



 |
 |
 |
|||
 |
 |
 |
|||
 |
 |
 |
 |
 |
 |
Implant Forms Osteotomy
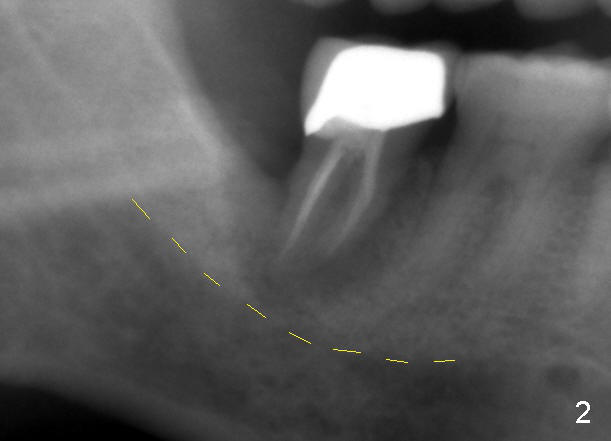
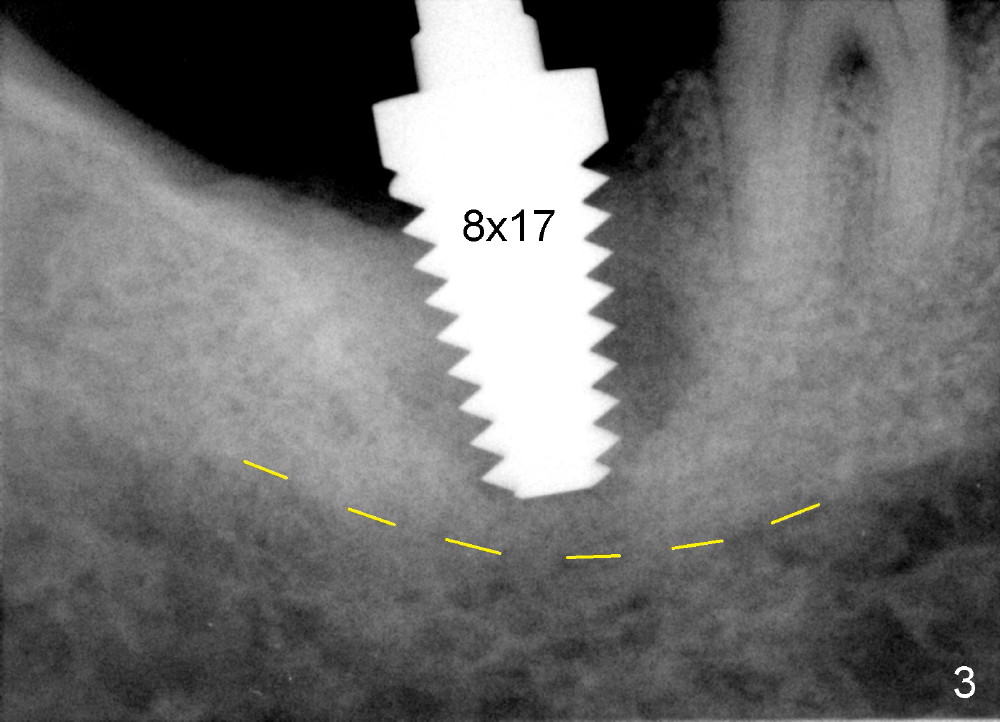
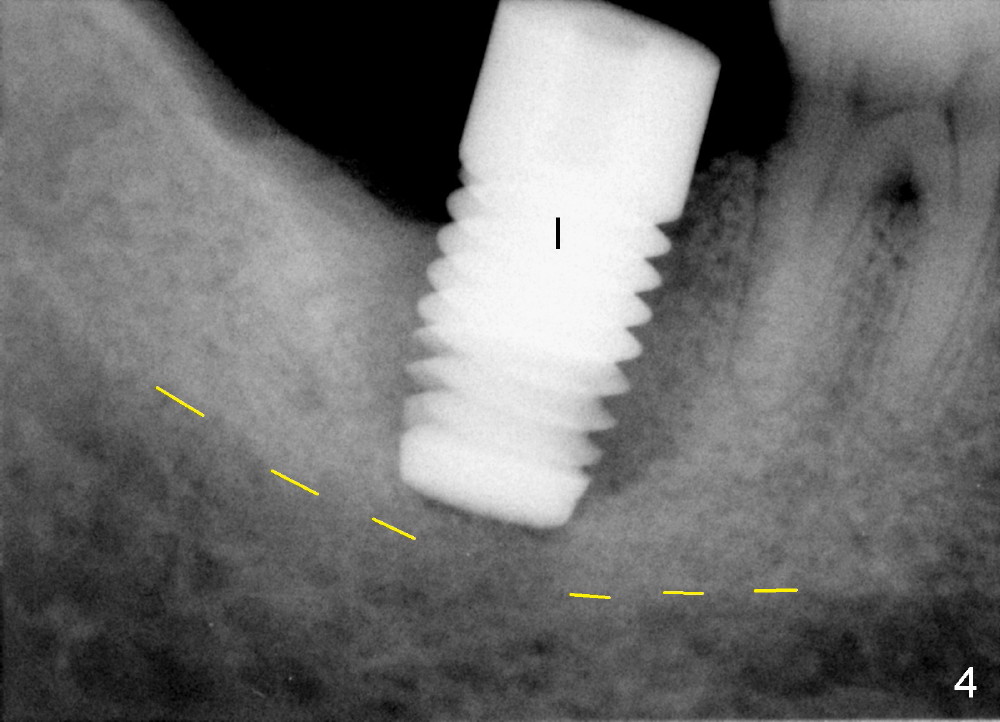
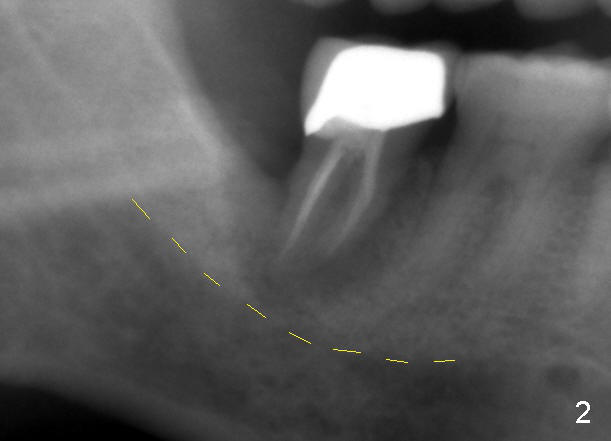
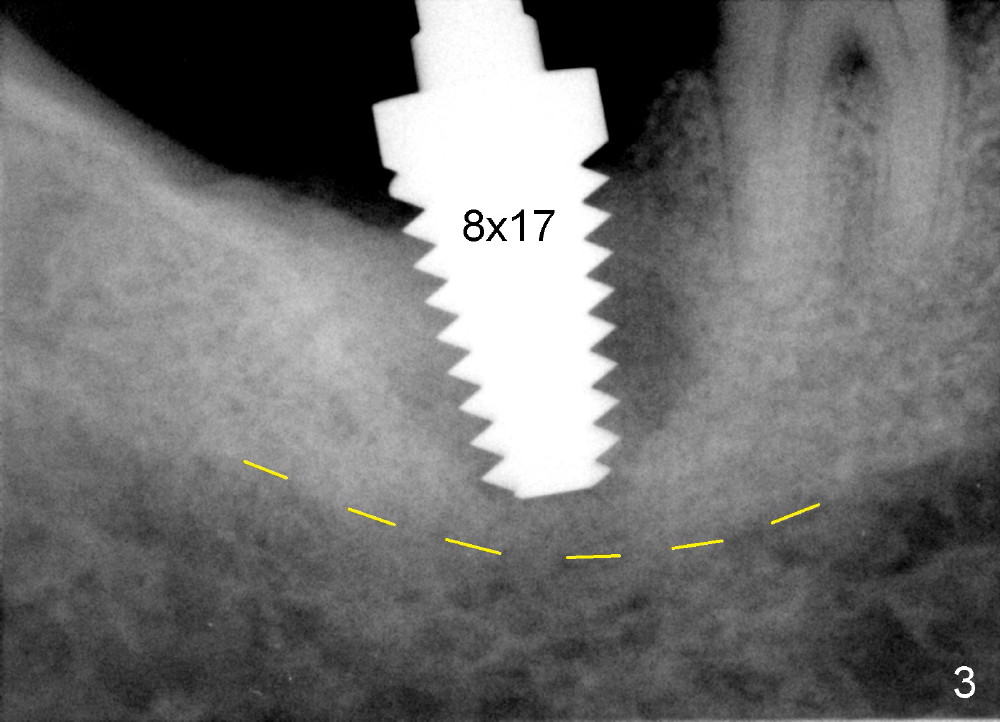
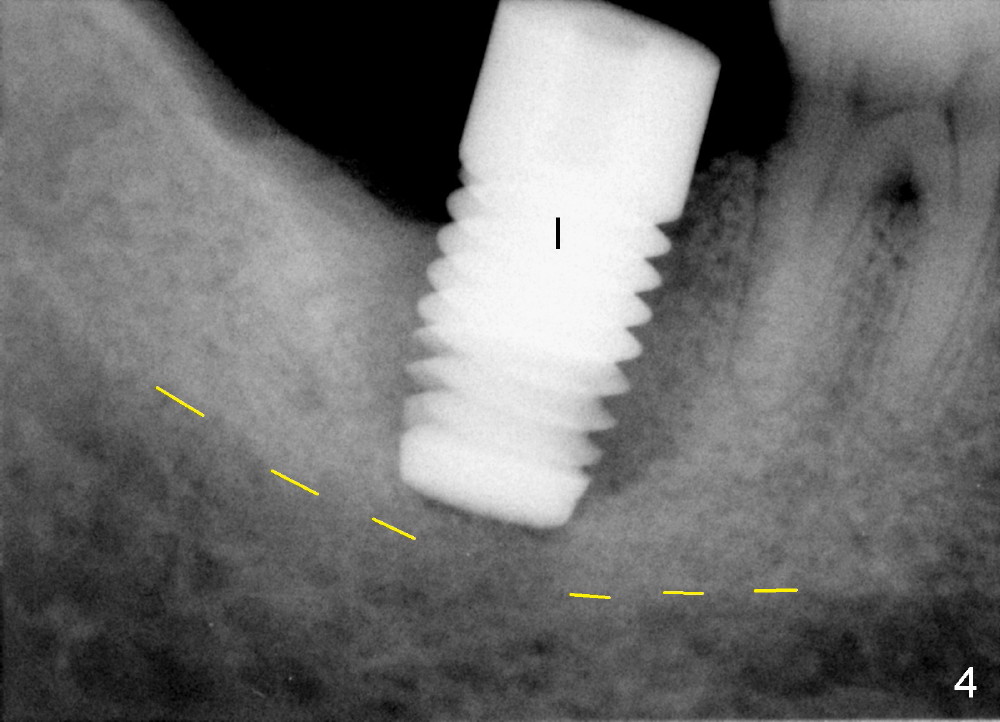
A 51-year-old man is a probable bruxer and has developed signs and symptoms consistent with root fracture at the lower right 2nd molar for 2 years (Fig.1). The periradicular radiolucency appears to have increased 8 month ago (Fig.2, trimmed from a panoramus; yellow dashed line: upper border of the Inferior Alveolar Canal, IAC). Finally he agrees to have extraction. The socket is extremely large with intact walls. When a 8x17 mm tapered tap is inserted, it is loose (Fig.3). There is no binding when a 7.5 mm cylindrical osteotome is placed. Since there is no corresponding tap available, a 8x17 mm cylindrical implant is used to form osteotomy slowly and steadily and finish placement with insertion torque between 45 and 50 Ncm (Fig.4). Radiologically the apex of the implant is engaged to the bottom of the socket, whereas clinically the implant contacts the buccal and lingual plates. There is space mesially and distally for bone graft. No paresthesia is reported postop. The point is no drill being used for osteotomy when the socket is close to IAC. The patient returns for follow up 12 days postop. The perio dressing is dislodged, whereas the implant remains stable. There is no sign of infection. The gingiva attaches to the implant tightly. There is no excessive gingival recession, either buccal or lingual (data not shown).
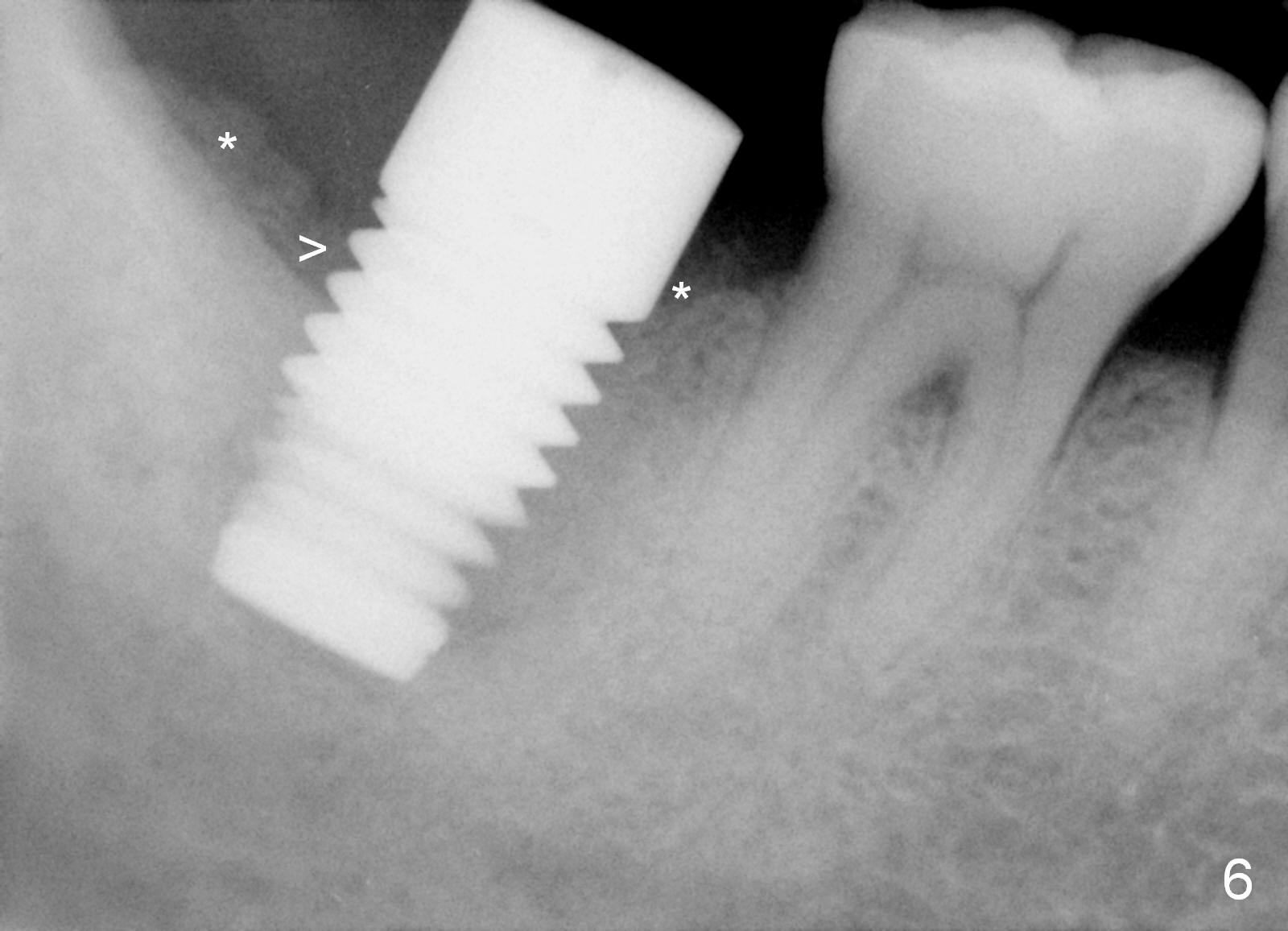
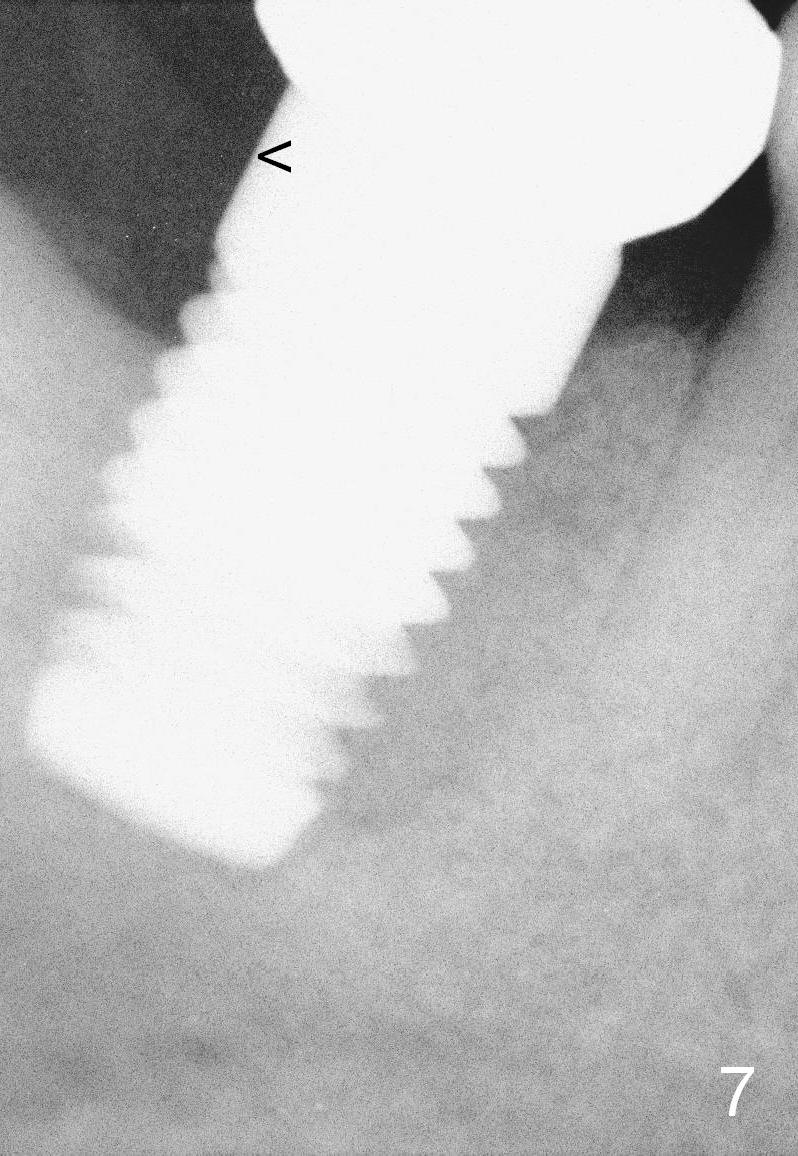
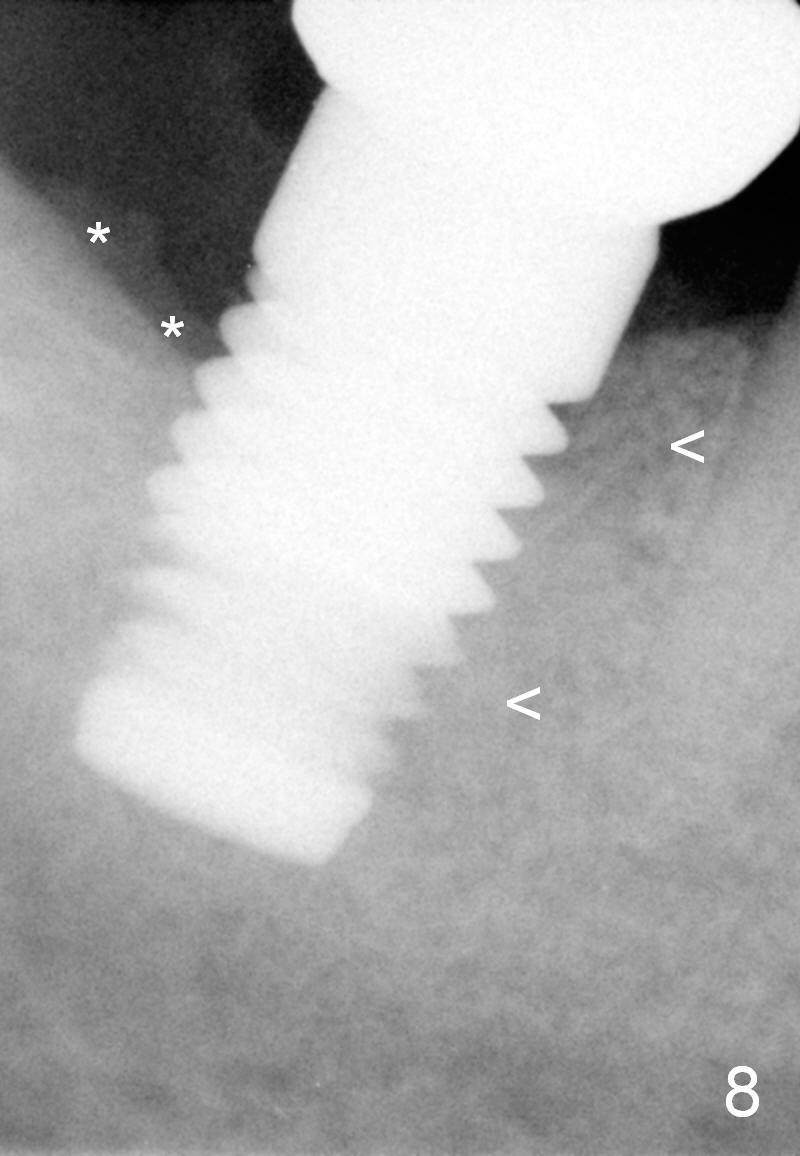
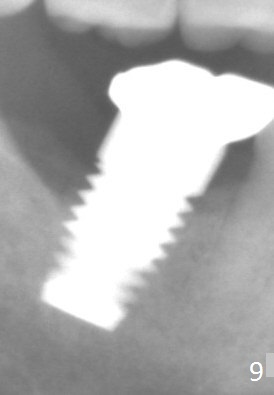
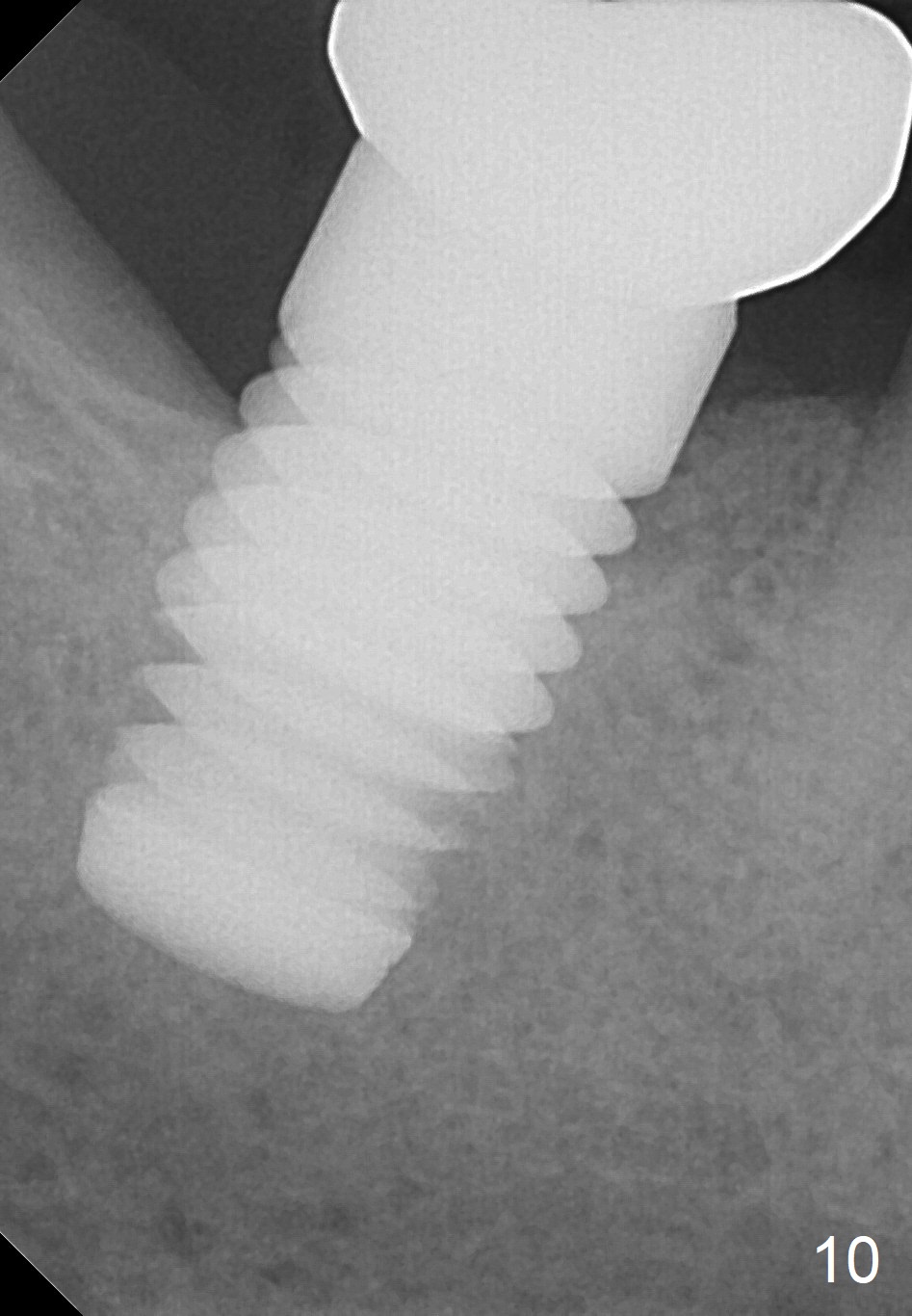
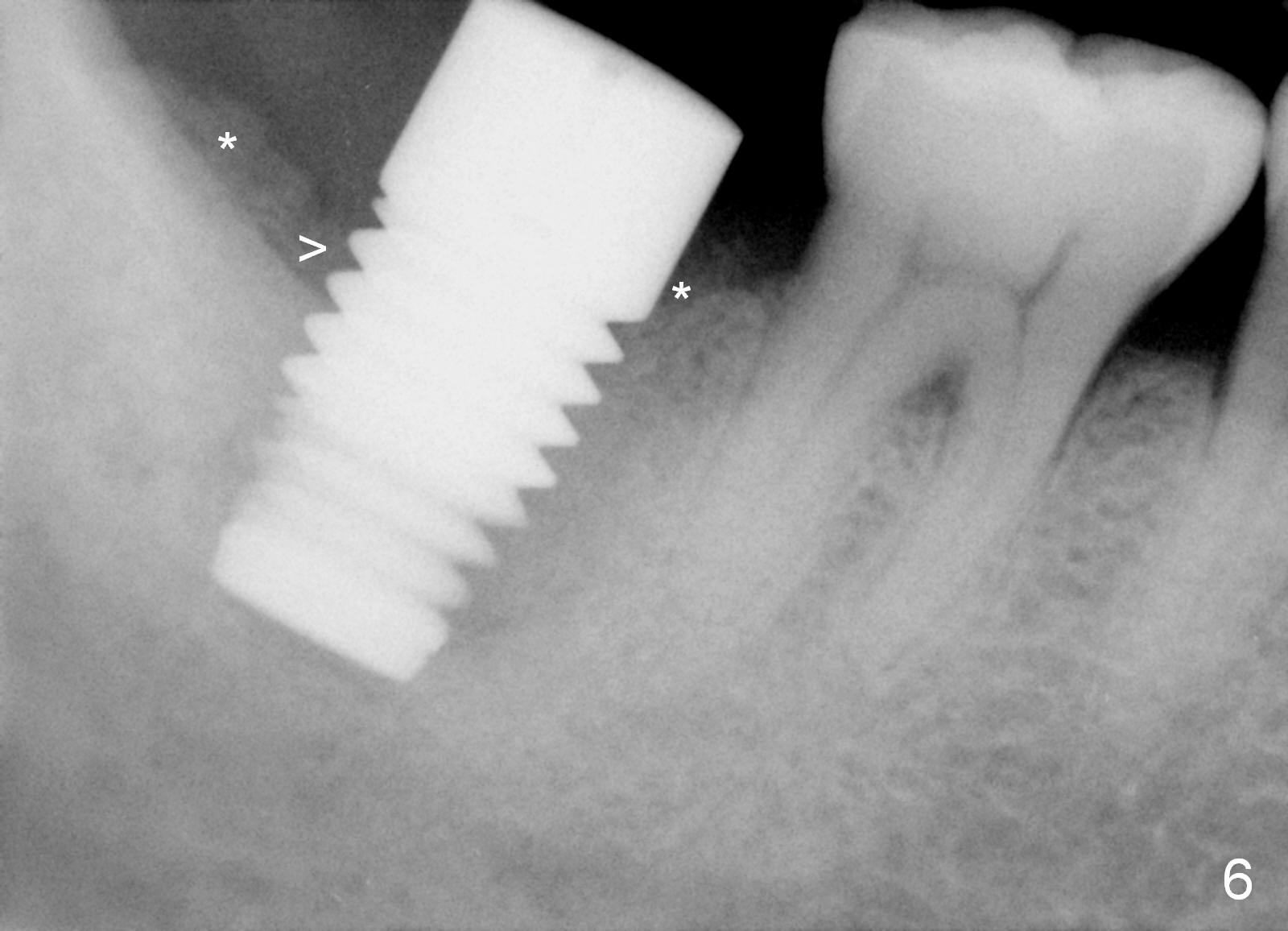
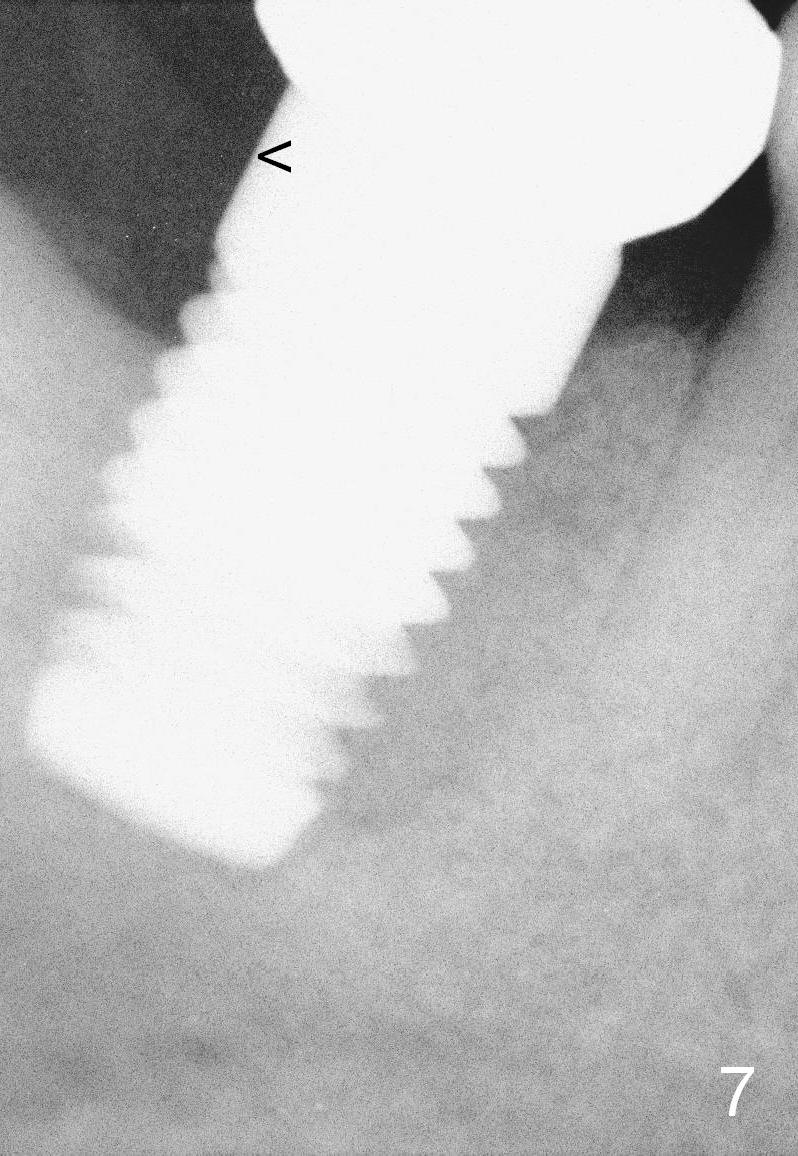
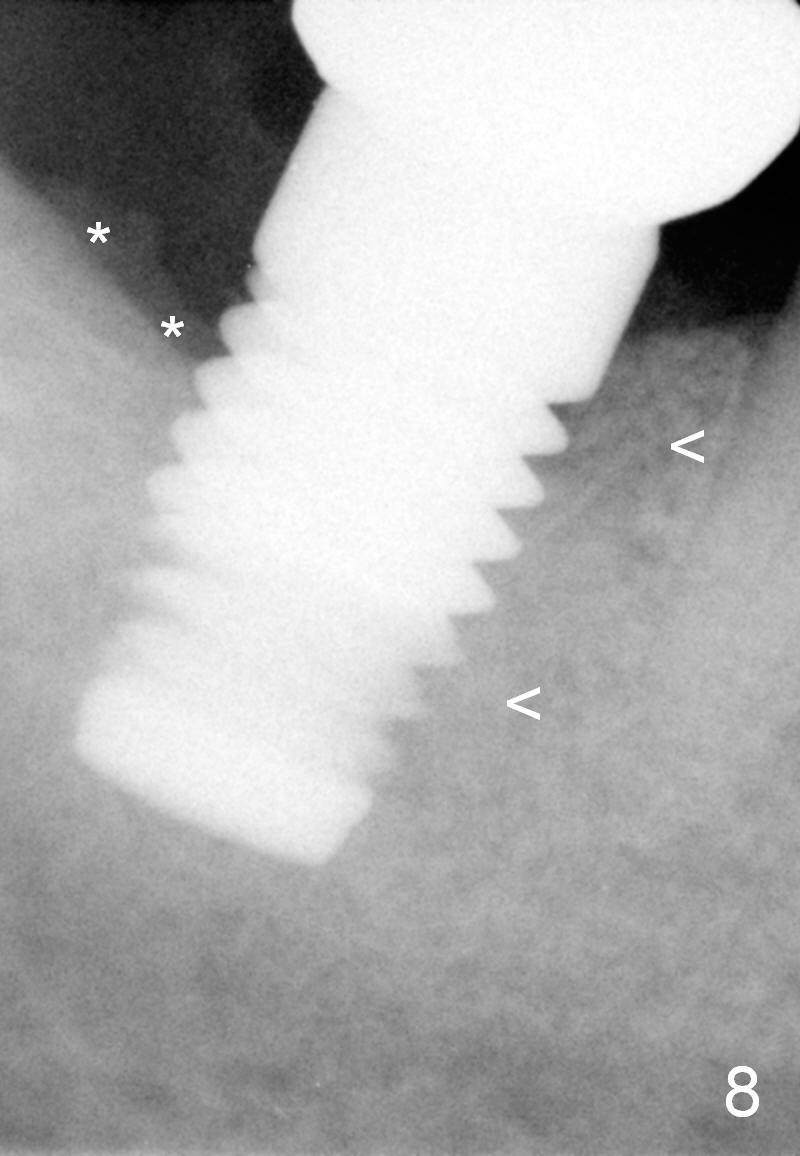
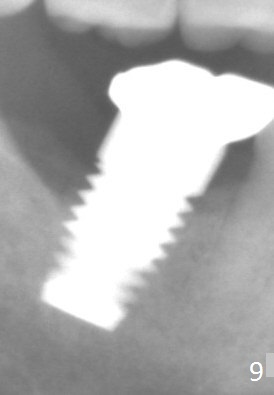
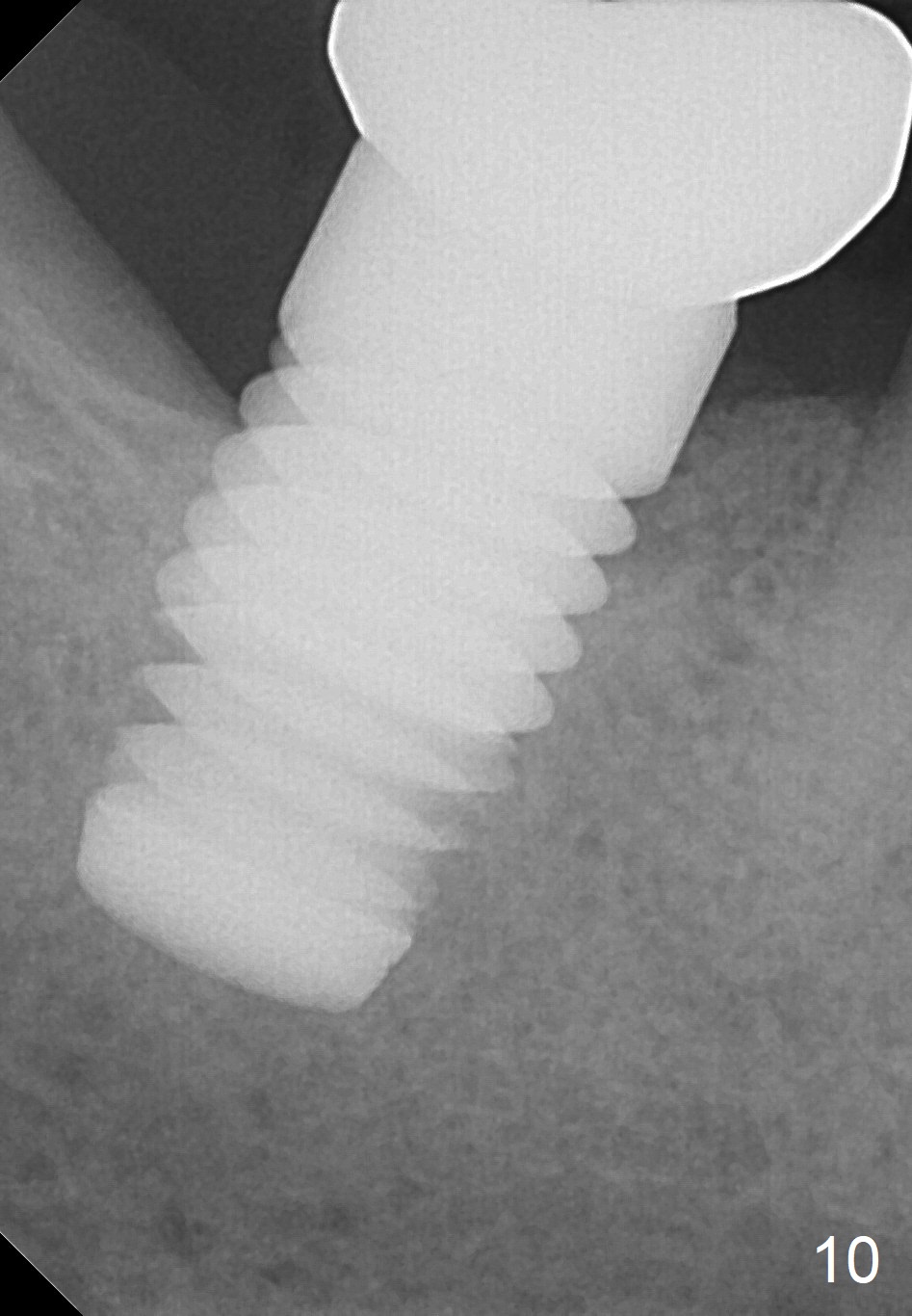
Although the buccal gingiva is recessed, the soft tissue around the implant is healthy 2 months postop (Fig.5). The implant is stable. X-ray at the same time shows bone graft (Fig.6 *) deposited near implant threads (>). The definitive restoration is delivered 3 months postop. Fig.7 is taken 1 month post cementation; the crown margin is supragingival (<: gingival margin), which is easy for cement removal. Seven months post cementation (10 months postop), the bone graft remains distal to the implant (Fig.8 *), while bone density mesial to the implant continues to increase (<). There is no bone loss 2 years post cementation (Fig.9 (pan)) or 2 years 7 months post cementation (Fig.10-12), although the rough part of the implant remains exposed buccolingually. The implant should have been smaller in diameter or placed deeper with a shorter implant.
Once the infected source is removed, primary stability is achieved and bone graft is placed, a large implant is most likely to heal in a large socket.
Return to
Lower Molar Immediate Implant Course
1
2
Upper
Lower
Cases
Xin Wei, DDS, PhD, MS 1st edition 11/16/2014, last revision 12/22/2018