
 |
 |
 |
 |
 |
 |
Where to Place Implant?
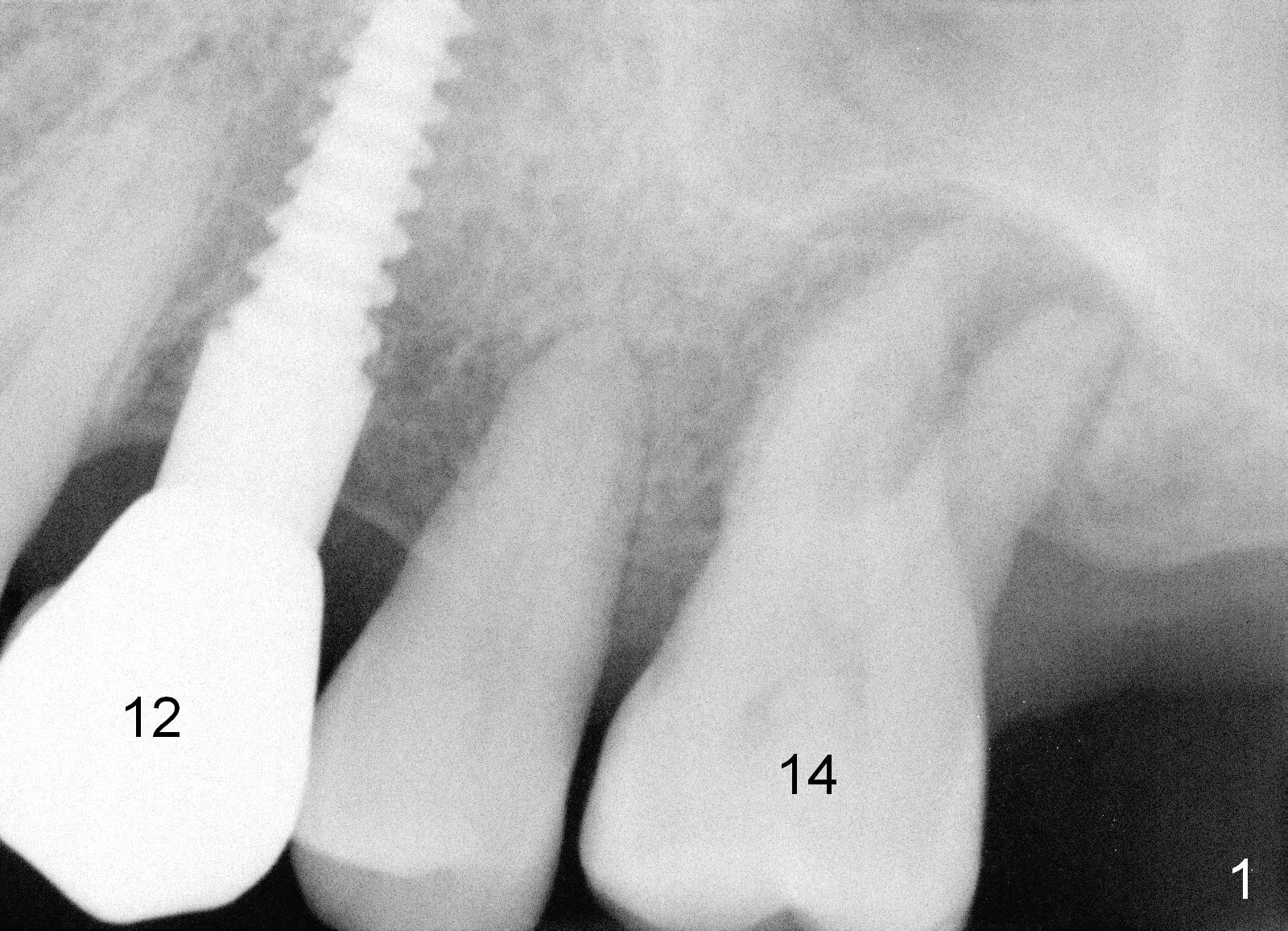
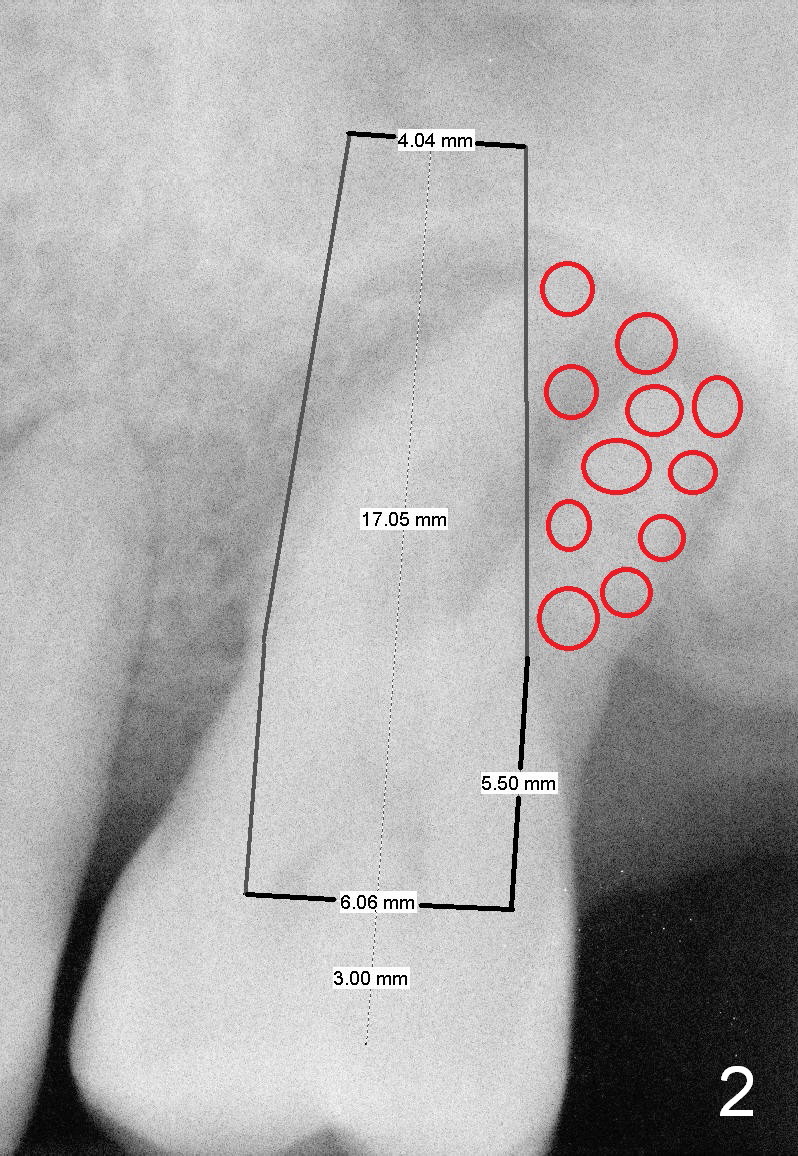
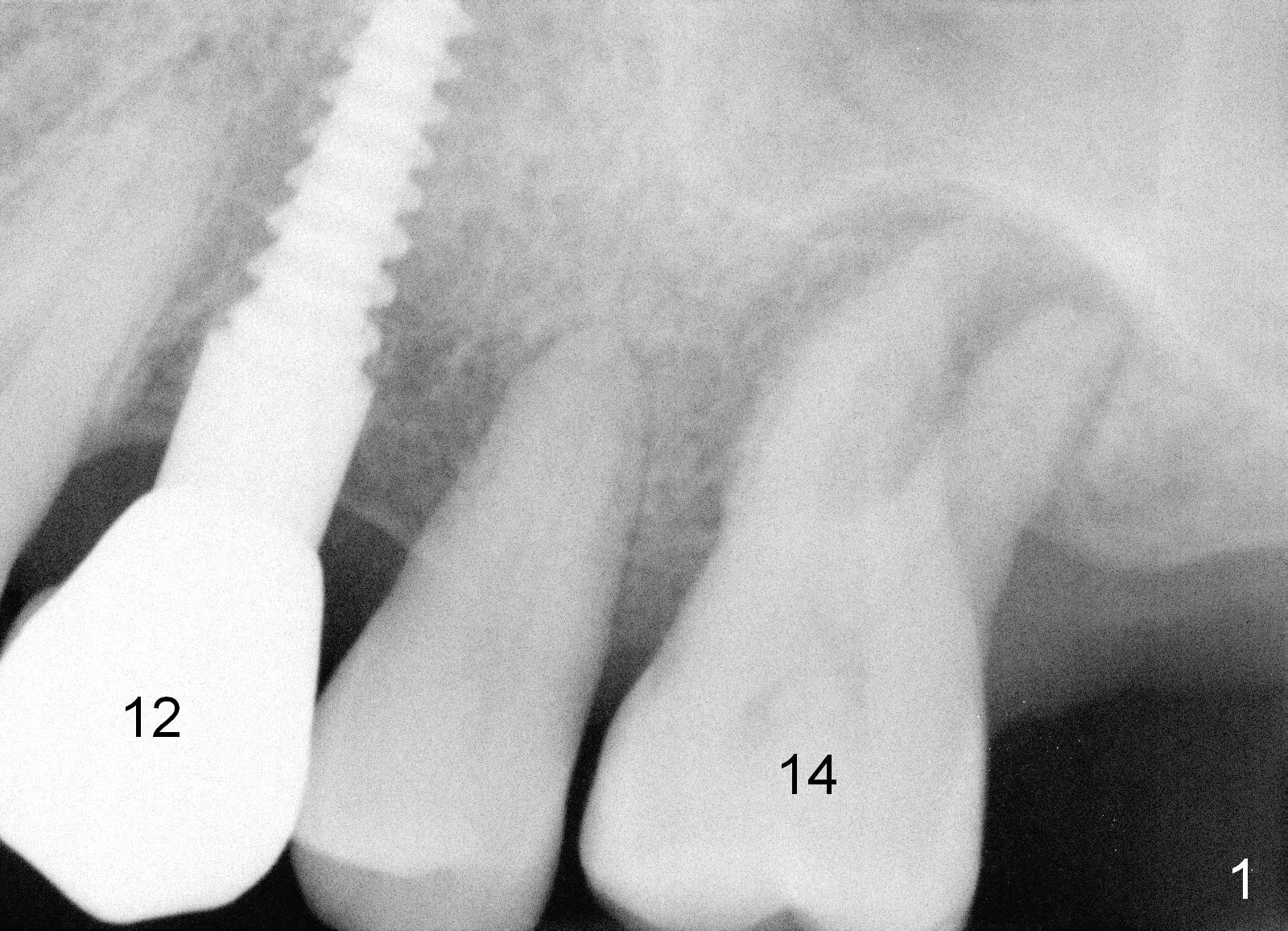
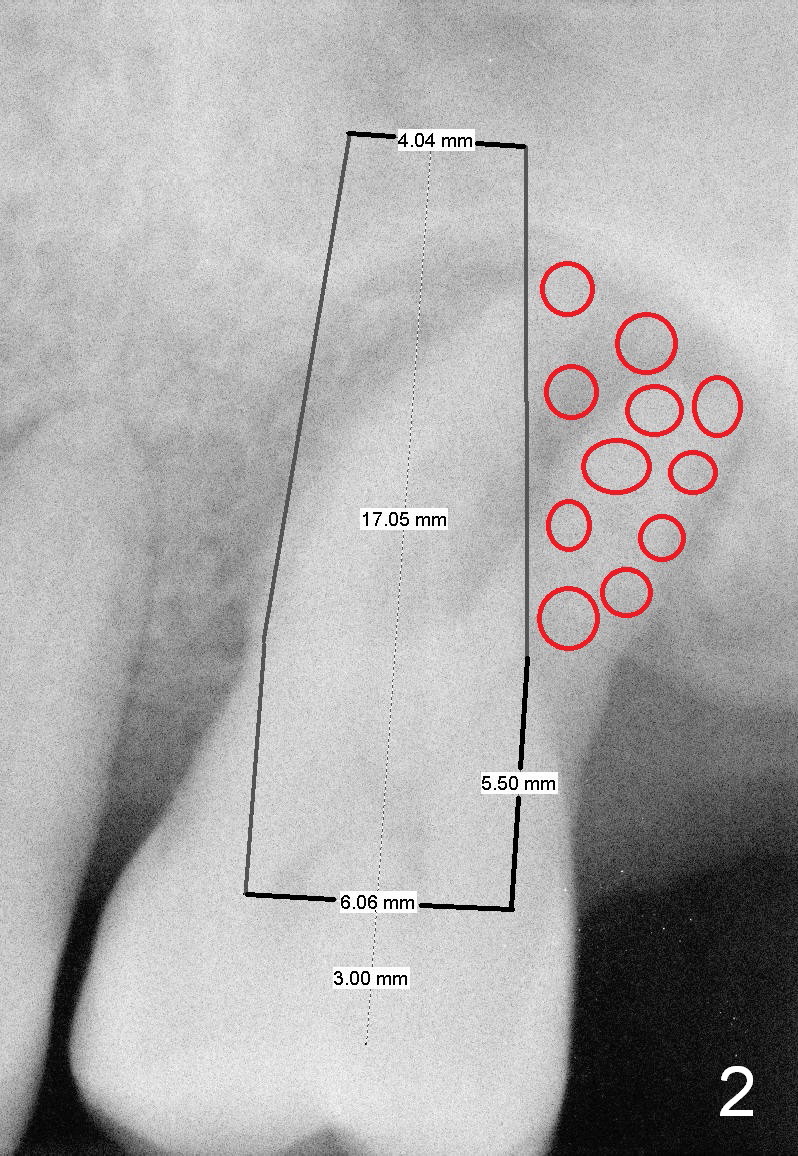
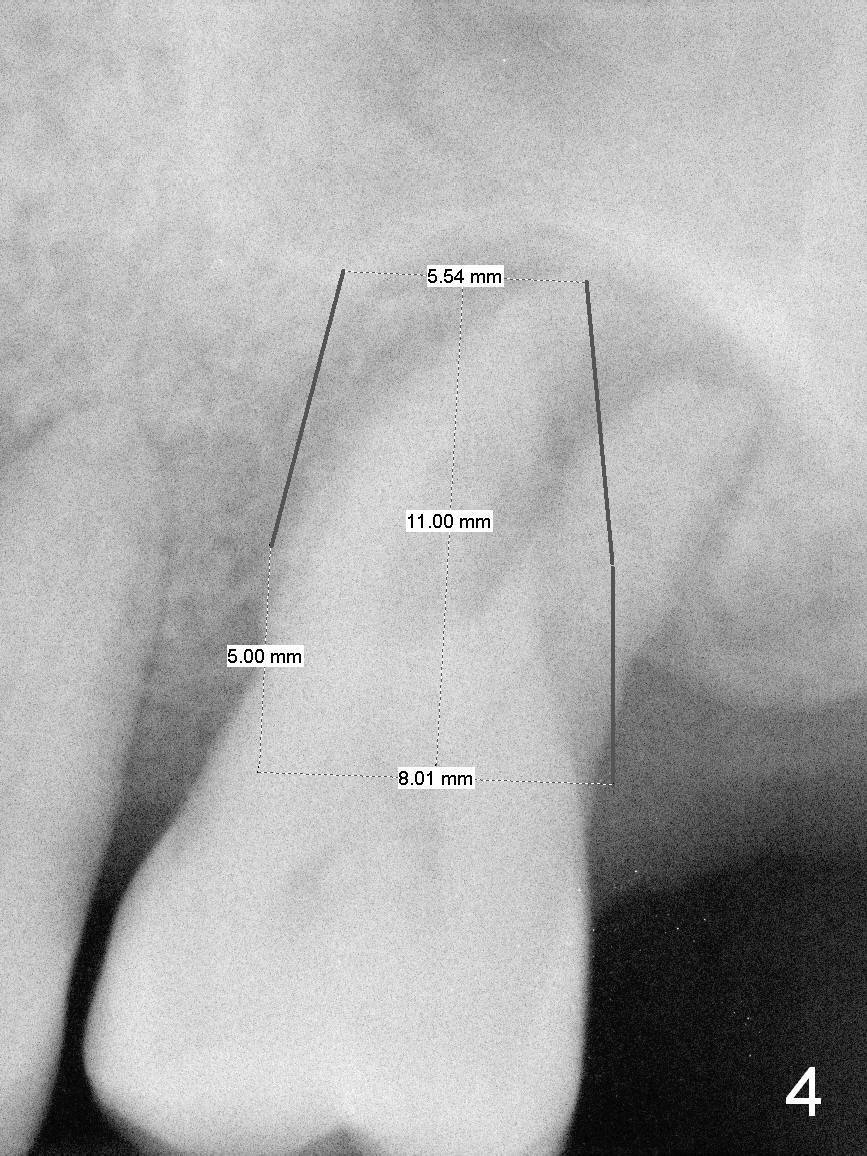
A 52-year-old man (DM) will return for #14 extraction and immediate implant nearly 2 years after #12 crown cementation. There is more bone loss distally than mesially. Clinically, the palatal recession is excessive (Fig.3). After socket debridement and 2% Xylocaine/1:50,000 Epinephrine gauze packing, osteotomy will be initiated in the buccomesial aspect of the septum, if the latter is present. Use 4.5 or 5x17 mm tap to test stability and more importantly determine how much thread exposure can occur palatally before placing a 14 or 17 mm long implant (Fig.2). A fair amount of bone graft will be inserted distopalatally (red circles in Fig.2). If primary stability is achieved, use an immediate provisional to close the socket opening.
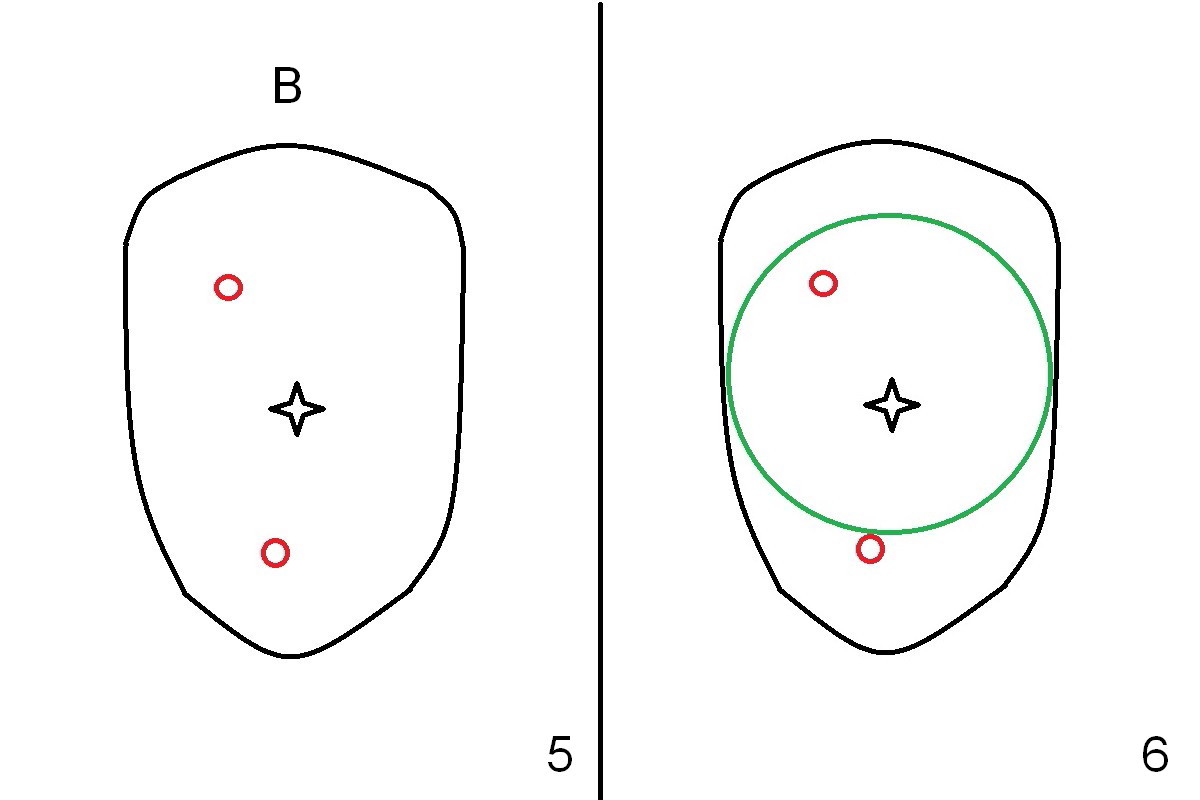
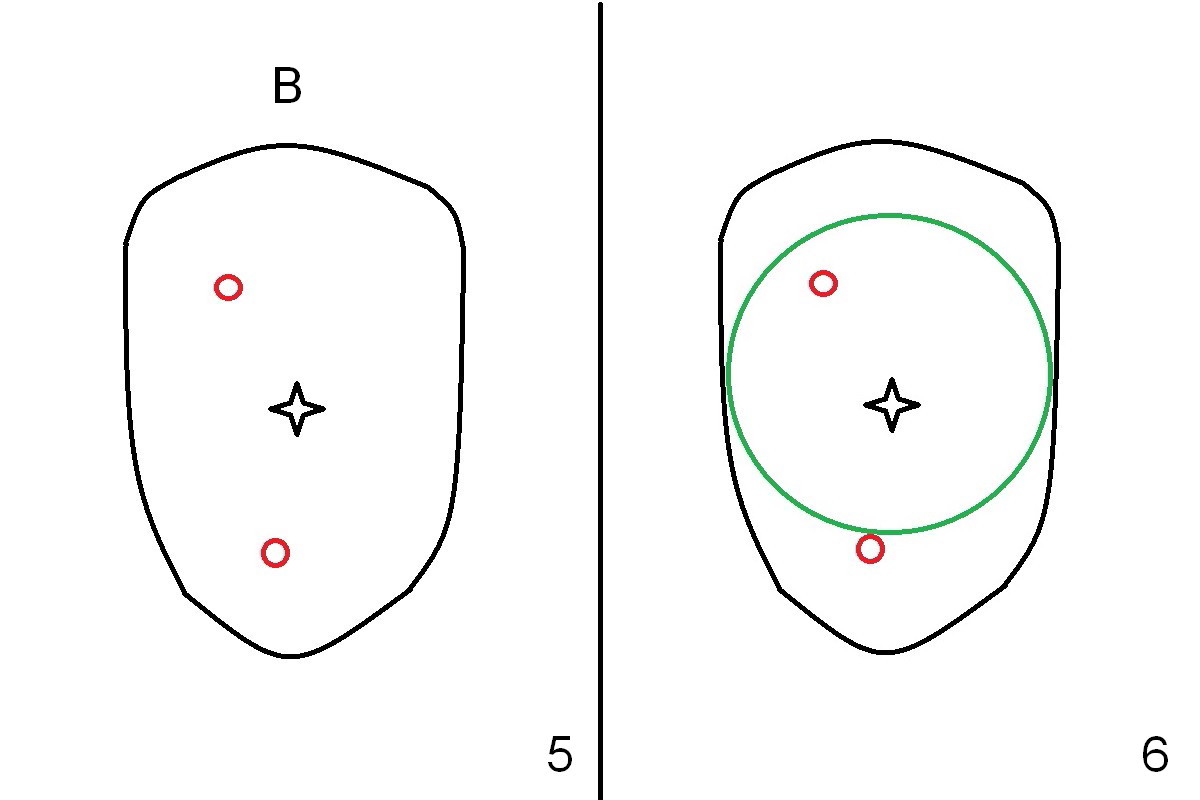
When the tooth is extracted, there is abundant granulation tissue in the socket. There is a perforation in the middle of the socket (Fig.5 (occlusal view of the socket) black star). A 2 mm osteotome is used to create an osteotomy palatally or buccally (Fig.5 red circles). The bone is less than 1 mm. As expected, the palatal wall is low. It appears that socket preservation is the treatment option. After placement of Osteotape in the bottom and palatal wall of the socket, allograft mixed with Osteogen is placed. The graft is covered by a 6-month collagen membrane, which is sutured in place. Implant placement is scheduled in 4-6 months. Although this is an acceptable treatment modality, it is not the best.
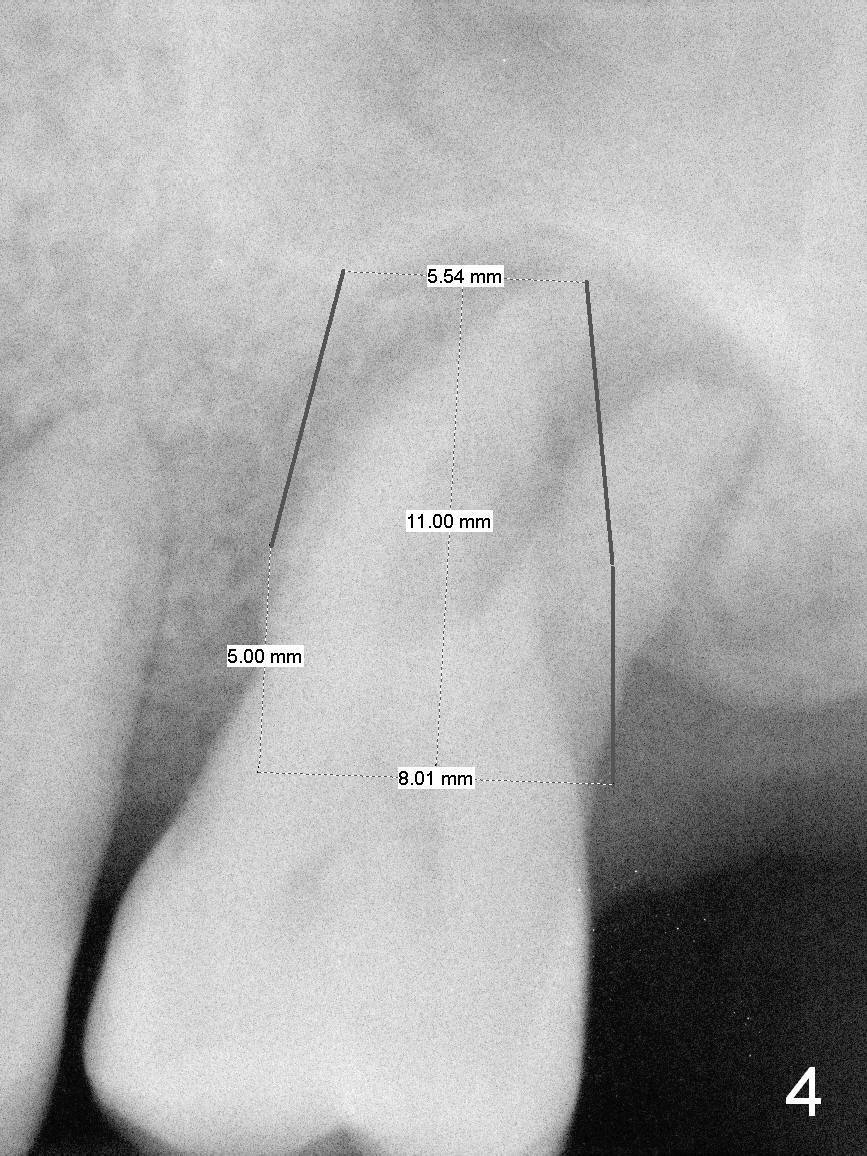
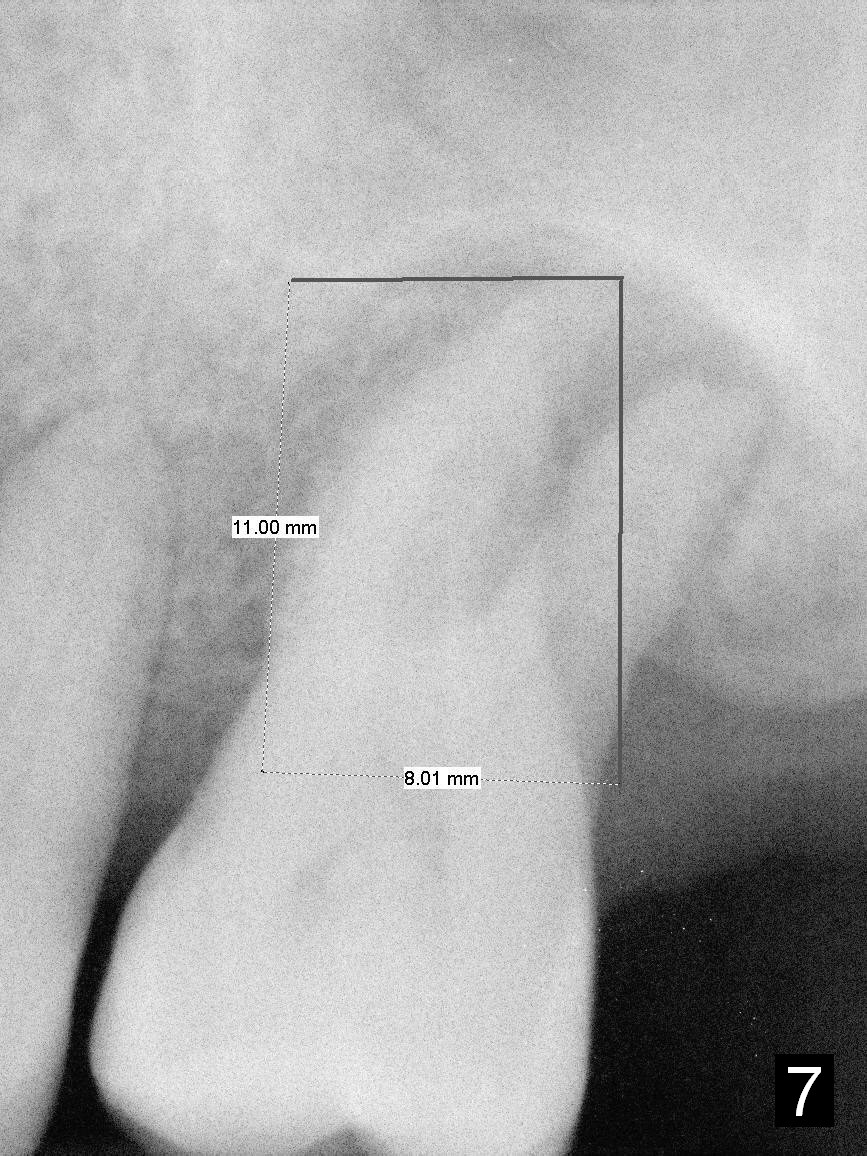
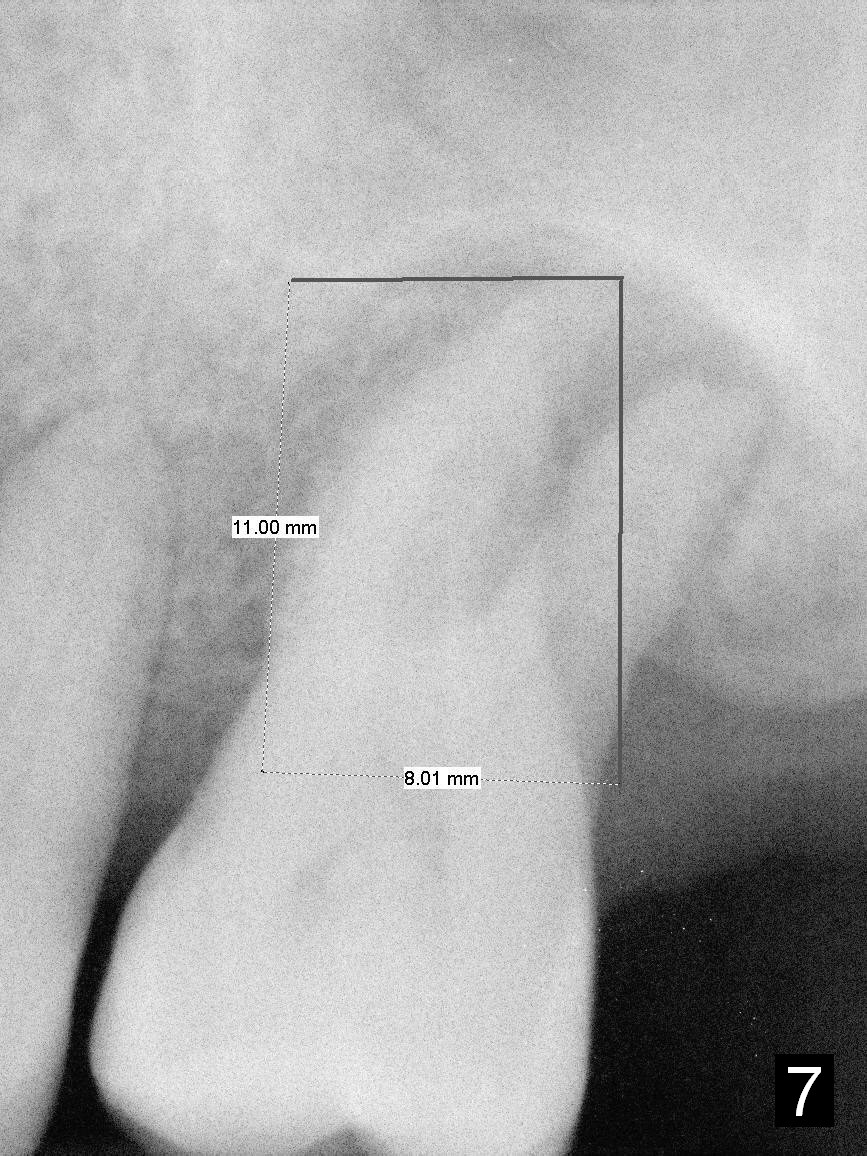
A large implant is place so that the mesiodistal dimension of the socket is obliterated by the implant (Fig.6 green circle). The buccal (Fib.5 B) and palatal gaps are filled with bone graft. It appears that either tapered (Fig4) or cylindrical (Fig.7) implant should be able to occupy the socket and obtain primary stability without perforating the sinus floor.
Return to Upper Molar Immediate Implant
Xin Wei, DDS, PhD, MS 1st edition 10/18/2015, last revision 02/07/2016