


 |
 |
 |
 |
|
 |
Extraction
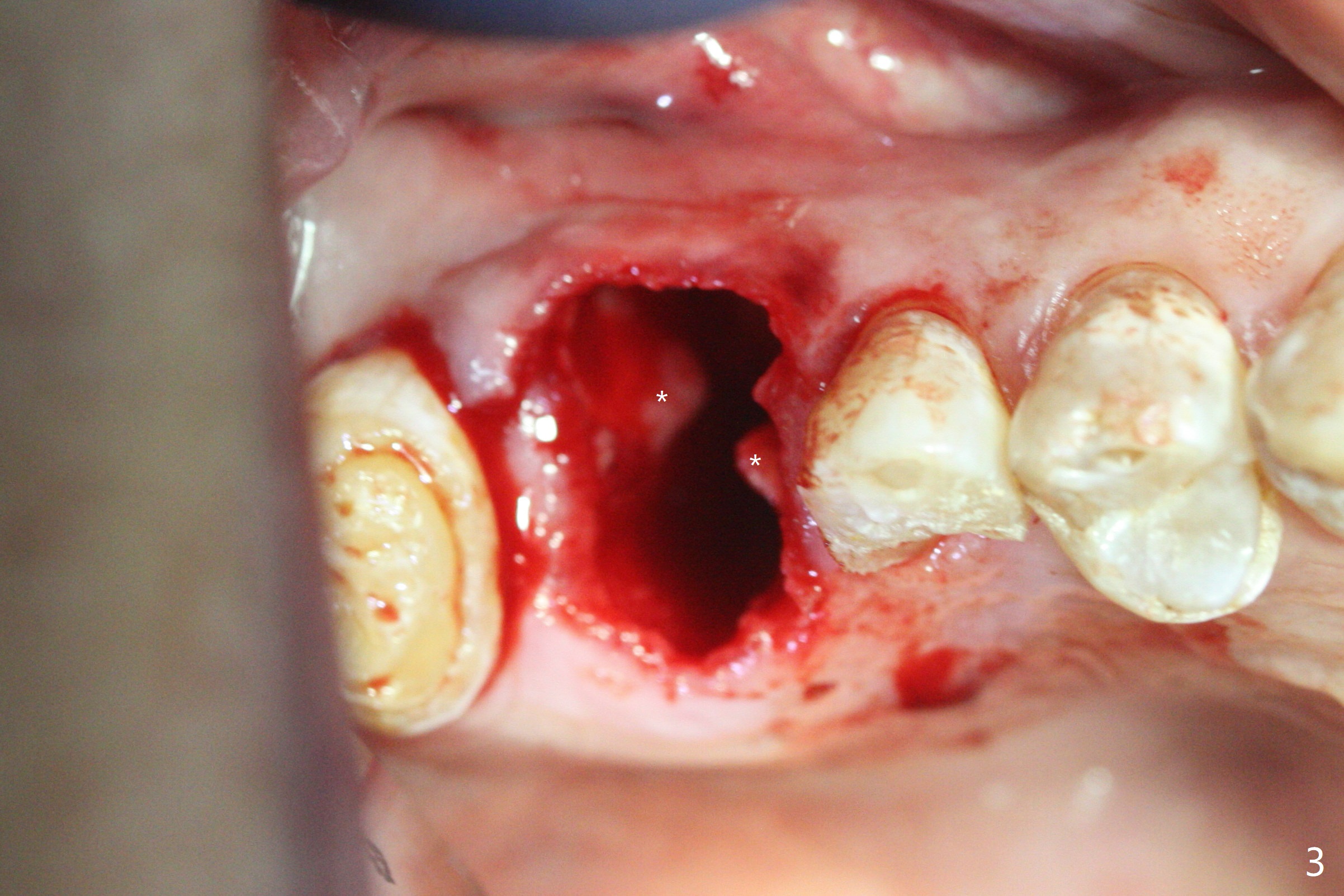
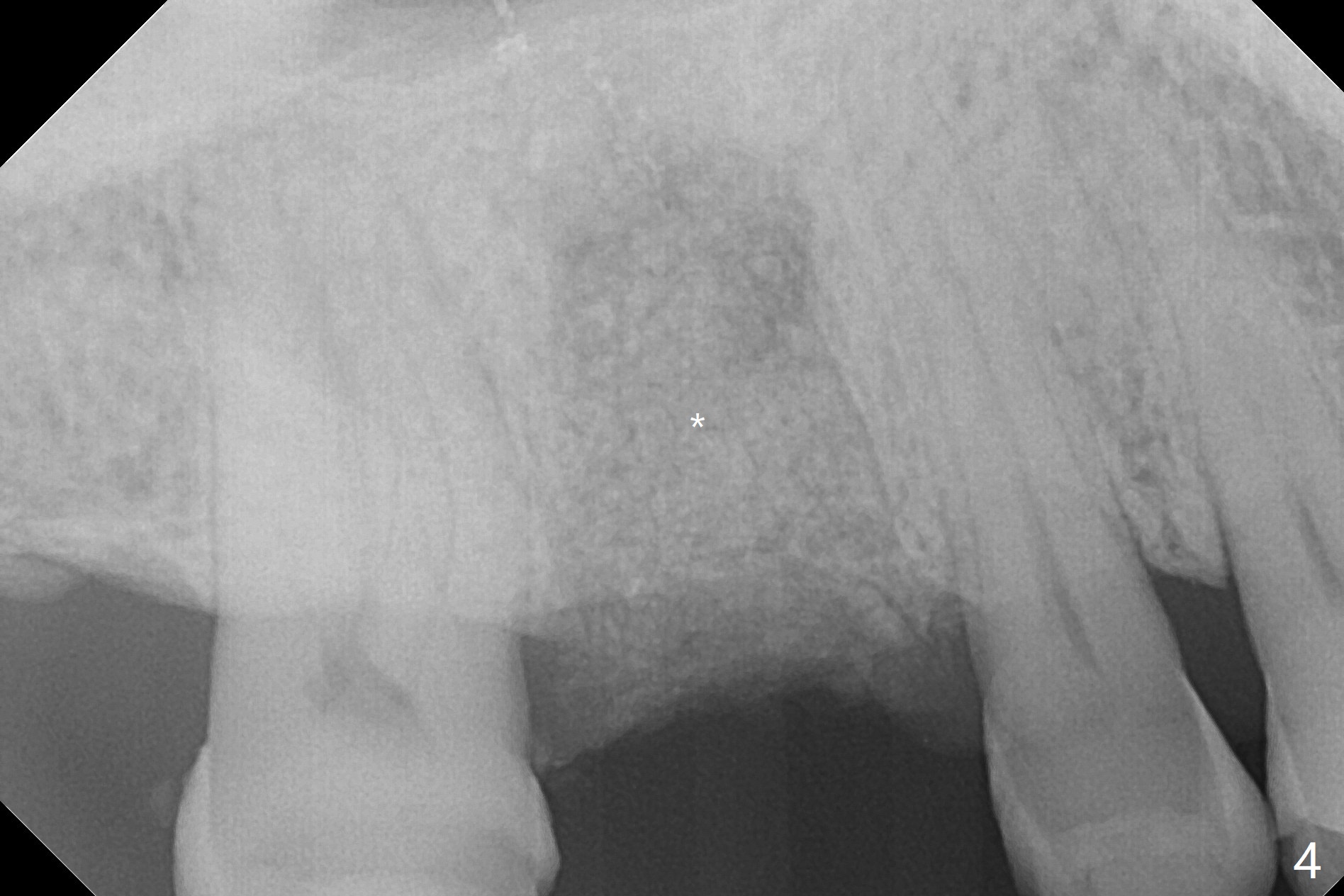
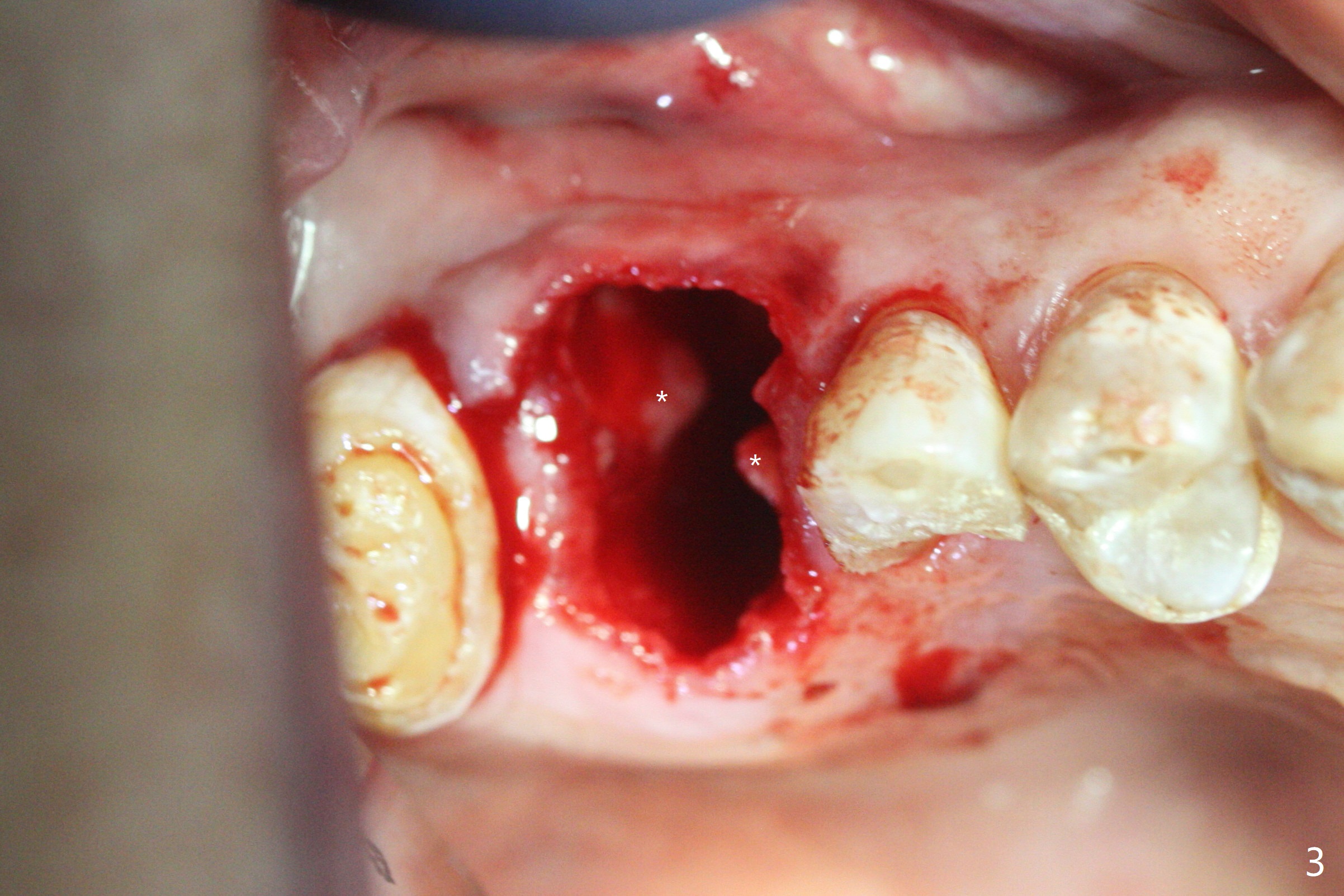
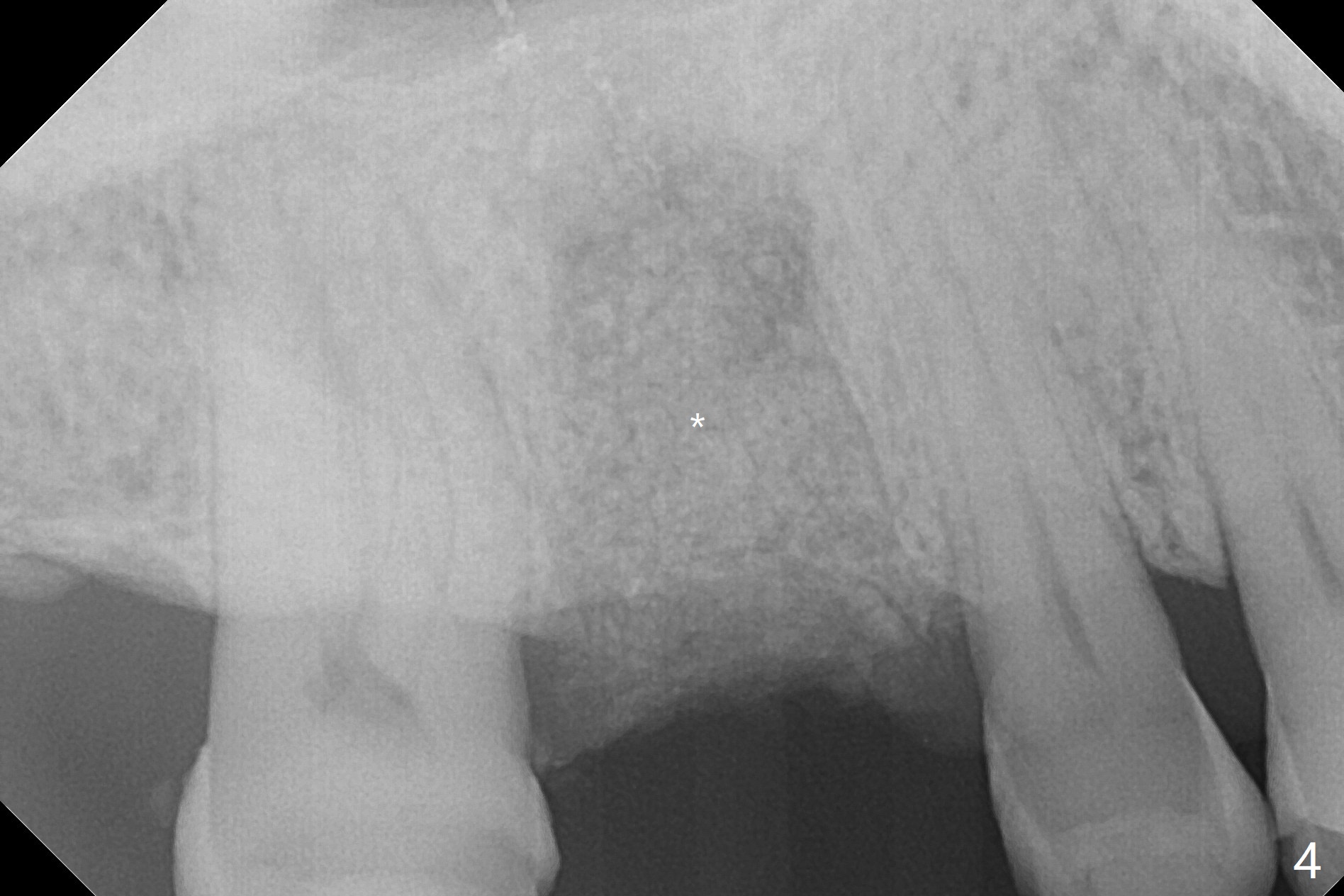
for Bruxer
A 56-year-old man with signs of bruxism (multiple occlusal wear and tear, Fig.1) returns from an endodontist office because of failed RCT retreatment at #3 (Fig.2 (* palatal swelling; > fistula)). After difficult extraction, the socket is large without much septal bone (Fig.3 *). Because of lack of the apical native bone, immediate implant is not placed. If it has to be done, a large and long one is required. Instead socket preservation is finished (Fig.4 *). The socket is 20 mm deep, while the shank of surgical curettes is 20 mm. It appears that the most apical granulation tissue is hard to be removed. When 7-day oral Clindamycin is finished, the patient returns with chief complaint of recurrent pain and fistulae. In fact the palatal fistulae are flat without erythema. He returns asymptomatic 2 weeks postop; the fistulae are disappearing (Fig.5 ^) and the socket is healing (Fig.6).
Return to
Upper Molar
Immediate Implant,
Trajectory
Xin Wei, DDS, PhD, MS 1st edition
02/21/2019, last revision
03/09/2019