












 |
 |
 |
 |
||
 |
 |
 |
 |
||
 |
 |
 |
 |
||
 |
 |
 |
|||
Depth of Bone Graft
A 57-year-old man refuses treatment for the tooth #5 for 22 months (Fig.1). He suddenly shows up because of severe bleeding from the fistula of the tooth (Fig.2 <). After lengthened discussion, he agrees extraction (Fig.4) and immediate implant (Fig.5-8).
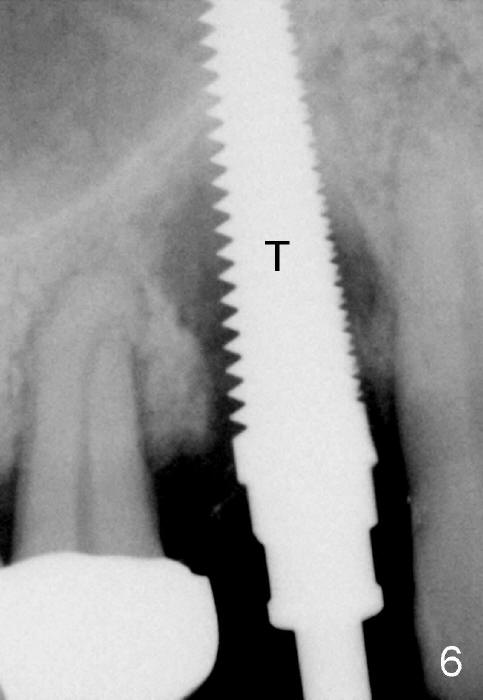
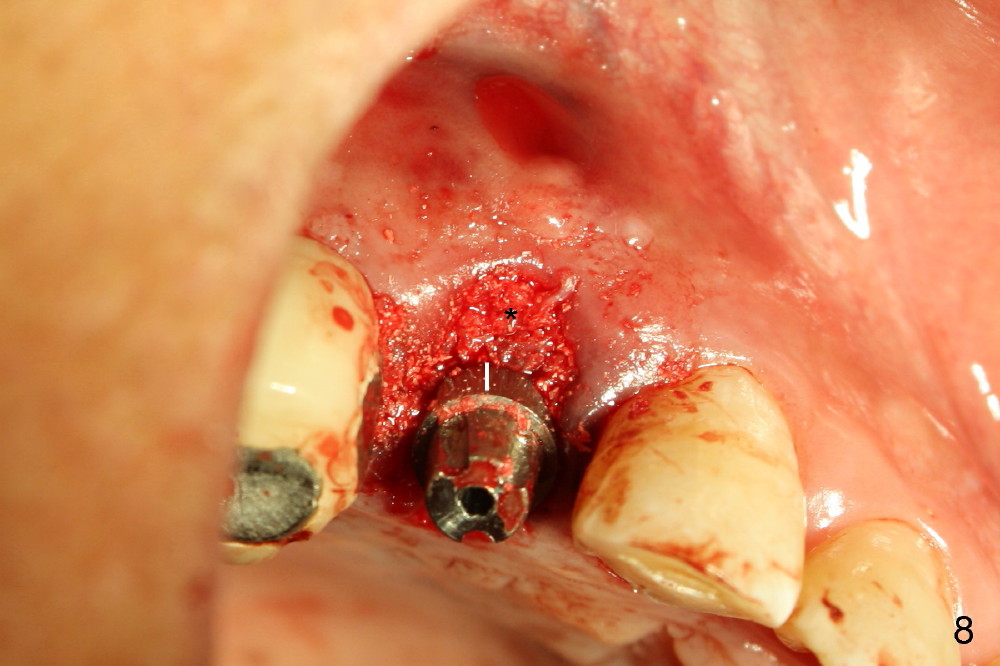
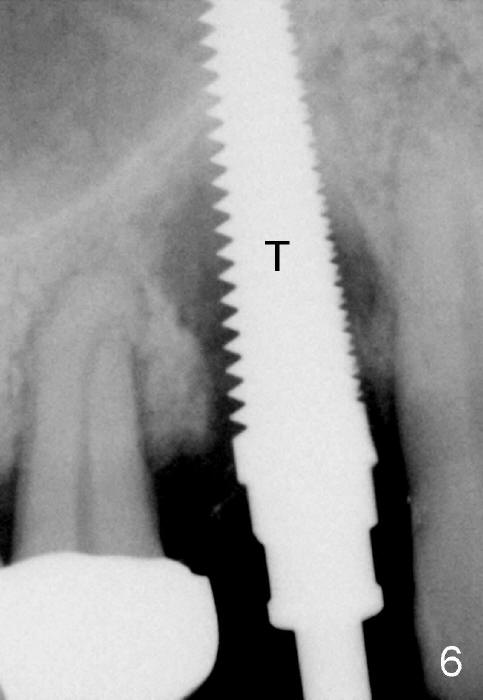
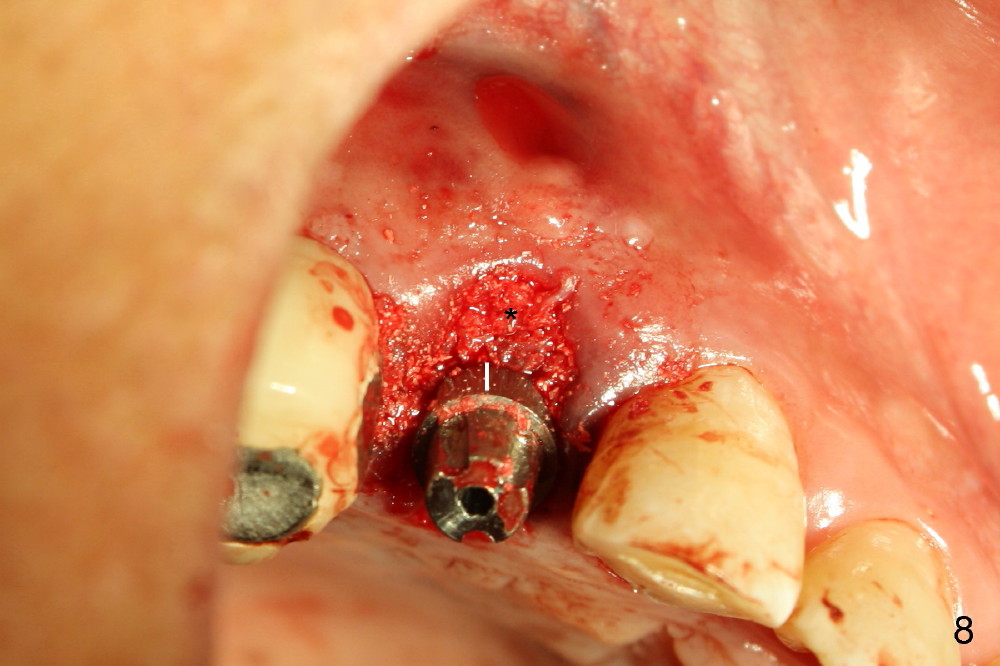
In spite of large periapical radiolucency (Fig.1 *), osteotomy is easier than expected. Use 2 mm pilot drill, 2.5-3.5 mm reamers from 14 mm (bottom of the socket) to 17 mm (sinus floor). The initial point for osteotomy at the bottom of the socket is easy to establish, because it is flat. By the time 5x20 mm tap is inserted, it is palatal (Fig.5). It is mandatory because the buccal plate has been perforated. The tap has to be inserted deeper (from 17 mm to 20 mm, Fig.6) to achieve stability. Insertion torque of 5x20 mm implant (Fig.7 I) is > 60 Ncm. The implant remains palatal so that there is space for bone graft (Fig.8 *). But the bone graft is a little over packed; there is no room to place collagen dressing. The latter will be dislodged and bone graft will be lost if perio dressing is loose prematurely. The perio dressing may have to be re-applied. Depth of bone graft is deemed sufficient if the implant threads are covered. Maximum will be on the rough surface. Physiologically, bone does not extend to the gingival margin.
As expected, the collagen dressing is dislodged when the perio dressing is off; fortunately the bone graft remains in place 7 days postop (Fig.9 *). To keep the bone graft in place, an immediate provisional (Fig.10 P) is fabricated and cemented; its margin (*) covers the graft. There is no occlusal contact in centric and lateral excursion. The patient is asked not to use this crown for 3 months.
Eighteen days postop, the patient returns for #4 root canal therapy; PA shows bone graft next to the implant (Fig.11 *). Twenty-two days postop, the immediate provisional is dislodged with loss of bone graft over the middle of the buccal surface of the implant (Fig.12 *). The implant and abutment are prepared so that the margin is advanced apically (Fig.13 ^) with accentuation of the retention grooves (*). The provisional is relined and recemented.
Exam of the extracted tooth shows that loss of the tooth is more likely due to periodontitis (Fig.14) than endodontic lesion (Fig.15).
Return to Upper Bicuspid Immediate Implant
Xin Wei, DDS, PhD, MS 1st edition 11/03/2014, last revision 01/19/2018