



 |
 |
 |
 |
 |
|
 |
||
Post-Implant Infection
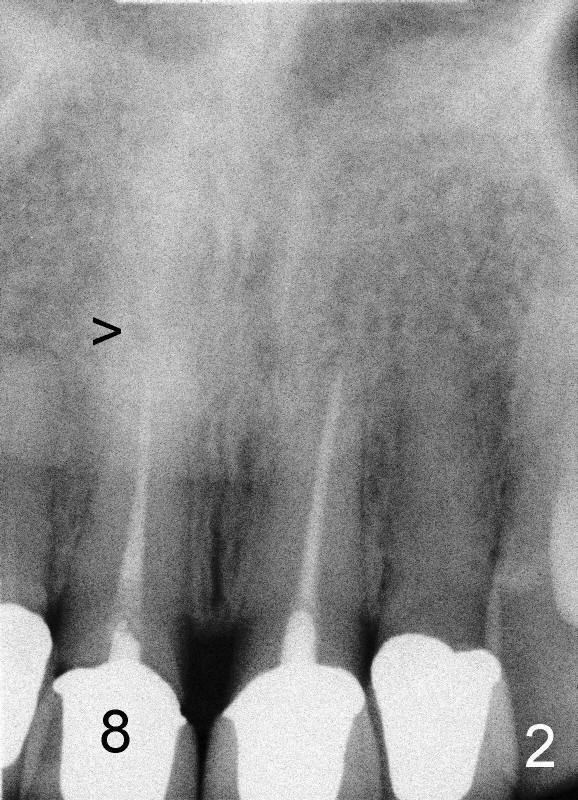
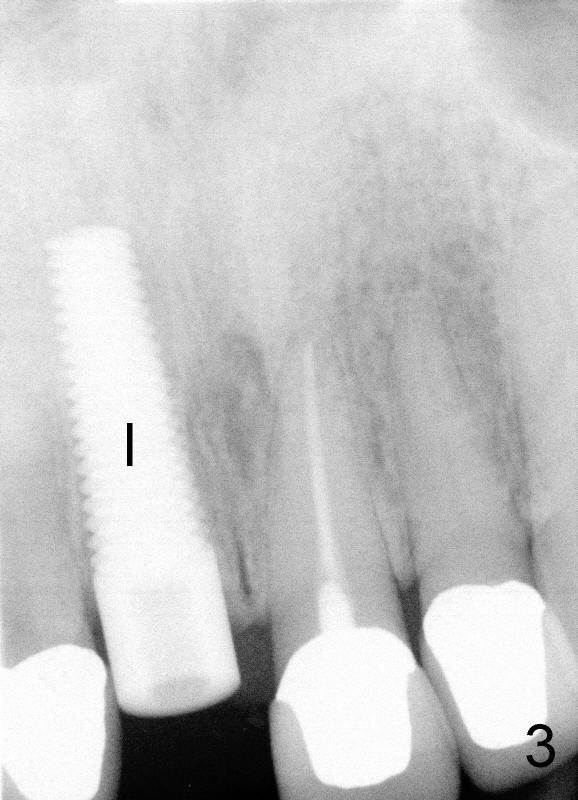
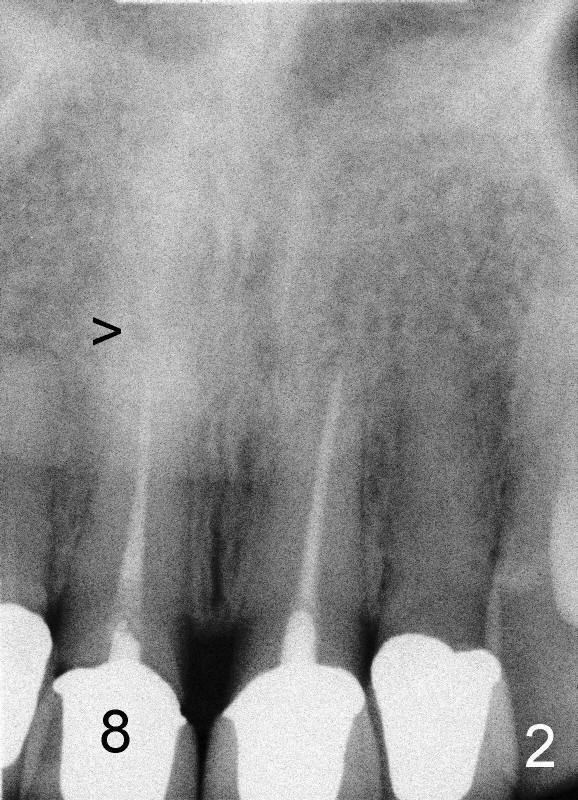
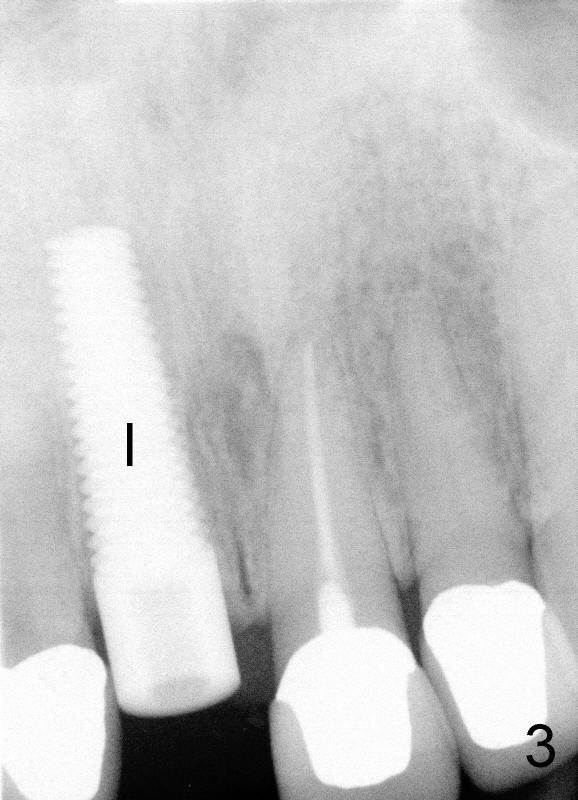
A 44-year-old lady has fractured #8 and agrees to have the tooth extracted after failure of recementation (Fig.1). Pre-implantation X-ray shows minimal periapical radiolucency (Fig.2: >). A 5x20 Tatum tapered implant is placed immediately after extraction (Fig.3: I). Perio dressing is placed and a flipper is delivered.
Six days post-op, the patient returned for follow-up. There is slight gingival erythema and edema over the implant. There is no contact between the flipper and the implant.
Sixteen days after surgery, the patient returned with chief complaint "I do not have pain, but there is a swelling". Exam shows that there is localized apical swelling with + fluctuance (Fig.4: *) and granulation tissue at gingival margin (>). Under local anesthesia, I & D is performed with sanguine exudate, buccal apical plate perforation with implant threads exposed. Tetracycline normal saline is used for irrigation. The patient was asked to return every 1-2 days for irrigation.
The patient felt better after I & D. She did not return for irrigation until ten days later (for Christmas). I & D incision heals. Swelling and granulation tissue re-appear (Fig.5,6). In two visits, the implant is stable.
Can we raise flap for more thorough debridement or just remove the implant?
Comments from Bernee Dunson DDS:
Comments from Dr. Borgner (Saturday, January 12, 2013 10:22 AM): I would also graft the defect along the root of the cuspid at the time of implant placement with irradiated bone. I agree with the comments of Dr Dunson concerning the infected implant. Since the implant shows no mobility, There is a good chance it will heal now that you have I and D the area. My criteria for placing an implant into an immediate extraction socket: 1- always insure the osteotomy is carried through the apex of the socket into healthy bone above or below the original socket(this removes apical pathology if present),2- always remove the very inner layer of the cribiform plate within the socket(again to remove possible pathology), 3- if grafting is necessary and there was ANY suppuration originally present in the socket I would use a synthetic graft ( Biogran,Osteogen,Perioglass) before placing the implant.
Xin Wei, DDS, PhD, MS 1st edition 01/08/2013, last revision 01/13/2013