


,%20Vera.jpg)



 |
 |
 |
 |
,%20Vera.jpg) |
 |
 |
 |
 |
|
 |
 |
|||
1st IBS Anterior Immediate Implant
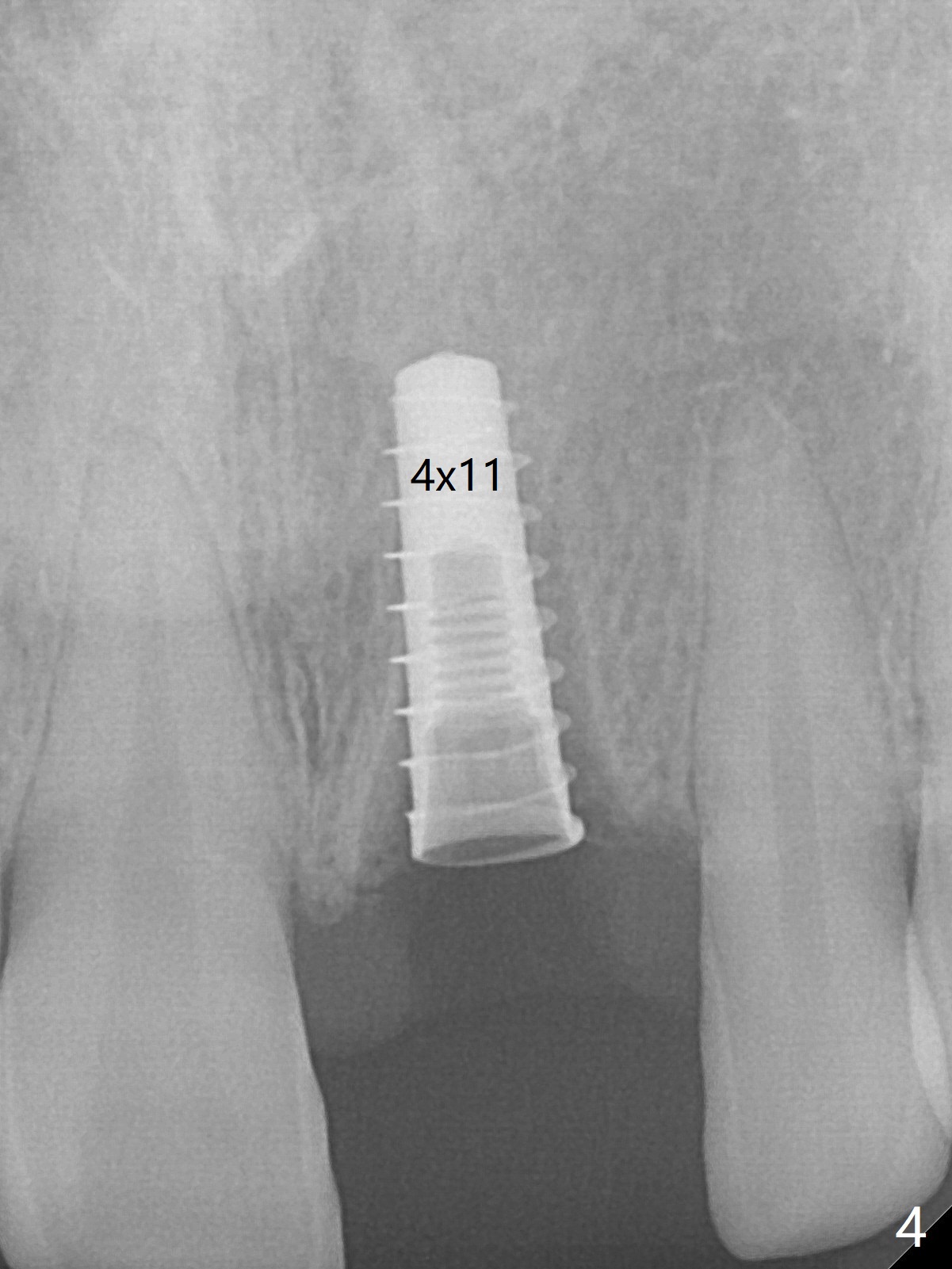
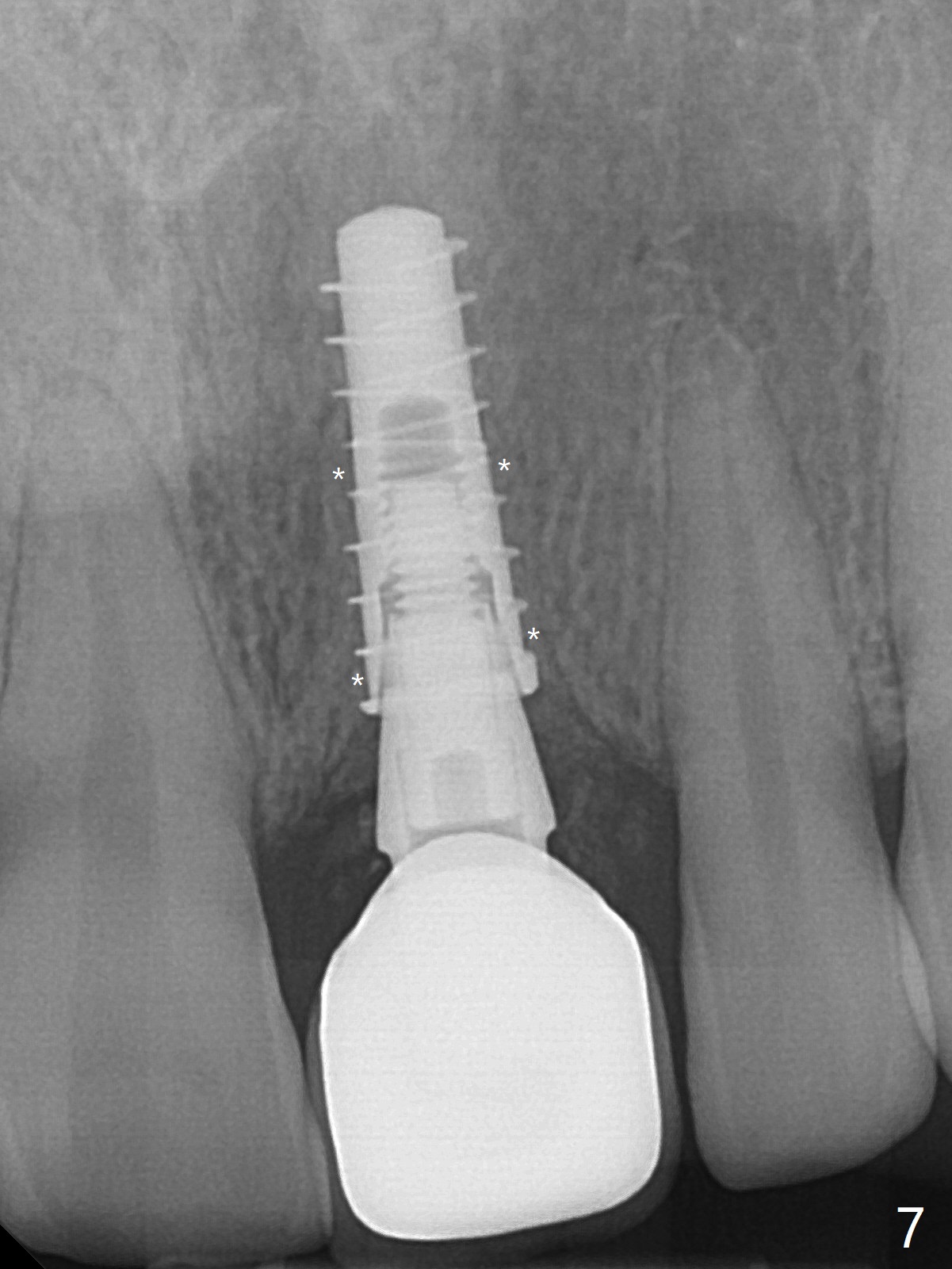
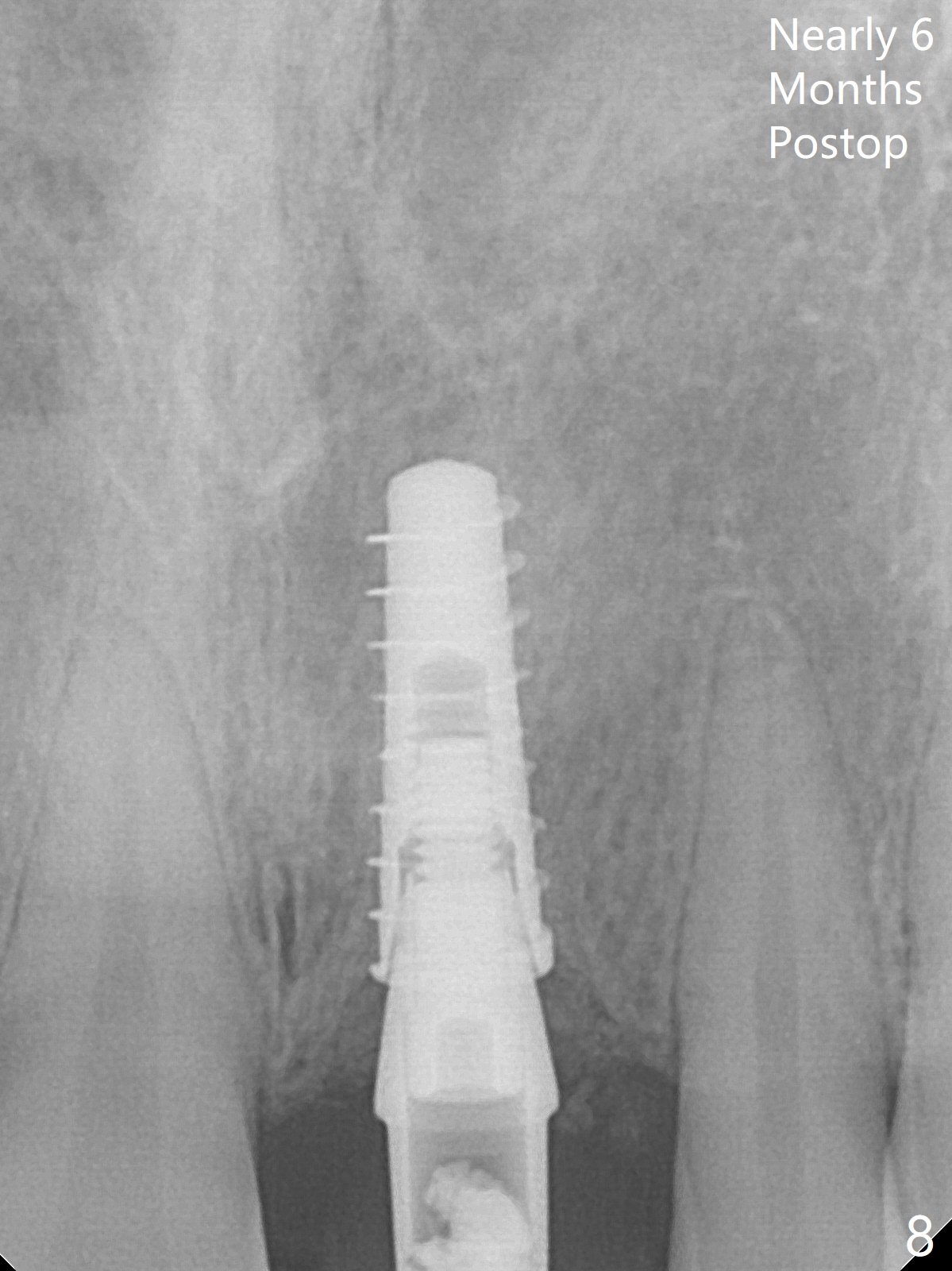
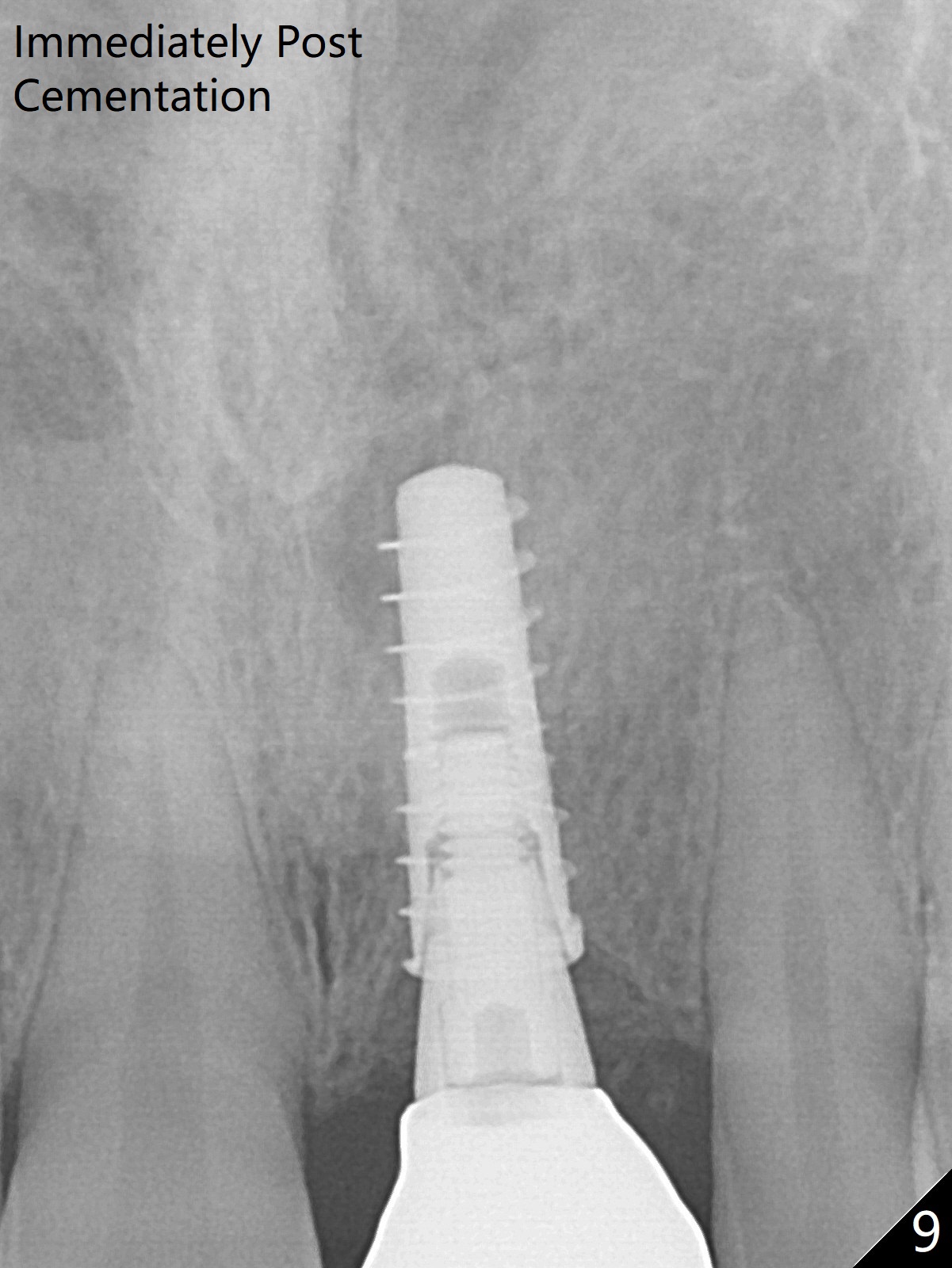
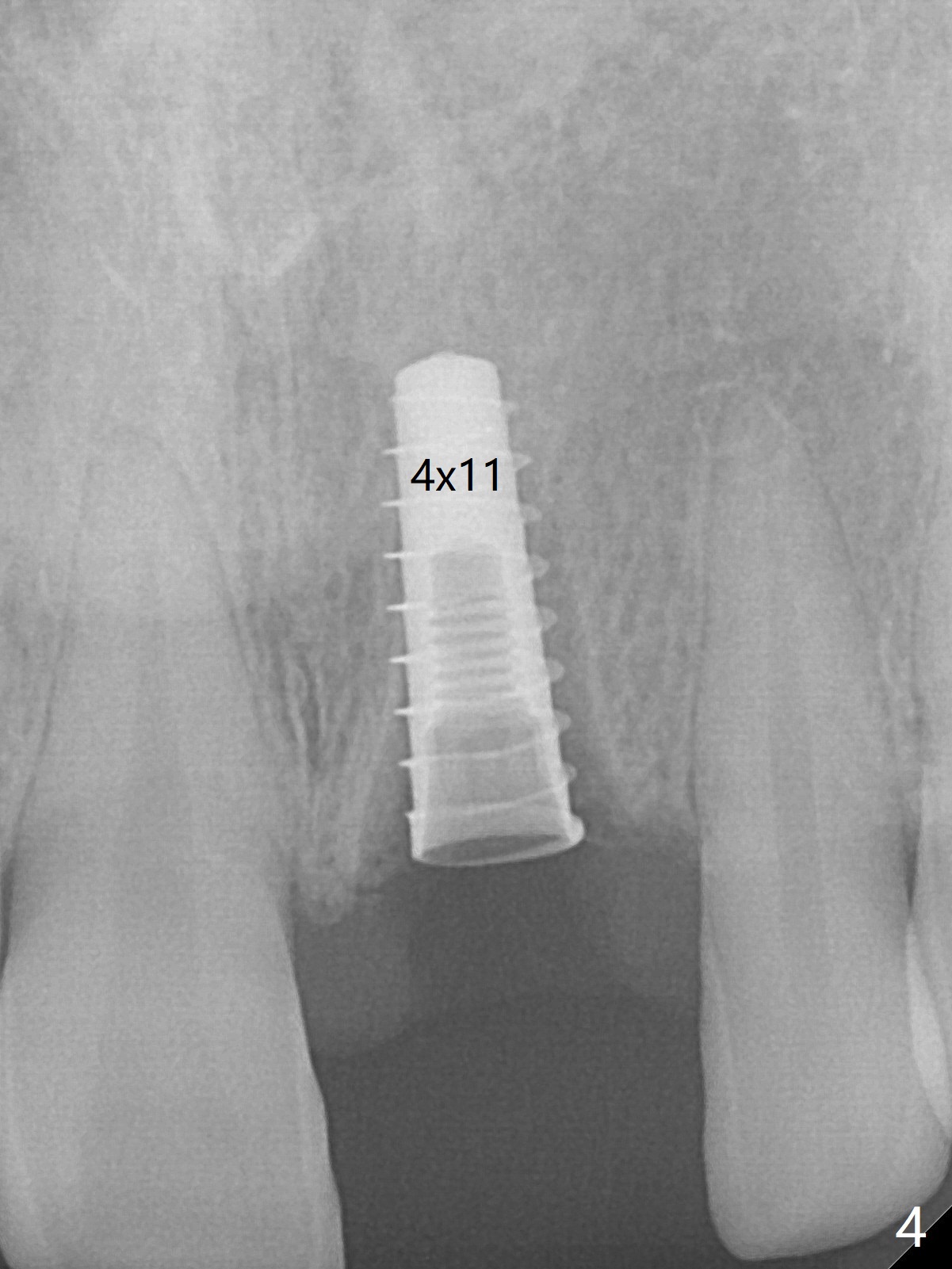
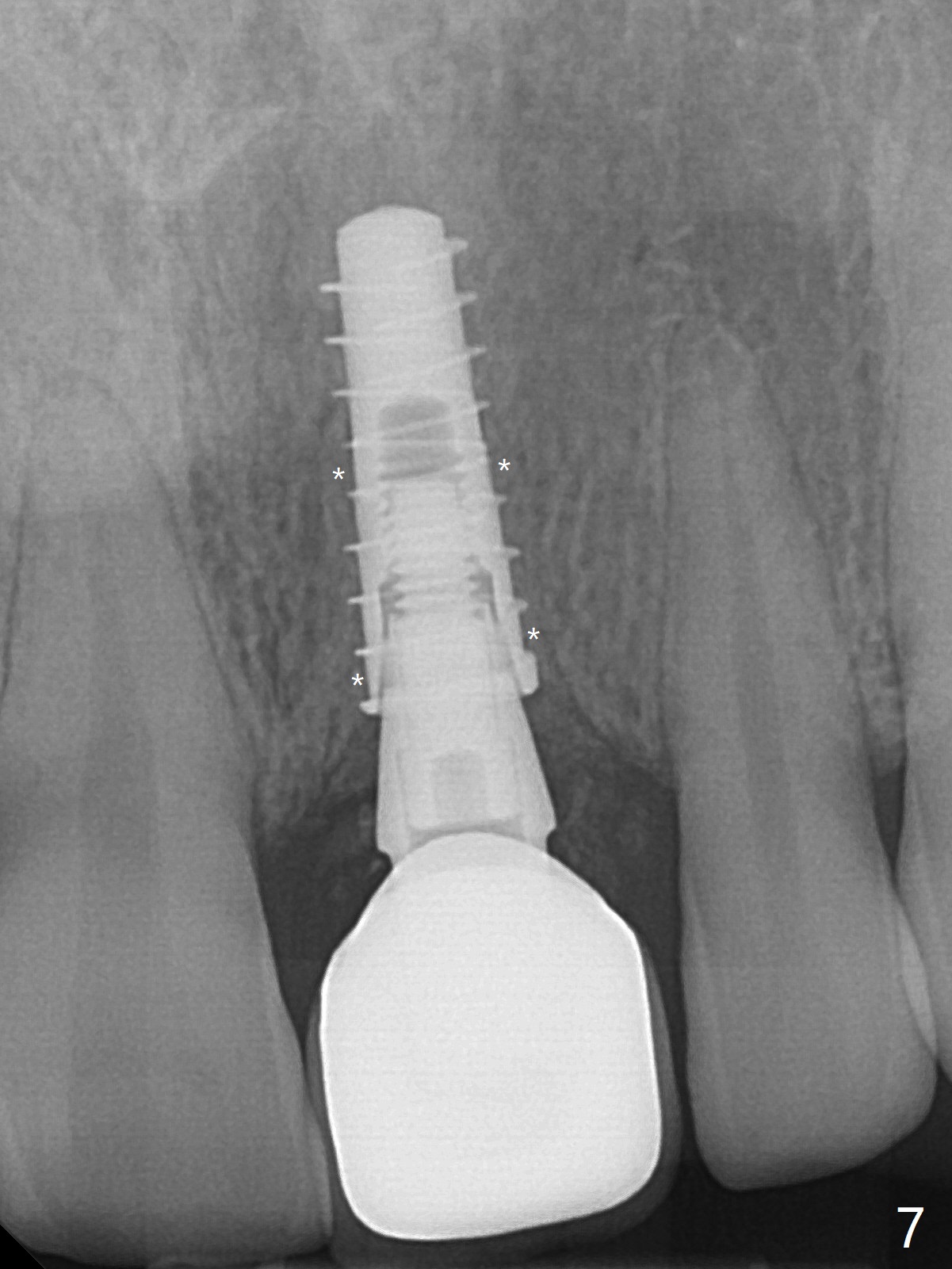
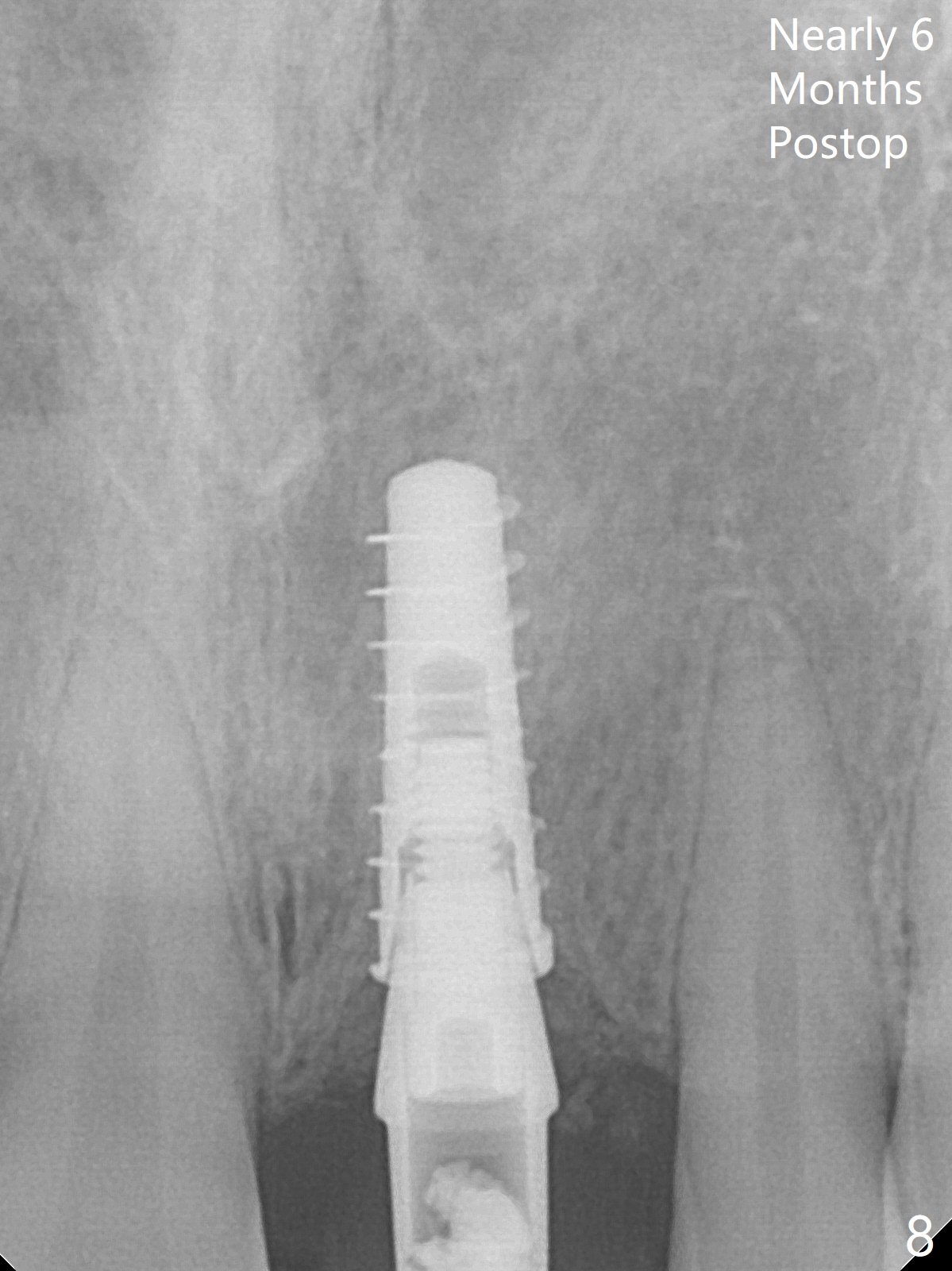
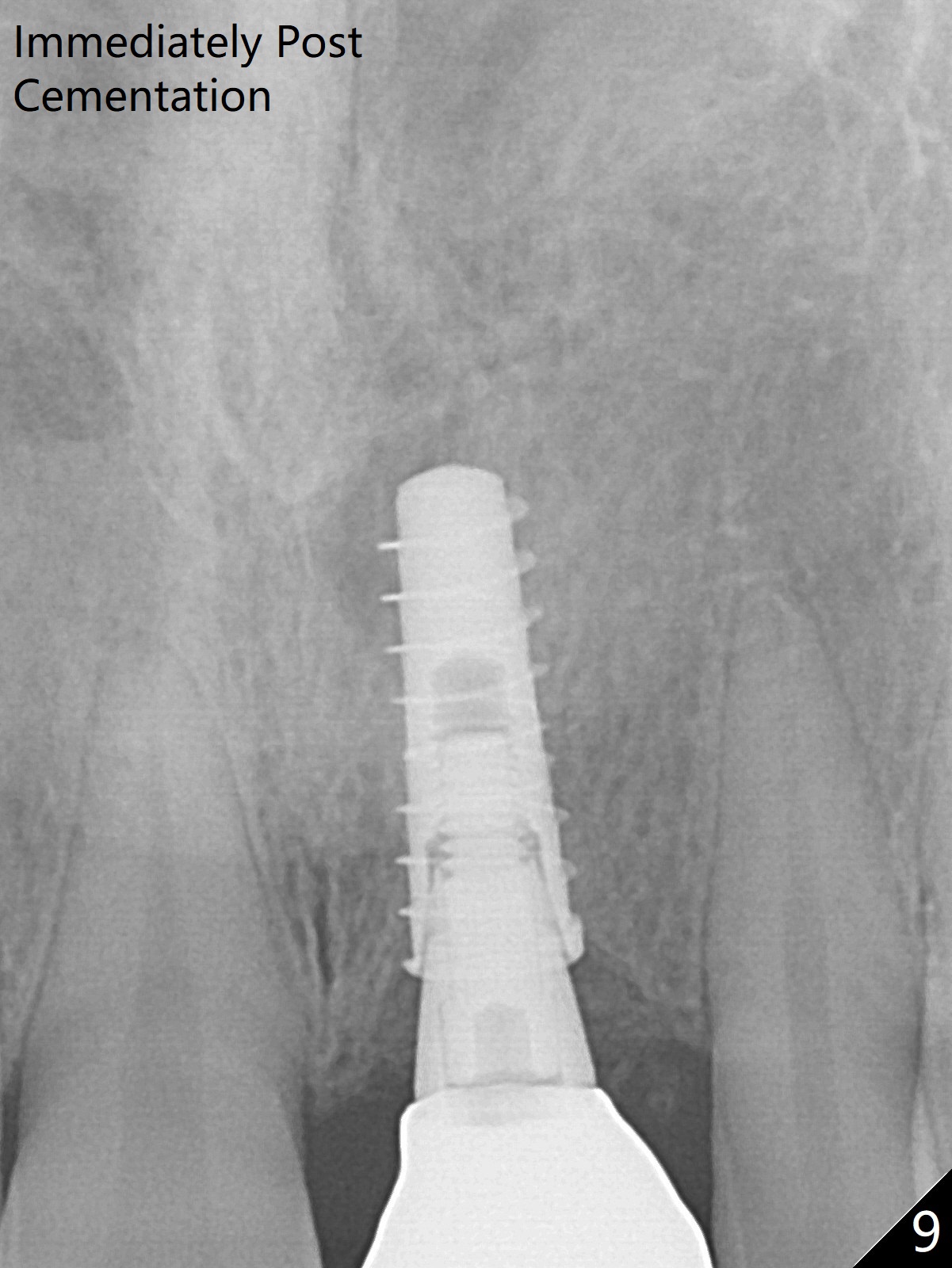
The mobile crown at #9 is buccoincisally displaced with the inflamed gingiva (Fig.1). Extraction turns out to be easy in spite of subgingival fracture (socket shield not indicated). The buccal plate is intact. Initial osteotomy is off (Fig.2). After change in trajectory (Fig.3), single drill technique is adopted (3.3 mm Magic Drill for 13 mm) and a 4x11 mm dummy implant is placed with 40 Ncm and 1 mm subgingival palatal (Fig.4). The definitive implant is placed deeper with >50 Ncm (Fig.5); with placement of a 4x5.7(2) mm abutment and mixture of autogenous bone and Vera Graft (*), the existing crown (9) is relined and inserted as an immediate provisional. The gingival margin erythema reduces at #9 eleven days postop (Fig.6). One day earlier, the patient accidentally bit on a piece of broccoli with pain for several hours. It appears that a 13 mm long implant should have been placed. The periimplant space appears to be filled with denser bone 3.5 months postop (Fig.7 *). Impression is not taken because of gingival bleeding, which is in turn probably due to the low margin. A new provisional is fabricated. The patient does not feel any discomfort when she returns for impression nearly 6 months postop (Fig.8). There is no access hole of the crown. No residual cement is noted immediate post cementation (Fig.9). With use of water pik, the gingiva is healthy around the permanent crown; the gingival embrasures should be able to close in time (Fig.10 *). The patient reports that palatal swelling 6 months post cementation reduces after use of water pik (Fig.11).
Return to Upper Incisor Immediate Implant Xin Wei, DDS, PhD, MS 1st edition 10/10/2017, last revision 10/06/2018