





 |
 |
 |
|
 |
 |
 |
 |
  |
 |
 |
|
 |
|||
Fill in Large Molar Socket
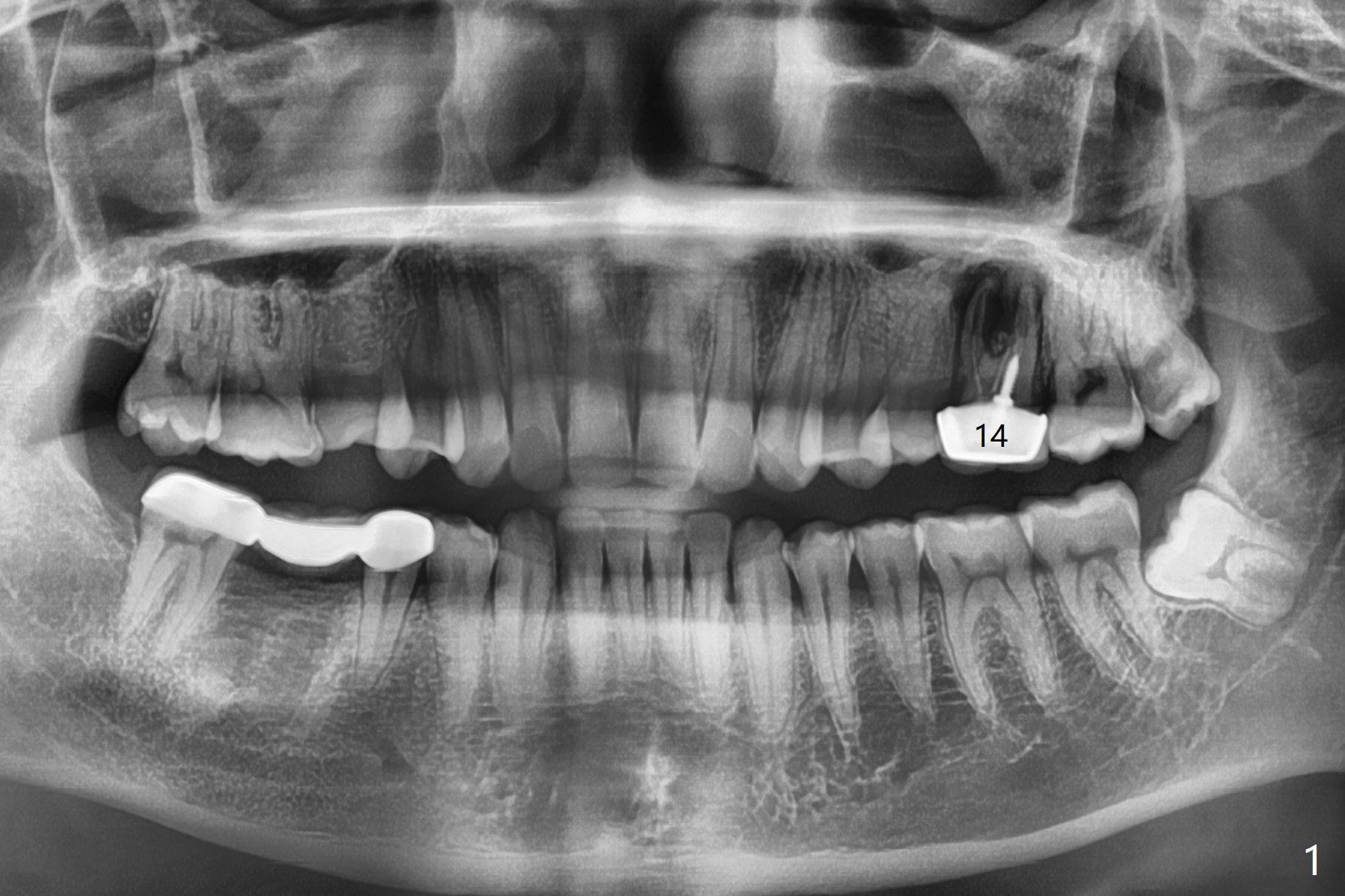
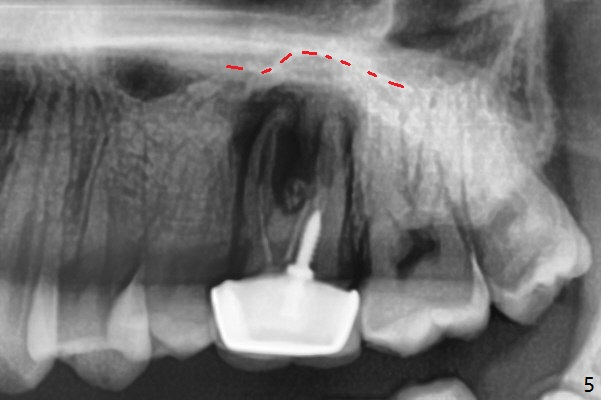
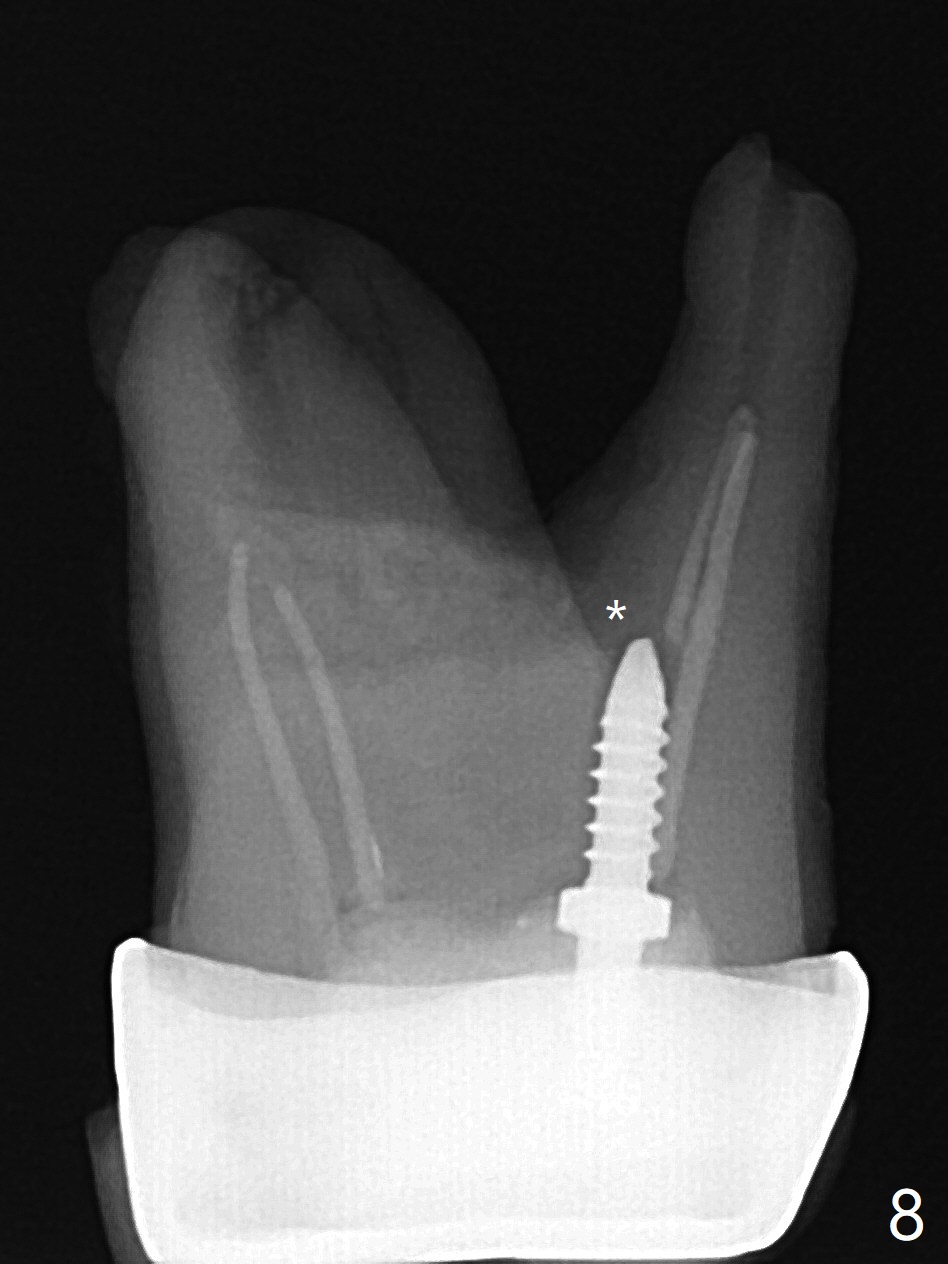
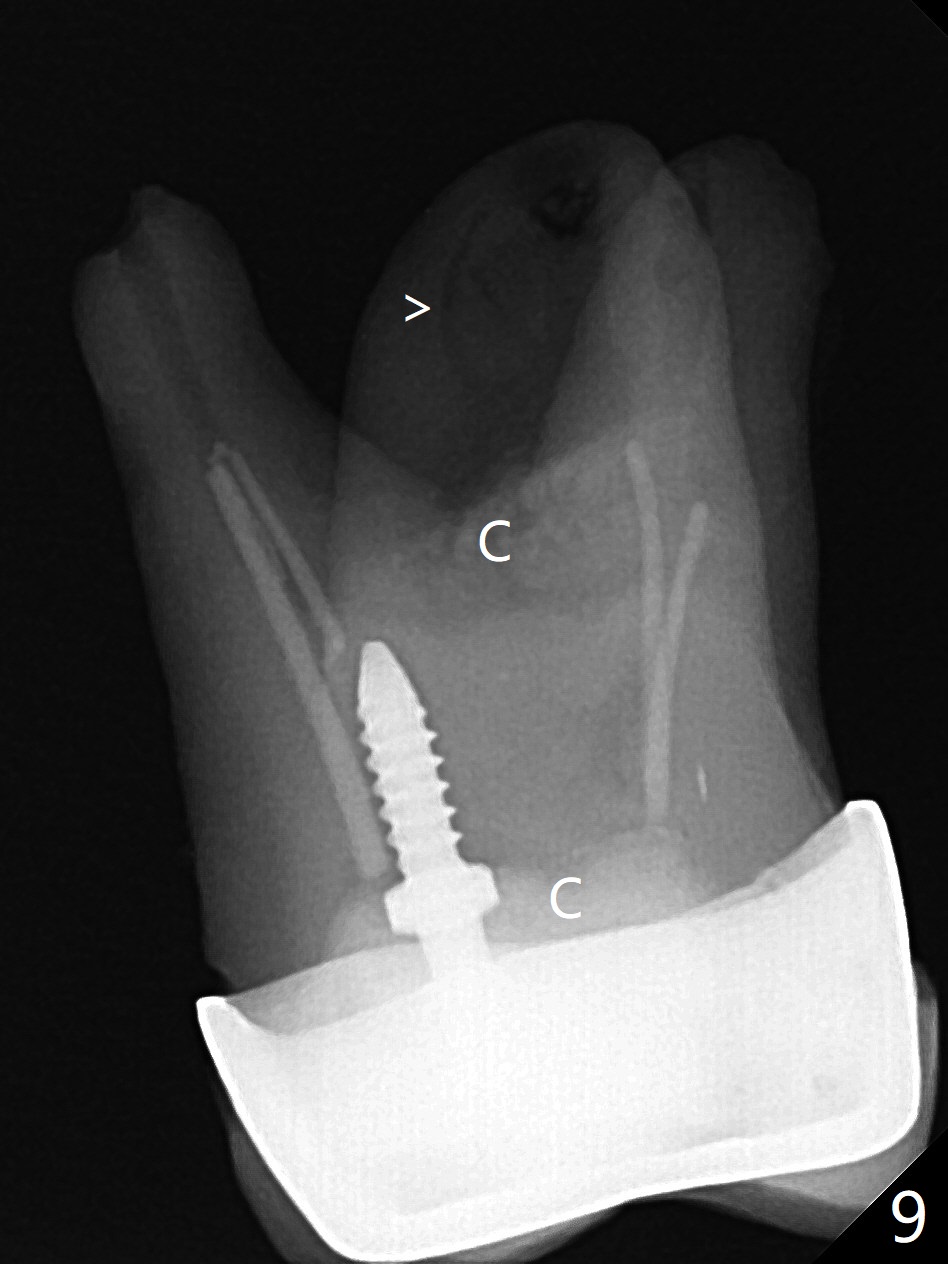
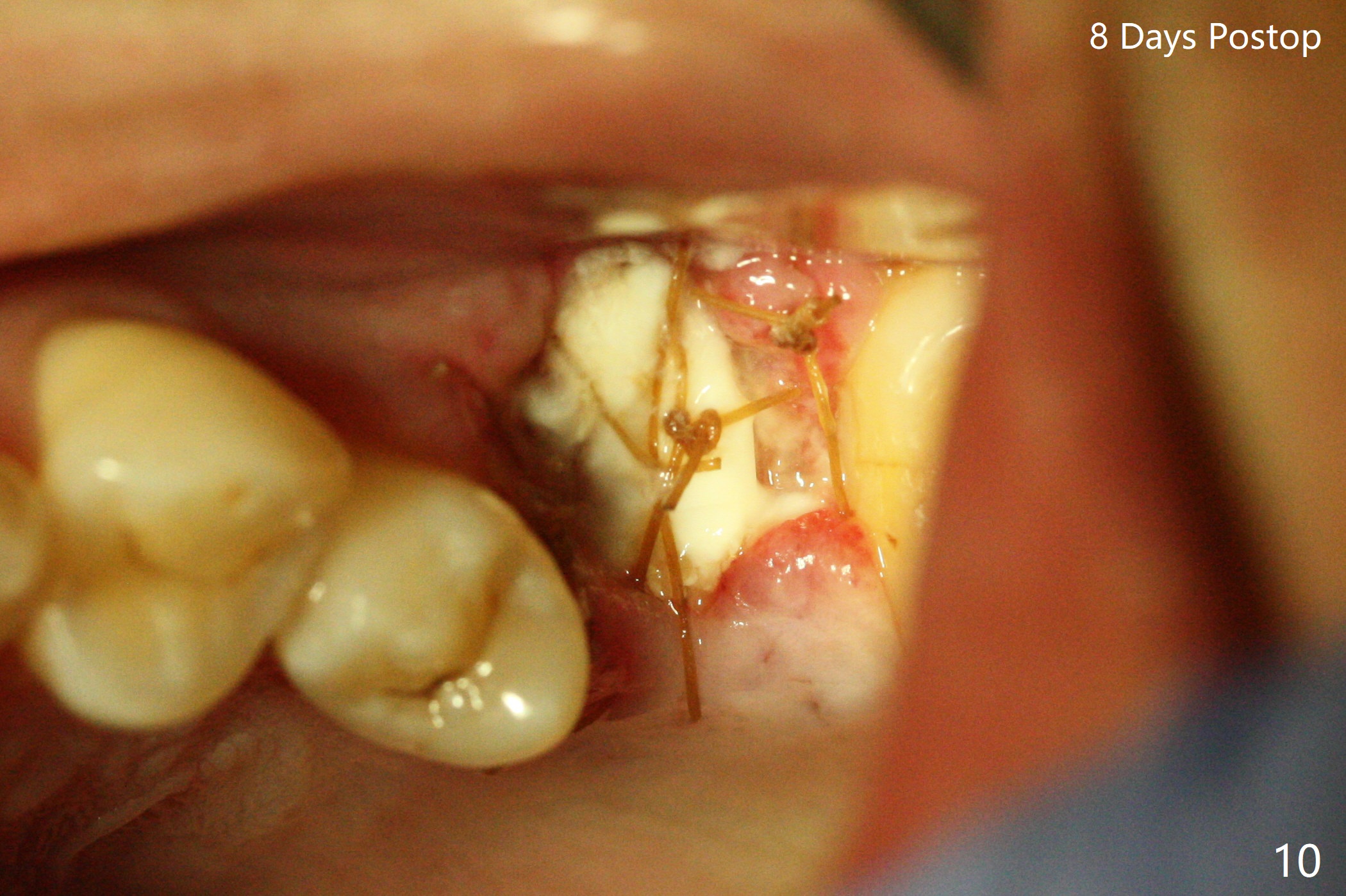
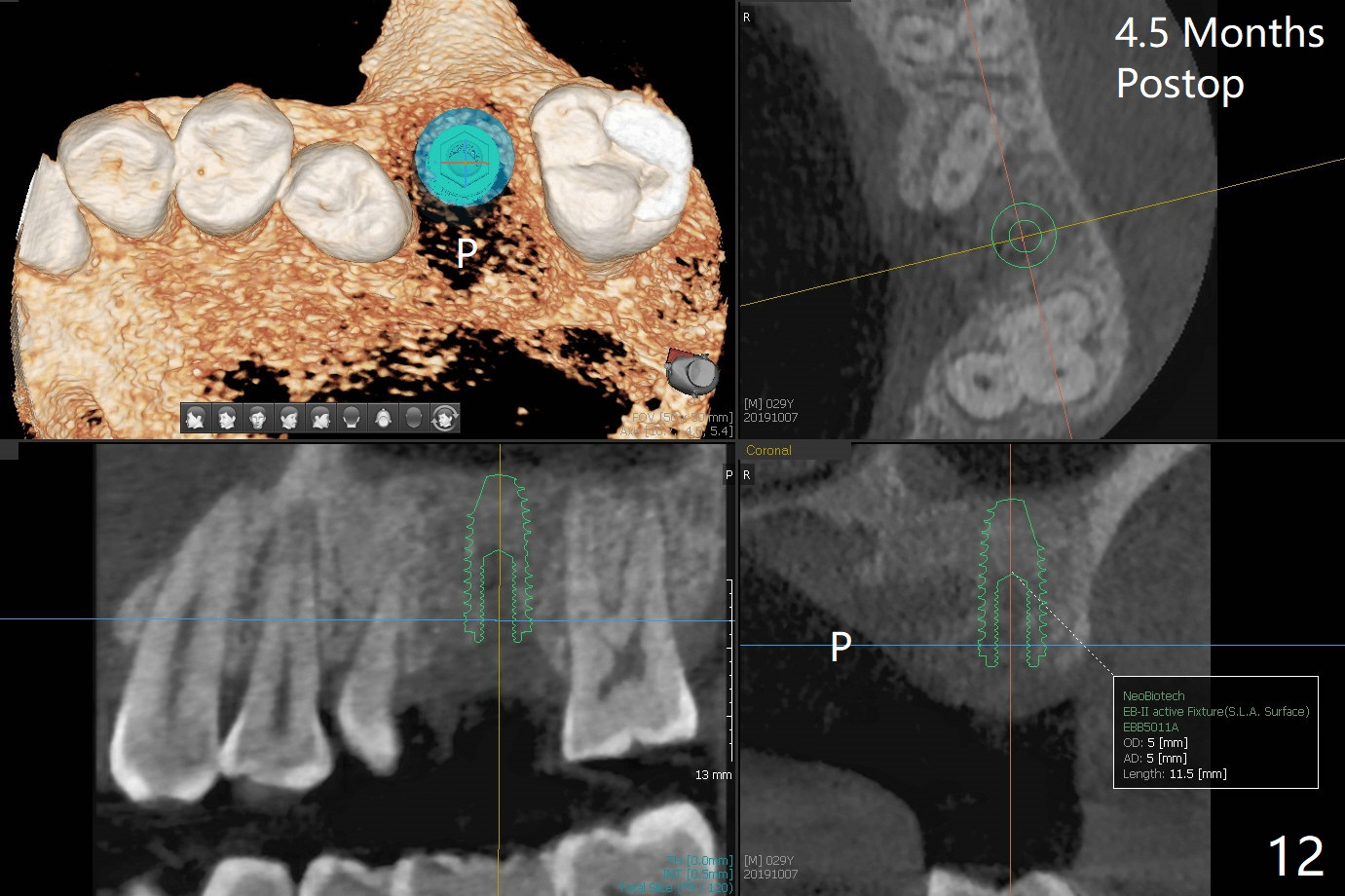
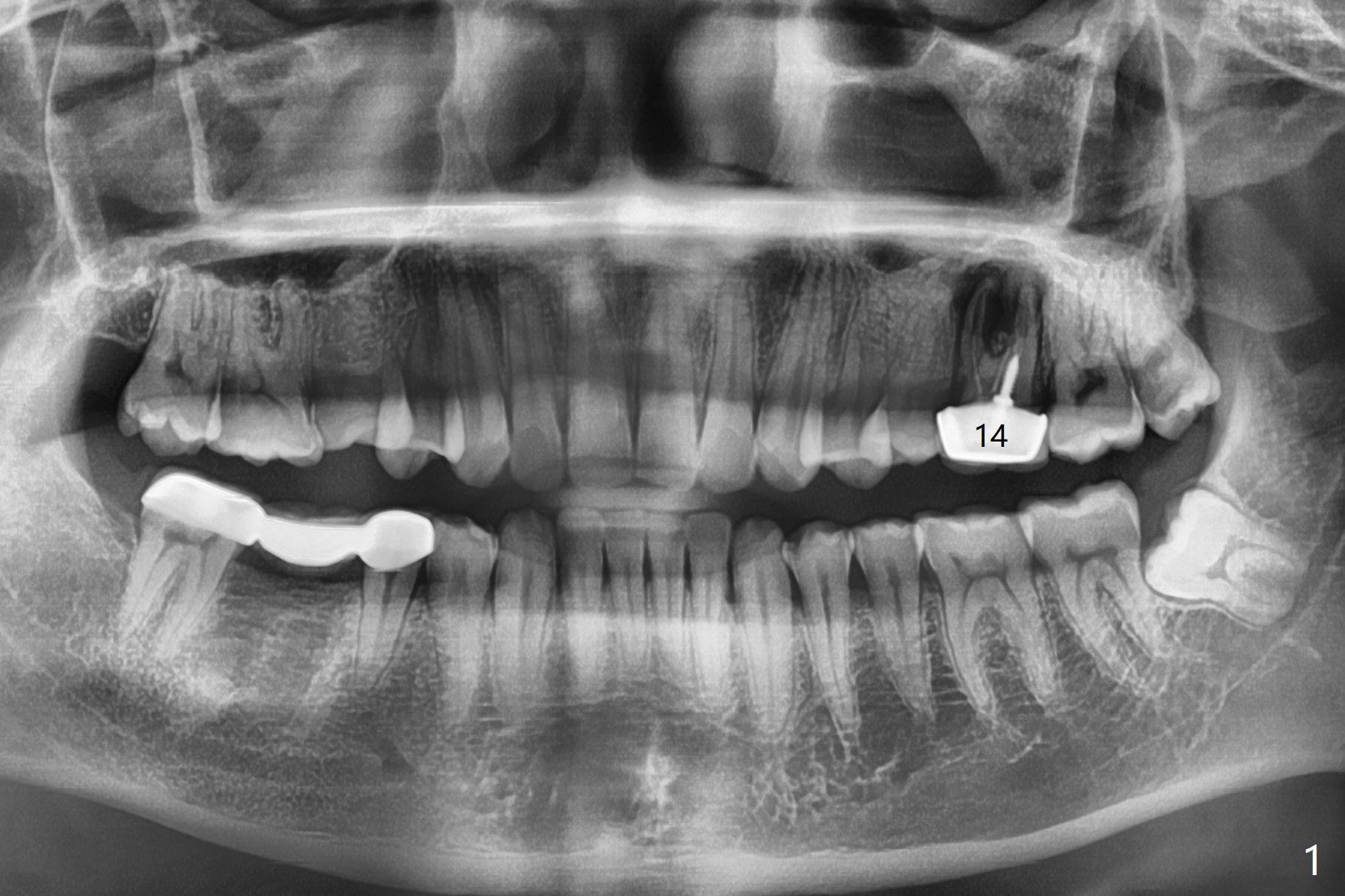
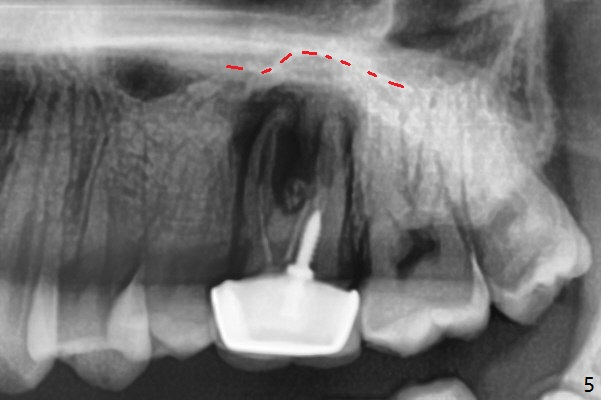
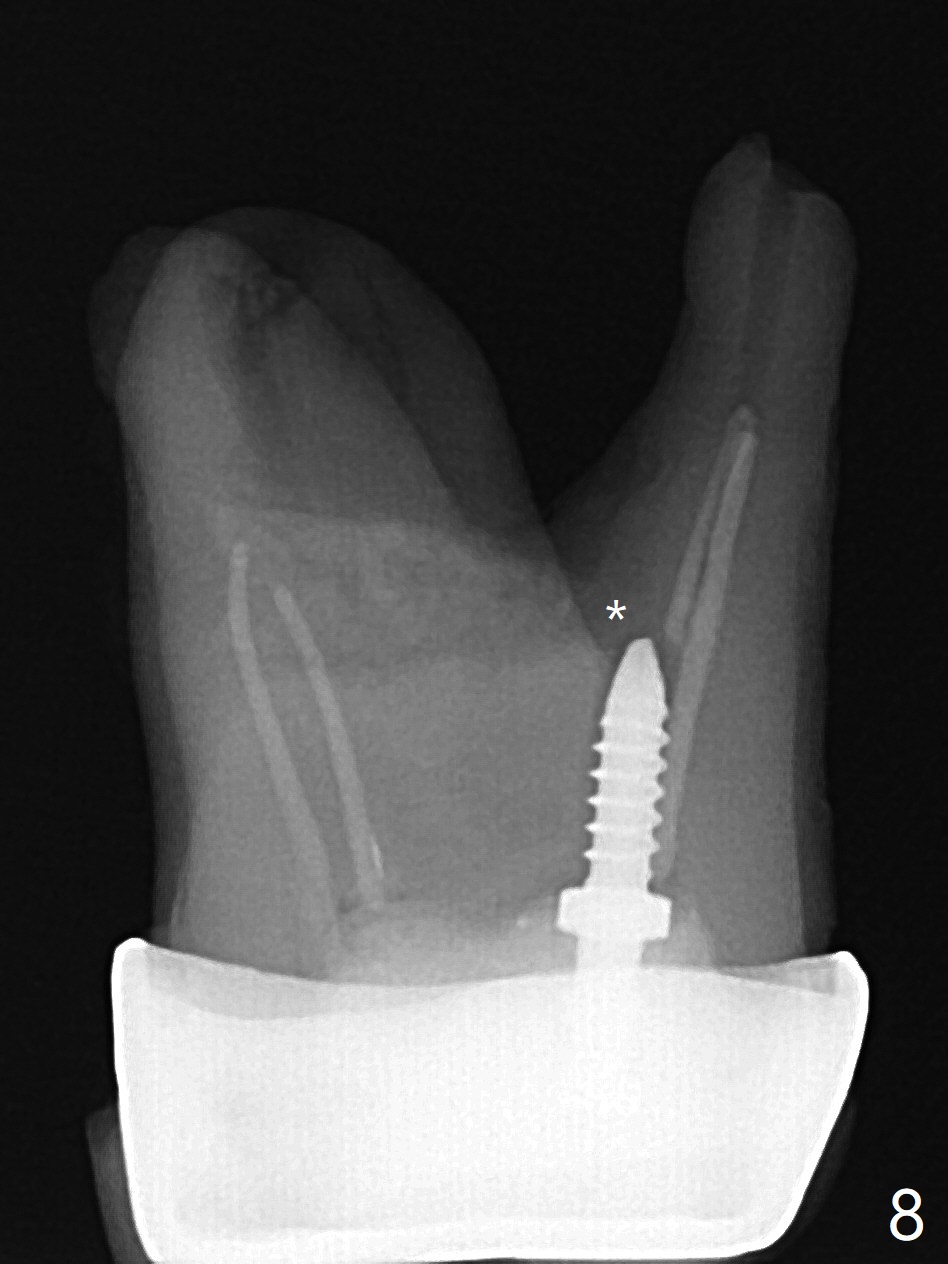
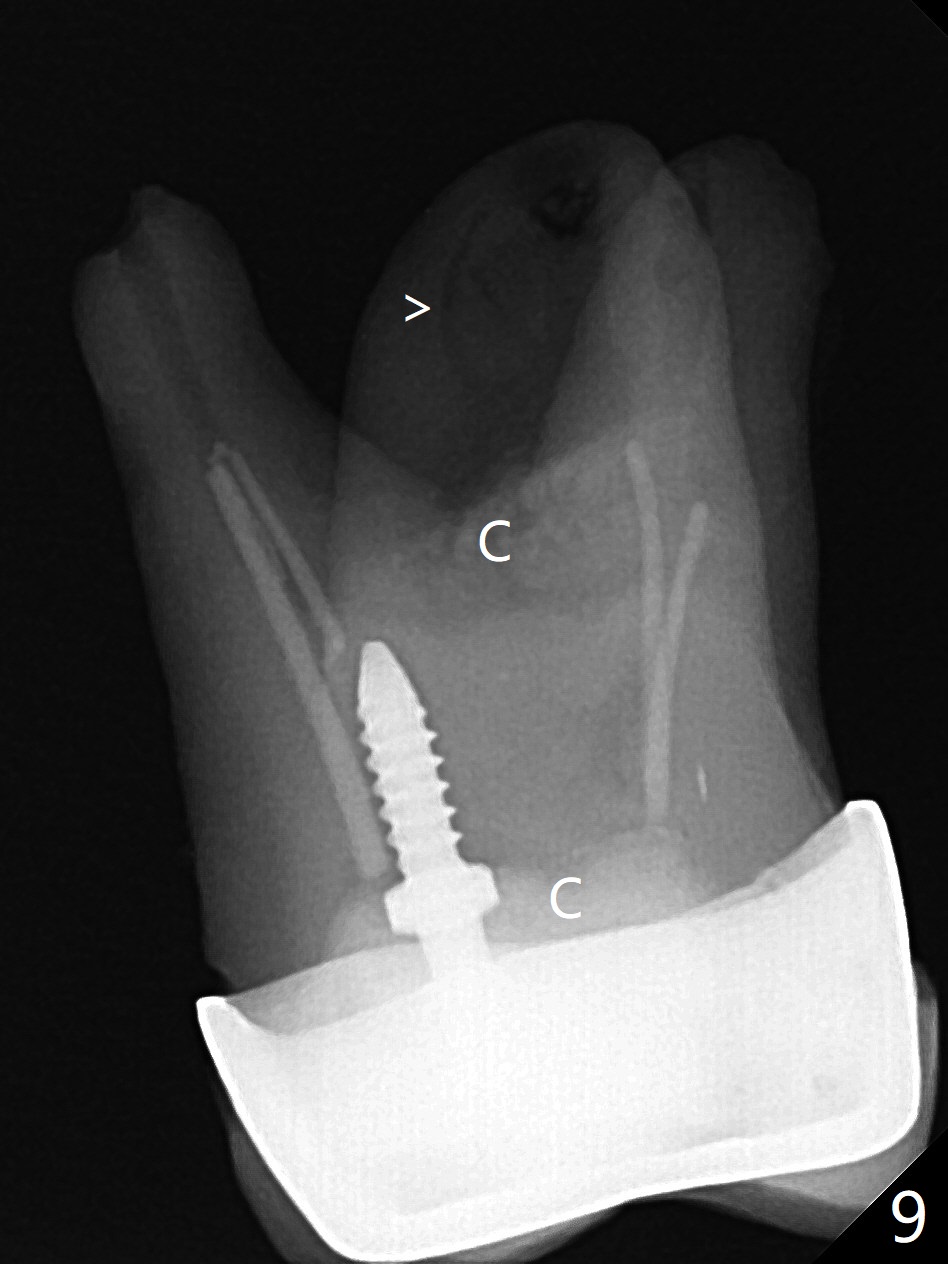
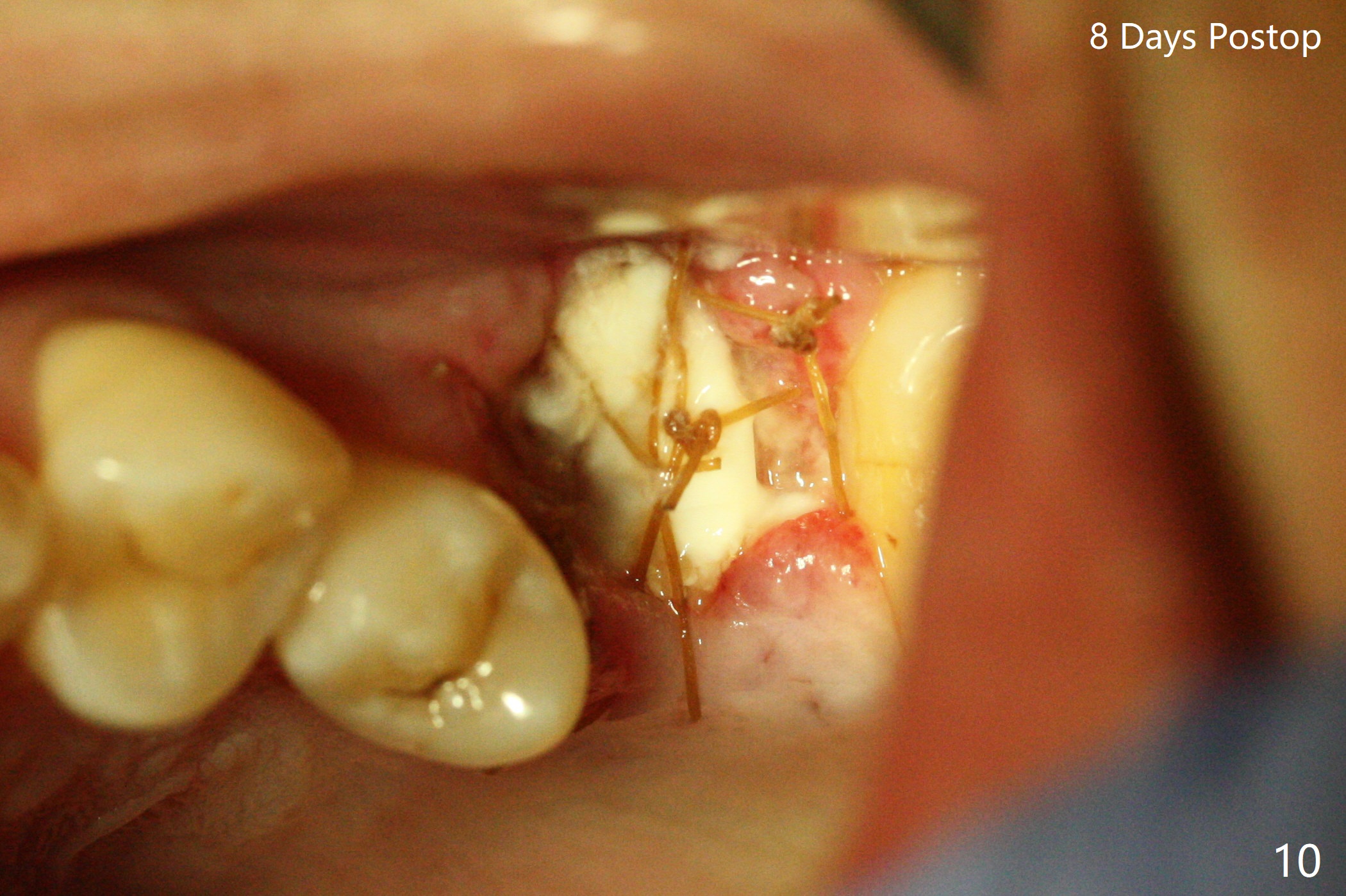
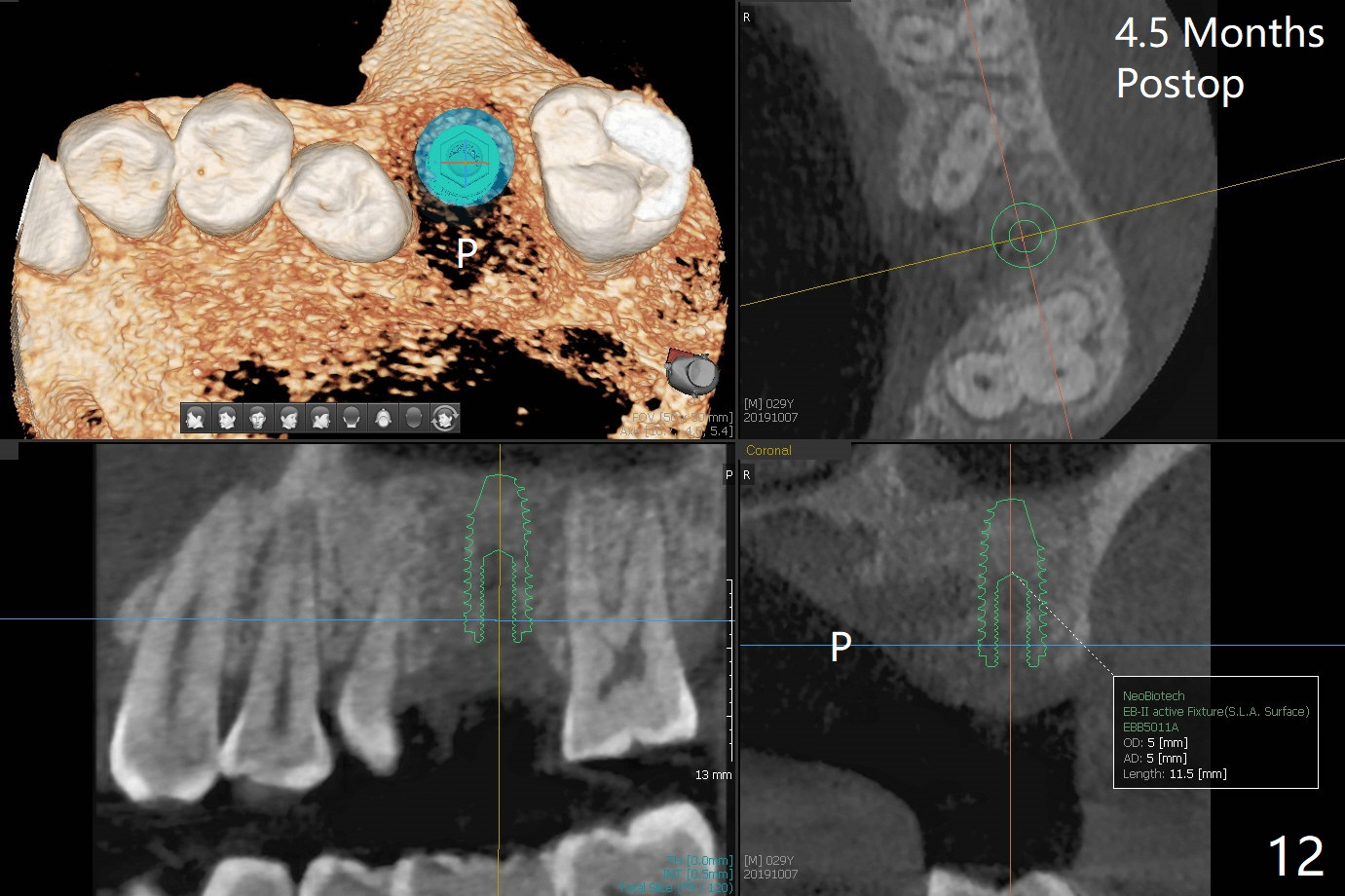
A 29-year-old man has pain in the upper left quadrant. It appears that the tooth #14 has endo and post failure with palatal fistula (Fig.1,2). The septum is almost non-existent; the palatal wall is low, while the sinus floor is present. Sticky bone is placed first against the defective palatal wall and presumably pushed as high as to the sinus floor (Fig.3-5). PRF plug/membrane and 6-month membrane are used to close the socket with 4-0 Chromic gut suture apparently securely, followed by periodontal dressing. Examination of the extracted tooth shows granulation tissue between the roots (Fig.6 *). Underneath the granulation tissue is cement-like material (Fig.7 C). Distal-to-mesial X-ray examination shows possible furcation perforation (Fig.8 *), while mesial-to-distal one the cement-like material in the furca and pulpal chamber as well as MB2 (Fig.9 >). The patient returns 8 days postop, reporting pain reduction, but wants to have #16 extracted. The periodontal dressing is loose, but stuck with 2 sutures underneath. When the dressing is removed, the wound looks normal (Fig.10). In fact the dressing is re-applied. The 6-month membrane has lost 1 month postop. The majority of the socket heals except the palatal (Fig.11 *), as related to the existing palatal fistula/defect (^). Orthodontics is being considered. If the buccal plate collapses 4.5 months post extraction, socket shield should have been done. In fact the buccal plate is robotic, while the bone density is low palatal in CT (Fig.12).
Return to
Upper
Molar Immediate Implant,
Trajectory
II
Xin Wei, DDS, PhD, MS 1st edition
05/22/2019, last revision
10/19/2019