


 |
 |
 |
 |
 |
 |
 |
 |
 |
Implant for Bruxism
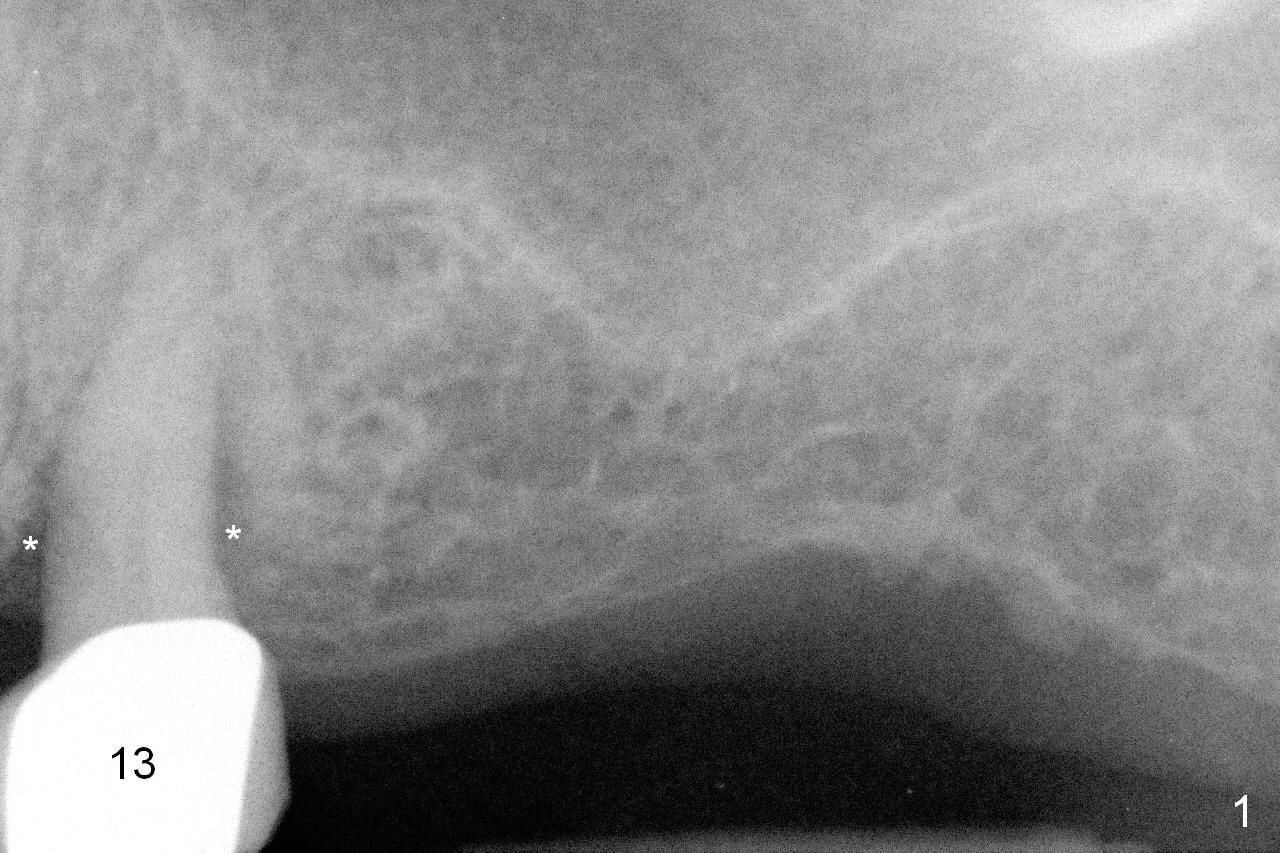
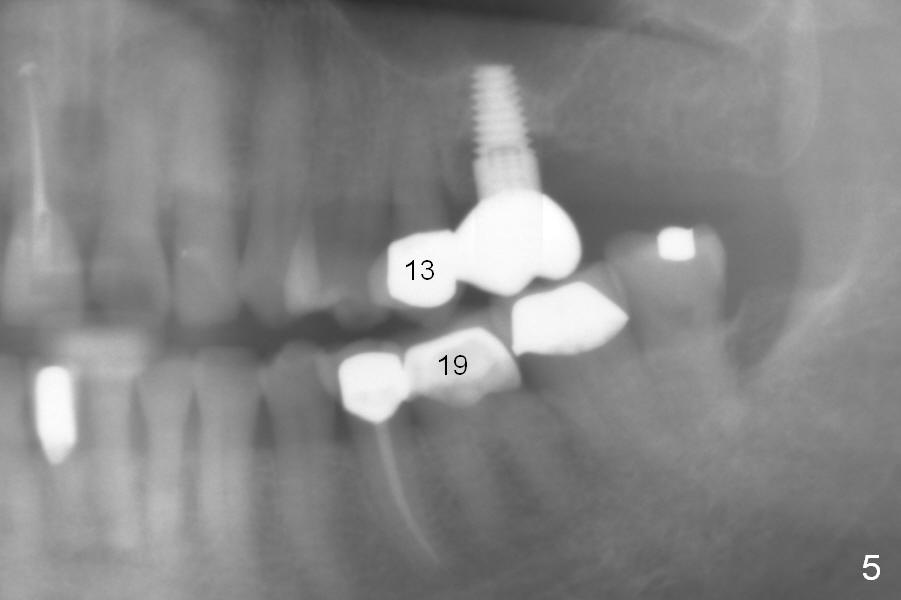
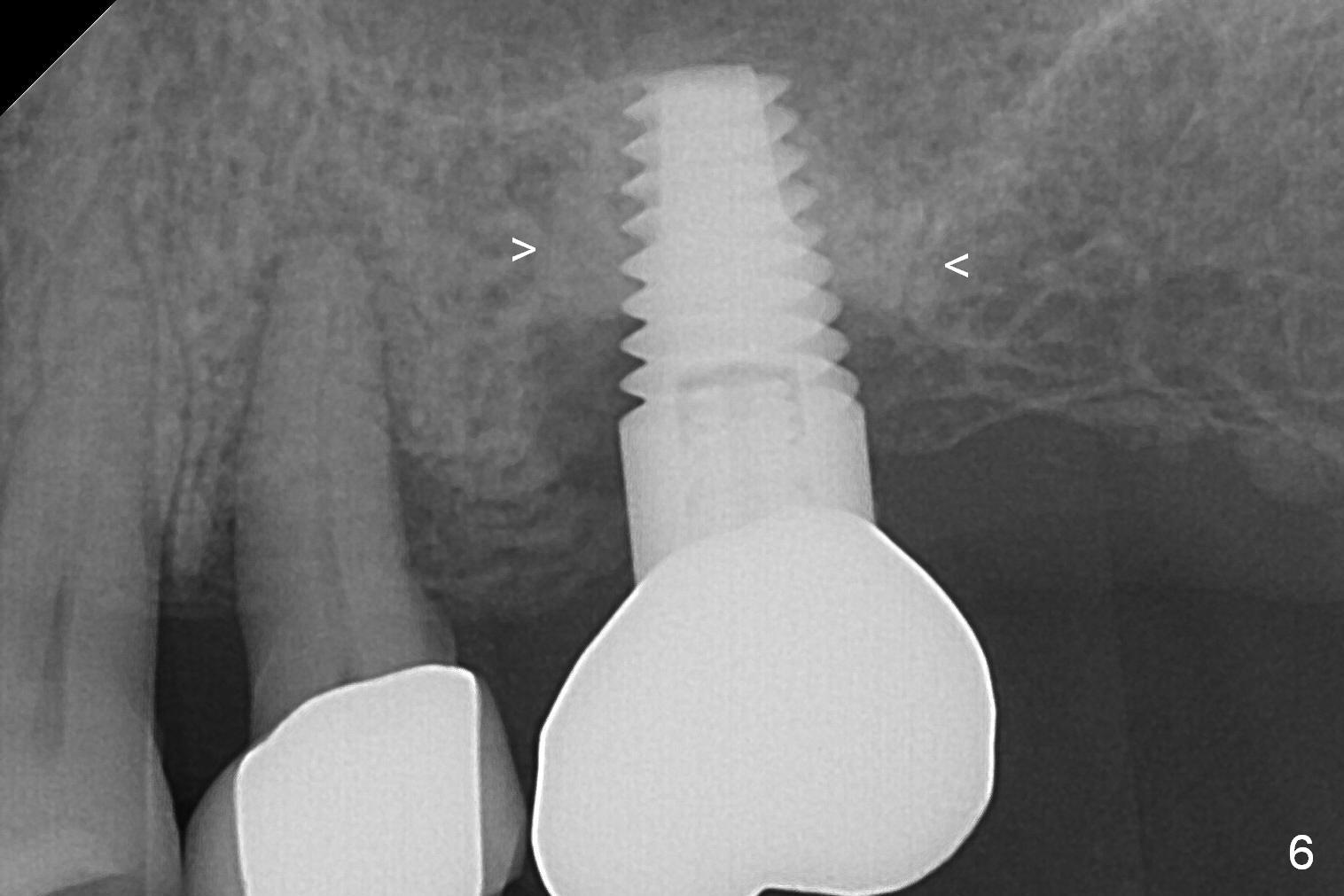
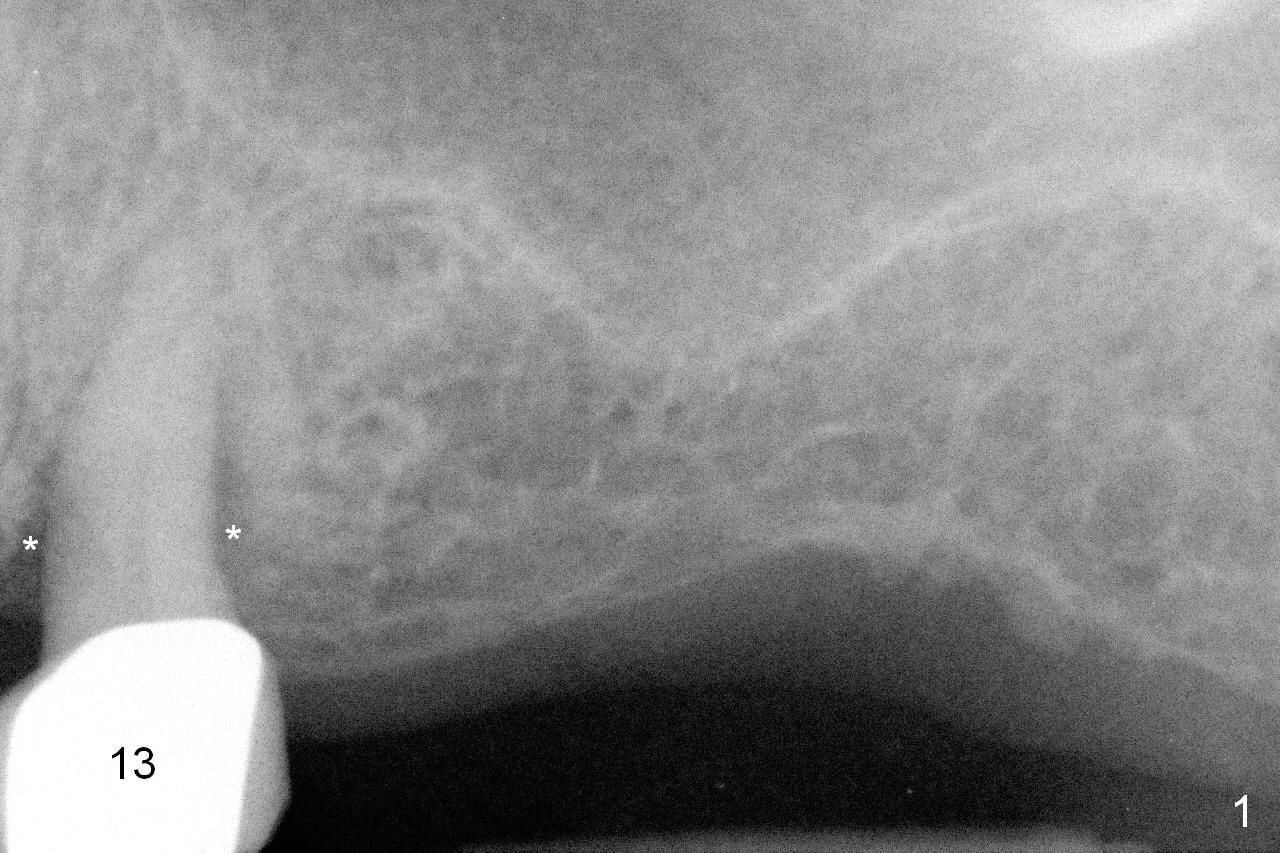
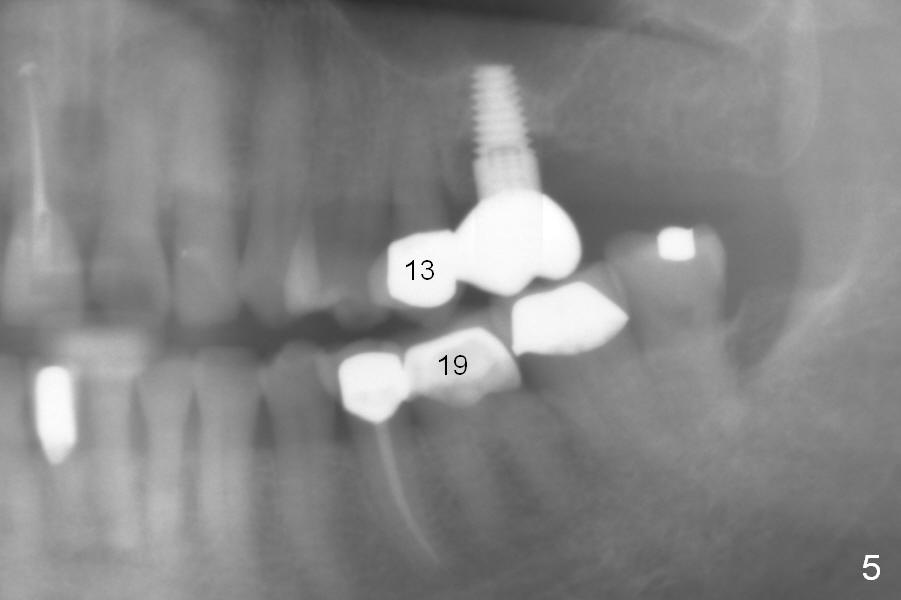
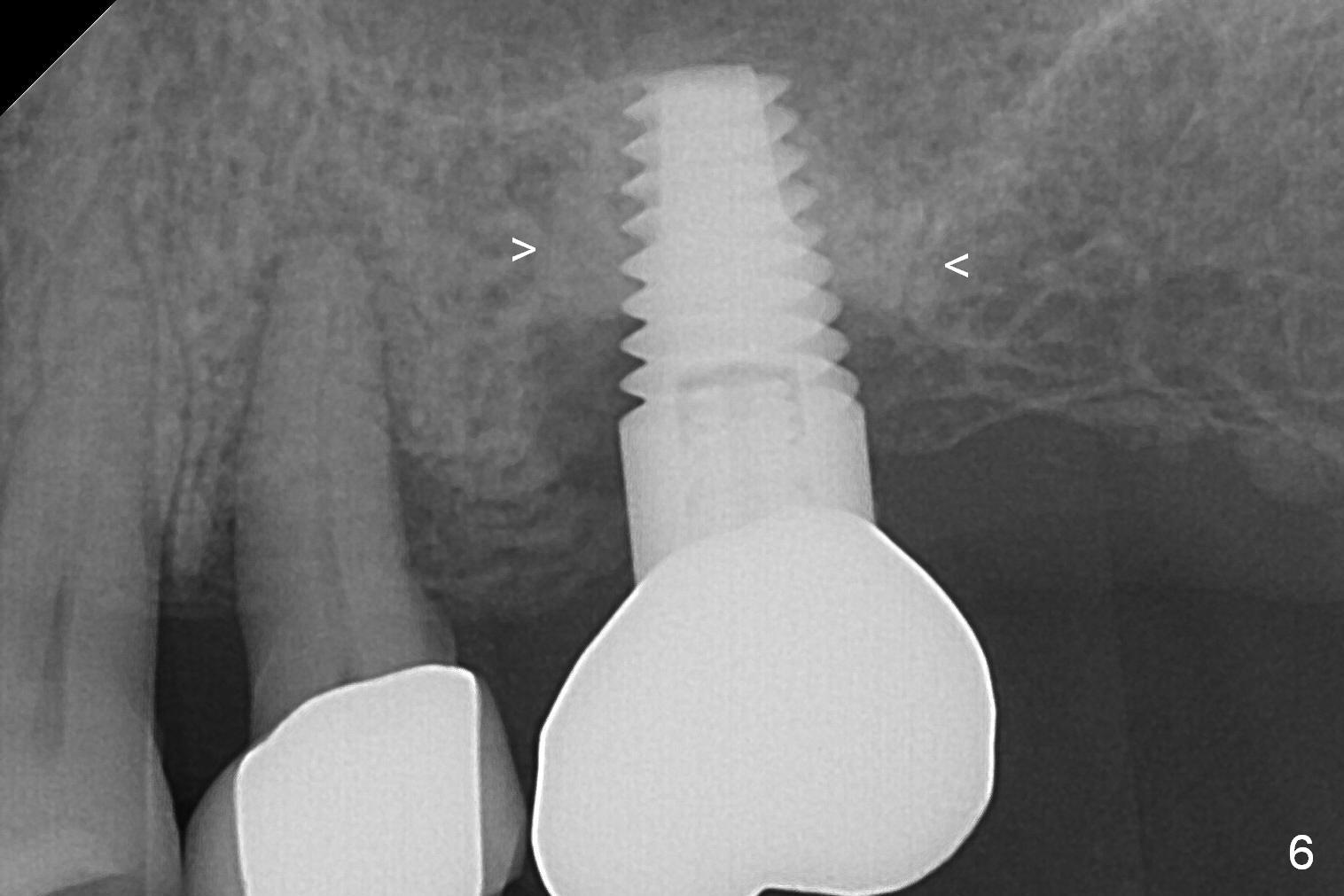
A 73-year-old woman is a possible bruxer with partial edentulism; the tooth #13 had increased periodontal ligament (pdl) space 4 years ago (Fig.1 *). A 5x14 mm tissue-level implant is placed at the site of #14 (Fig.2). The implant appears to be osteointegrated in 6 months (Fig.3). There is crestal bone loss 8 months post cementation (Fig.4 *). The persistent increased pdl at #13 is most likely associated with occlusal tramua from the tooth #19 (Fig.5 (13 months post cementation of #14)). Three years post #14 cementation, the tooth #13 has mobililty II (Fig.6); bone density increases around the apical half of the implant (arrowheads). Normally bone density is the highest coronally where functionality dictates. This indicates the bone loss is getting worse at #14 as well.
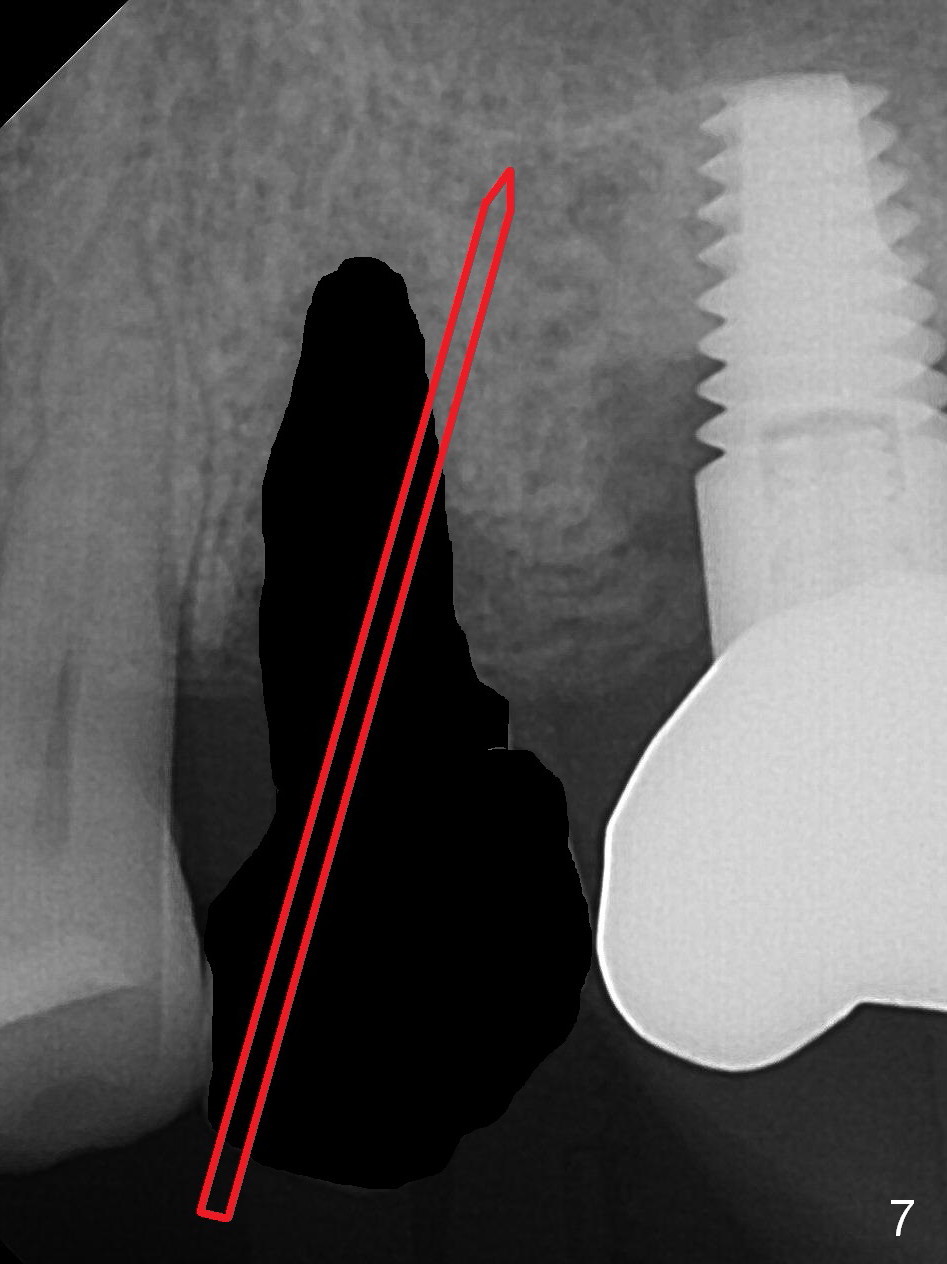
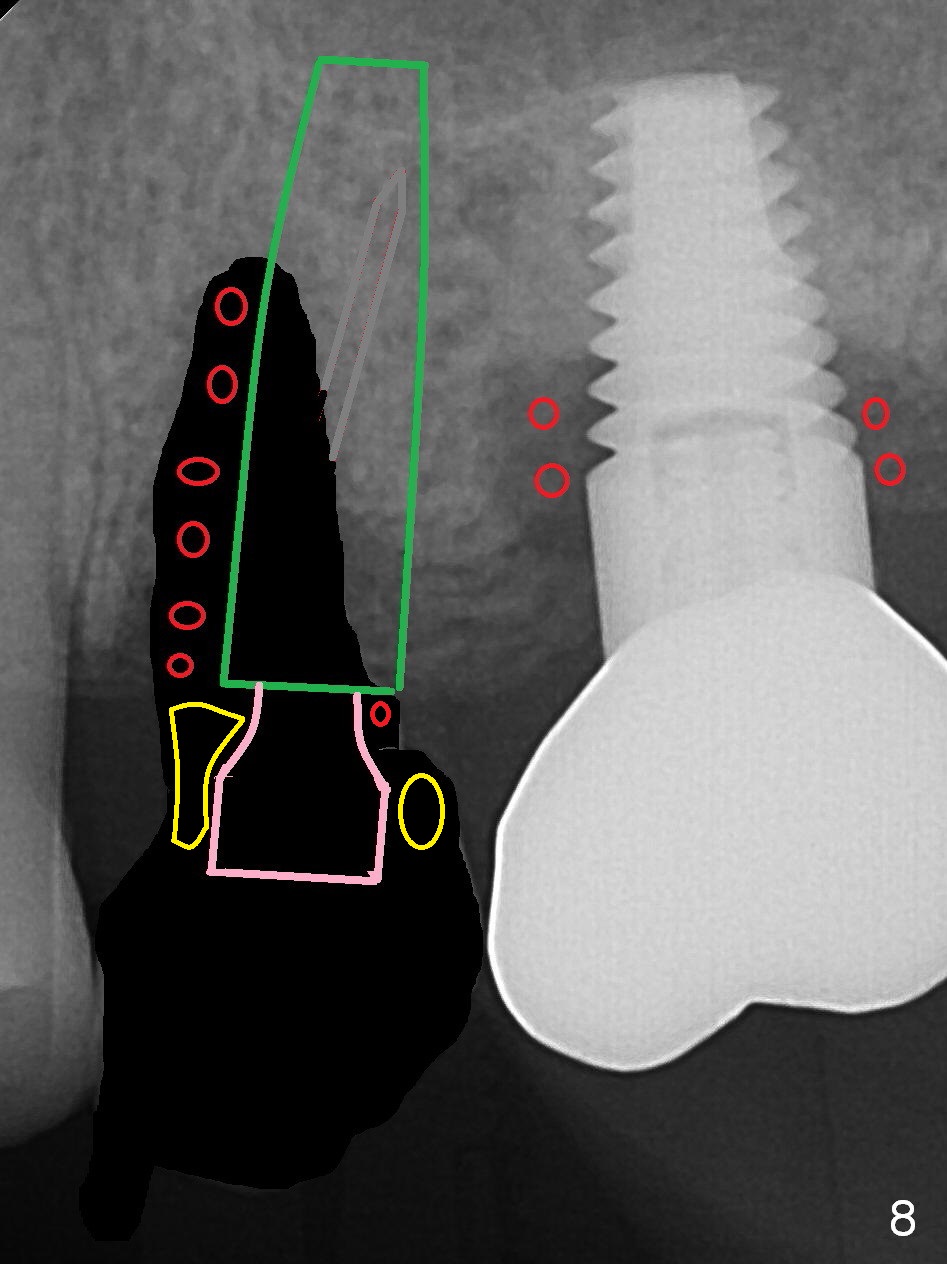
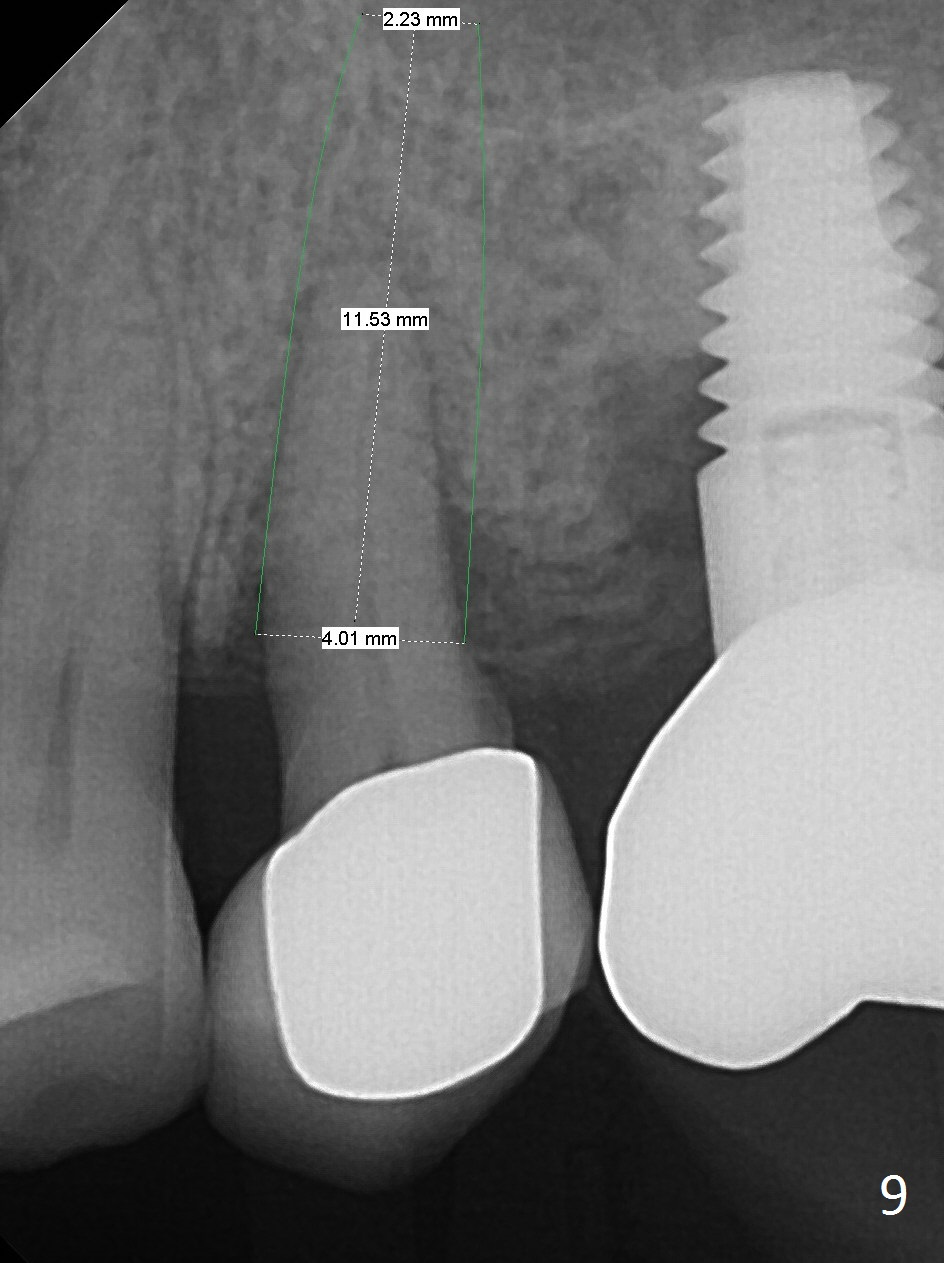
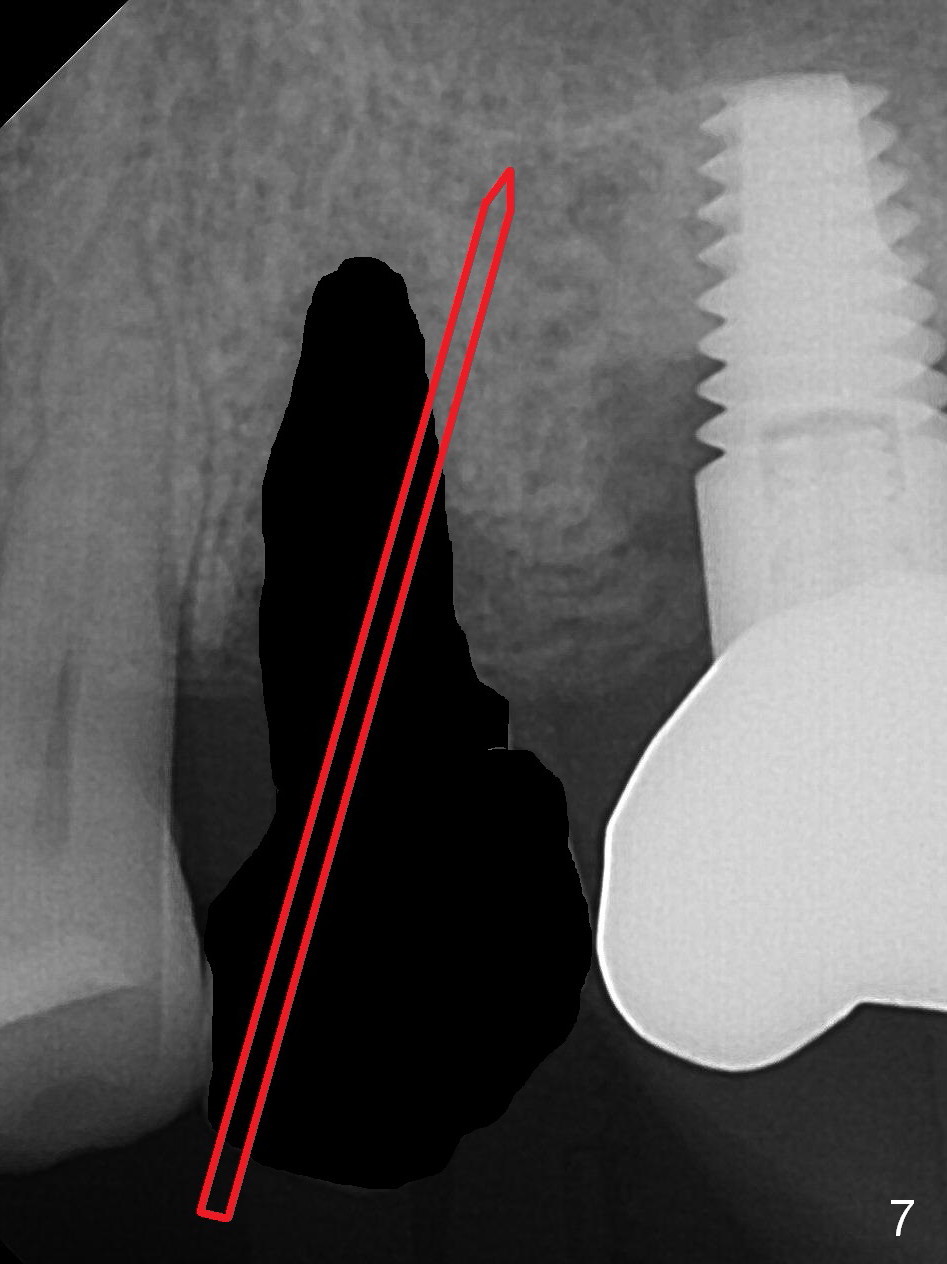
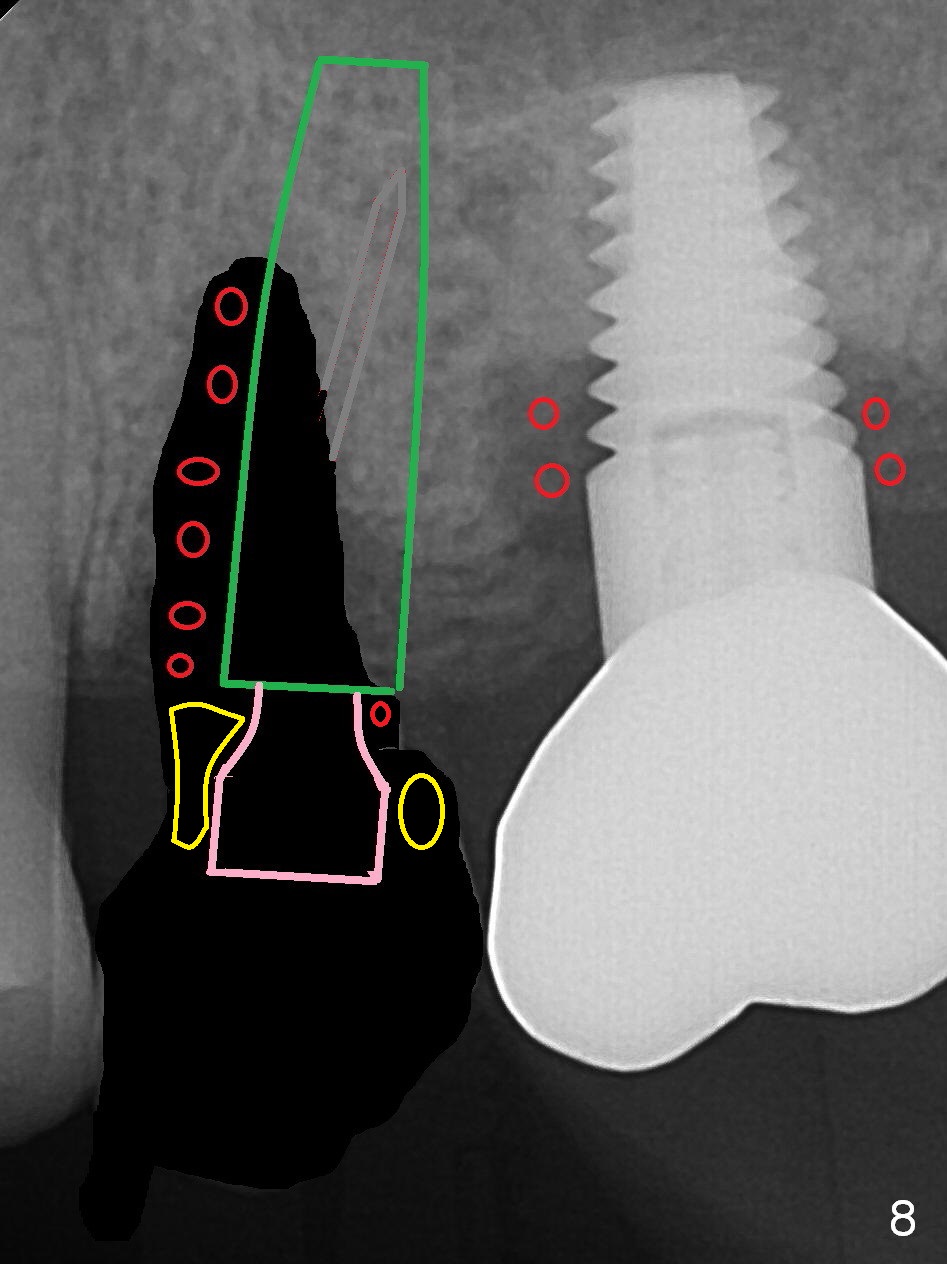
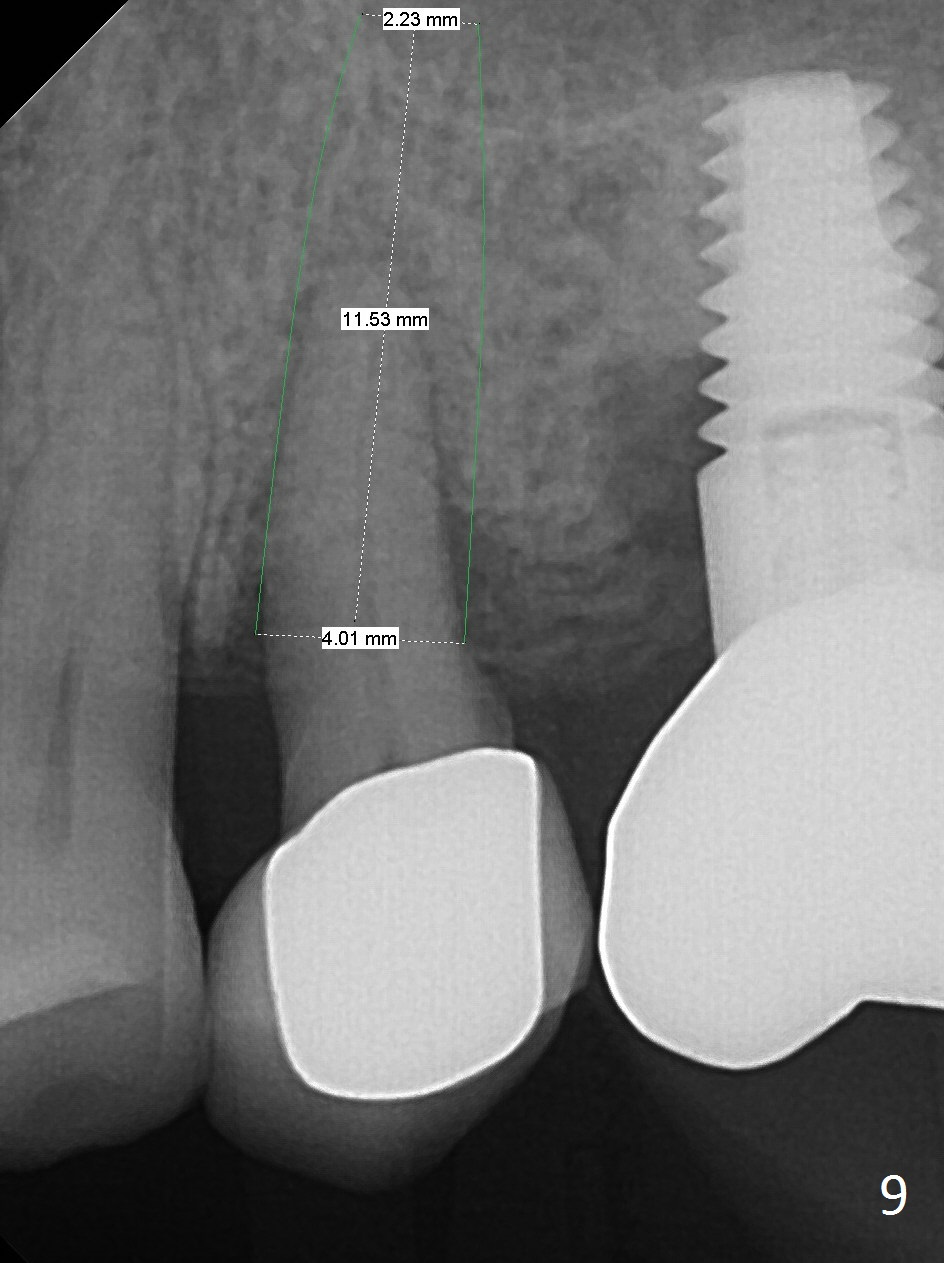
To compensate for bruxism, the implant at #13 should be as large and long as possible. After extraction (Metronidazole), take PVS impression of the socket. Start osteotomy in the distal wall of the socket (Fig.7 red). The initial depth is 11 mm (gingival level). Increase the depth once the trajectory is confirmed (Fig.9). After implant placement (Fig.8 green), place bone graft (red circles) in the mesial portion of the socket as well as in the coronal portion of the implant at #14 (incision). Use a healing abutment (pink), collagen plug (yellow) and suture to close the socket opening.
Fracture of the teeth at #5 and 8 is other manifestation of bruxism. Take PAs and photos for these two areas before surgery at #13.
Return to Upper Bicuspid Immediate Implant, IBS
Xin Wei, DDS, PhD, MS 1st edition 03/22/2017, last revision 01/19/2018