
,%20bone%20graft.jpg)

.jpg)
 |
 |
 |
,%20bone%20graft.jpg) |
 |
 |
 |
  |
.jpg) 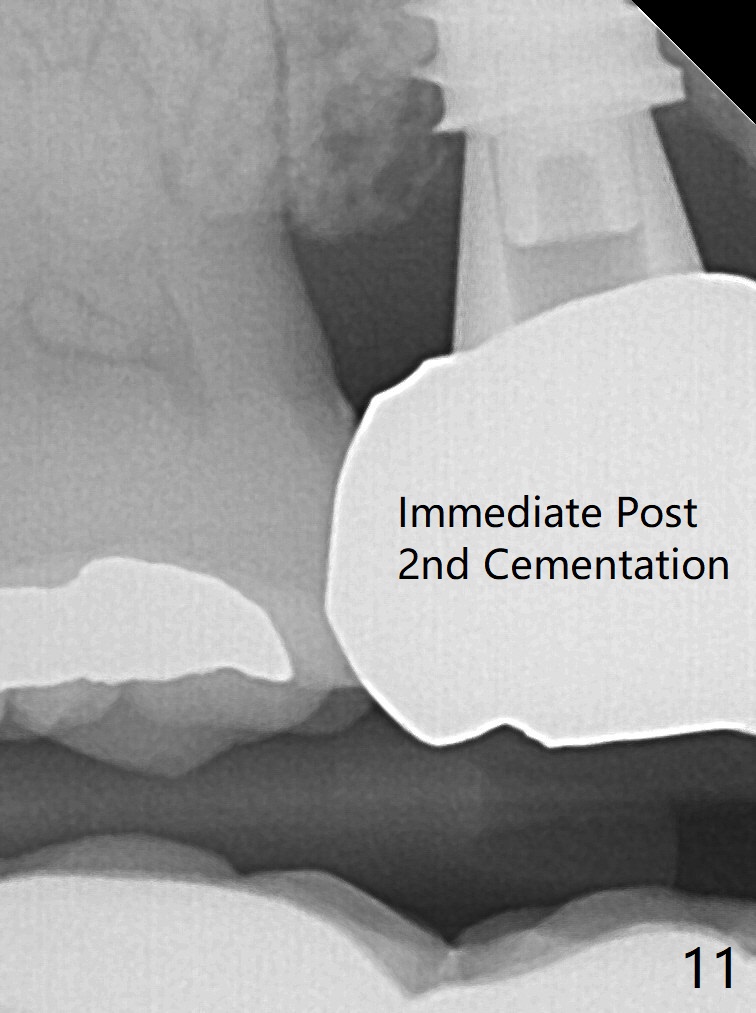 |
 |
Implant Placed in Septum
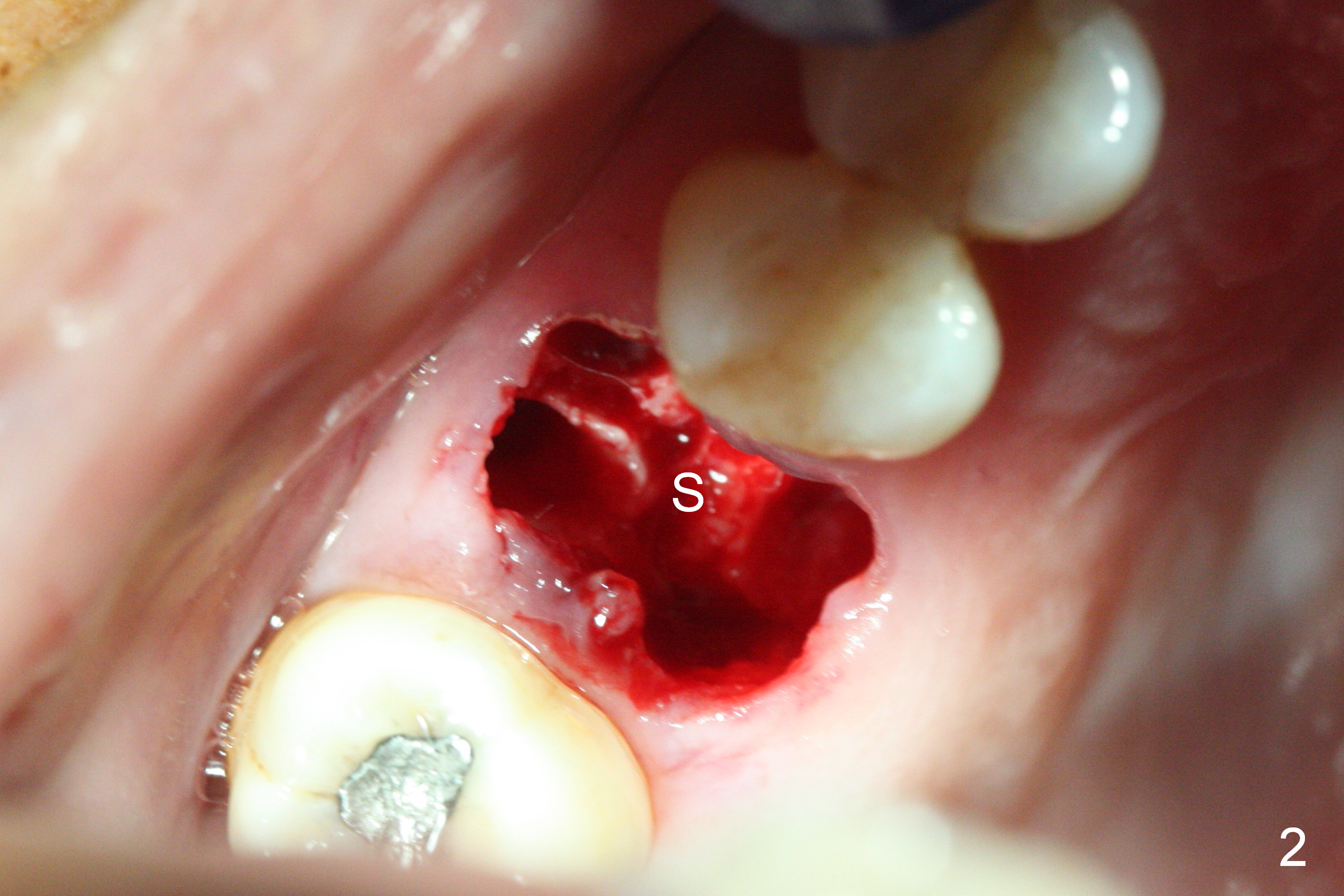
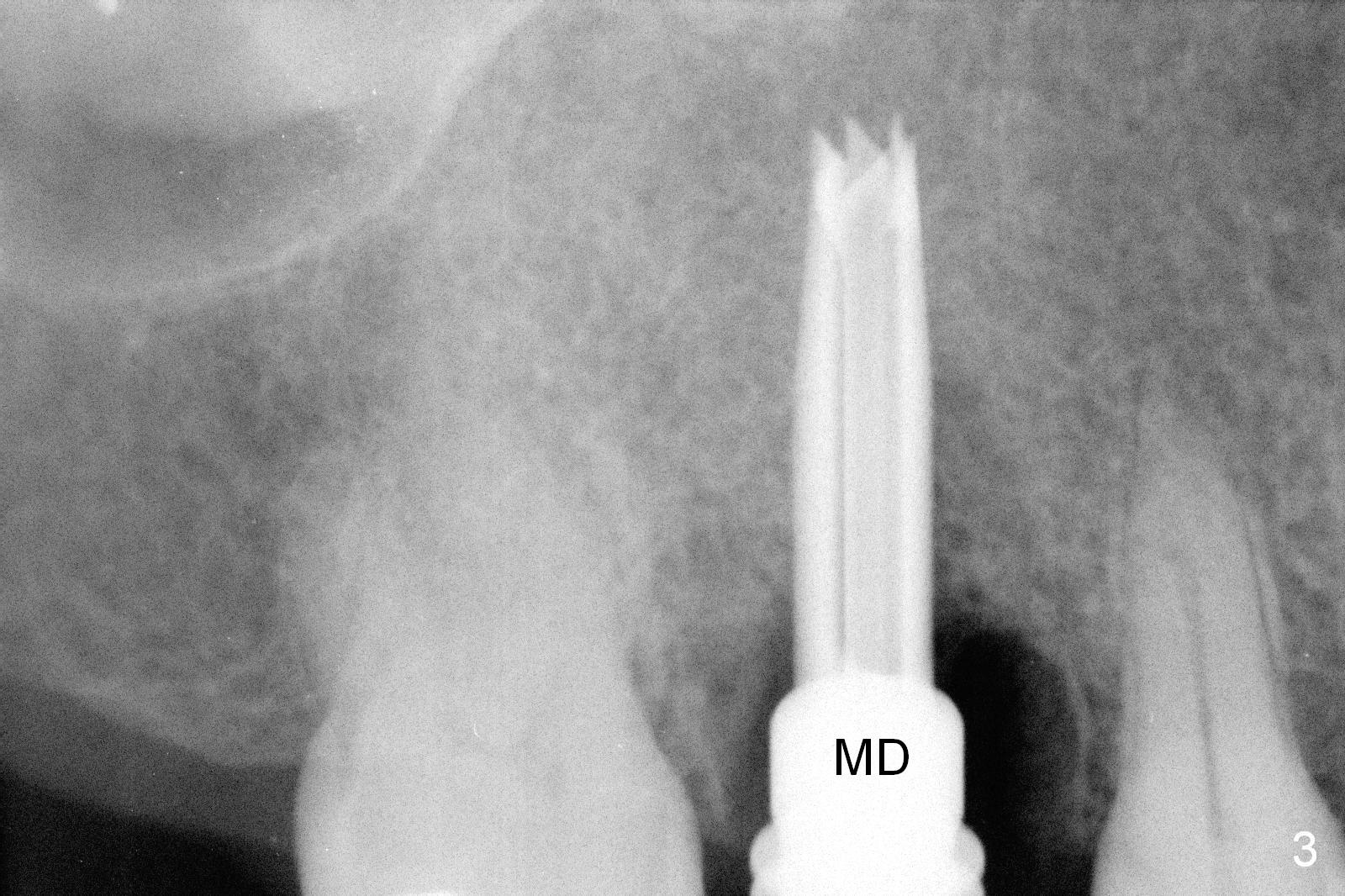
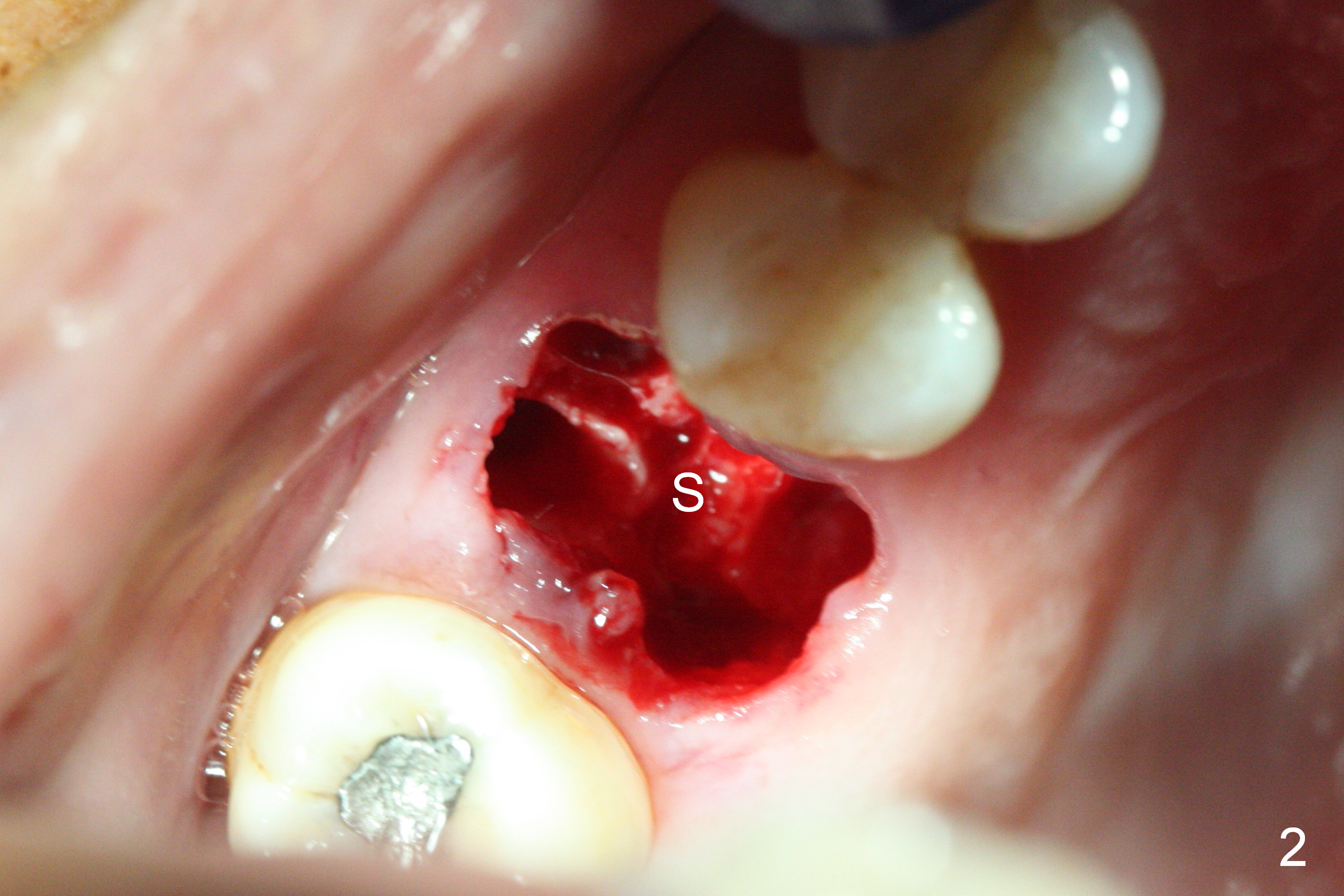
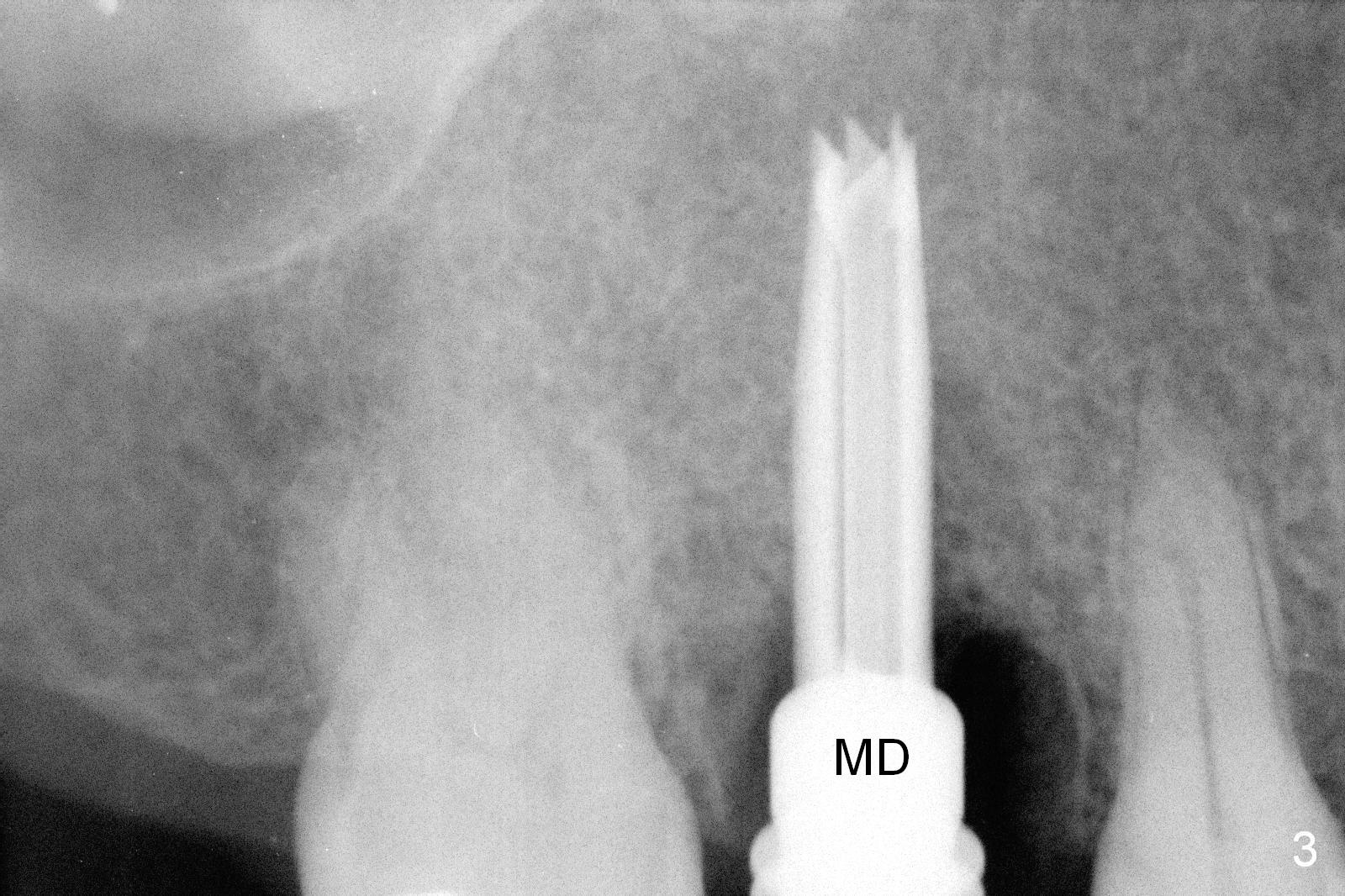
The polyp in the pulpal chamber of the tooth #3 (Fig.1) originates from the distal gingiva. After extraction, buccal plate perforation is found apical to the distobuccal socket. The septum is large (Fig.2 S). Osteotomy is initiated in the middle of the septum with 1.6 mm drill until 3.8 mm Magic Drill (MD) (Fig.3). The last drill is 4.3 mm, followed by 4.8 mm Magic Expander since the palatal wall of the osteotomy is thin after the last drill. A 5x13 mm IBS implant is placed with ~ 45 Ncm. The apical portion of the 3 sockets is filled with Osteogen plug and the coronal portion with autogenous bone (harvested from MD), mixed with allograft and Osteogen (Fig.4 * as well as collagen plug in the most superficial portion of the sockets). A 6.5x4(4) mm pair abutment (Fig.4 A) is placed to hold an immediate provisional in place.
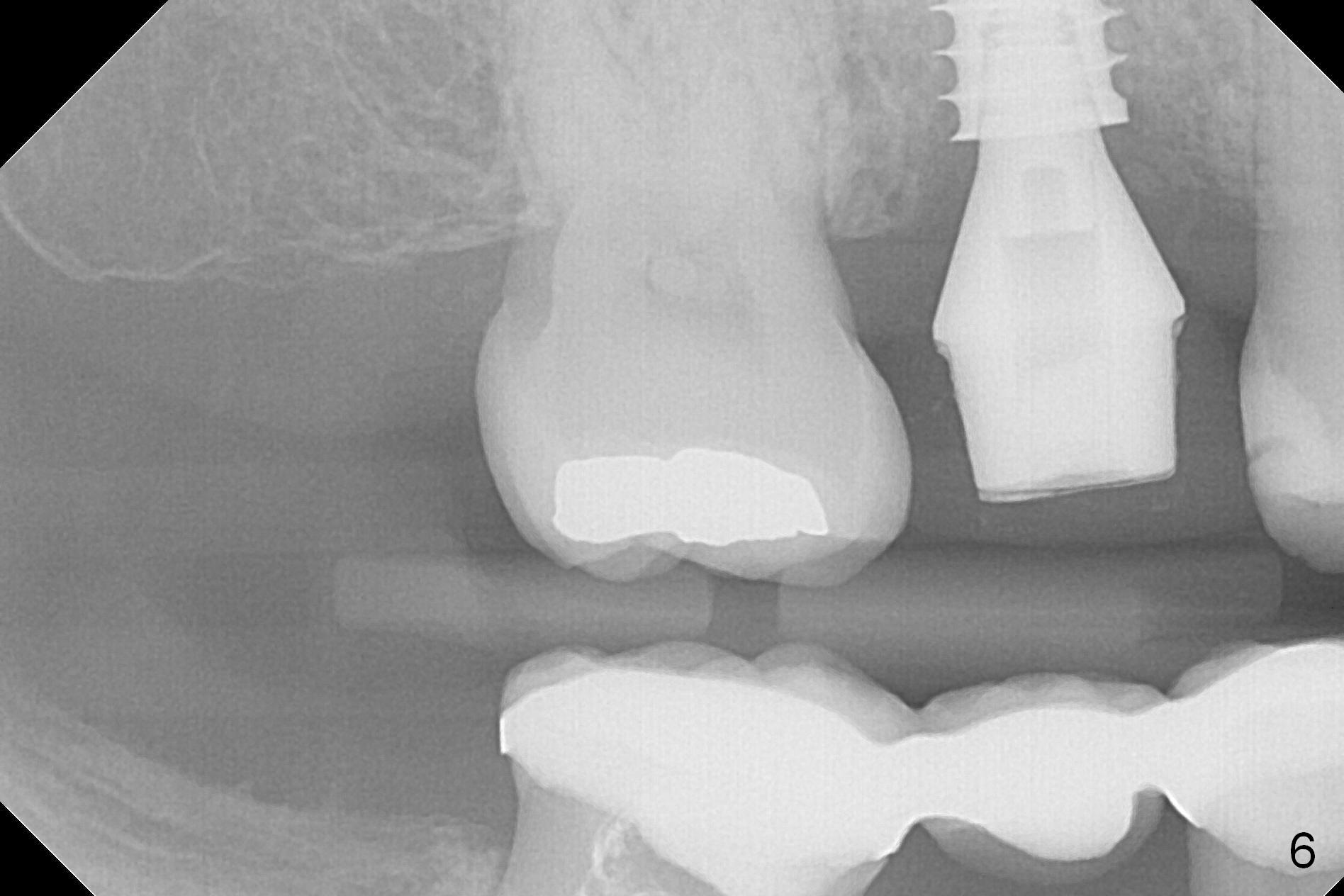
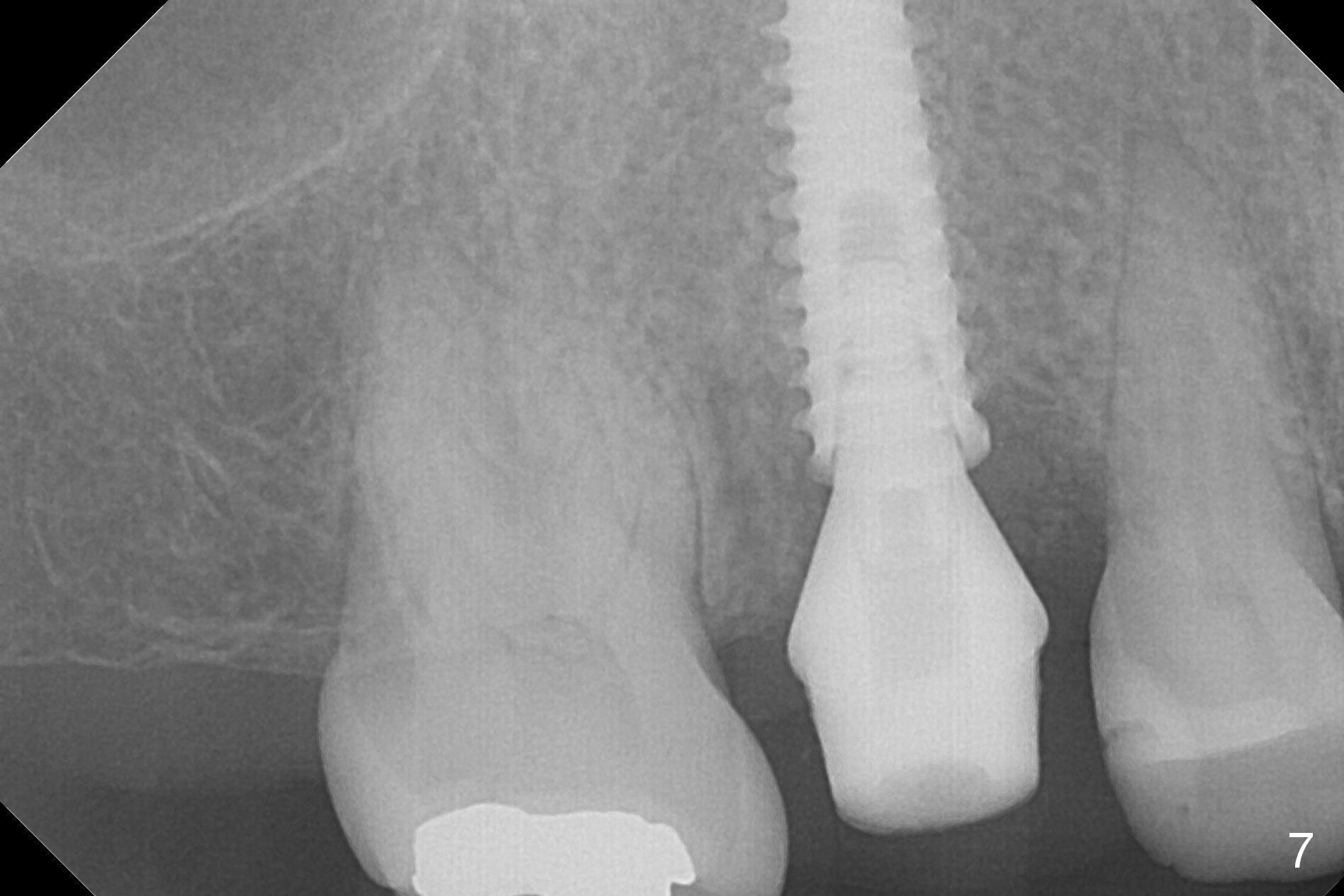
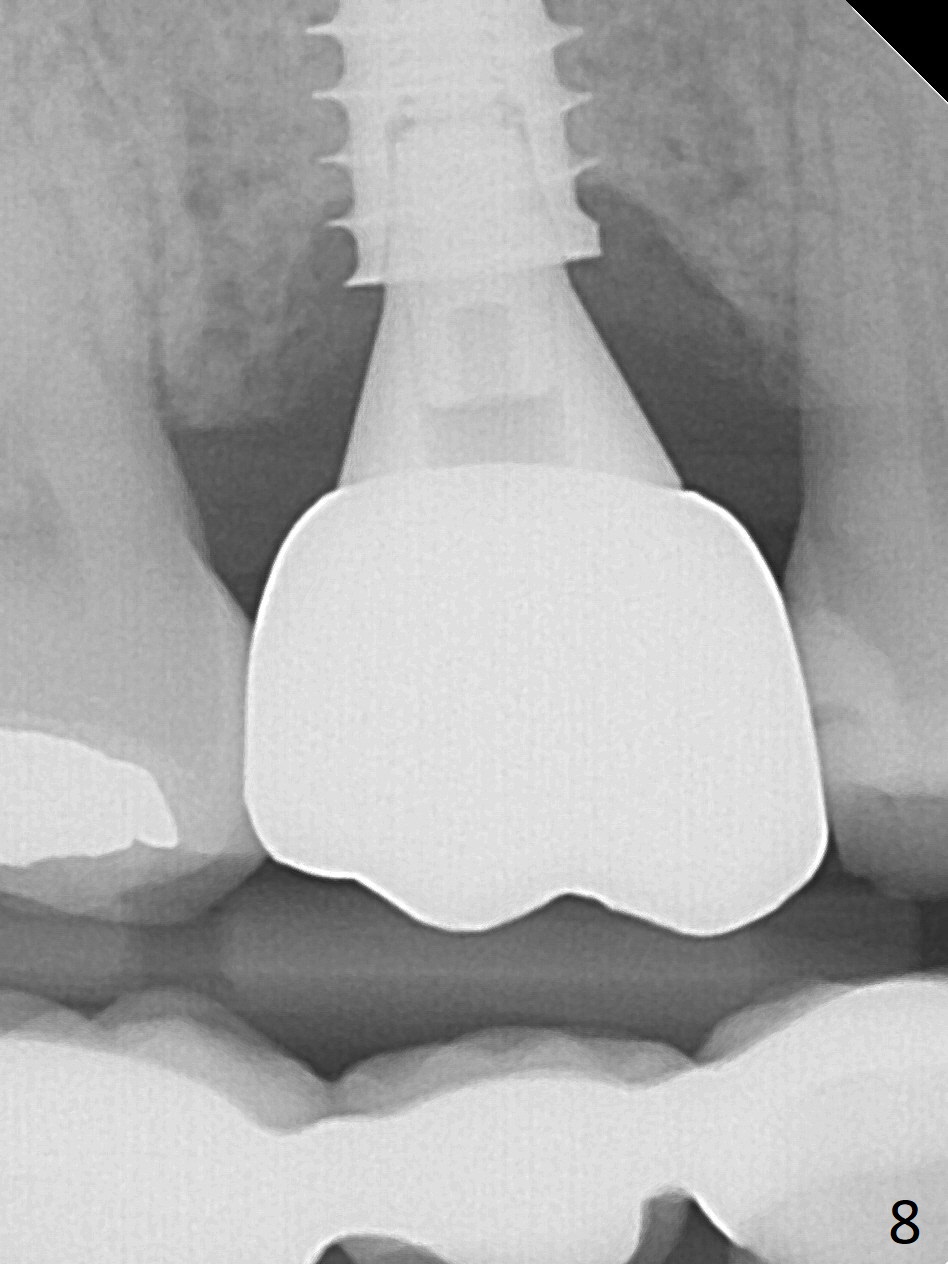
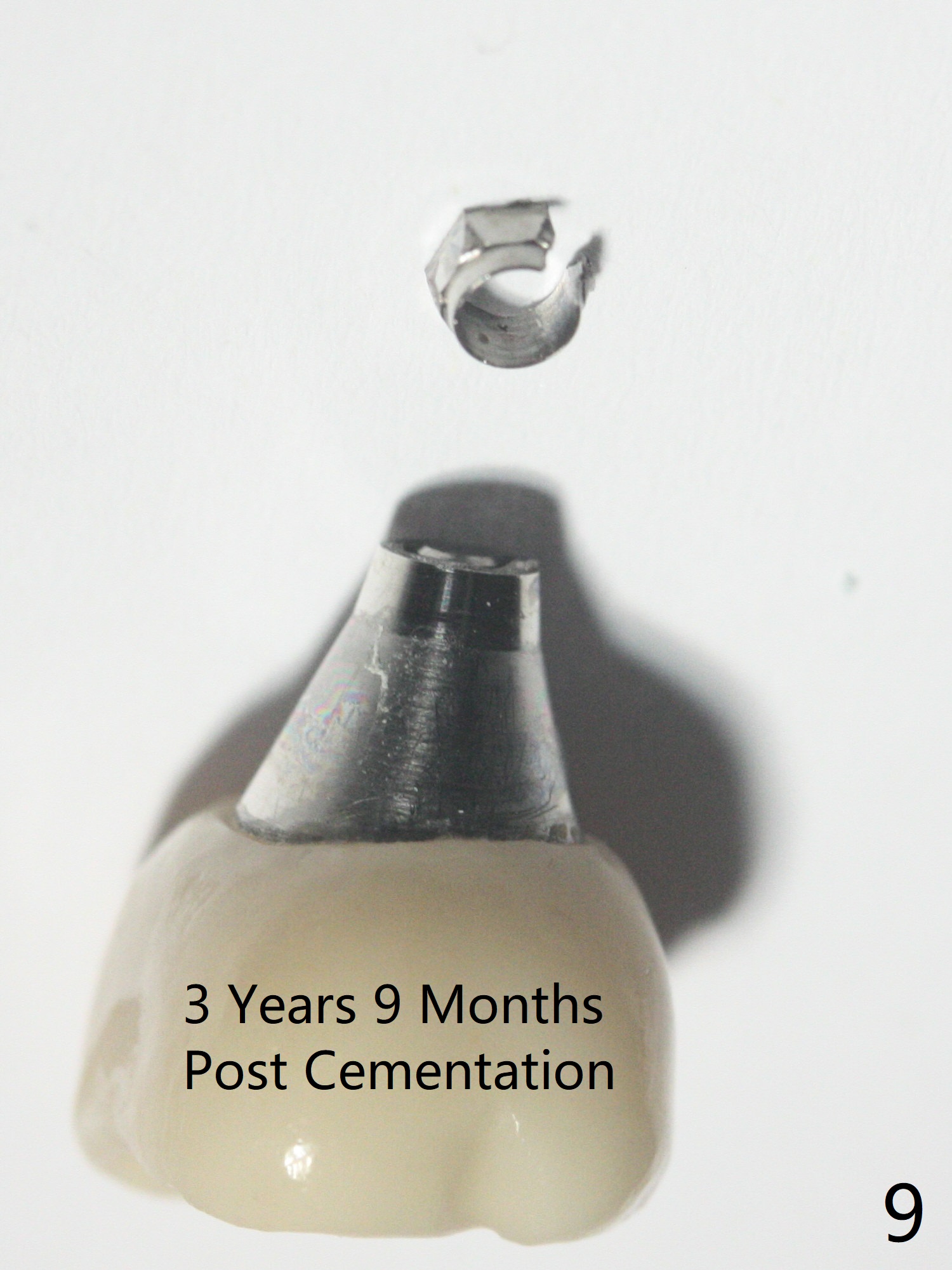
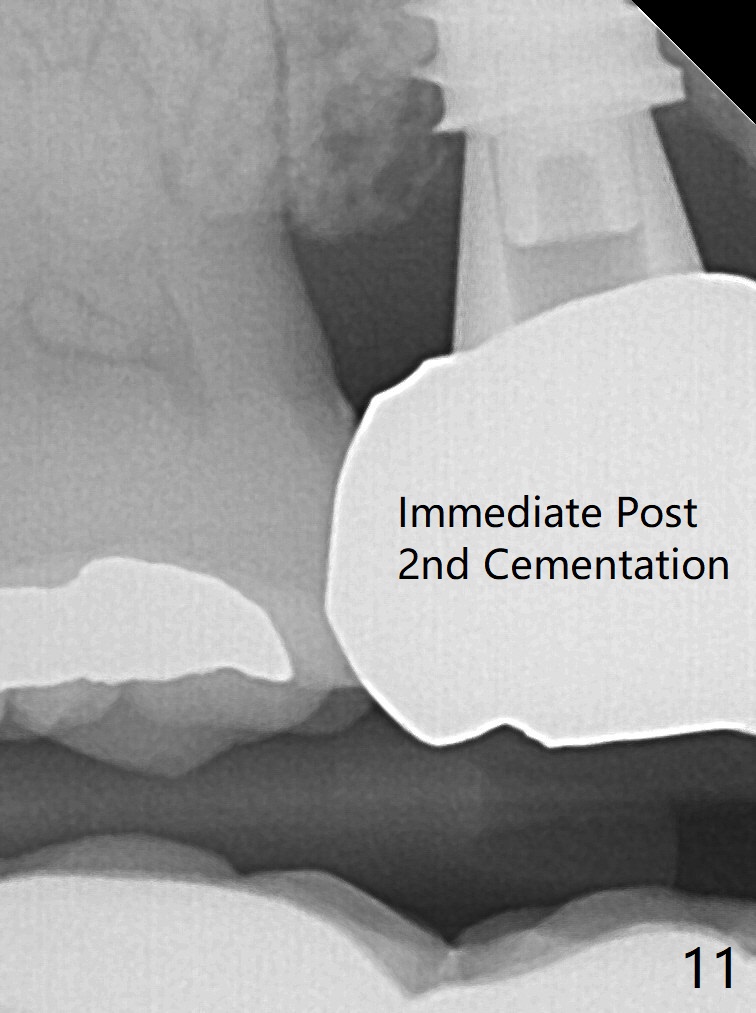
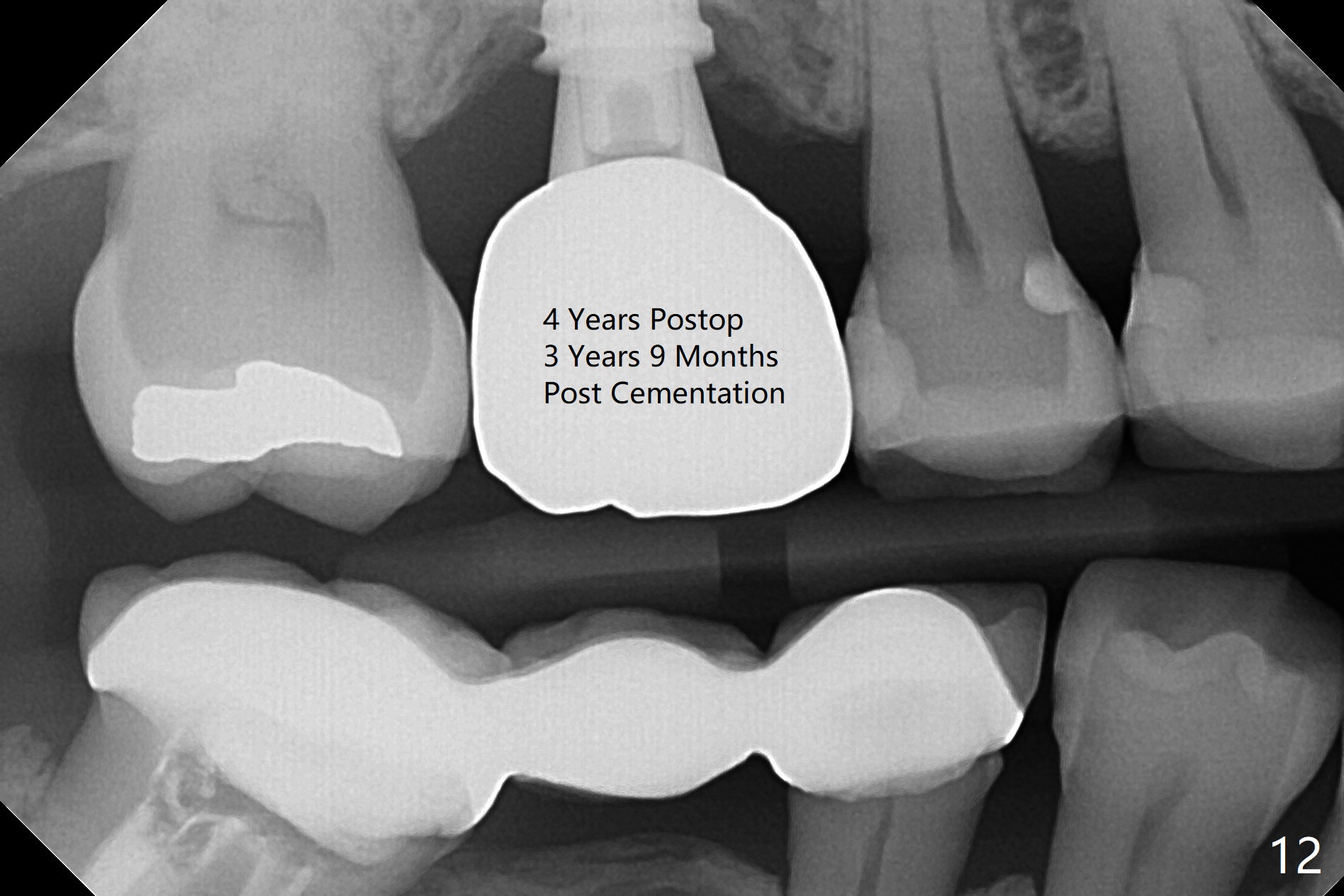
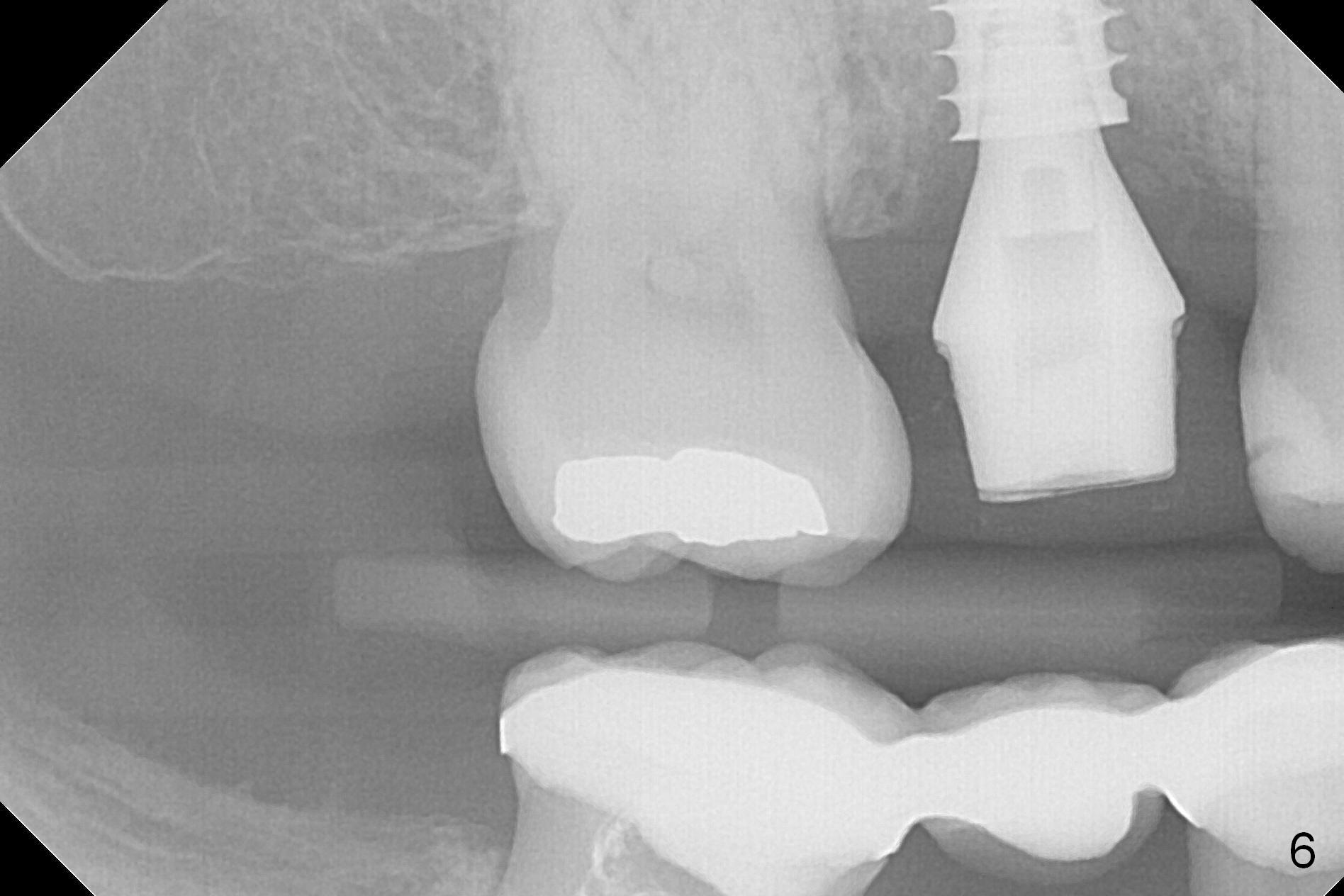
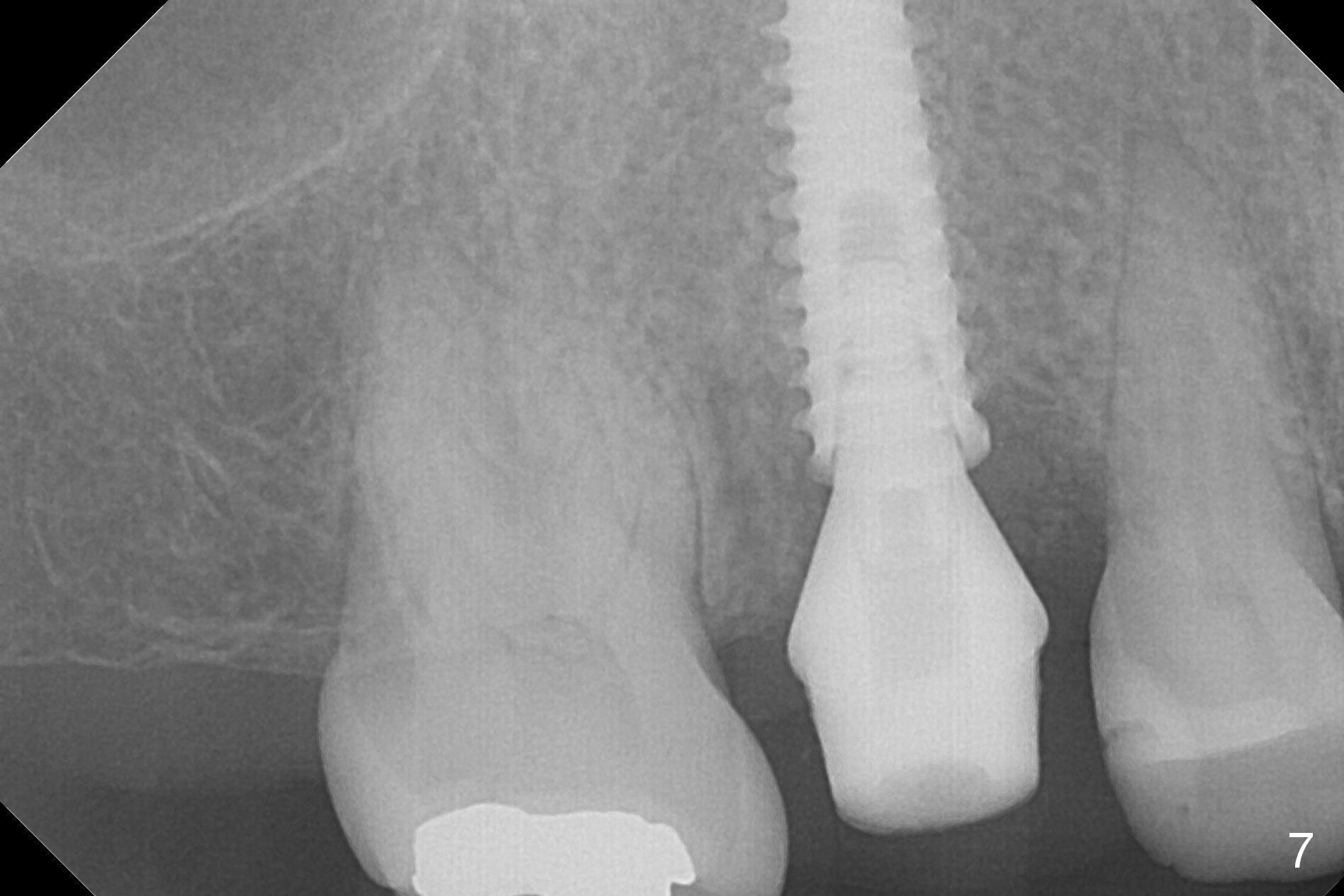
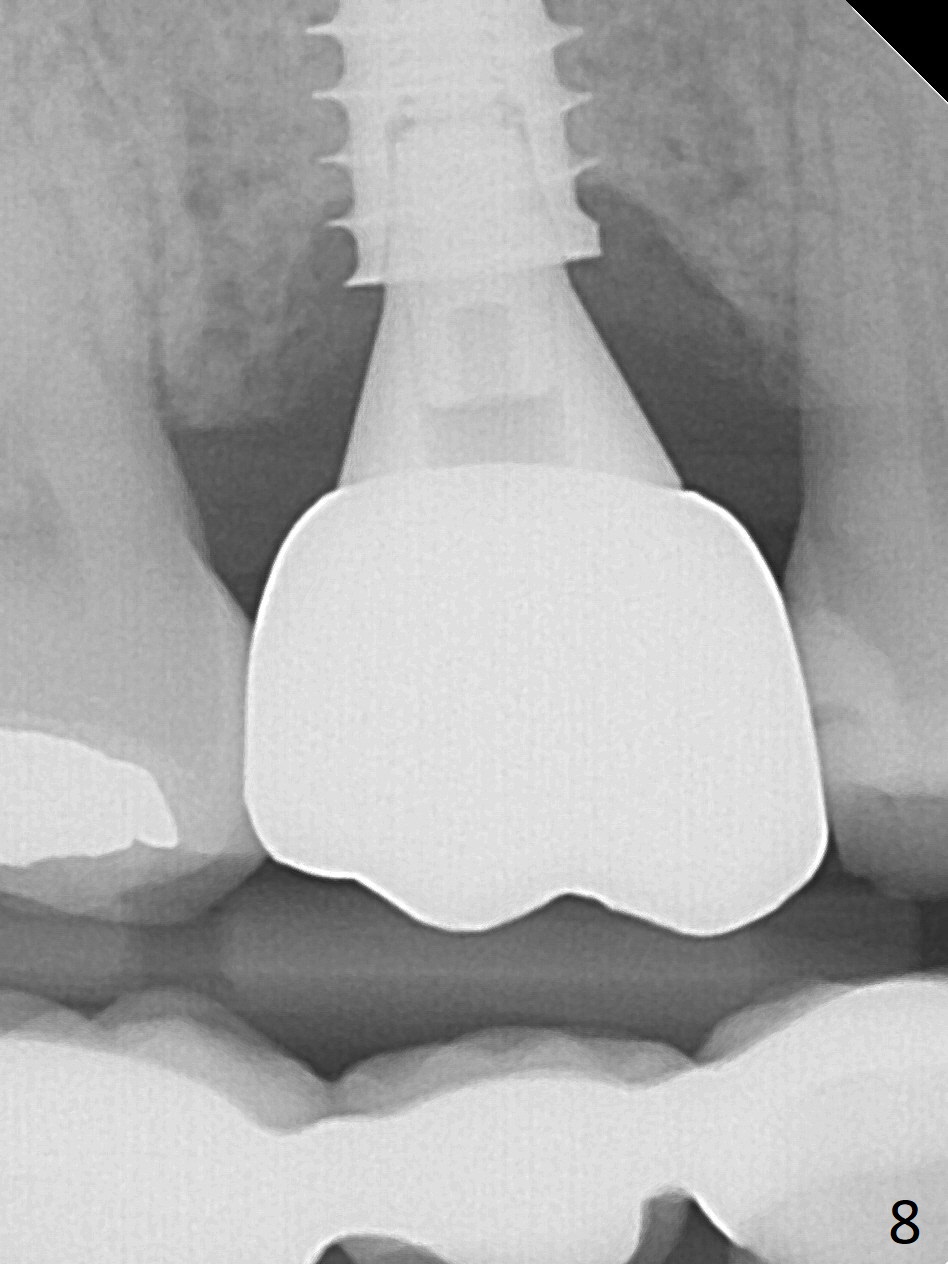
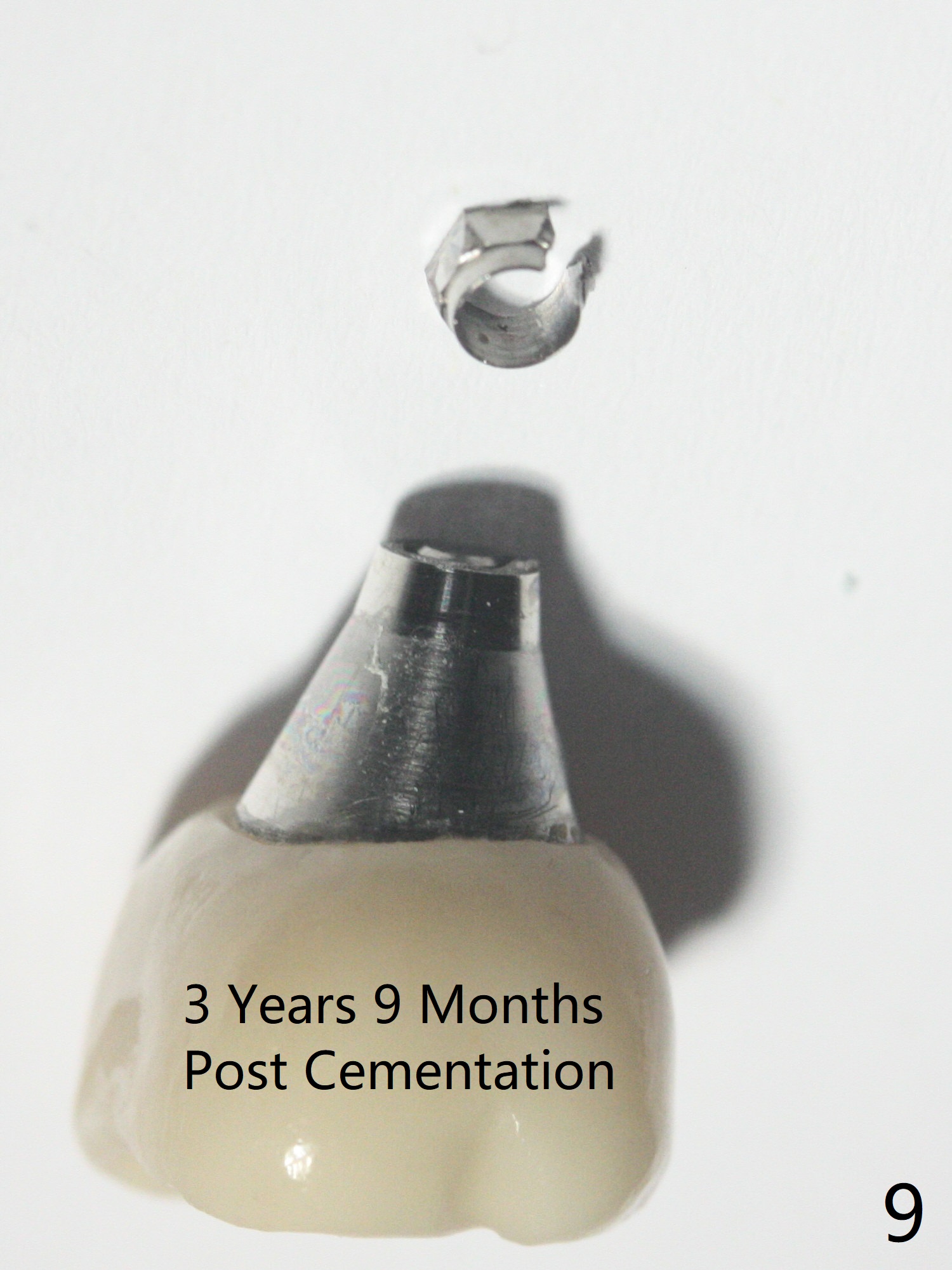
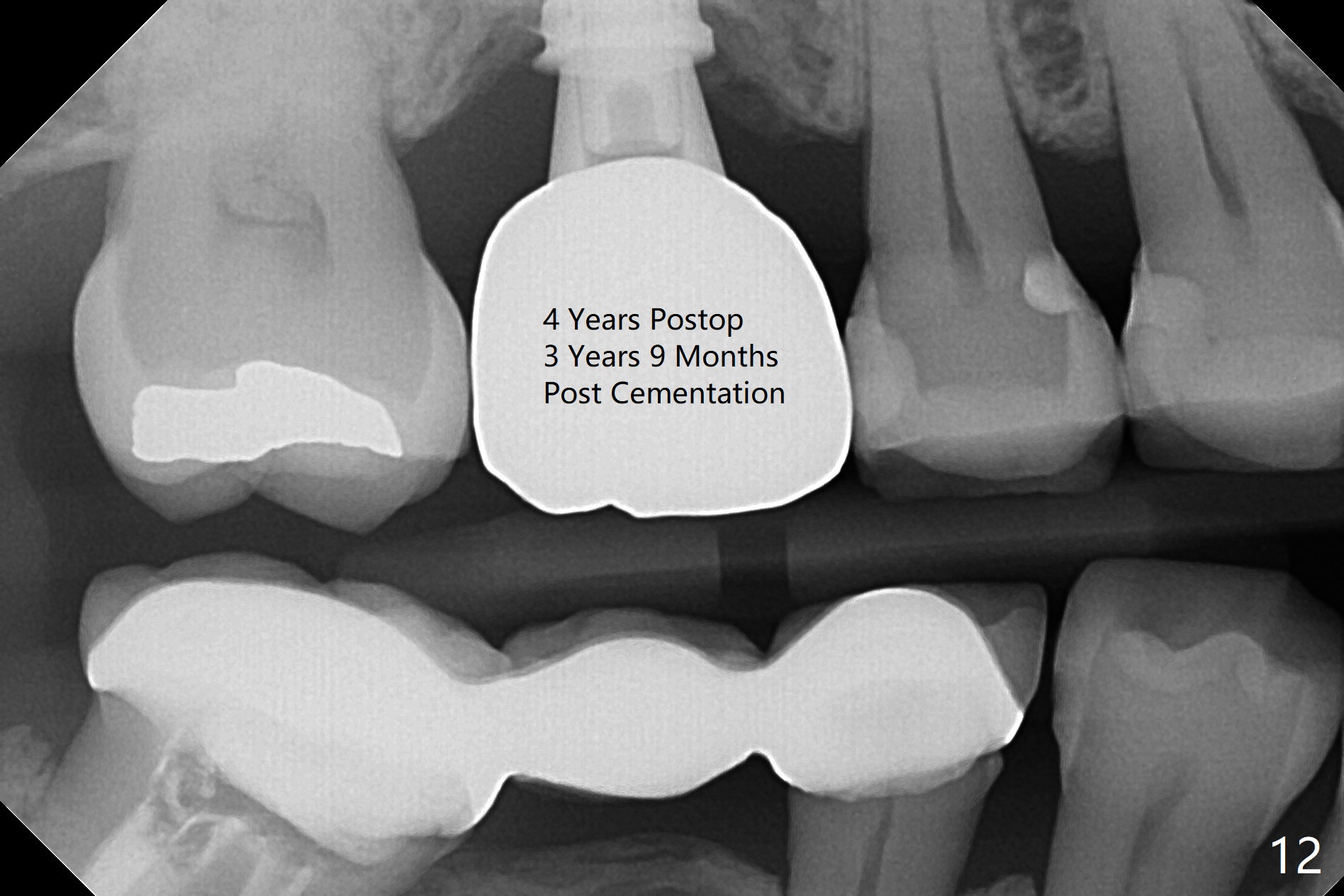
Three weeks postop, the socket has been healing with simultaneous buccal plate collapsing (Fig.5 *, as compared to Fig.2). A larger abutment (7.0-8.5 mm) or a provisional with buccal subgingival margin may decrease the postop shrinking (1,2). There is no bone loss 3 months postop (Fig.6,7). The screw needs to be retightened 9 months post cementation (Fig.8, when the tooth crown is being fabricated at #18). Unilateral mastication is a predisposing factor, since the tooth #19 is missing. When the crown becomes loose again 3 years later, the hex fractures inside the implant. After its removal (Fig.9), a narrower abutment is placed for a new crown (Fig.10: 5x4(4) vs. 6.5x4(4) mm). The implant was placed deep enough without thread exposure; now with apparently complete abutment seating (Fig.11,12). The similar complication may recur due to refusal to have implant at #19 (fear of nerve injury).
Return to Upper Molar Immediate Implant, Prevent Molar Periimplantitis (Protocols, Table) 19 Screw 螺丝松动 分类
Xin Wei, DDS, PhD, MS 1st edition 11/15/2016, last revision 03/14/2021