



 |
 |
 |
 |
||
 |
 |
 |
 |
 |
|
 |
|||||
Emergency Immediate Implant
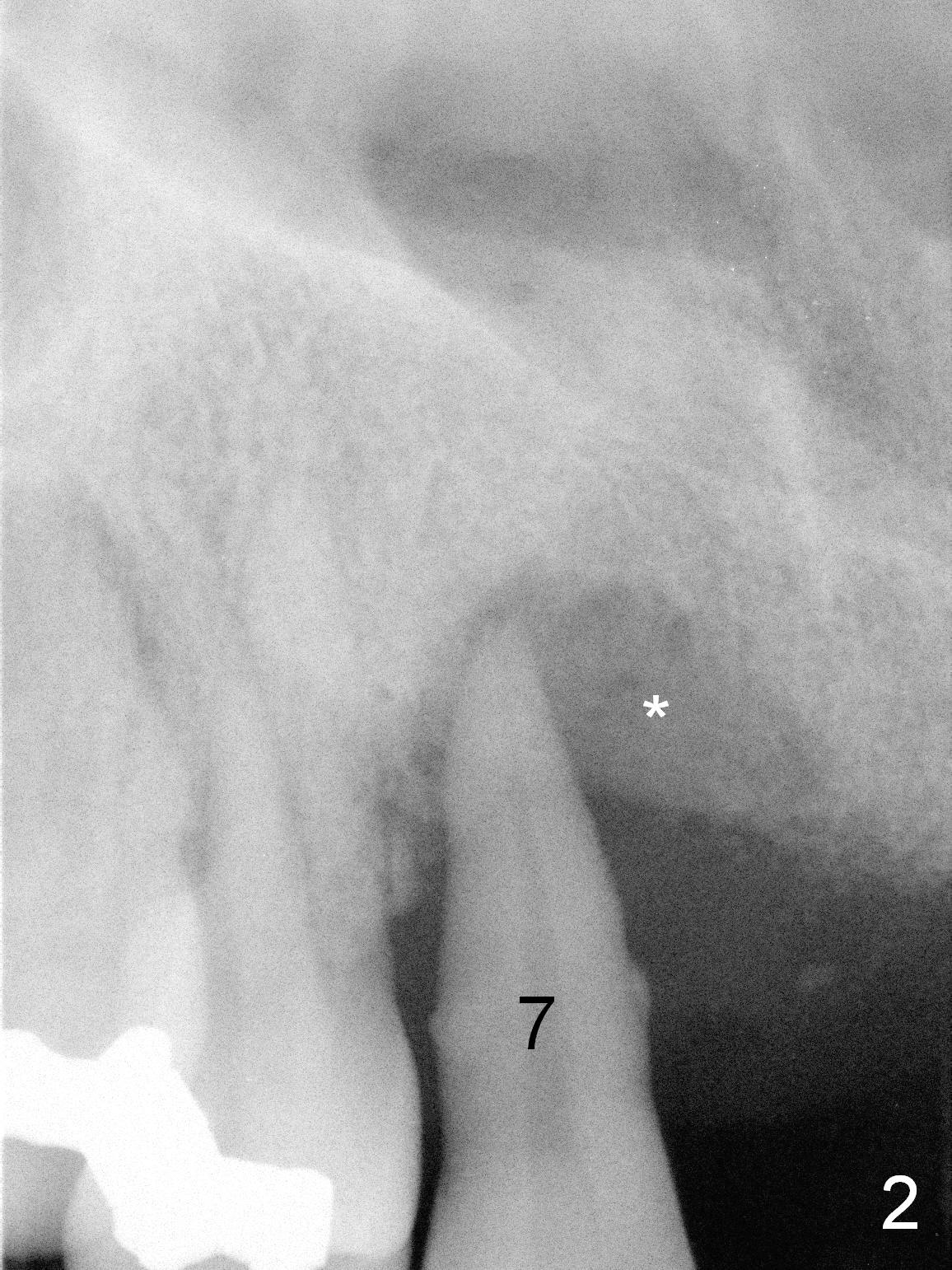
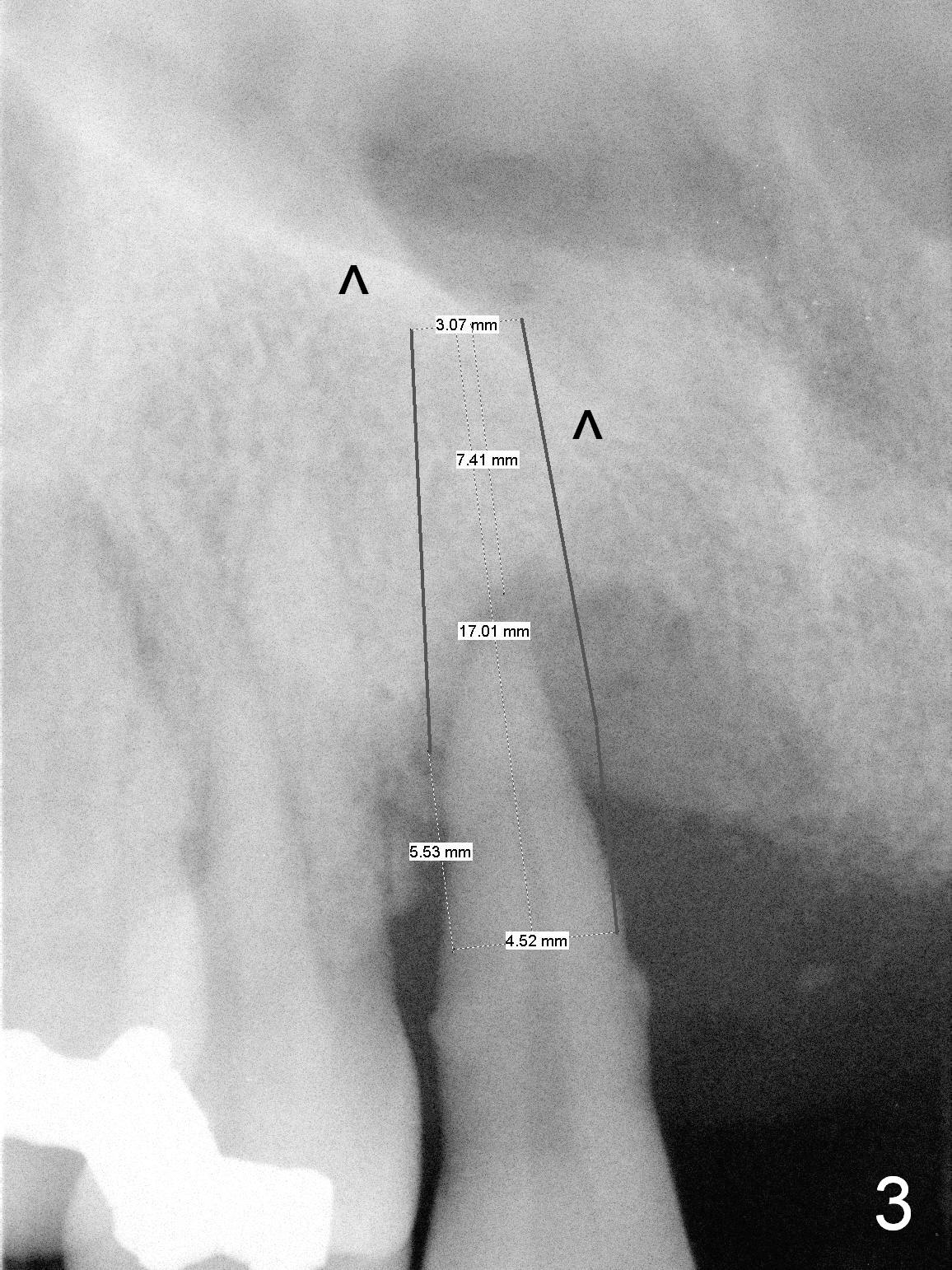
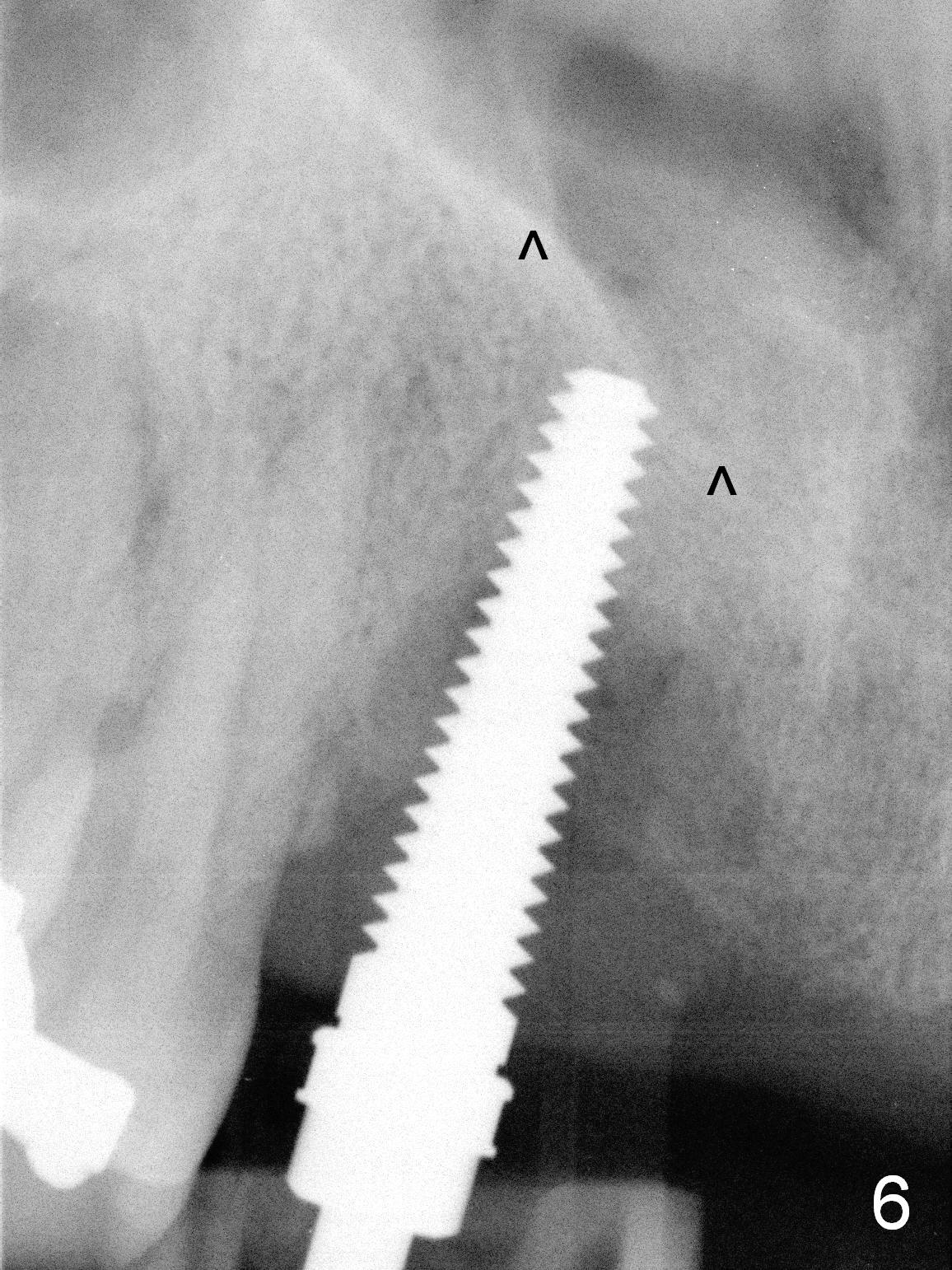
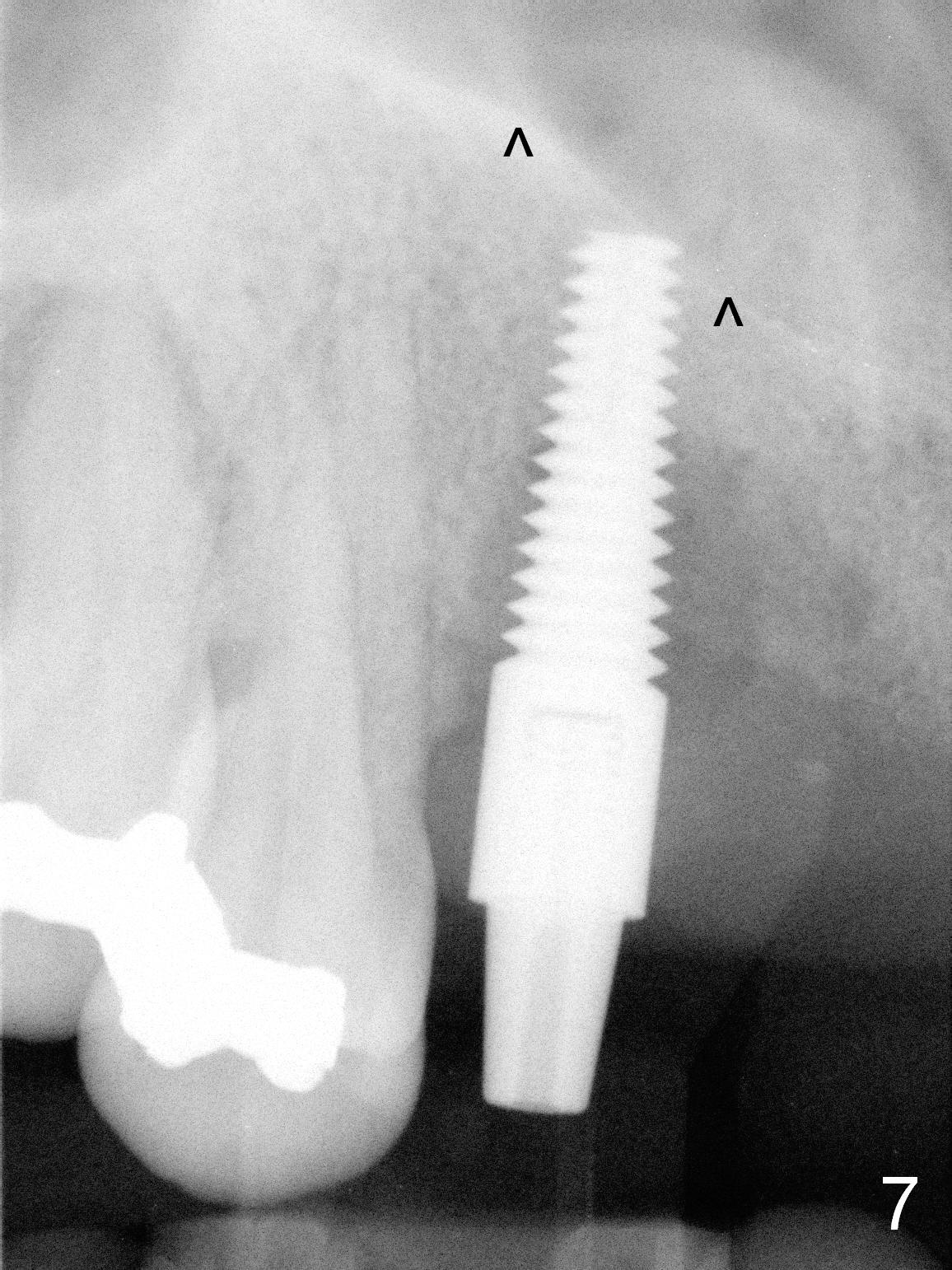
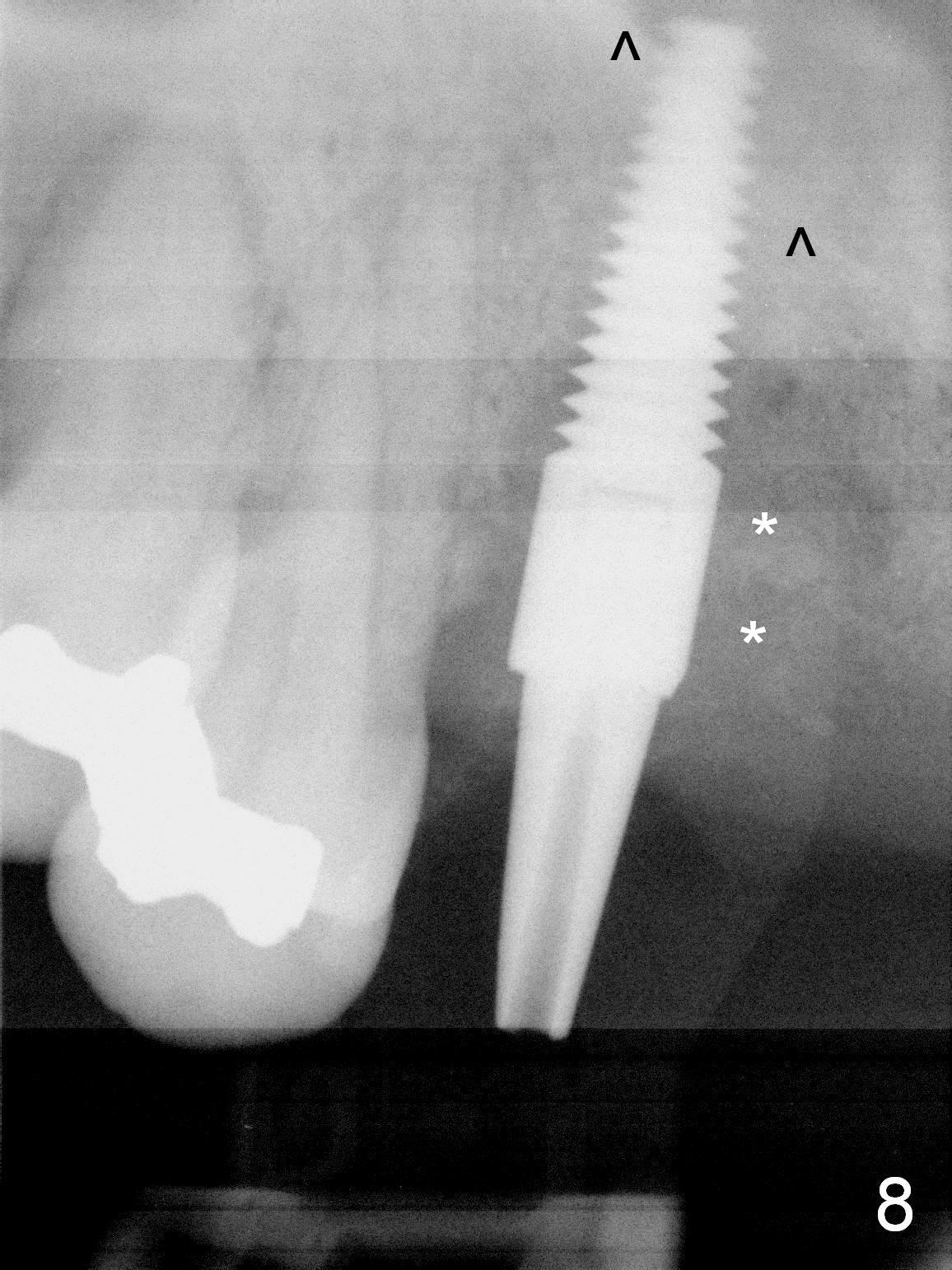
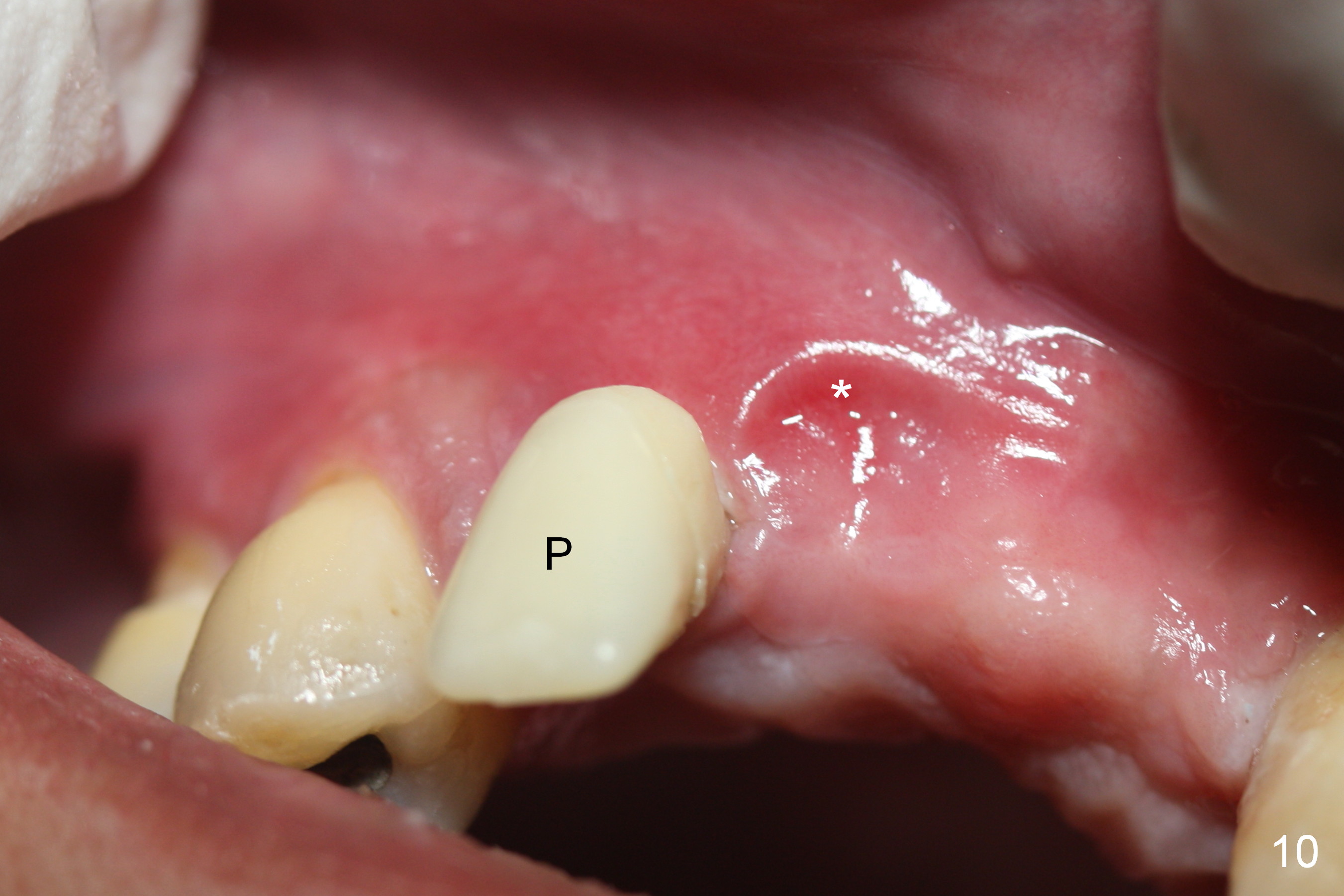
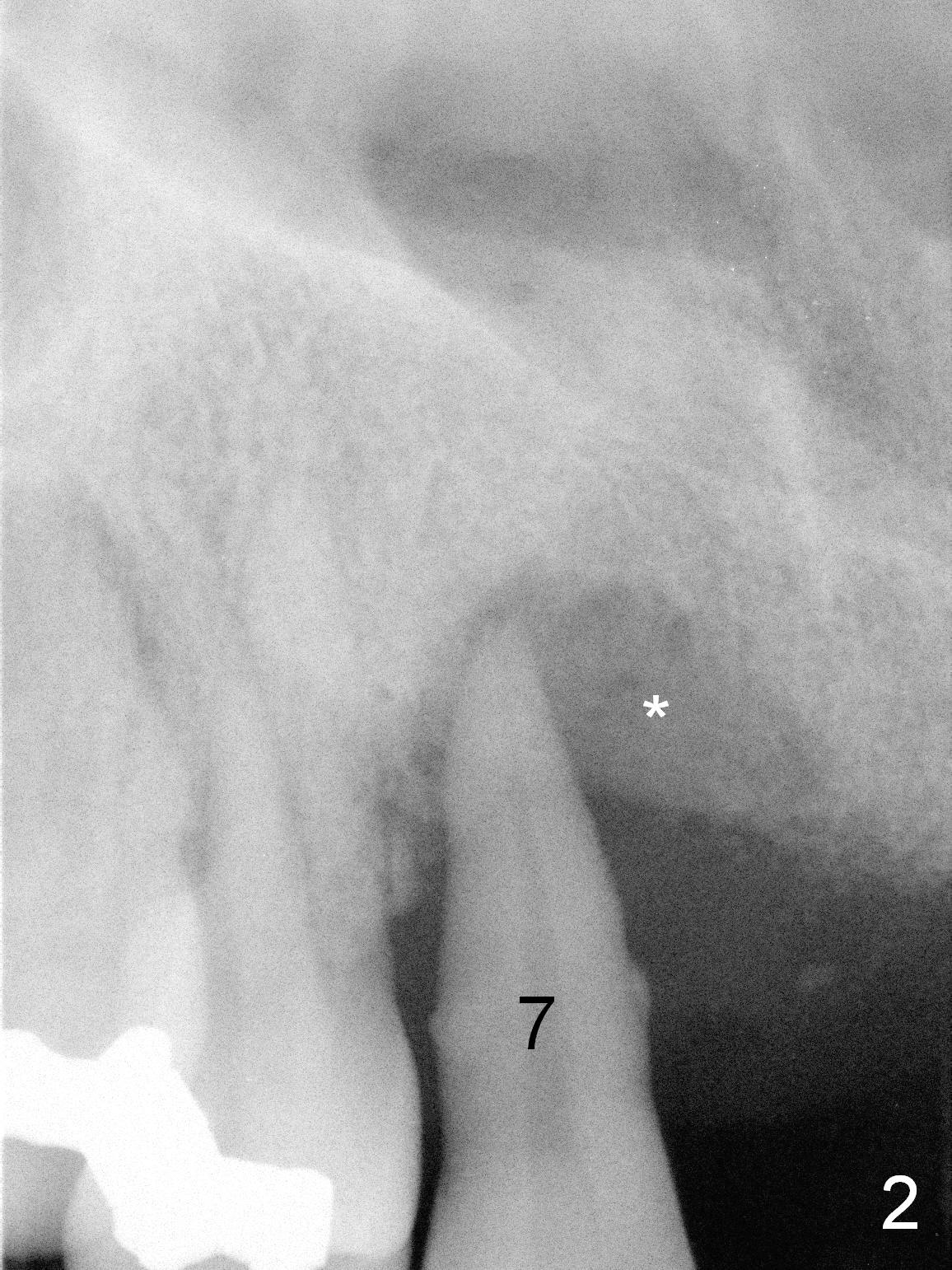
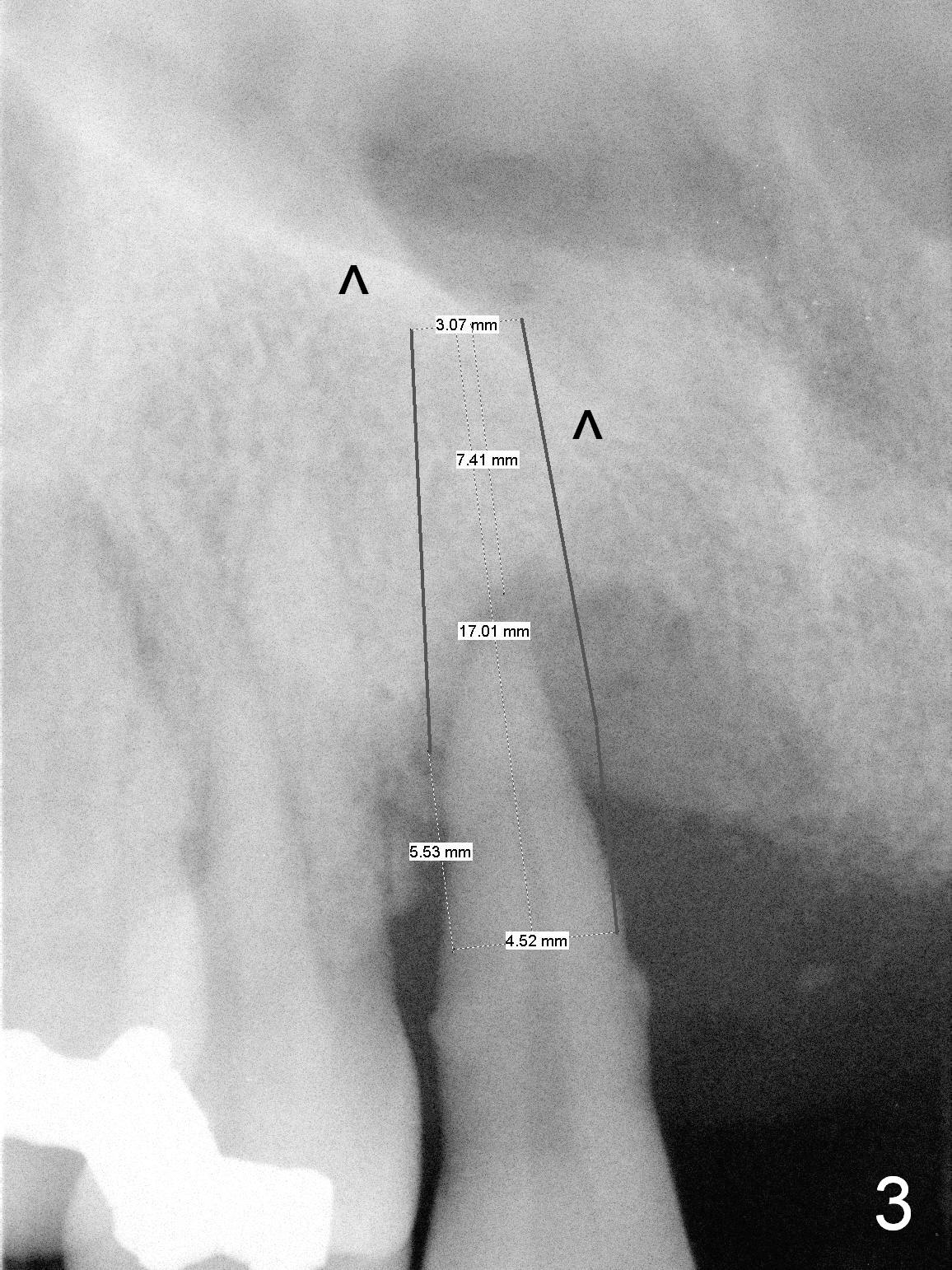
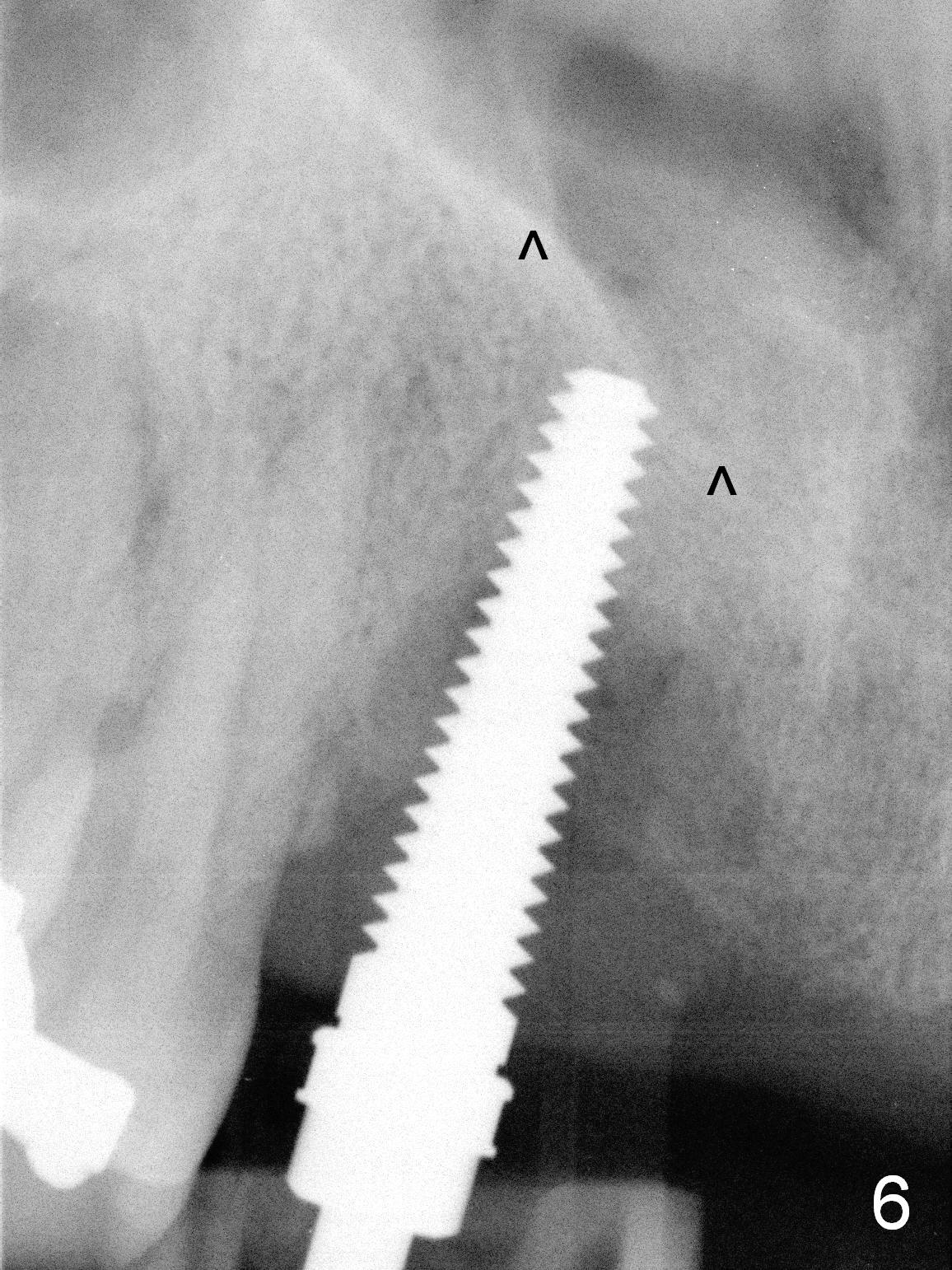
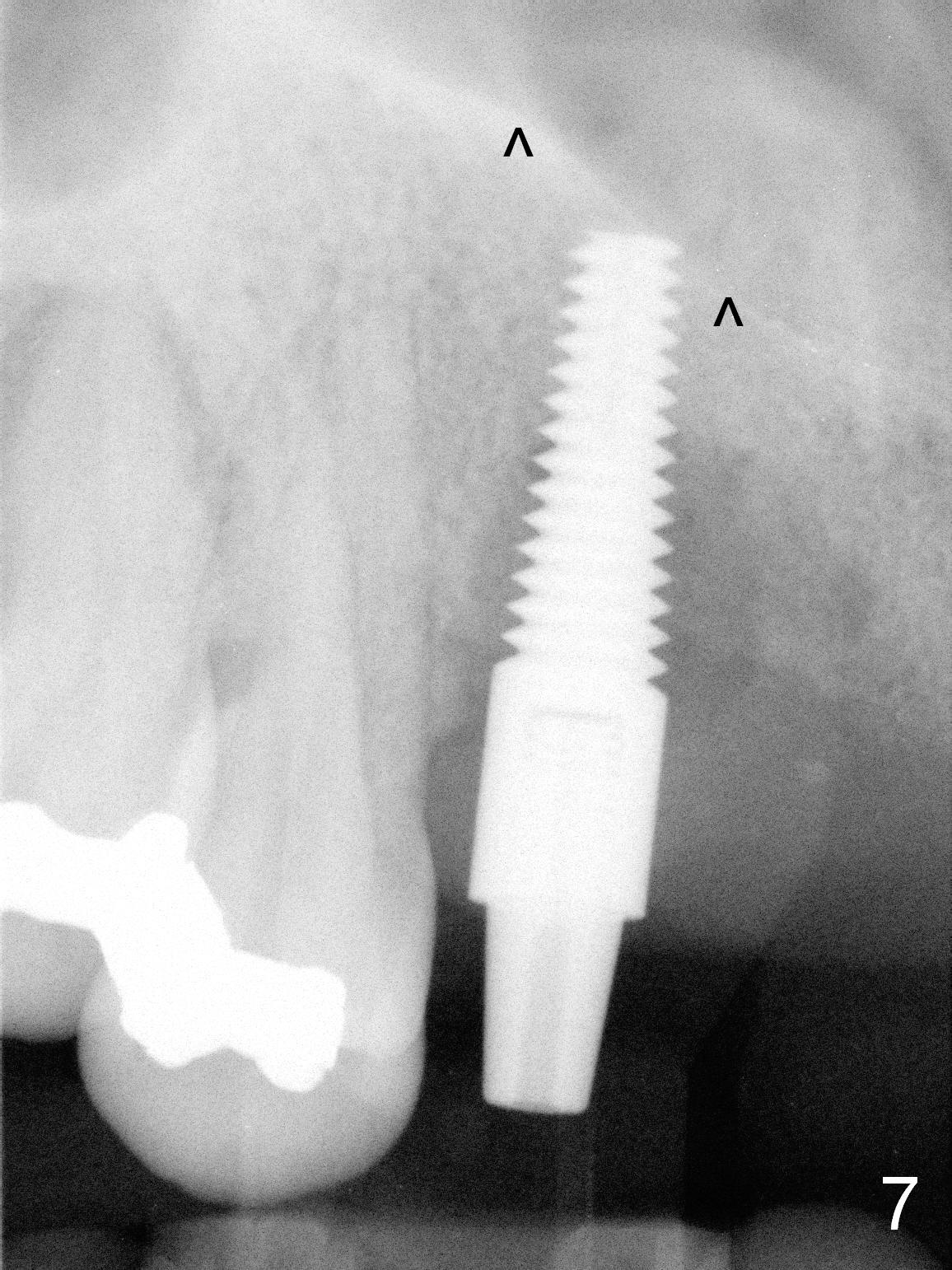
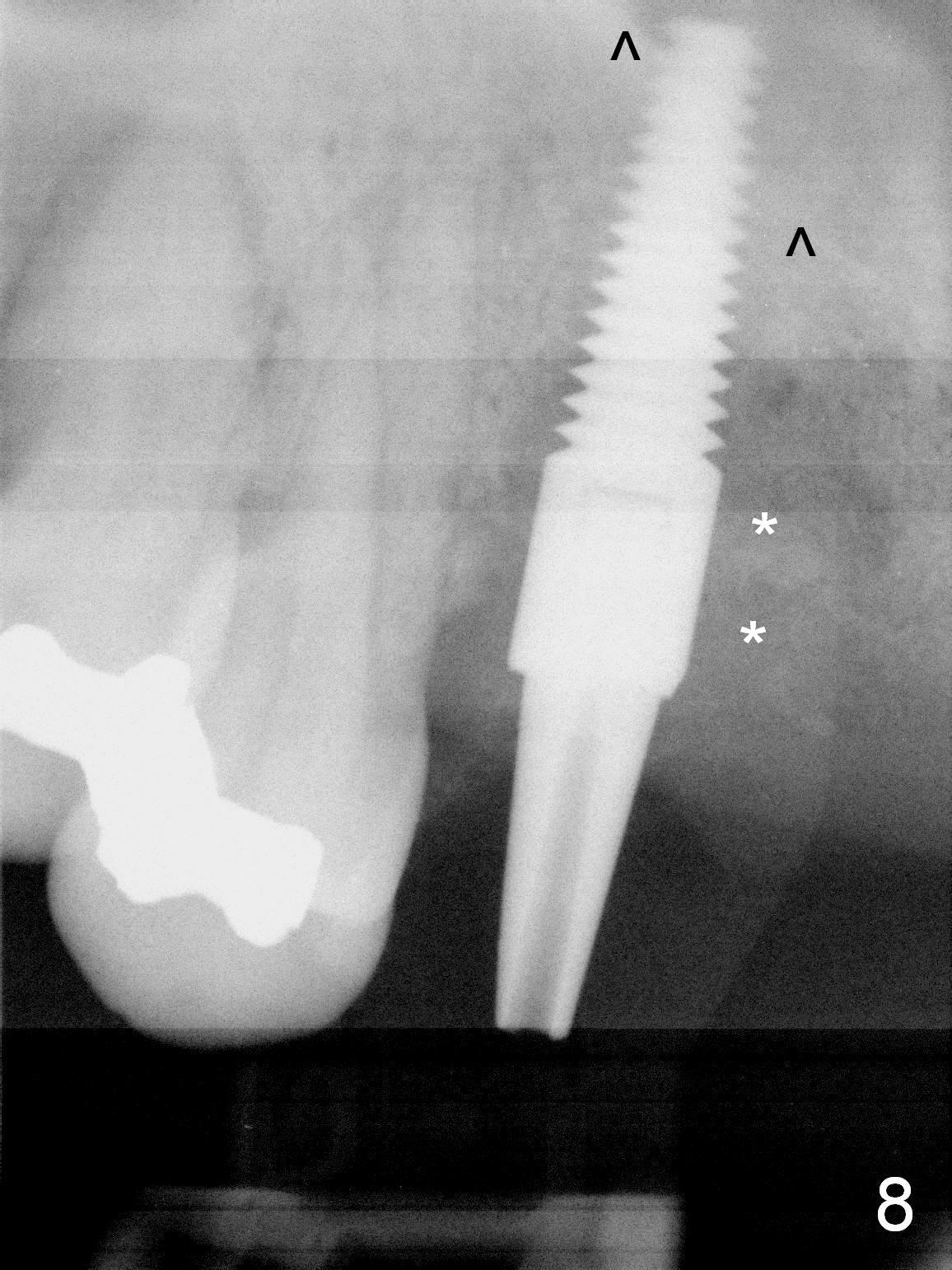
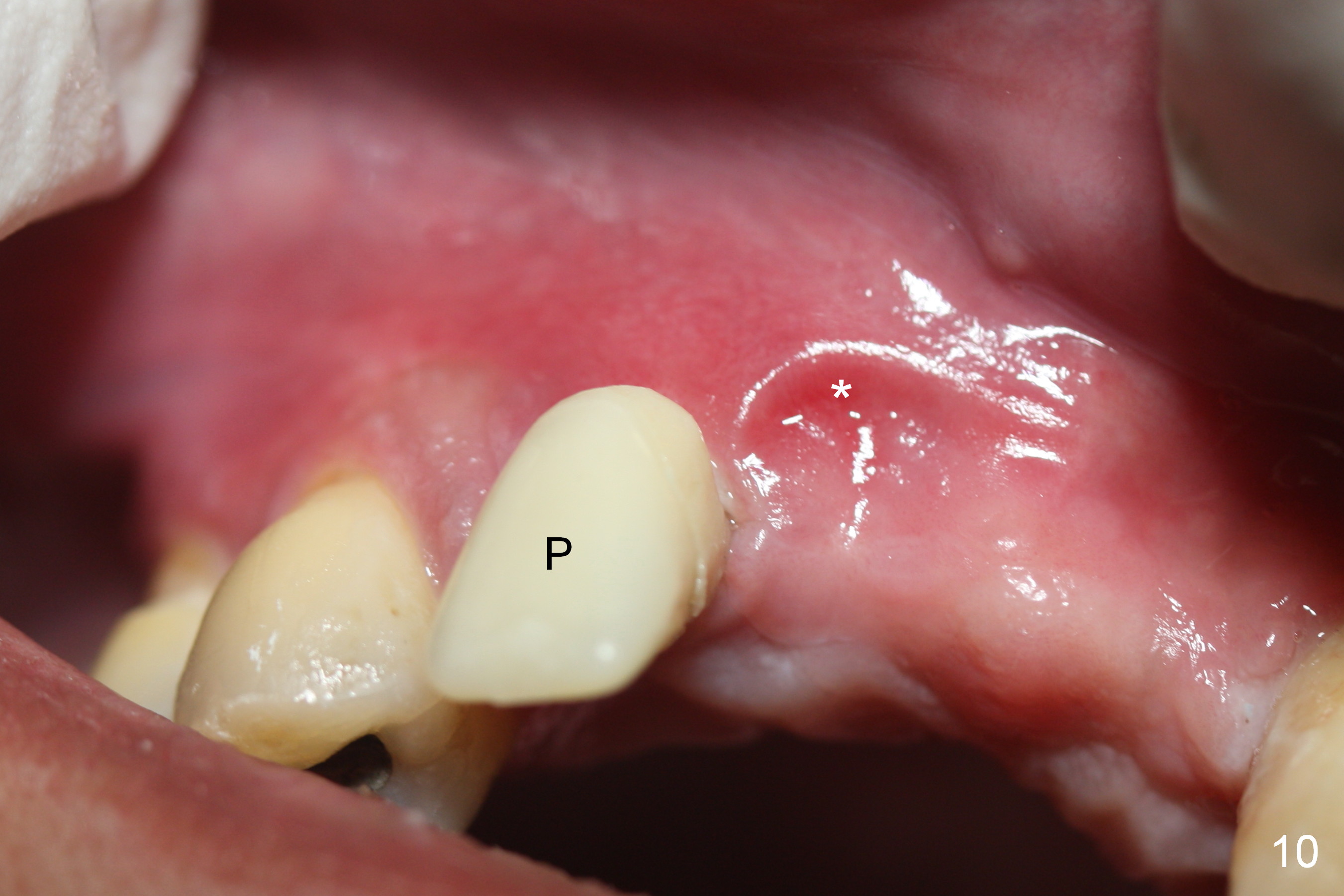
A 49-year-old man has chronic periodontitis with partial edentulism. The tooth #7 has an acute episode: pain, swelling and mobility (Fig.1,2 *). After taking 2 g of Oral Amoxicillin, the affected tooth is to be extracted and an immediate implant is placed close to the nasal floor (Fig.3 ^). As expected, the buccal plate is found to be absent after extraction (Fig.4 *: Metronidazole gauze). An osteotomy is initiated as palatal as possible and as close to the nasal floor as possible (Fig.5 ^). In spite of the fact that osteotomy site is underprep (in diameter), a 4.5x17 mm tap (Fig.6) and implant (Fig.7) are not stable. With an increase in depth of osteotomy and penetration of the nasal floor, the implant achieves satisfactory primary stability (insertion torque of 50 Ncm, Fig.8). The drawback is that the margin of the soft tissue level implant (Fig.9 black *) is subgingival (white *: bone graft). An immediate provisional has to be provided to keep the gingiva from growing over the restorative margin. One week postop, the inflammatory edema is subsiding around the provisional (Fig.10 P), while the partial denture presses the subsiding edematous tissue (*). At this time the provisional contacts the neighboring natural tooth; 4 months postop, the provisional appears to shift mesially.
Return to Upper Incisor Immediate Implant
Xin Wei, DDS, PhD, MS 1st edition 11/17/2015, last revision 01/19/2018