








 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
|
 |
 |
 |
 |
Apical Foramen Leak
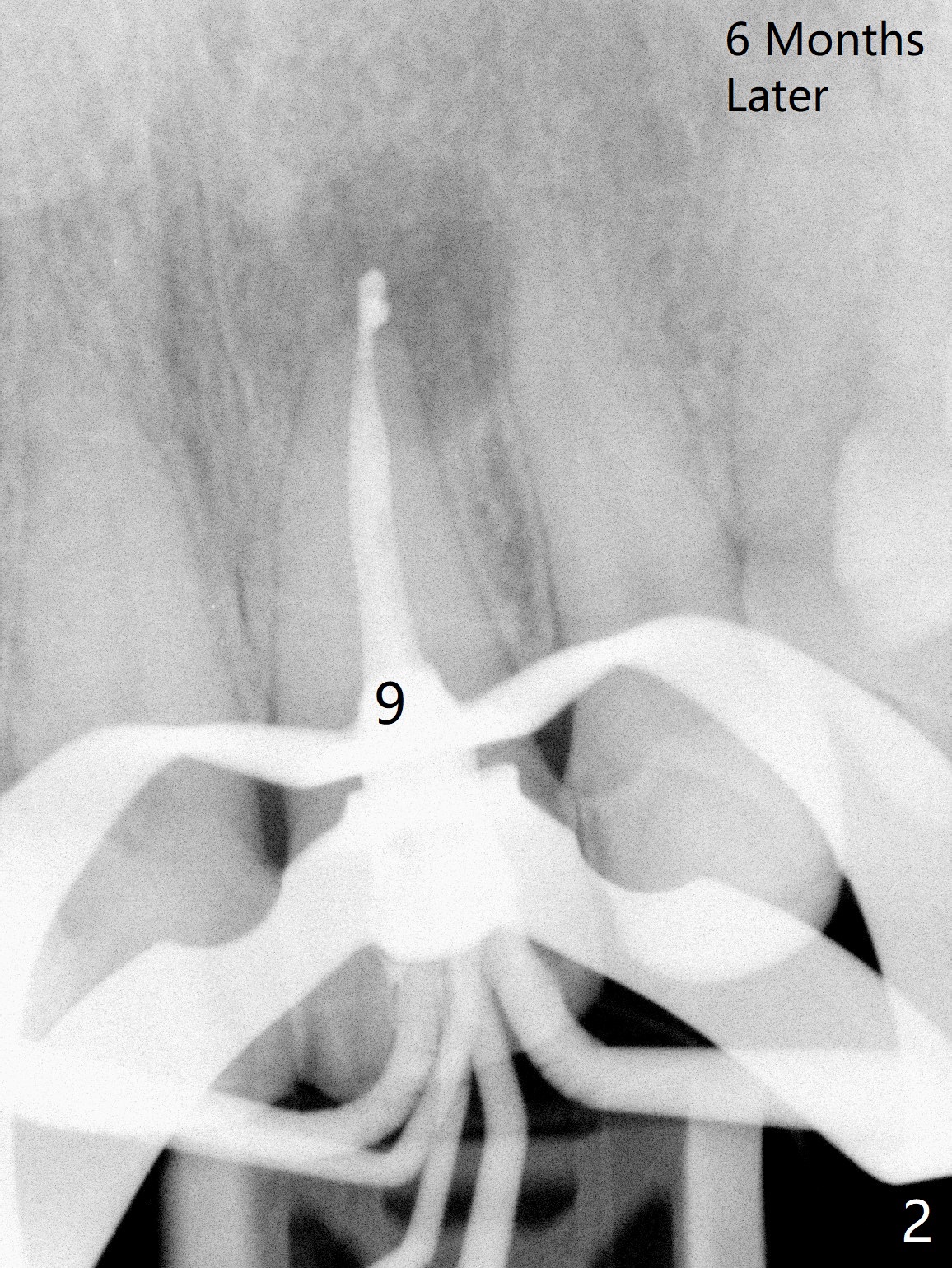
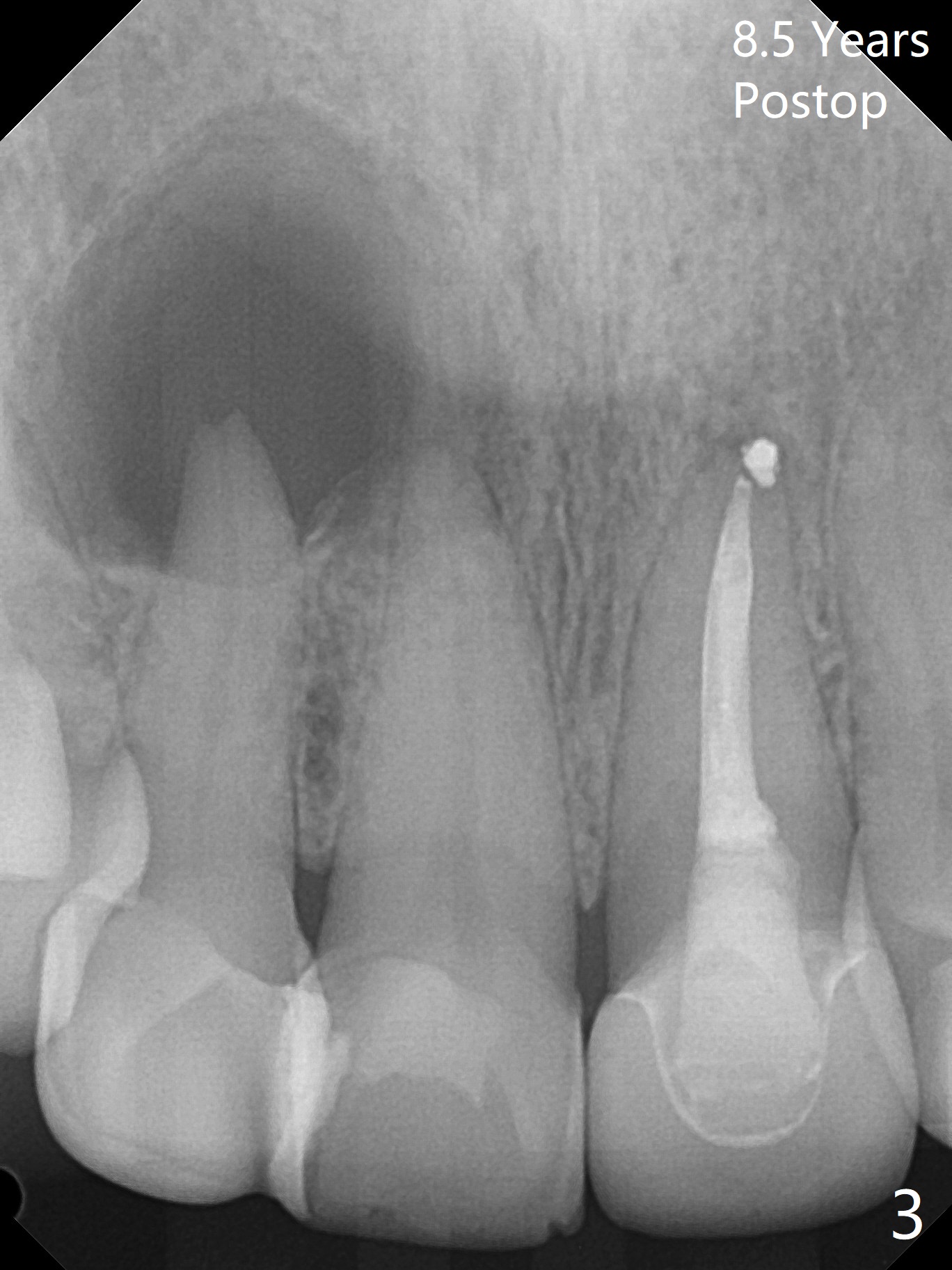
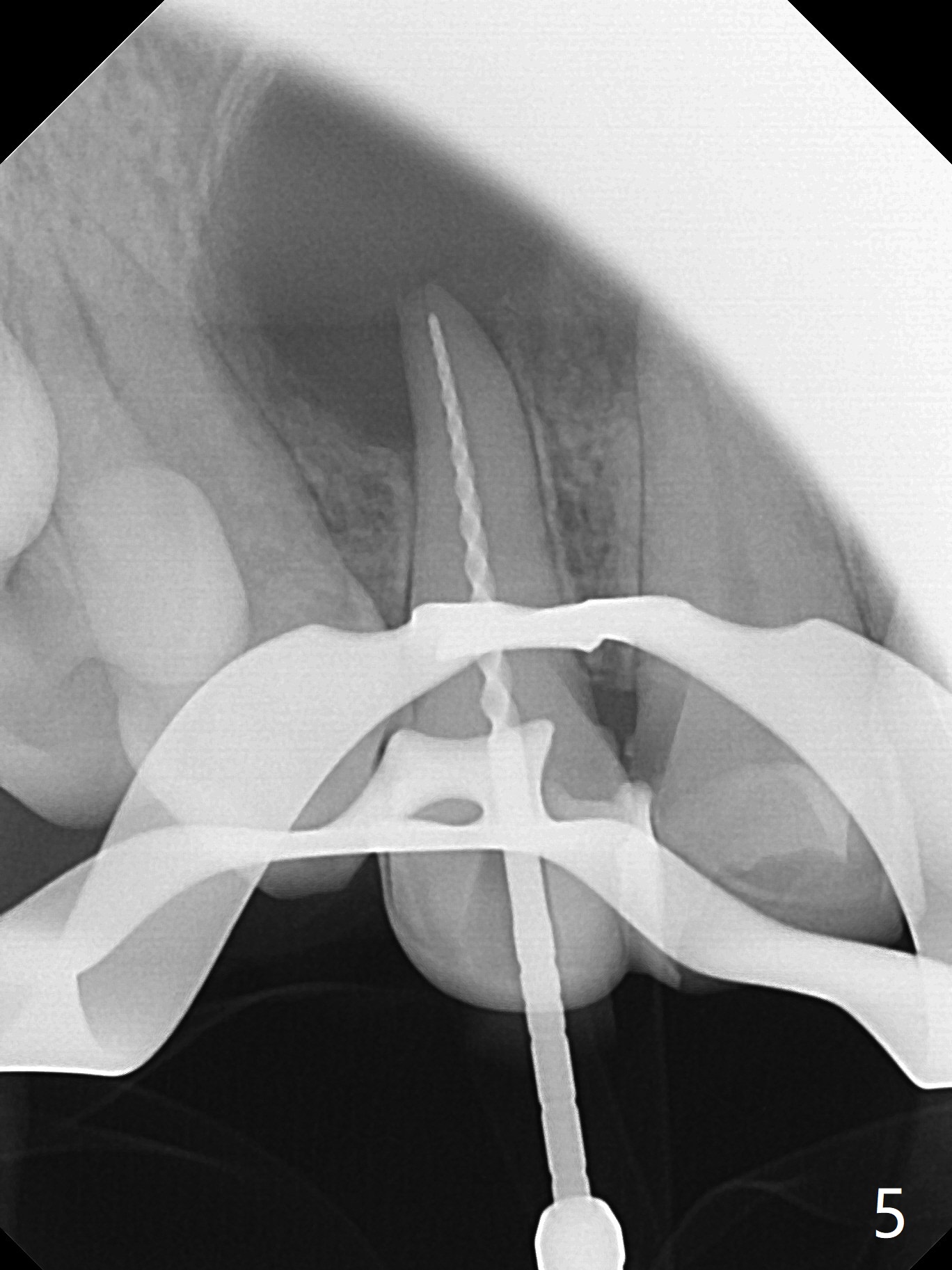
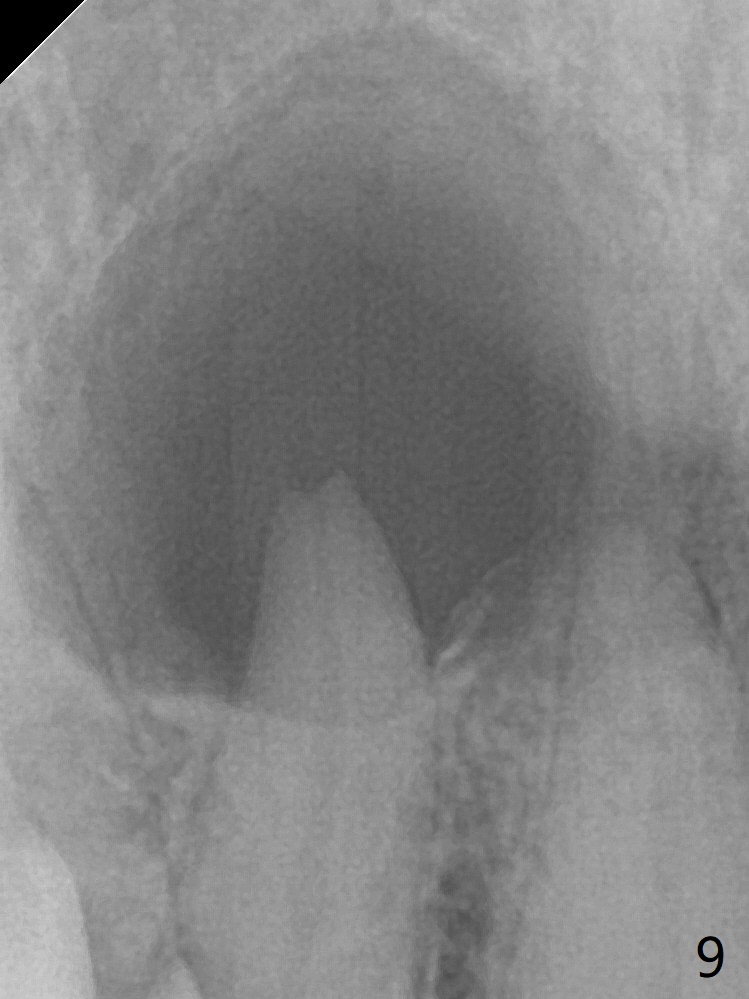
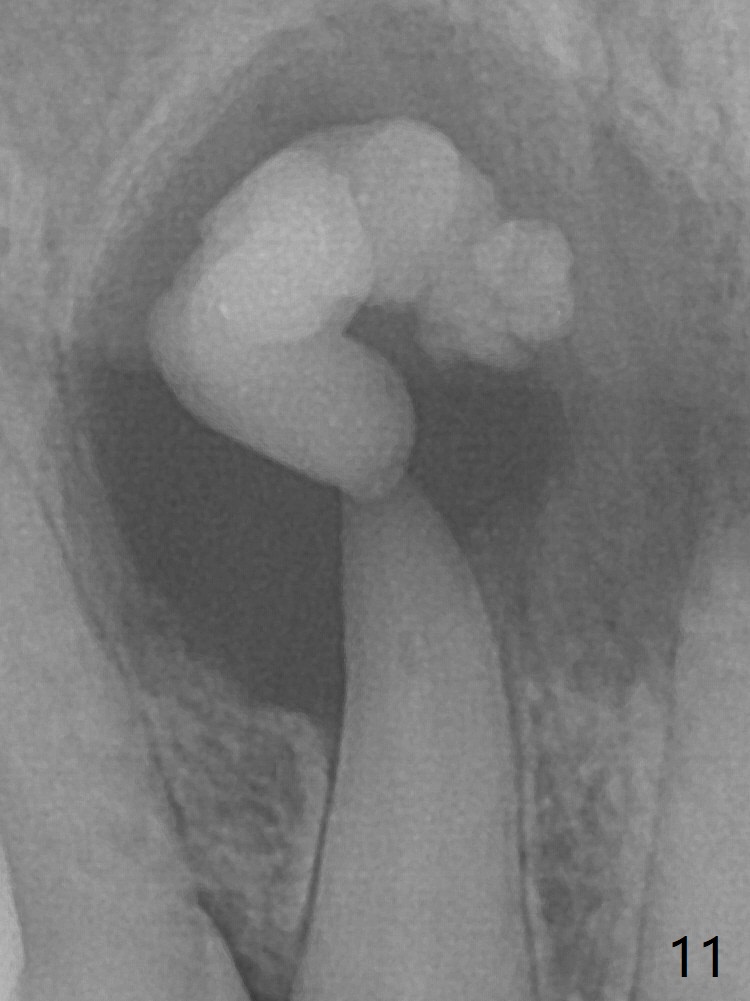
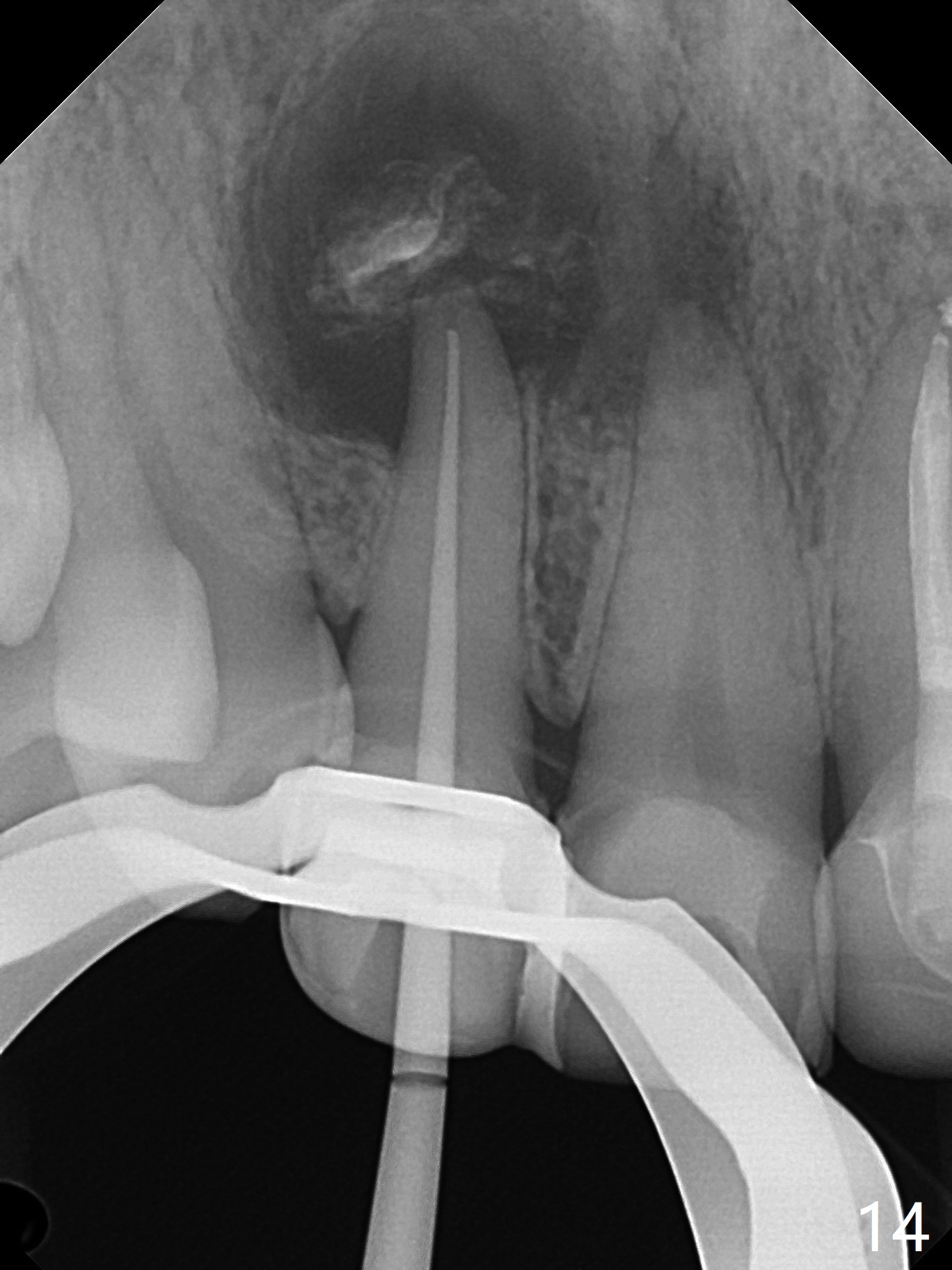
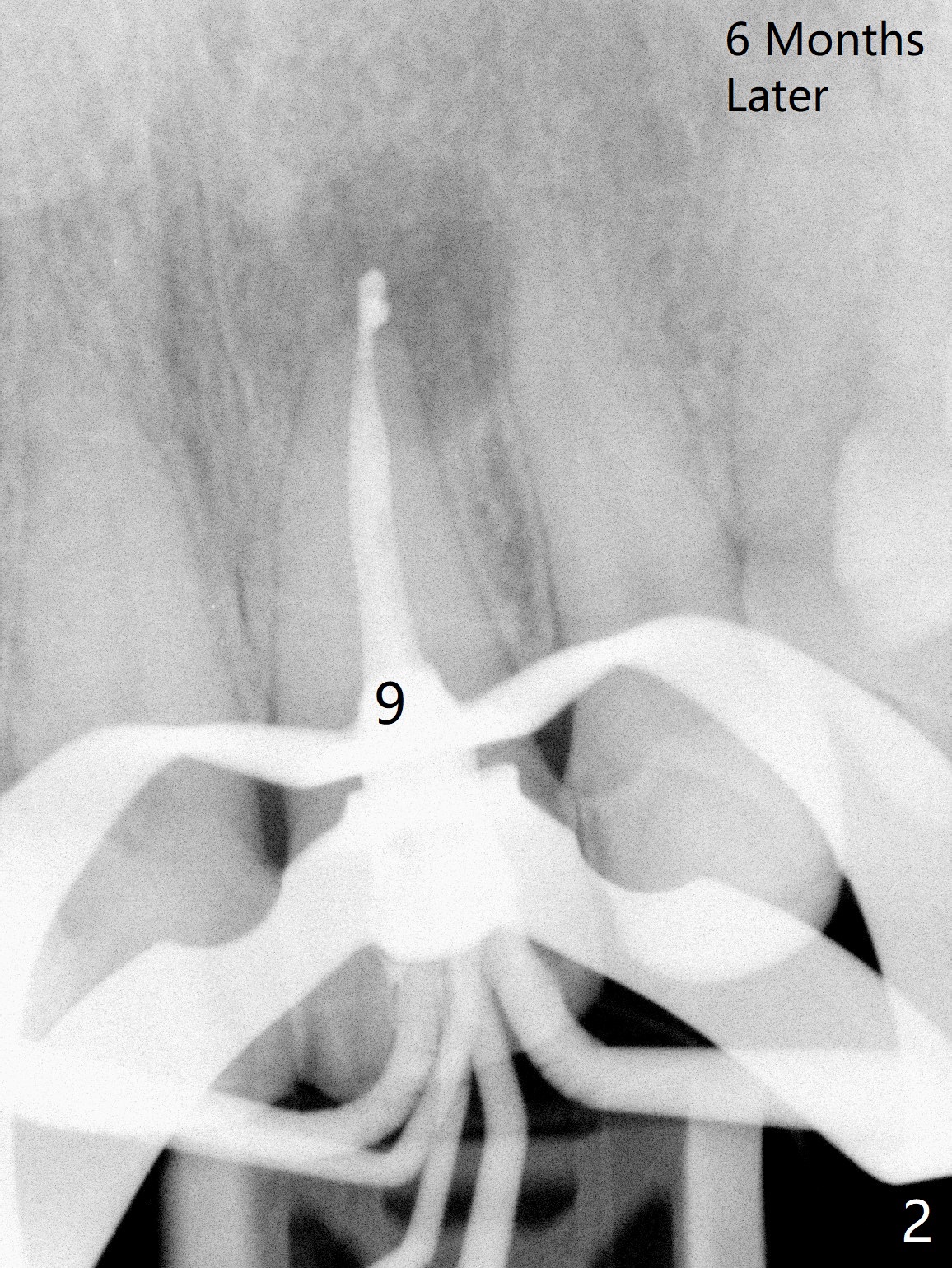
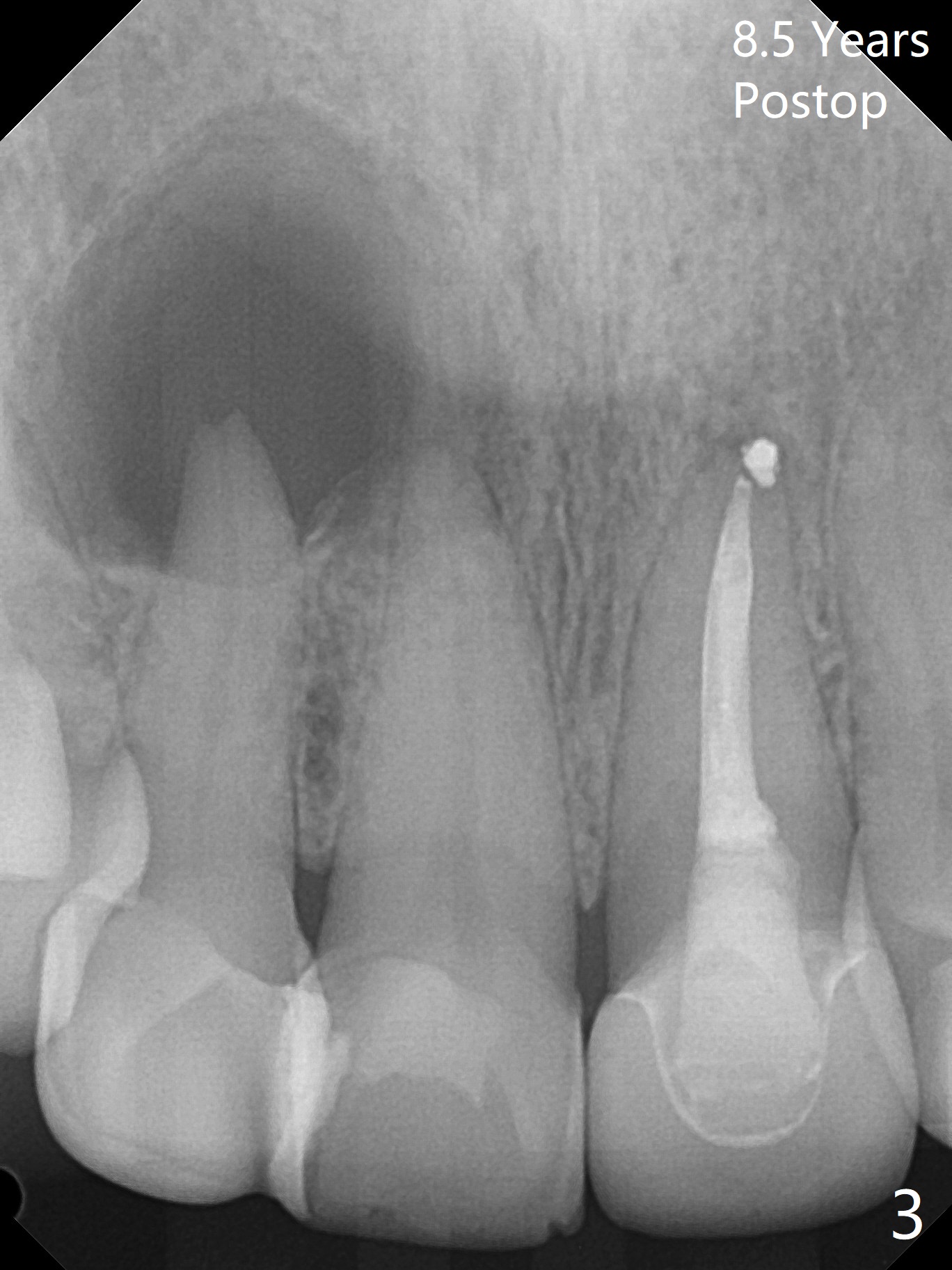
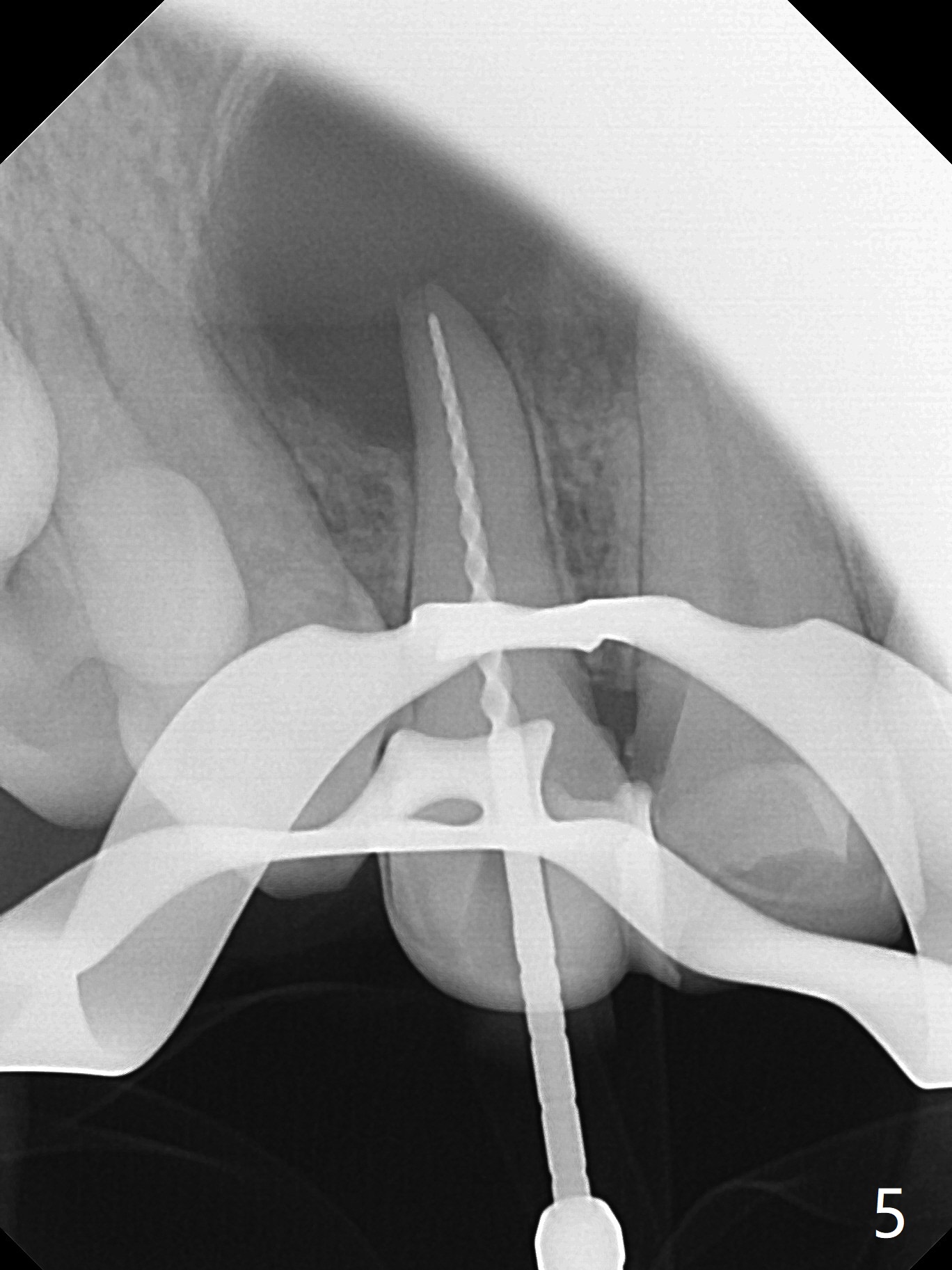
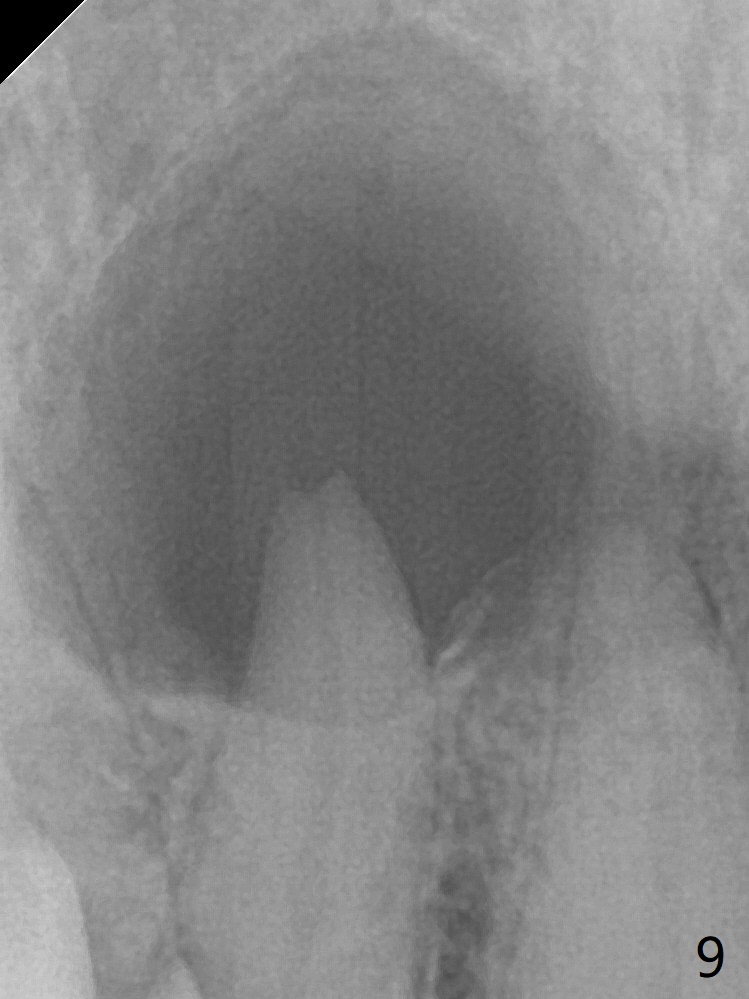
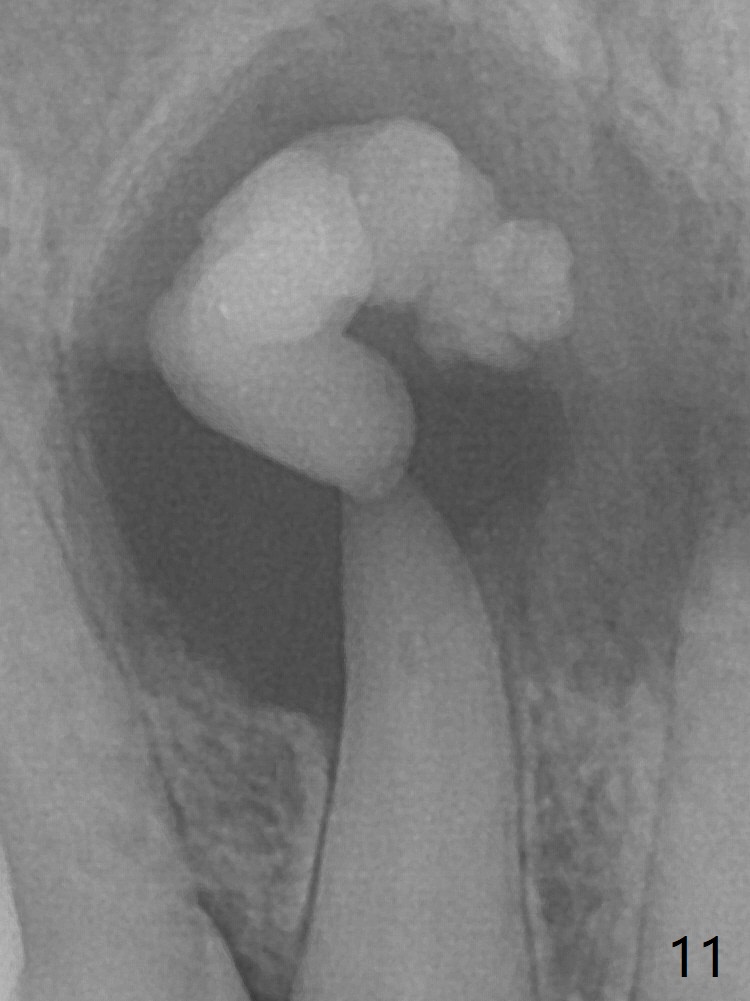
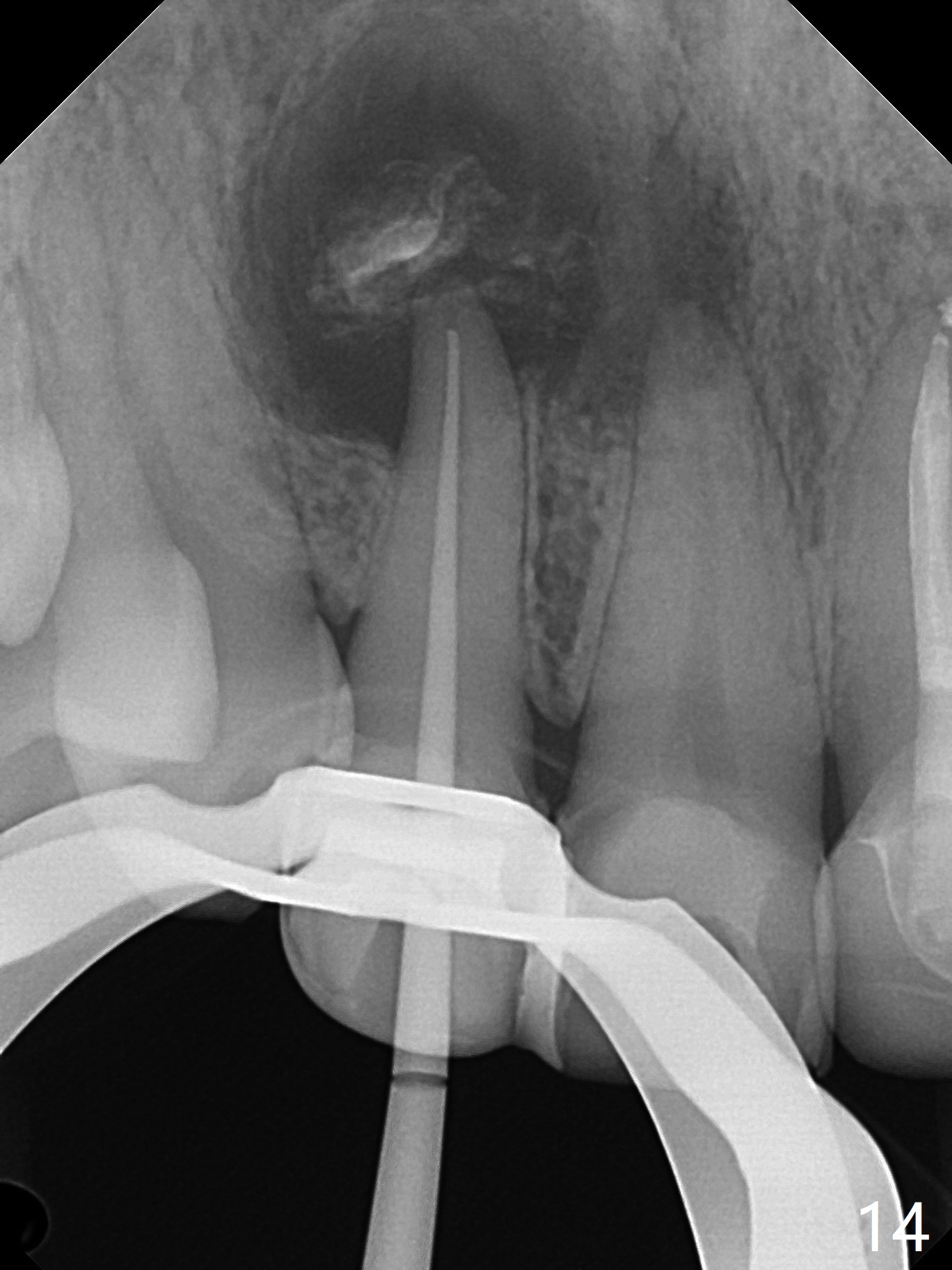
A 47-year-old woman (dental phobic) presented to clinic 9.5 years ago with periapical radiolucency (PARL) at #7 and 9 (Fig.1). RCT was done at #9 because of fistula and symptom 6 months later (Fig.2). While PARL increases at #7 without symptom, that at #9 disappears 8.5 years postop. Three months later, the patient returns for #7 RCT because of the abscesses (Fig.4 *) and pain. Intraop PA is taken with a 30/.06 rotary file in the canal with 19 mm working length (Fig.5). After use of #15 hand file for 20 mm, Ca(OH)2 paste is applied in the canal. When the rubber dam is removed, the abscesses enlarge (Fig.6), which may be related to sodium hypochlorite leakage. A dental explorer is used to try to find a bony opening to the large PARL without success (Fig.7). A postop PA reveals the leakage of Ca(OH)2 paste (Fig.8). Review of the preop PA (Fig.3,9) and intraop PAs (Fig.5,10) shows possible apical resorption and open apical foramen, which is the basis for the paste leakage (Fig.8,11). Careful analysis (with magnification and room light off) of pre- and intra-op PAs should be able to avoid use of #15 hand file out of apical constriction and the complication. The abscess has receded 1 month later (Fig.12). The paste has been resorbed 1 month later (Fig.13). A 30/.06 Gutta Percha is inserted at 18.5 mm (Fig.14 vs. 30/.06 file at 19 mm, 15 file at 20 mm last visit). Fig.15 is the final PA after closure of the access with composite (Fig.15).
Return to Professionals Xin Wei, DDS, PhD, MS 1st edition 09/06/2019, last revision 10/04/2019