
.jpg)
.jpg)


.jpg)


 |
 |
 |
 |
.jpg) |
|
.jpg) |
 |
 |
.jpg) |
||
 |
 |
||||
Immediate Provisional Stabilizes Implant
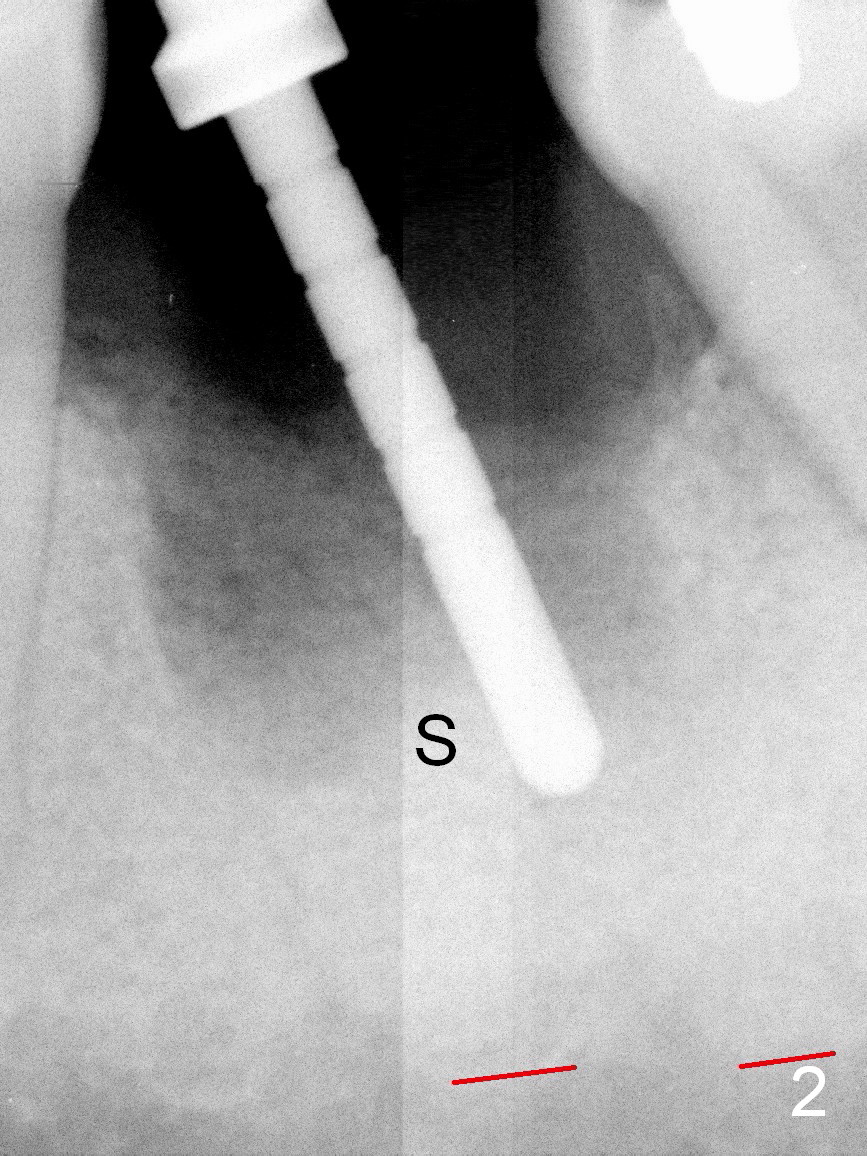
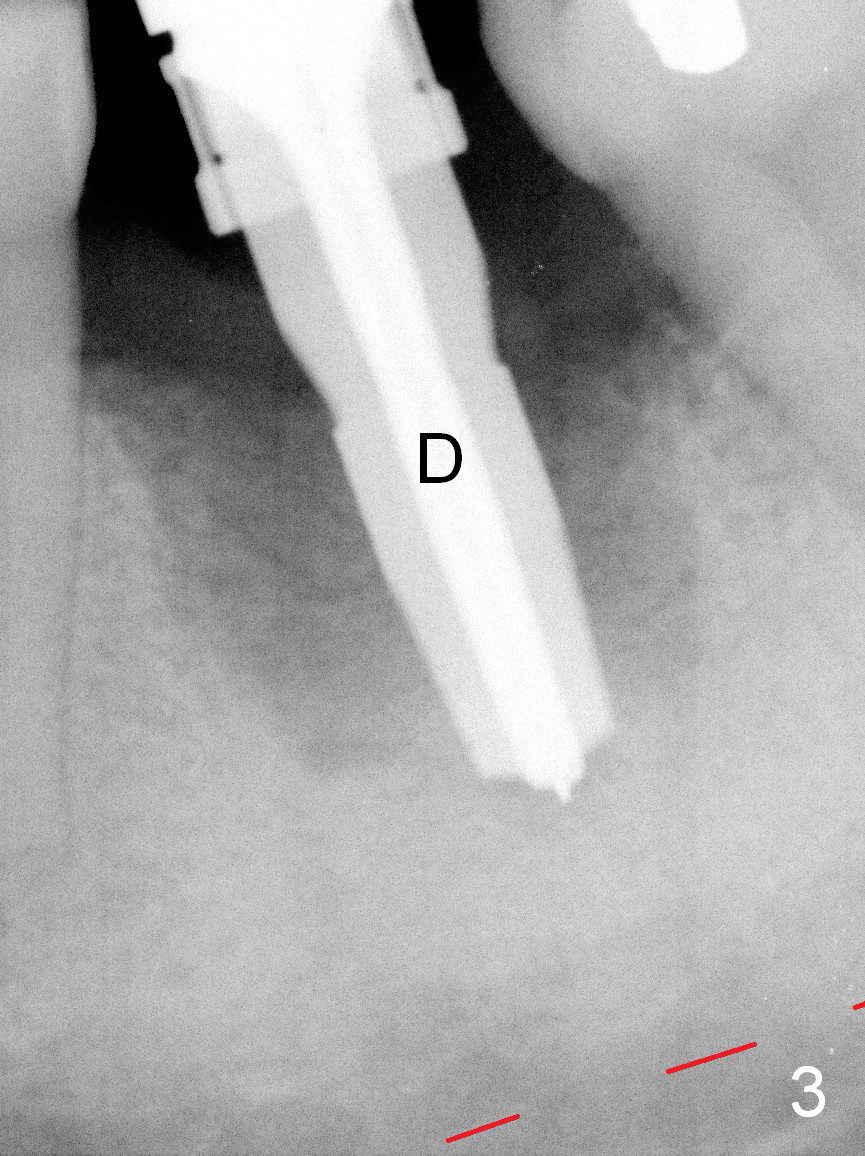
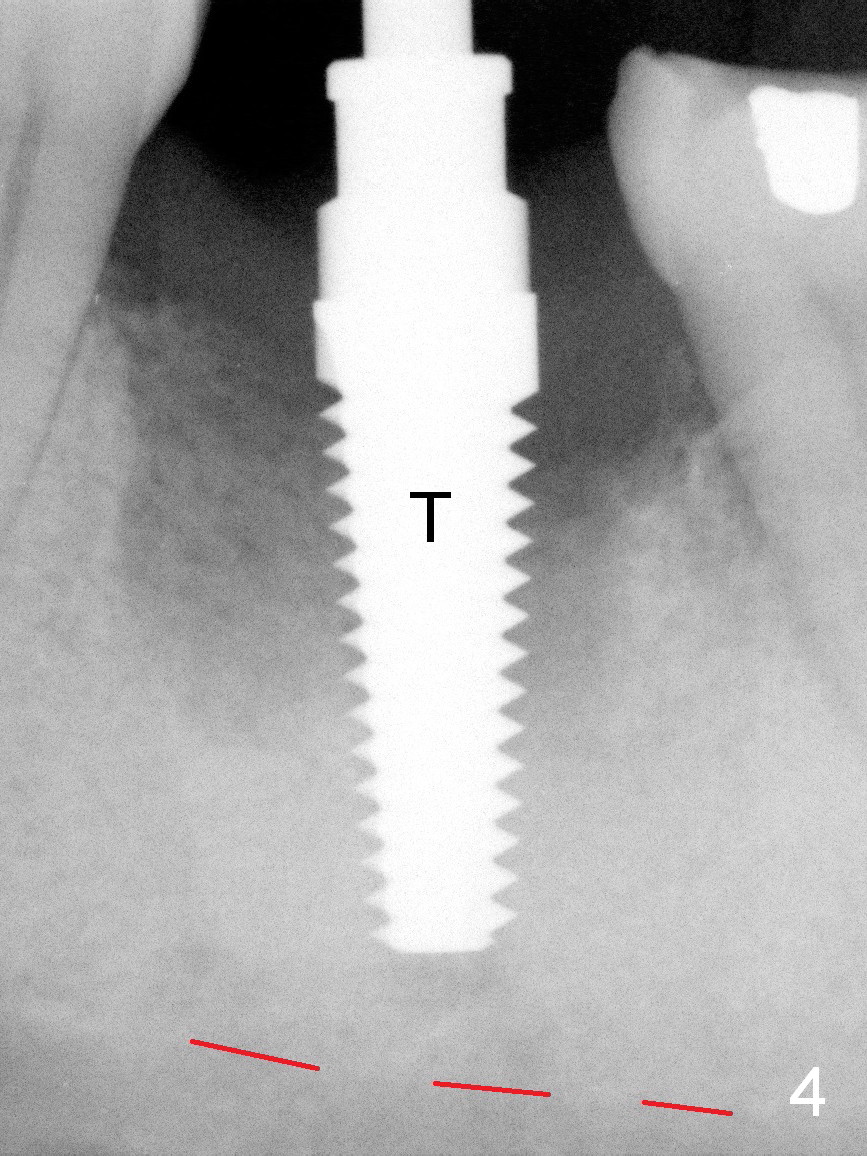
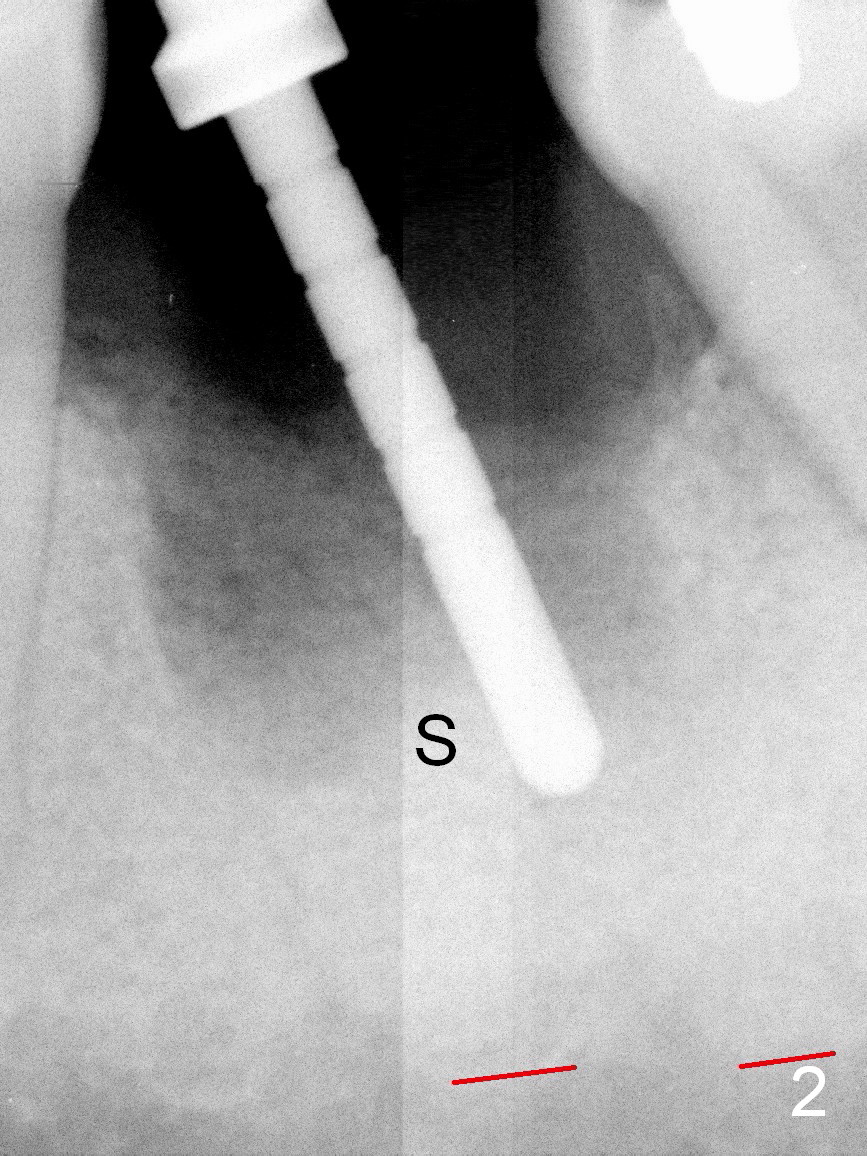
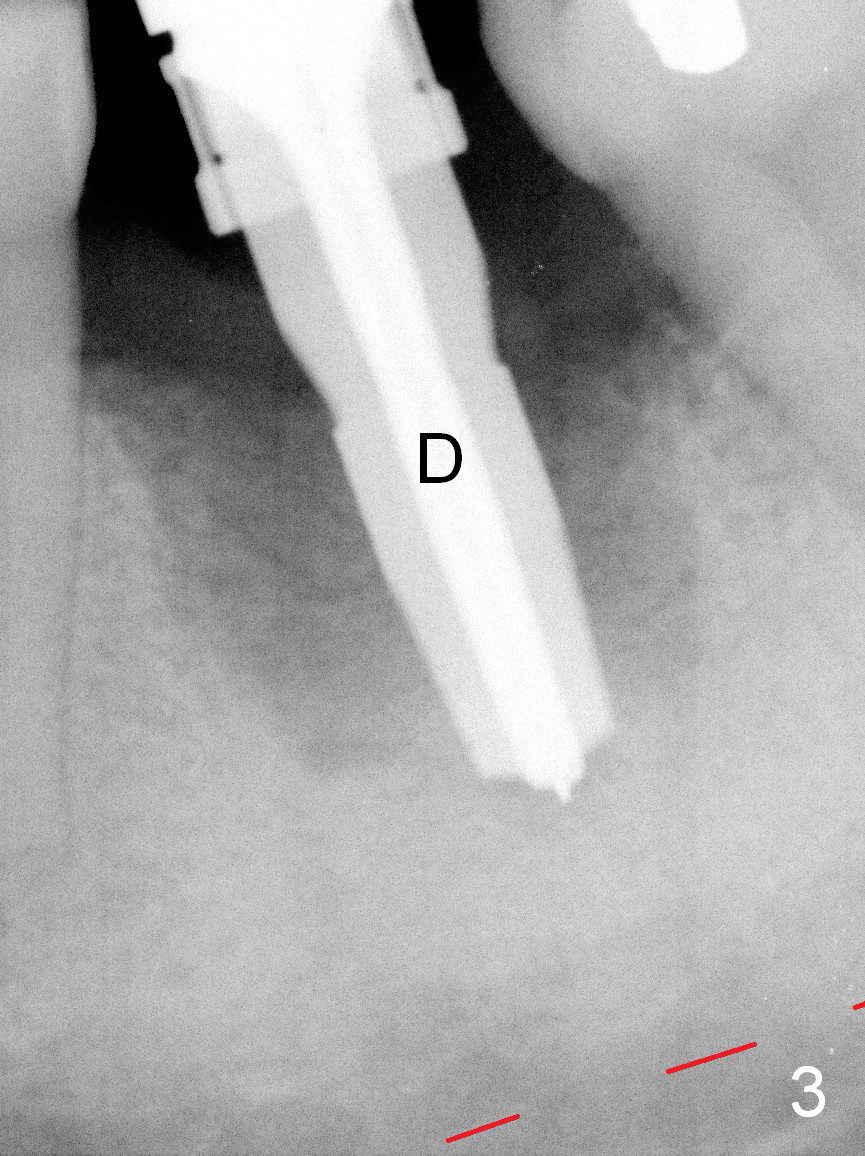
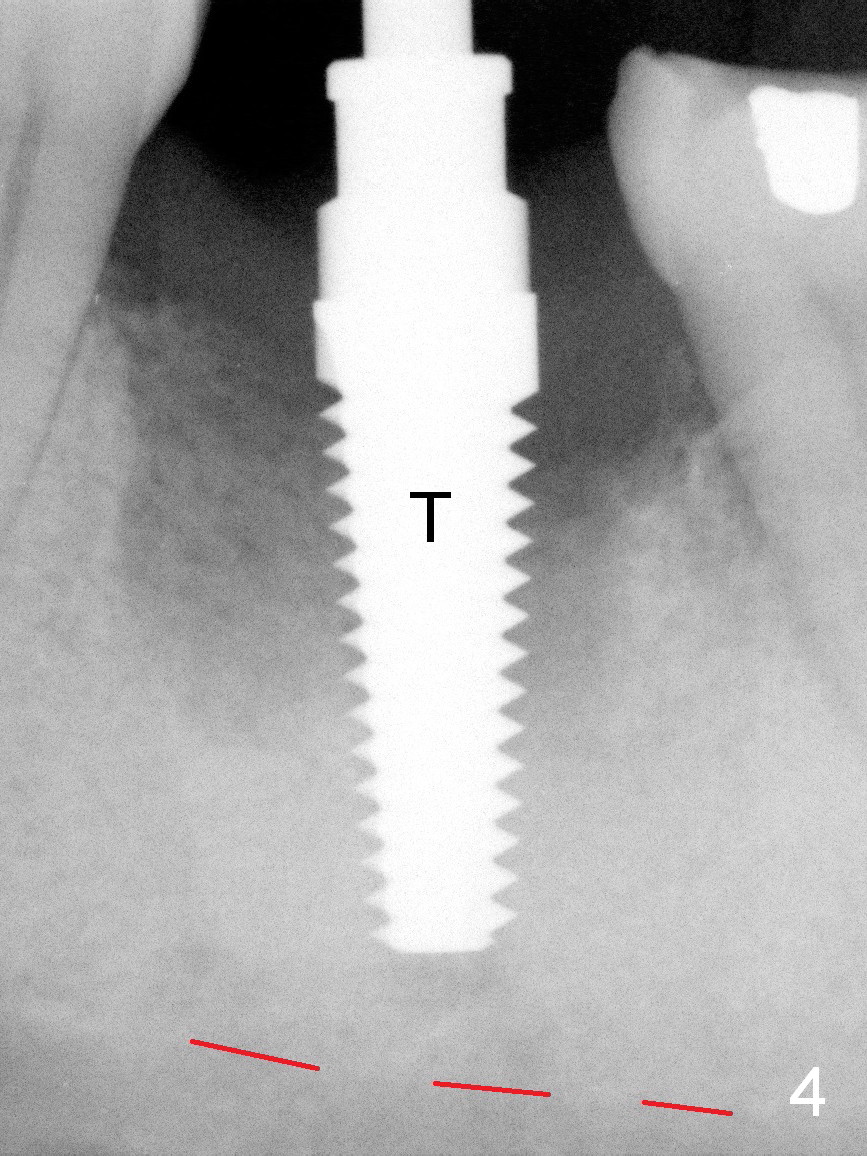
A 37-year-old lady (MP) presents to clinic with chief complaint of bad smell from lower right crown (Fig.1: #19; red dashed line: superior border of the Inferior Alveolar Canal). One of the most prominent pathologies is fracture of the distal root (<). After extraction, the socket is treated with 2% Xylocaine/1:50,000 Epinephrine. The coronal distobuccal plate is defective. Osteotomy is initiated as lingual as possible. The 1st intraop PA shows that the osteotomy is shallow and distal to the almost non-existent septum (Fig.2 S). The osteotomy is intended to move more mesially, but the result is not obvious when 4.5x14 mm drill is in place (Fig.3 D). The depth of the osteotomy is increased by 3 mm; a 5x17 mm tap is stable (Fig.4 T). A 5x12 mm implant (Fig.5 I) is placed until it cannot be turned. The implant is higher than the distal crest (^). In addition there is space apical to the implant (Fig.5*). After 5 mm drill is used, the implant is seated deeper with insertion torque < 35 Ncm (Fig.6). It suggests overprep. Anyway, an immediate provisional is fabricated after placement of an abutment (A). After reline, the provisional fits well. It has to be removed with forceps for occlusal adjustment. Finally the abutment/implant complex turns in the socket with fingers. The rotation/position of the complex is randomly adjusted. When the provisional is cemented, it does not seat completely, but is stable. If the implant osteointegrates, the provisional must play a role in stabilizing the implant. Bone graft is placed in the gap prior to cementation (Fig.6 *).
The out-of-state patient requests pain med 3 days postop. It would be the best to uncover the implant or place a healing abutment when the implant was found to be unstable.
When the patient returns 1.5 months postop, the provisional has been fractured (Fig.8 lingual view). The abutment is loose. Intraop analysis of a PA shows existence of the peri-implant defect (Fig.7). When the abutment is removed, the implant is found to be stable. As a new smaller abutment (Fig.9: 6.8x4(3) mm) is being torqued at 35 Ncm, the abutment/implant does not turn. Impression for final restoration is taken. Postop analysis of PAs in Fig.6,7 shows that the peri-implant defect has been reduced in 1.5 months. Immediately postop, the fourth coronal large thread is buried in the solid bone, whereas 1.5 months postop the third thread appears inside the base bone.
It appears that the loss of the provisional in this case is due to untightening the abutment. The most secure method to fix the abutment/implant in place is to apply setting acrylic to the undercut without taking it out immediately. This is called provisional without cement (1 2 3 4 5). Bone density increases in the peri-implant space 16 months post cementation (Fig.10) and continues to increase 2 years 8 months post cementation (Fig.11).
Return to
Lower Molar Immediate Implant,
Posterior Immediate Provisional,
#30
Xin Wei, DDS, PhD, MS 1st edition 11/30/2015, last revision 11/09/2018