


|
|
|
||
|
|
|
Osteotomy and Orthodontic Extrusion
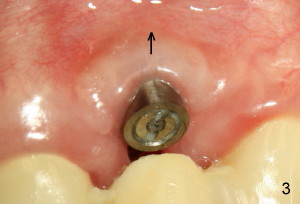
A D implant (4x16mm) was placed too apically and buccally (Fig.1). Originally, implant placement with bone expansion was designed to correct soft and hard tissue deficiency associated with #10 edentulism. Three weeks postop the gingiva (*) is attached to the implant (I). Five months postop the gingiva shrinks more apically (arrow in Fig.3), corresponding to postop bone resorption proximal to the implant (compare arrowheads in Fig.2,4).
It appears that the malpositioned position needs combined surgical and orthodontic correction. Two types of incisions are designed for osteotomies. Incision 1 (along gingival sulcus and two accessory in Fig.5) provides visibility and determines the extent of osteointegration, whereas Incision 2 (two incisions lateral to implant in Fig.7) keeps gingiva-implant seal/attachment intact.
Combined surgical bur and thin osteotomes (Tatum) will be used to finish osteotomies (Fig.6 black lines). While keeping the palatal periosteum attached, the bone block will be separated. After soft tissue healing, orthodontic extrusion of #10 will begins with brackets to be placed from #6 to #13. The bone block and more importantly the gingiva will be directed downward (Fig.8 arrow) as well as lingually. If orthodontic extrusion has resistance, a mini-implant will be used, probably in the lower jaw.
Prior to osteotomy, a ten-degree offset abutment will be placed, cemented (temporarily?) and prepared initially. A temporary crown is fabricated in a position normally to the implant (malpositioned). When the temporary crown is moved to normal position, the once malpositioned implant will be expected to be normal in position with normal overlying soft tissue configuration.
Hello Dr. Wei. The implant appears to be well integrated. Therefore, this problem can be solved by a segmental osteotomy. The fact that the implant is too far anterior can be corrected with asymmetrical preparation. The too high position can be corrected only by replacing it or a segmental osteotomy moving the implant and its integrated bone in an inferior direction. Dr. Borgner 08/31/2011
Yes when place too apically the bone would die back a little. NOW I always use
my periodontal probe to measure the tissue thickness before I decide how deep I
place the implant. Always try to leave
about 1/2 to 1 mm of the etch surface above the bone. Also always try to pack a
little bone graft to the inter-proximal space, then use a mini flap to close off
the expanded gap without tension for the fibrin seal. About the buccal placement
issue, it does happen. That is why this
is difficult procedure to master. You have to focus at all time, and monitor and
adjust the direction of the osteotome. There are two solutions
1. Use pink
porcelain to cover the cervical area. Patient may or may not like it.
2. Also
give patient a choice of surgical correction of it by vascularized segmental
osteotomy. THAT MAY ALSO HELP TO CORRECT THE VERTICAL ISSUE TOO. Joseph
Lau, DDS 08/31/2011
Xin Wei, DDS, PhD, MS 1st edition 08/28/2011, last revision 08/31/2011