






 |
||||
 |
 |
 |
 |
|
 |
 |
 |
 |
|
Treatment of Pain after Lower Third Molar Extraction
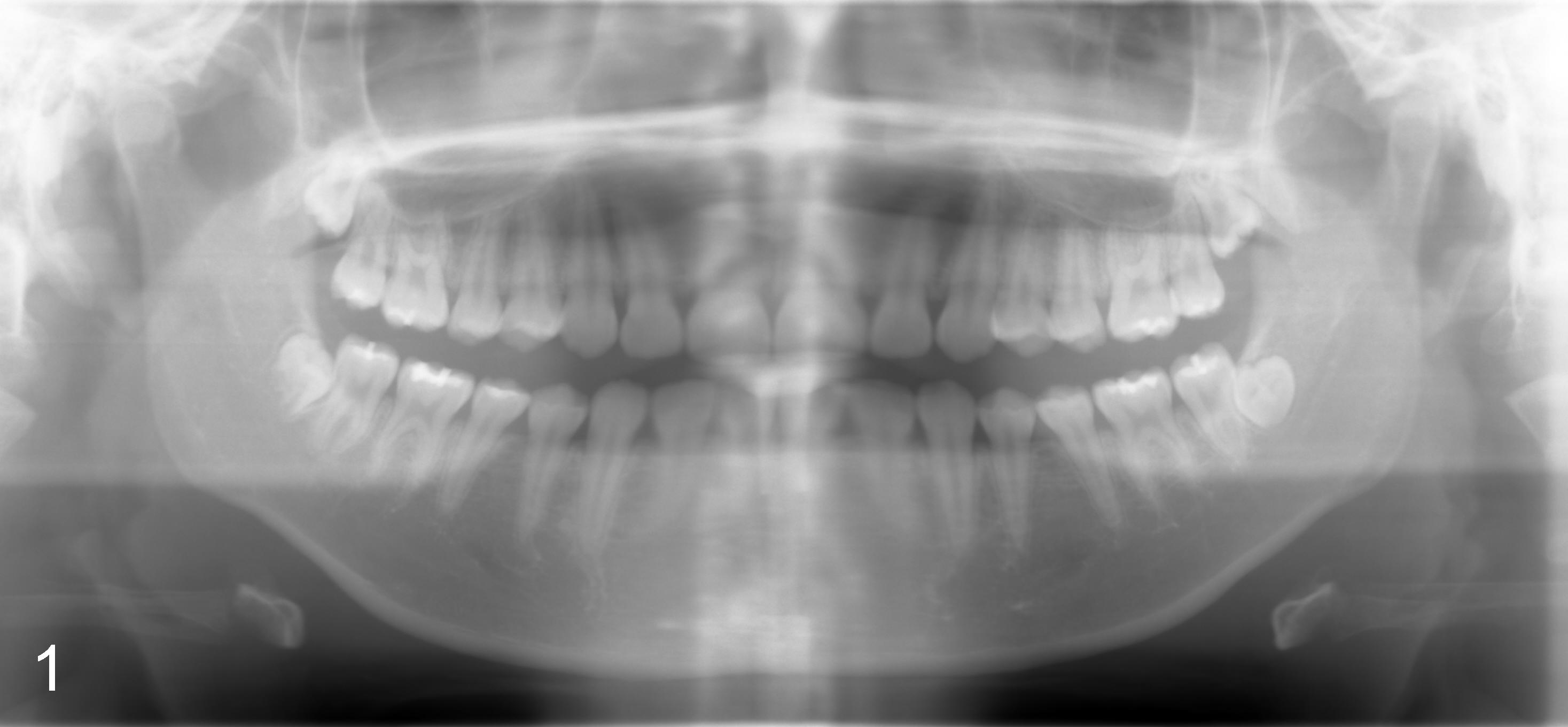
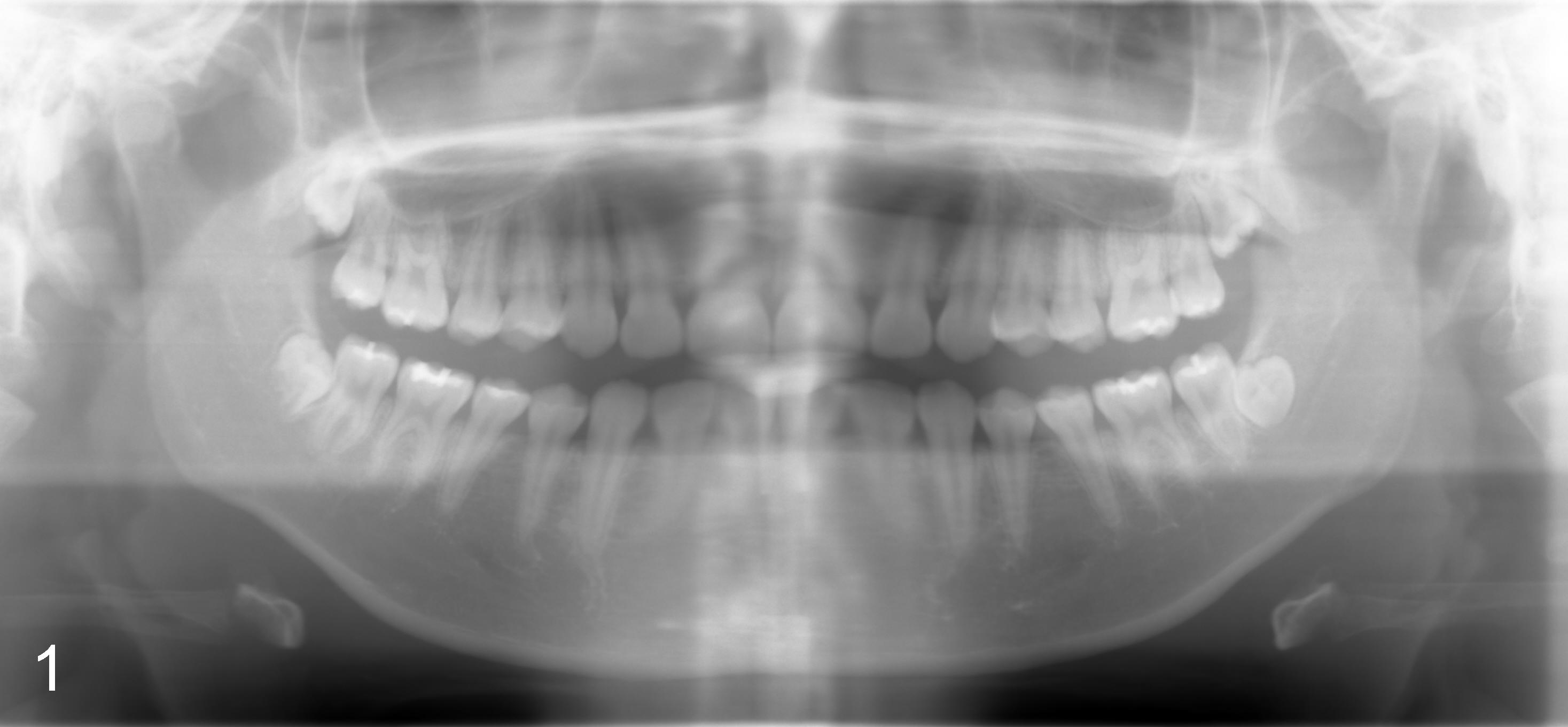
Sixteen-year-old (10 month) Asian female returned to clinic for #32 ext under local anesthesia. Panoramus was taken 2.5 yrs earlier (Fig.1). Surgery includes hockey stick incision, buccal trough, elevator, forceps extraction (Fig.2,3 (B: buccal view, L: lingual)), curettage of tooth bud sac and plain gut suture. Post-op medication consists of Amoxicillin, Lortab and Medrol Dosepak. A month later, the patient returned for #17 with chief complaint (cc) "a lot of swelling after extraction". Surgery and post-op med are the same as for #32 except that the tooth #17 was sectioned several times. The tooth fragments were not saved. It appears that the tooth #17 had yet to develop the roots. Five days after extraction, the patient returned with cc "my lip is still numb". Paresthesia was defined as shown in Fig.4. Vitamin B complex (B1, B12) was recommended. Two days later, she was asked to return for panoramus (Fig.9 as compared to that of pre-op at the same magnification). The bottom of the socket is close to the inferior alveolar canal (IAC). Two weeks post-op, paresthesia was reduced as facial edema subsided (Fig.5), but the patient's main concern was "my lower left teeth (especially incisors) are tender. I cannot chew on the left side". The patient's mother reported that the patient screamed suddenly when she ate. The pain did not subside for two months. Oral and maxillofacial neurosurgeon and cone beam CT were suggested.
The pain is somewhat similar to trigeminal neuralgia. Carbamazepine (Tegretol) was prescribed at 100 mg PO Bid for two weeks. No improvement was reported in the first week. In the early second week, the patient reported sudden reduction in pain. The dose was increased to 200 mg Bid on the third week. The patient reported continuous improvement in pain control with increase in dose. The pain completely disappeared when the patient finished Carbamazepine at higher dose for two weeks. It seems that Carbamazepine can be tried for trigeminal-like pain after 3rd molar extraction.
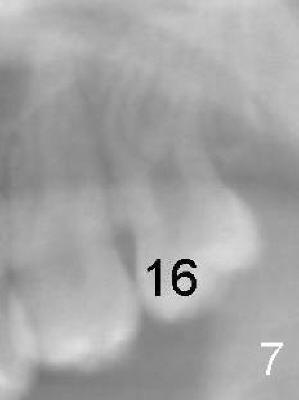
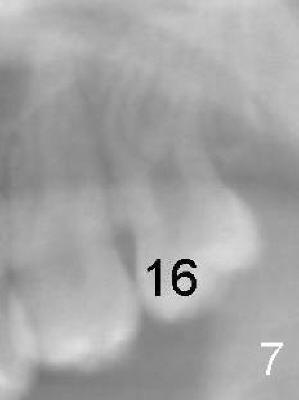
How to avoid inferior alveolar nerve injury during third molar extraction? Although the teeth #16 (compare Fig.6 and 7) and #32 (compare Fig.1 vs. 2/3) show more root development in 2.5 years, the socket of the tooth #17 does not appear to separate from IAC (compare Fig. 8/9) probably due to lingual impaction. To avoid nerve damage, control the depth of surgical bur when making buccal trough and/or sectioning the tooth if it has close relationship to IAC. There appears to have been no change in crown relative to IAC in 2.5 years in this case (due to lingual impaction). In addition, update pre-extraction X-ray (panoramus) more frequently for patients under the age of 20 or take CBCT if indicated.
Xin Wei, DDS, PhD, MS 1st edition 01/13/2011, last revision 04/08/2011