
 |
 |
 |
  |
 |
 |
Periapical Radiopaque Lesion as Related Implant Placement
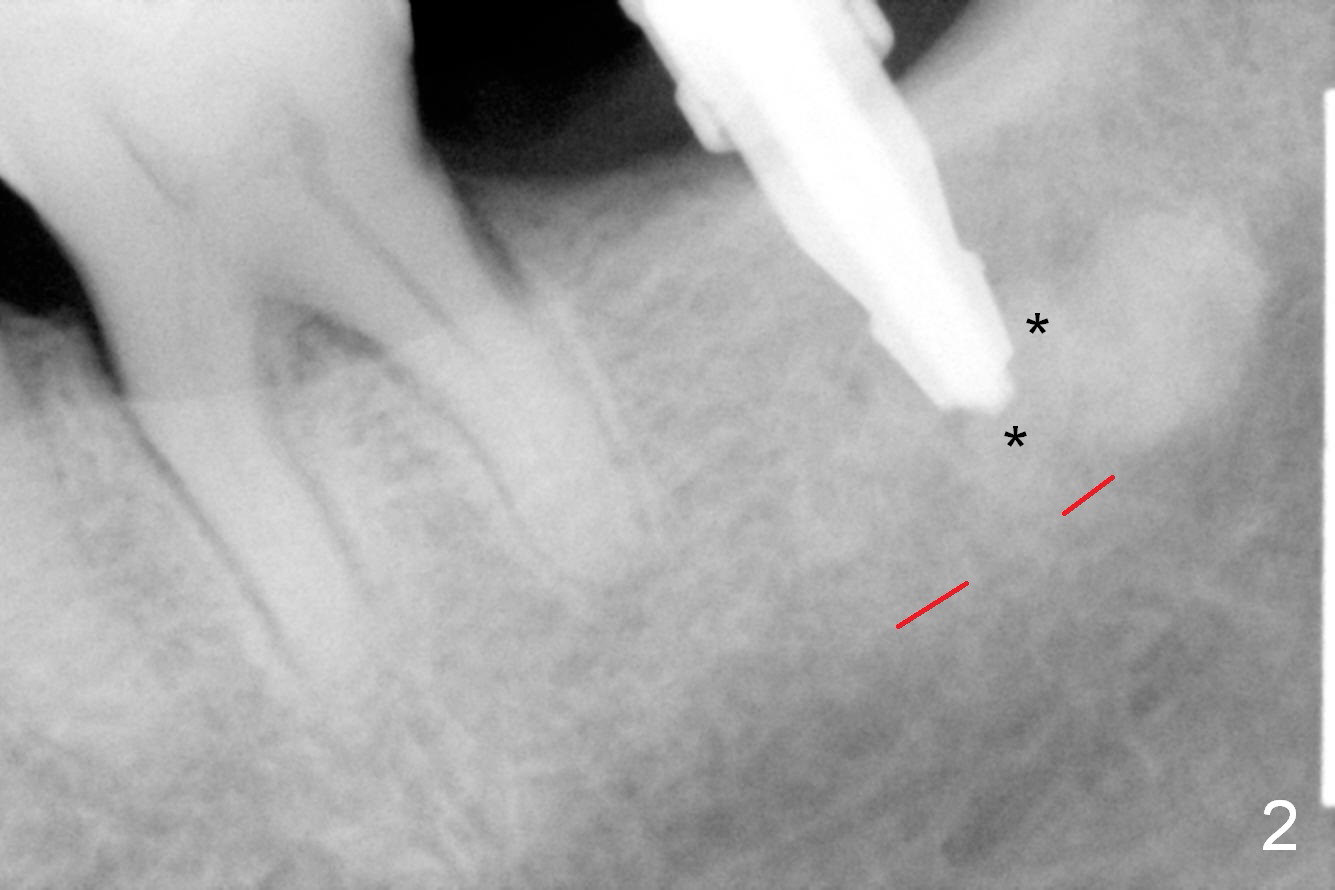
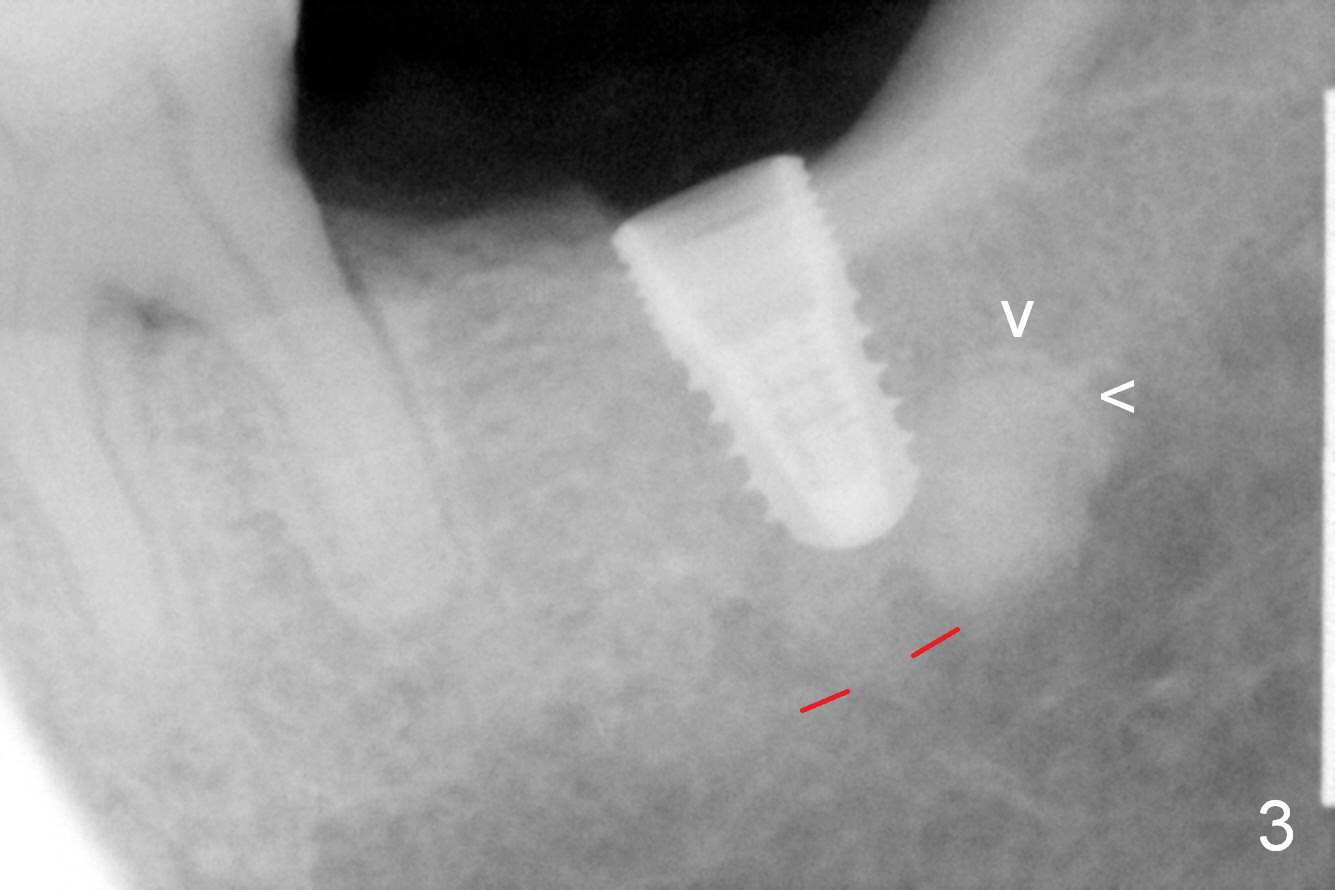
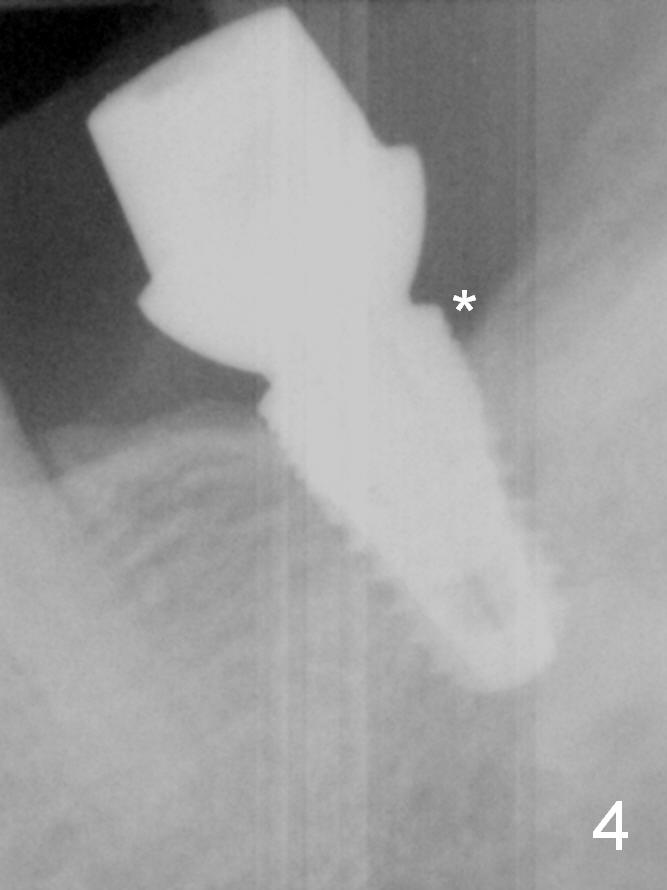
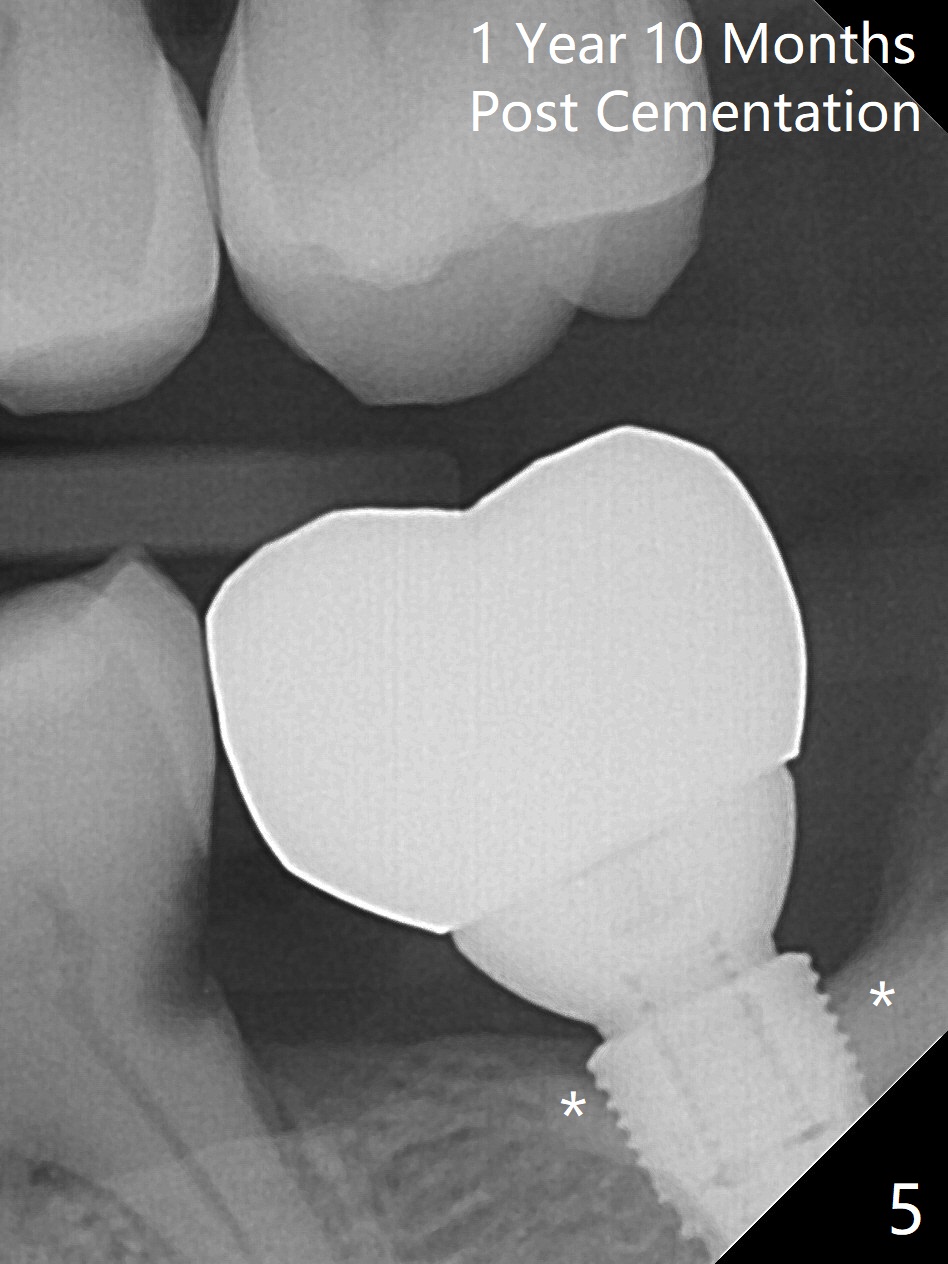
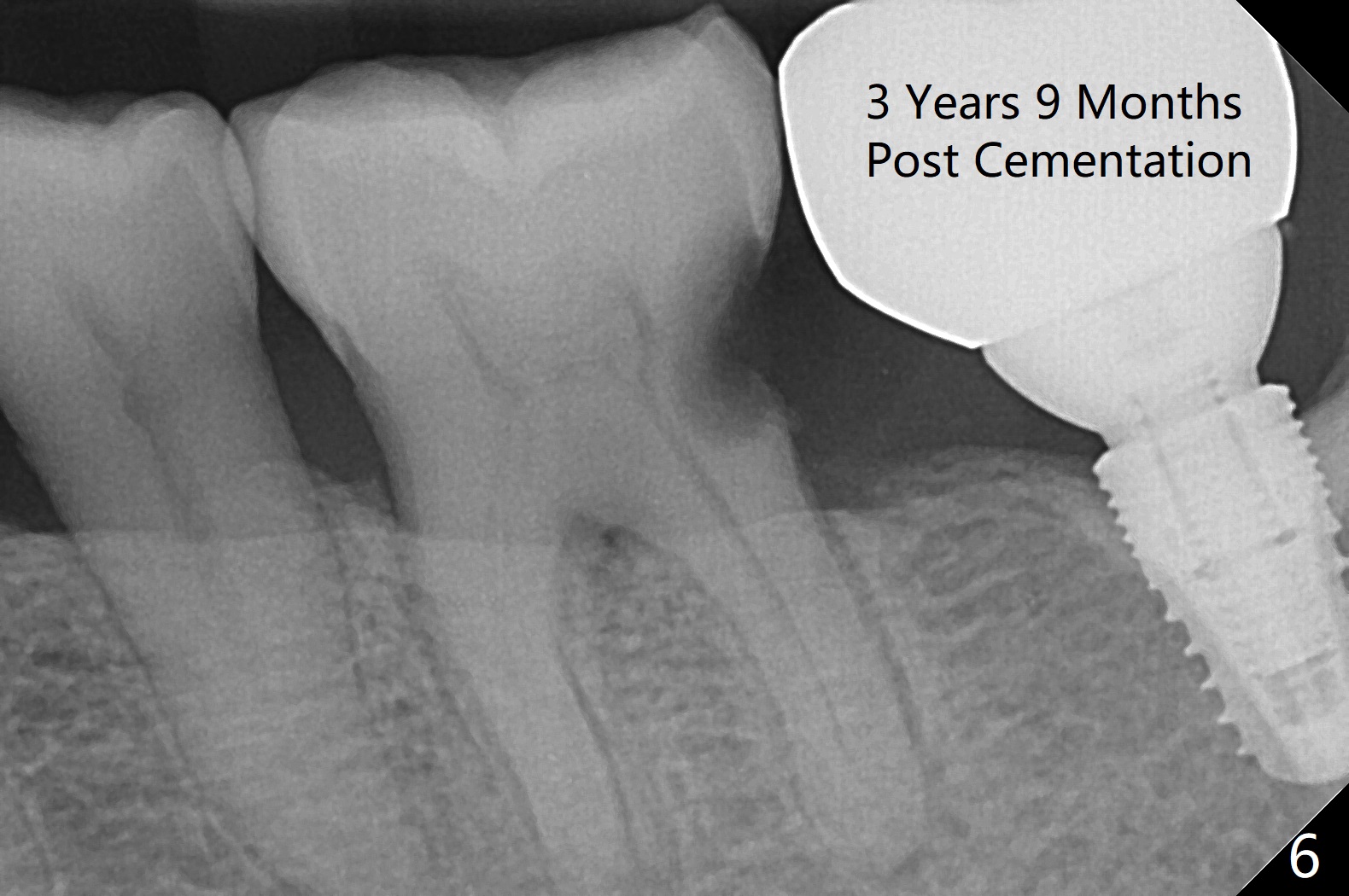
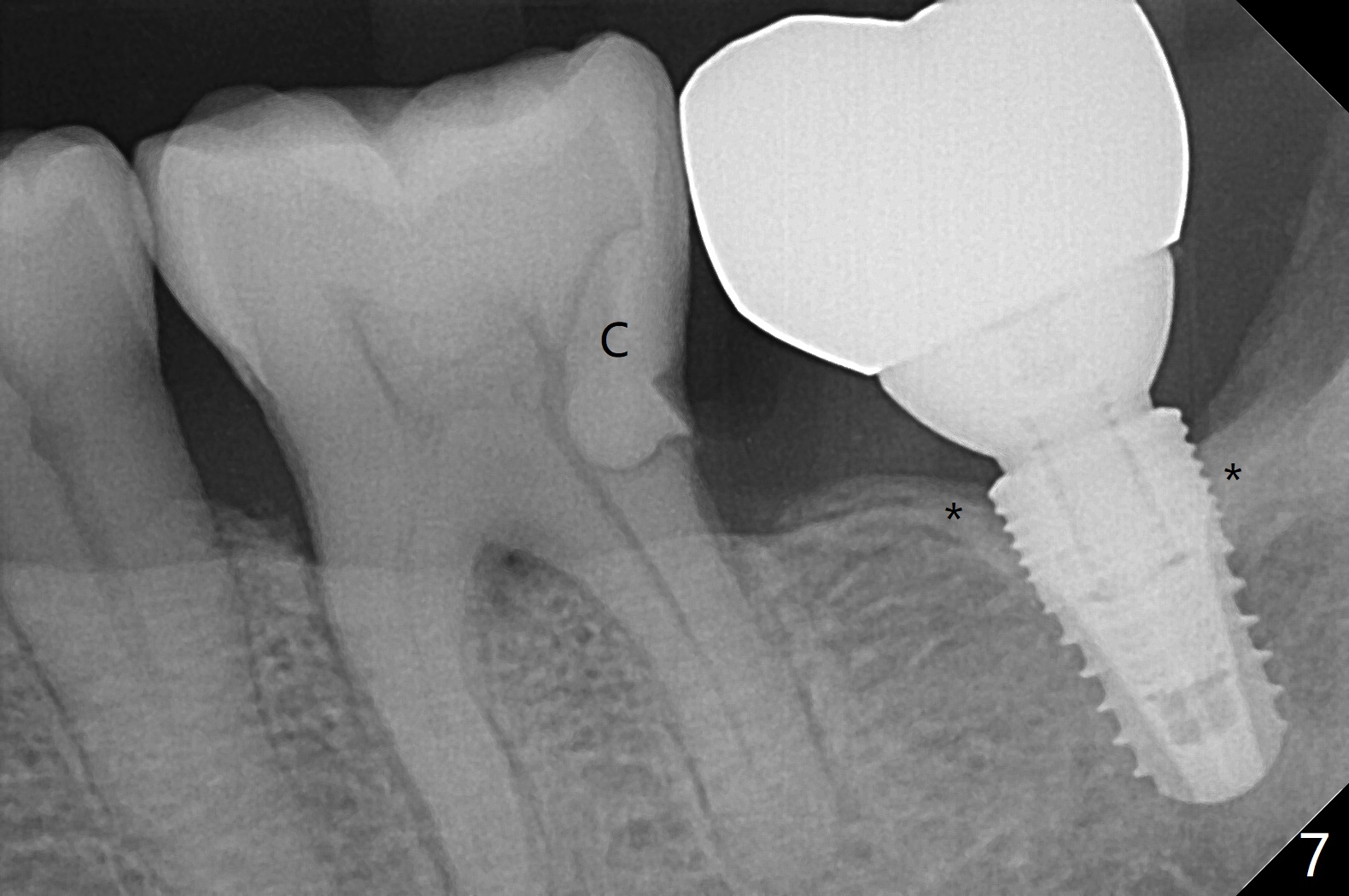
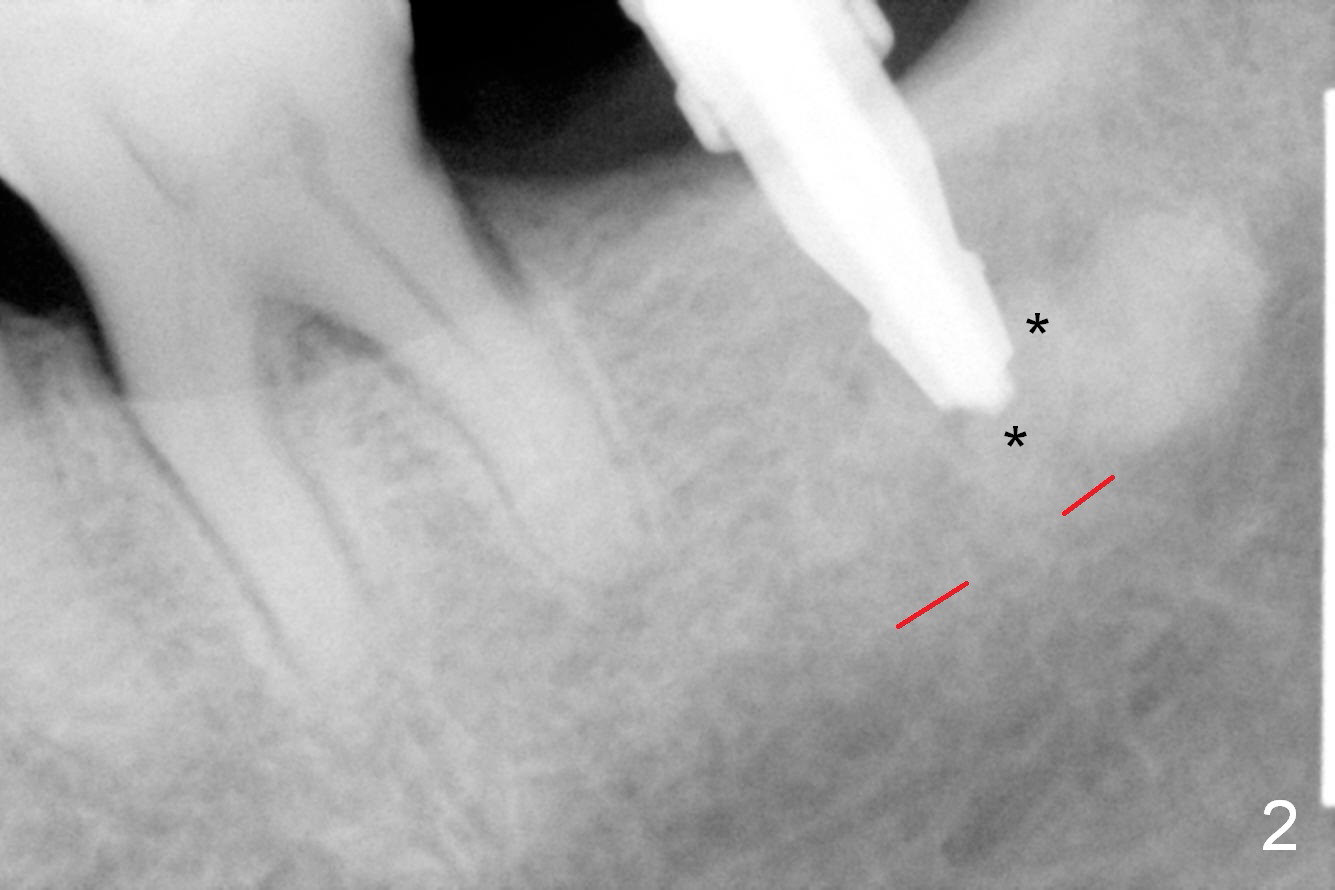
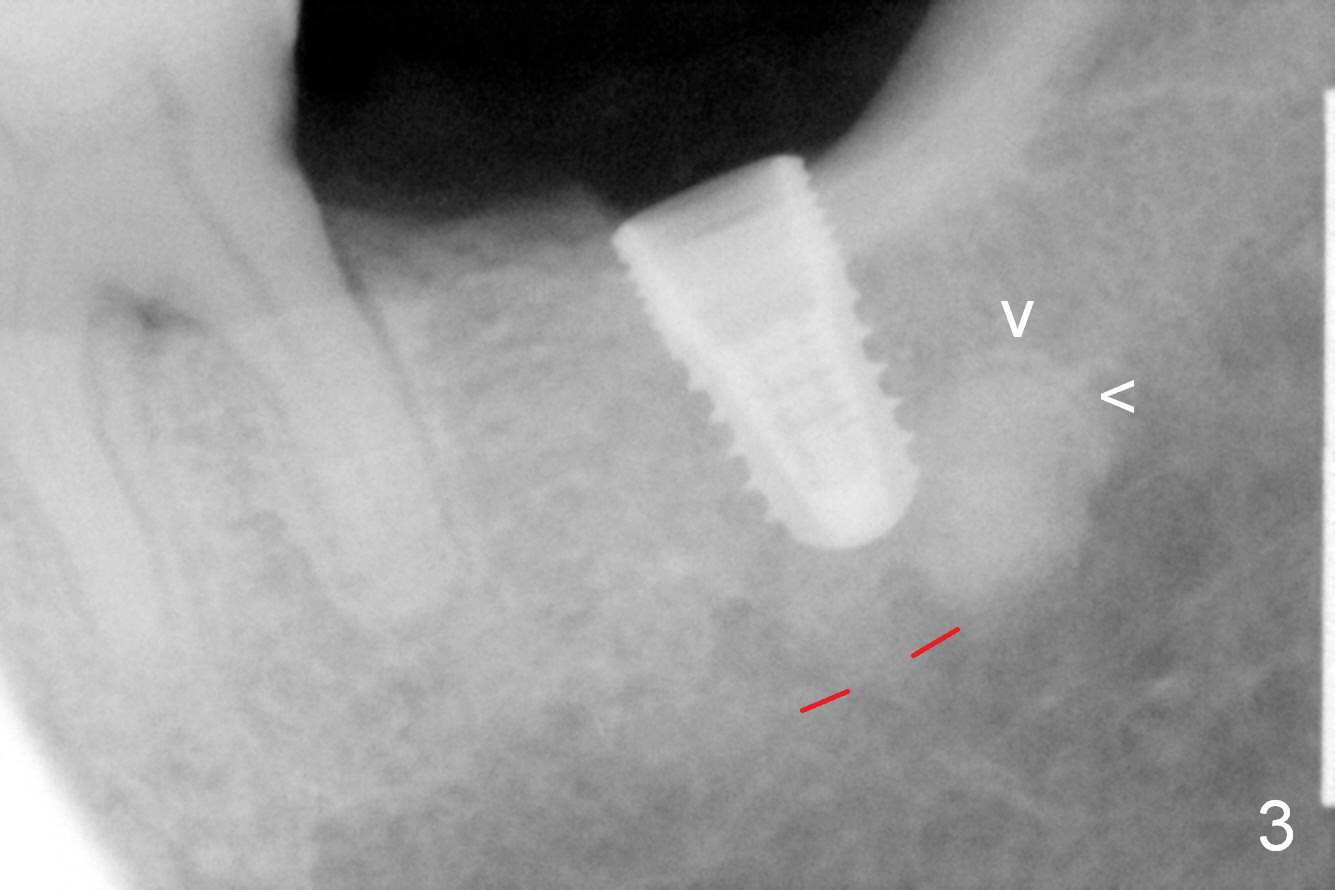
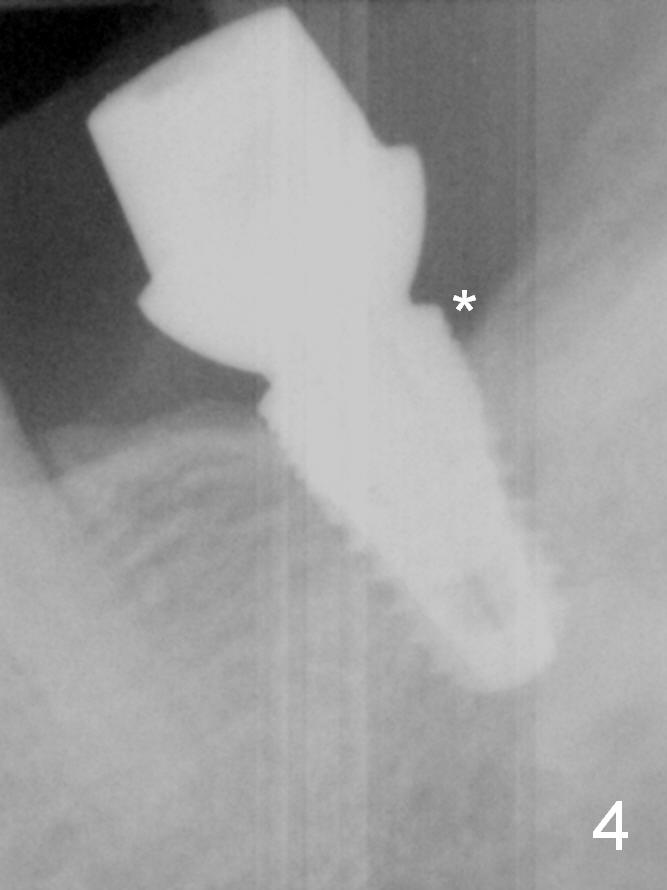
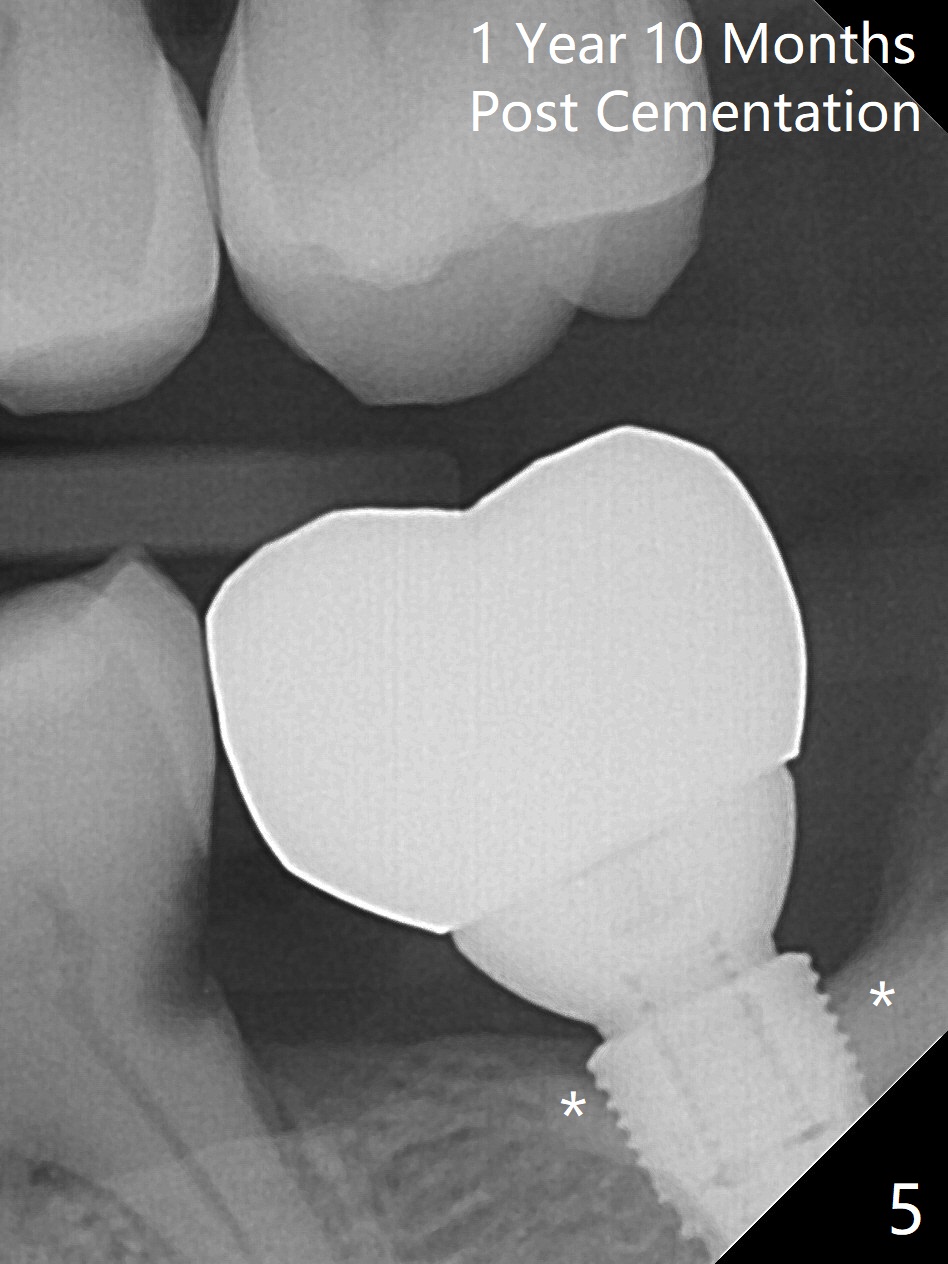
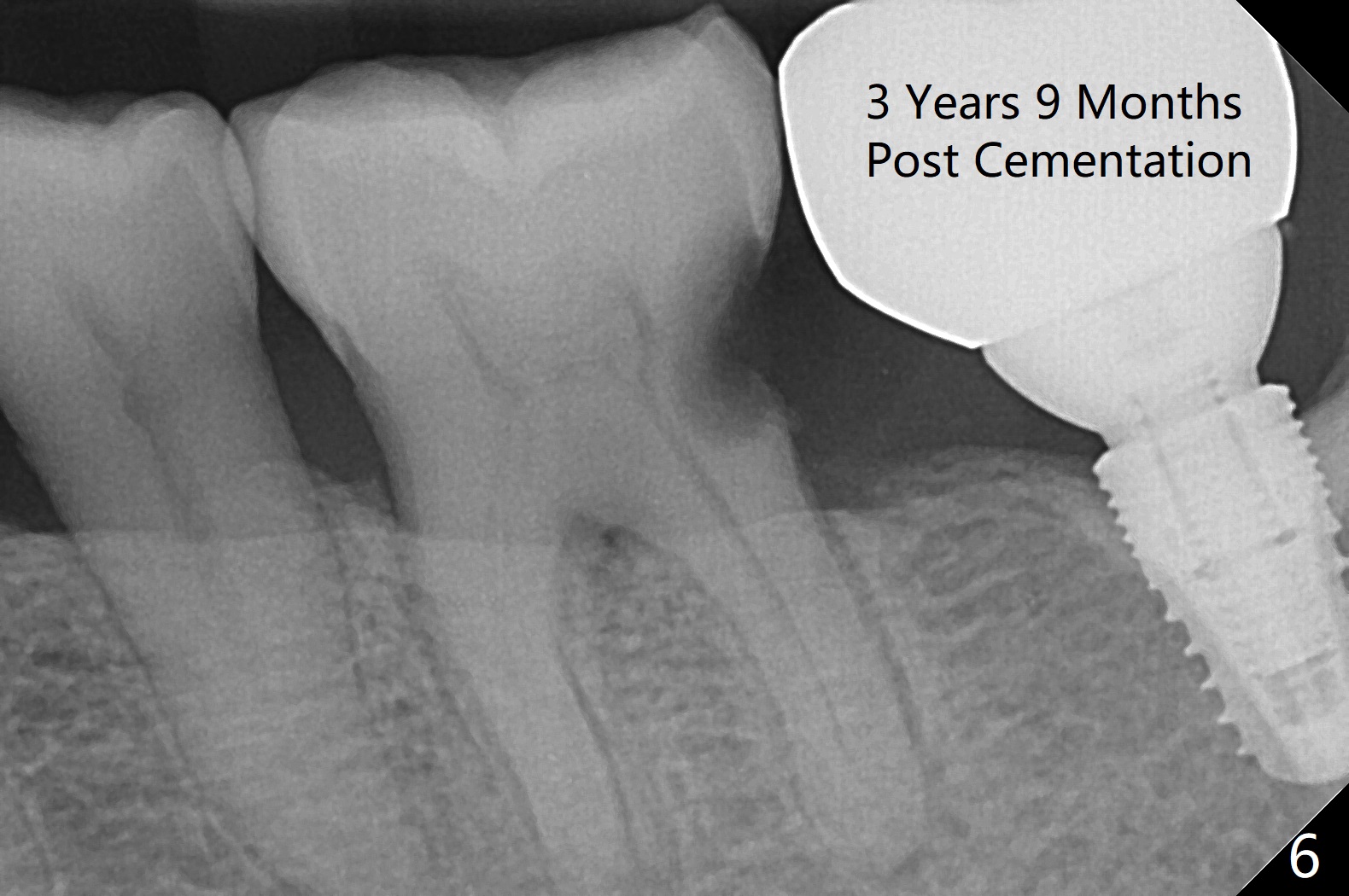
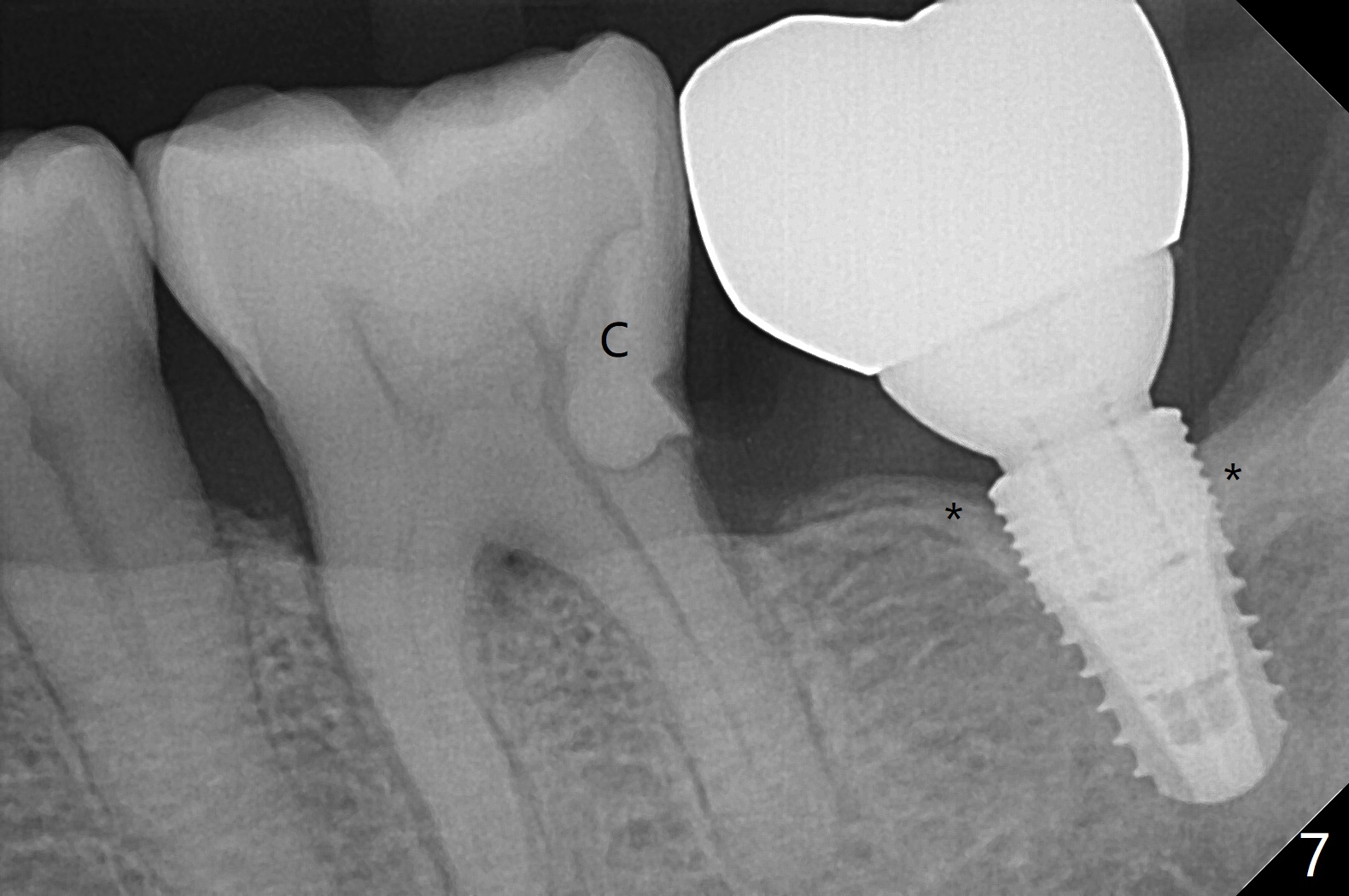
After establishing proper depth of osteotomy in the relatively narrow ridge at #18 (Fig.1 (red dashed line: the superior border of the Inferior Alveolar Canal)), the patient feels pain when the osteotomy is enlarged (Fig.2 with 4.5x8 mm drill in place) in spite of repeated local infiltration. The tooth was extracted 7-8 years ago. It appears that the pain is due to the fact that the osteotomy approaches part of the former periapical radiopaque lesion (Fig.2 *). Intrabony injection (into the osteotomy) alleviates the pain and allows placement of a 4.5x8 mm implant (Fig.3). It seems that the lesion is benign since it has a distinct border (Fig.3 arrowheads). There seems to be mild bone loss distally 7 months postop (Fig.4 *). Dense bone seems to be attached to the coronal threads of the implant 1 year 10 months post cementation (Fig.5). The sensitivity is worse when conservatively buccally approached composite dislodges 2 years later (Fig.6). RCT is imminent. When the patient returns for RCT 19 days later, the affected tooth has no percussion with endo ice response similar to #30. With the crown and abutment of #18 being removed, composite is placed distal at #18 (Fig.7 *). With local anesthesia, there is light pain during excavation with a visible canal (no hemorrhage). Return to Lower Molar Immediate Implant Trajectory II Xin Wei, DDS, PhD, MS 1st edition 01/28/2016, last revision 06/25/2020