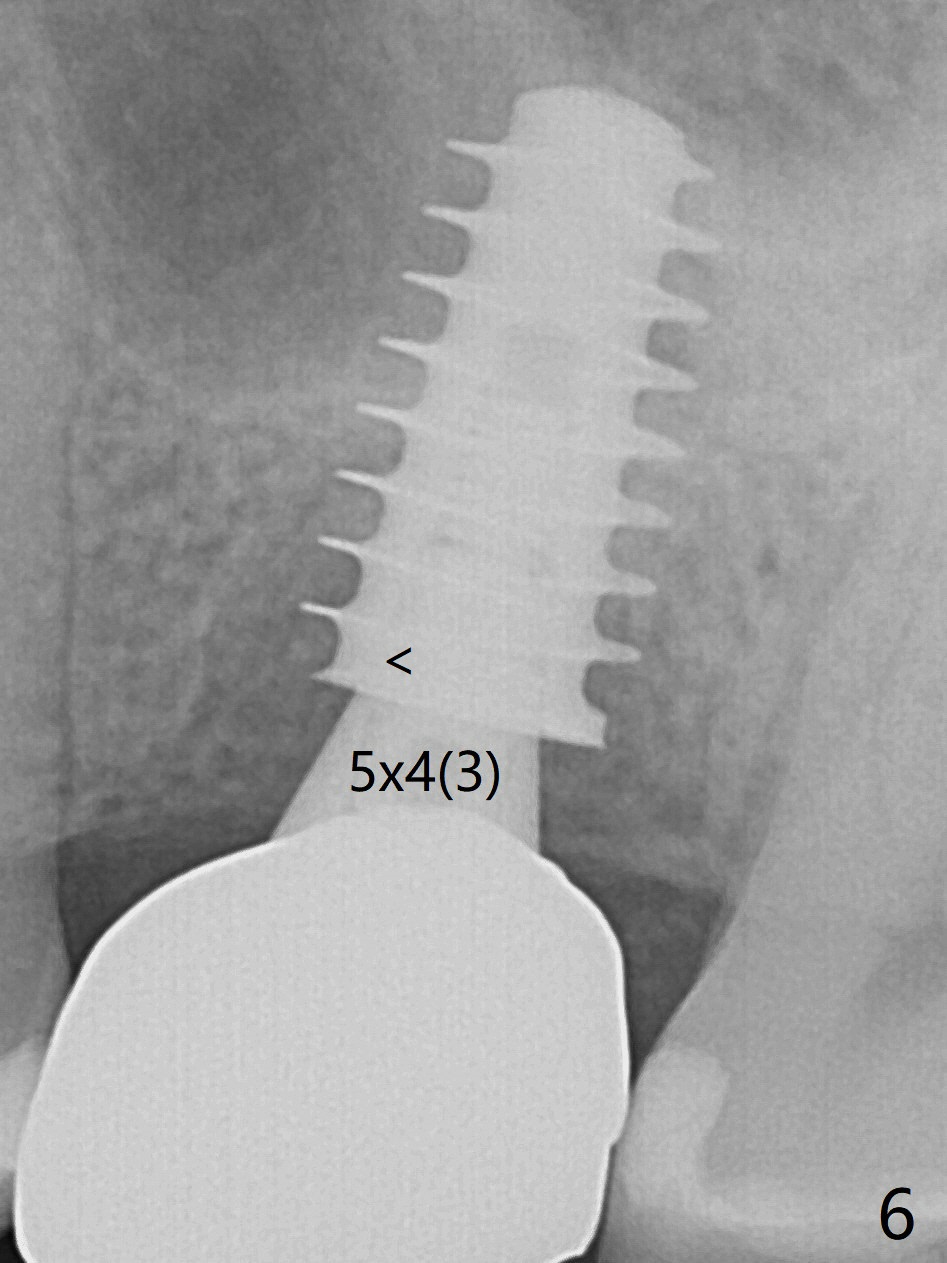
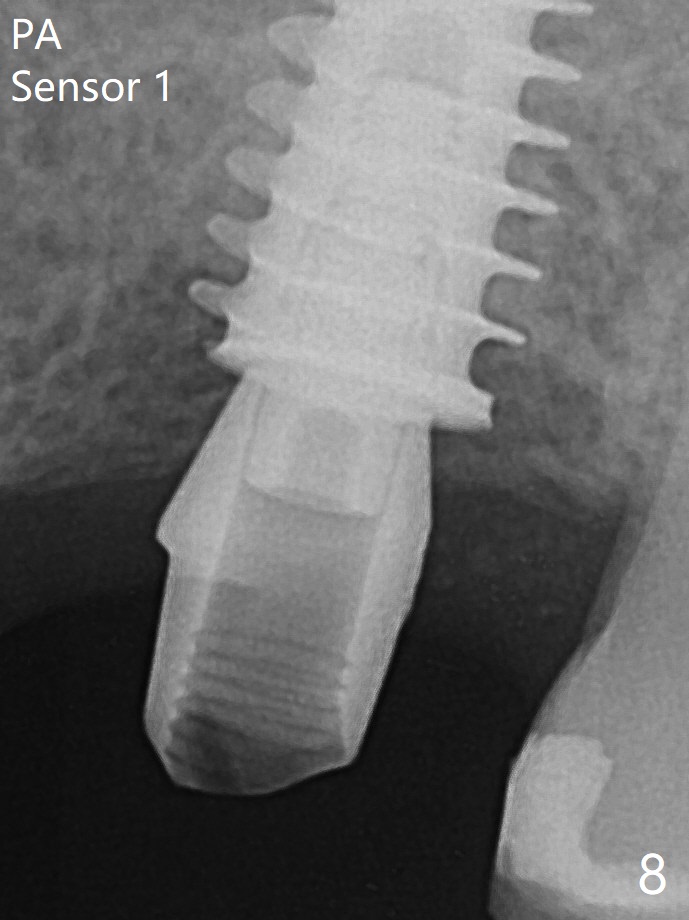
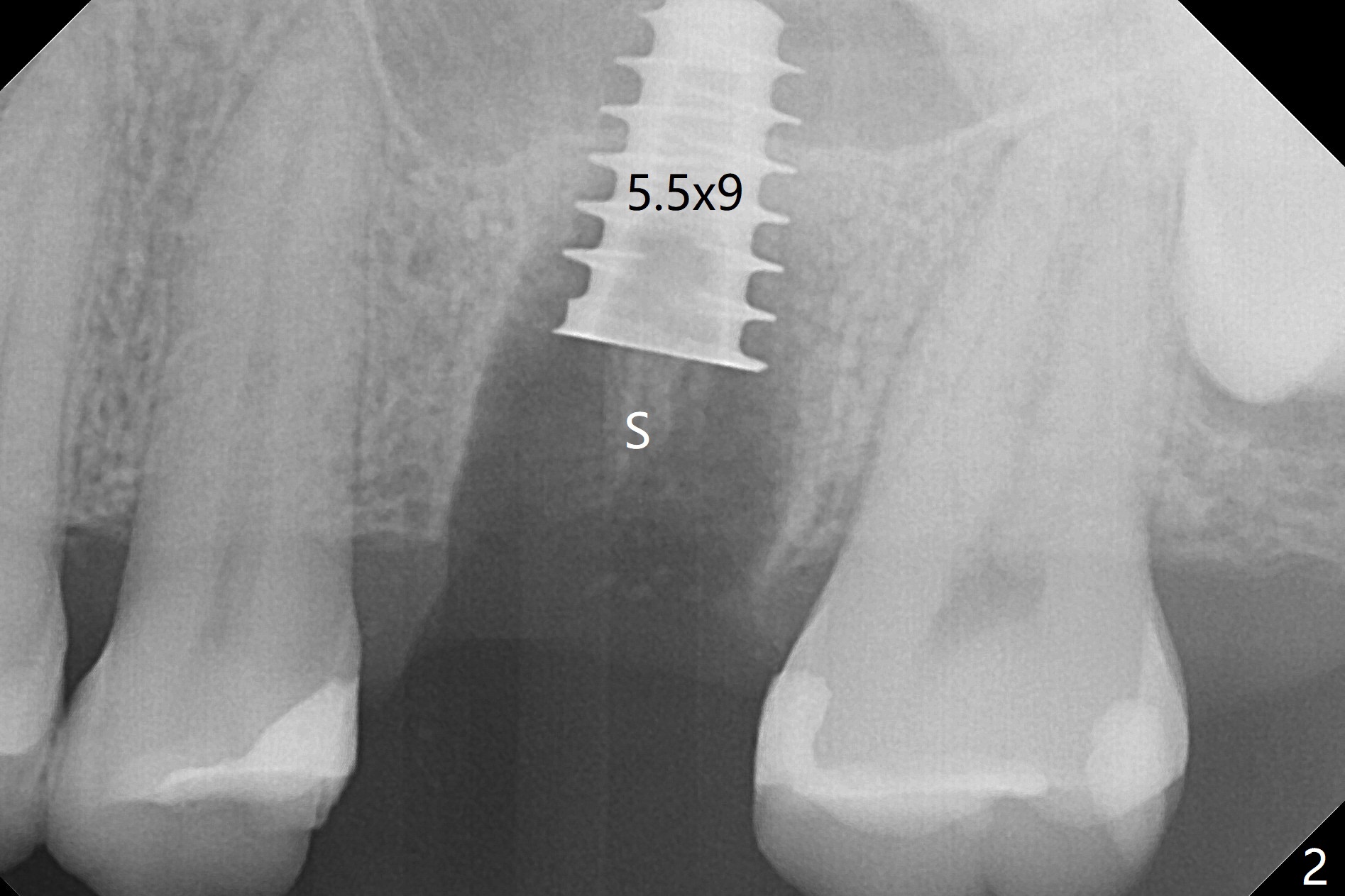
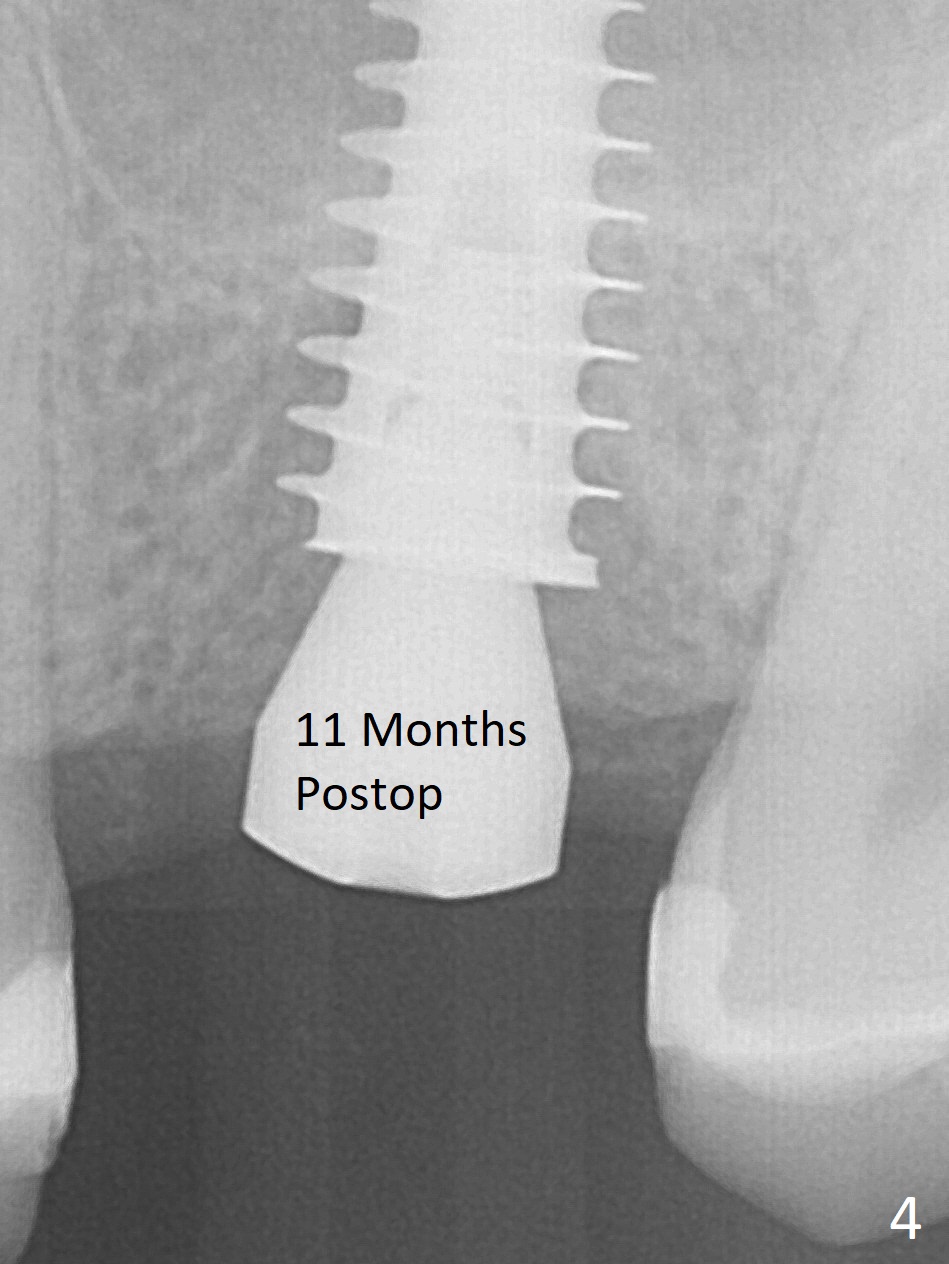
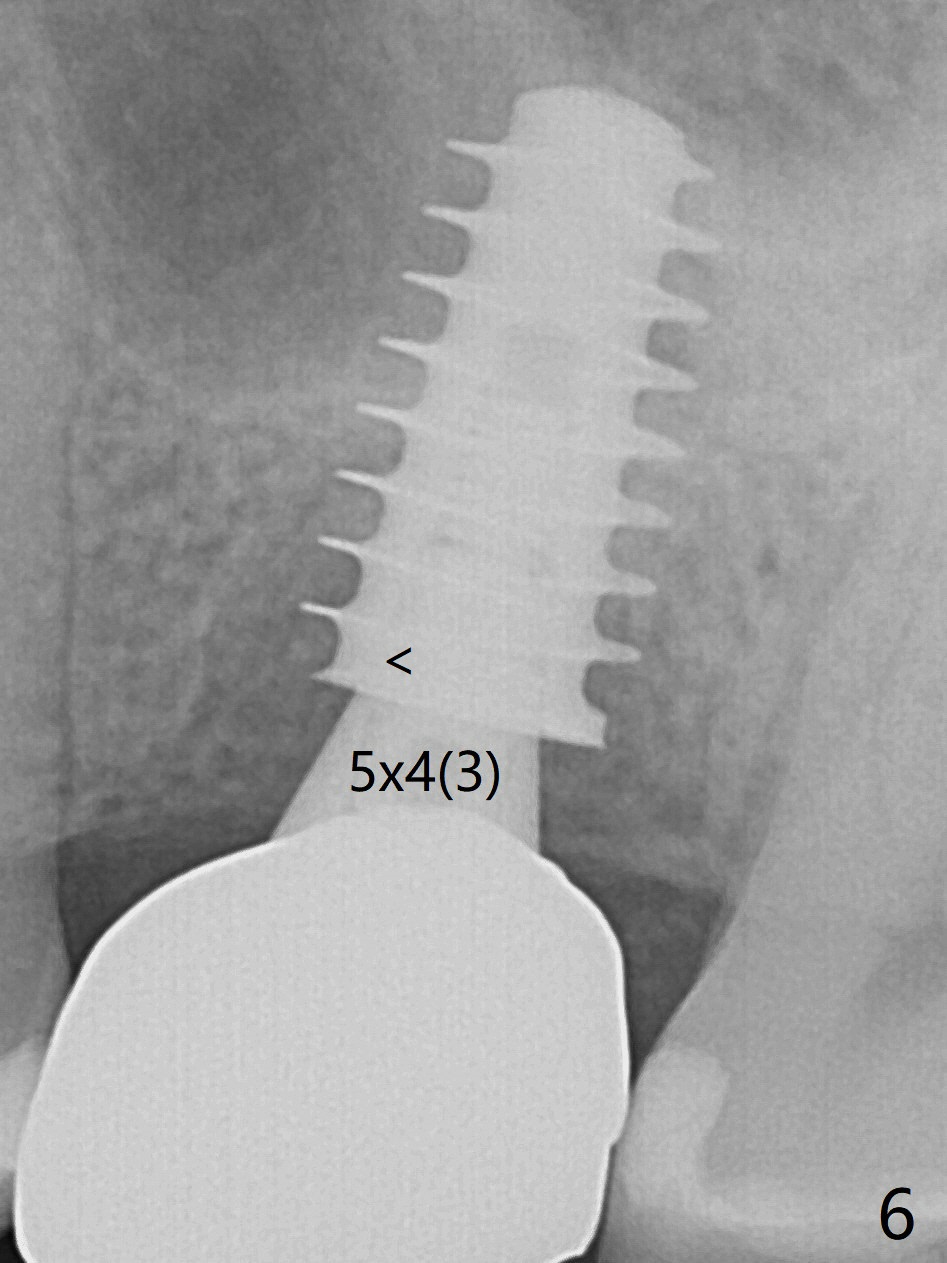
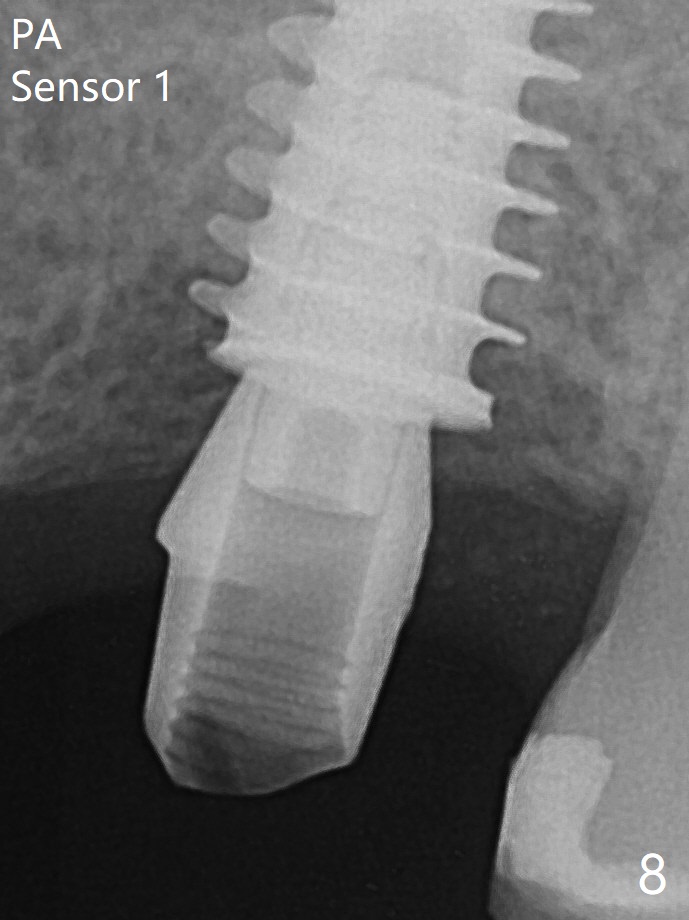
After extraction of the tooth #14 with palatal swelling (Fig.1 *), the septum (S in Fig.2) is found to be thin. Sequential osteotomy quickly deviates to the palatal socket. In spite of using Lindamann bur to remove the bone from the buccal portion of the osteotomy, the apical end of a 5x9 mm dummy implant slides into the palatal socket with the coronal end placed as buccal as possible for restoration (Fig.2 (poor trajectory)). Further use of Lindamann bur for buccal bone removal is not feasible, since the buccoapical portion of the osteotomy starts to be perforated with apparently intact sinus membrane. With insertion of Vanilla graft for sinus lift through the buccoapical portion of the osteotomy mentioned above, a 6x11 mm implant is placed with the same trajectory (Fig.2, <40 Ncm). With placement of a 6.5x4(3) mm abutment (off angle) and of Vanilla graft in the remaining sockets (Fig.2 *), periodontal dressing is applied. When the dressing is dislodged for the 2nd time (12 days postop with healing socket), an angled abutment 5x15 degree, 3 mm cuff, is placed and a provisional is fabricated. There is no sign of sinus infection. The provisional and angled abutment become loose without sinus infection 2 months postop. A 5.5x3 mm healing abutment is placed with light tenderness. If this case turns to be failure, do not stick an immediate implant from potentially infected socket into the sinus in the future. The socket appears to heal 11 months postop (Fig.4). Later a 5x4(3) mm abutment is placed for final restoration. The palatal margin is low. The abutment screw is loose <2 months post cementation, probably due to deep placement and poor trajectory (buccal). It becomes loose again 4 months later. Prior to retightening, a 6 mm profile drill is used. BW shows no bony interference (Fig.5 (opposing tooth occlusal wear; bruxism)), while PA shows the buccal bone, suggesting poor trajectory. The abutment is loose for the 3rd time 17 months post cementation. When the crown/abutment is removed, the hex is worn. After proximal reduction, the crown/abutment feels to be unable to be re-seated. When the crown is sectioned, the abutment itself is incompletely seated (Fig.7,8). The mesial crest appears to interfere with seating (Fig.8). When the 5.2x3 mm dummy abutment is seated, the buccal margin is subgingival, while the palatal one supragingival, suggesting the buccally tilted implant (guided surgery essential). A 4.5x4(4) mm pair abutment seems to be seated completely (Fig.9). The hex of the 5x4(3) mm abutment is worn, but the abutment seems to be able to be seated completely (Fig.11), although not so crisply (easily) as the unworn one clinically. Return to Upper Molar Immediate Implant, Prevent Molar Periimplantitis (Protocols, Table), Armaments Screw Xin Wei, DDS, PhD, MS 1st edition 06/26/2018, last revision 12/20/2020