
 |
 |
 |
  |
||
 |
 |
  |
|||
 |
 |
 |
 |
 |
 |
 |
 |
||||
Mesial Socket Placement
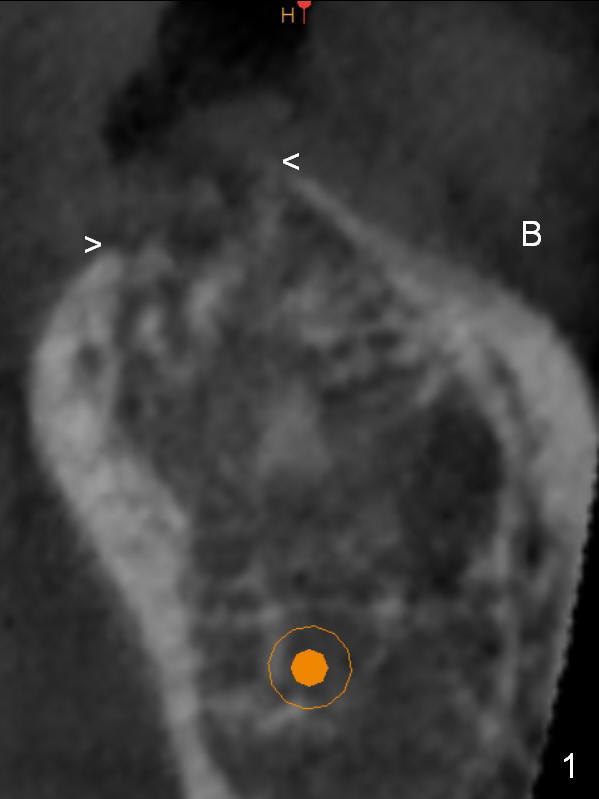
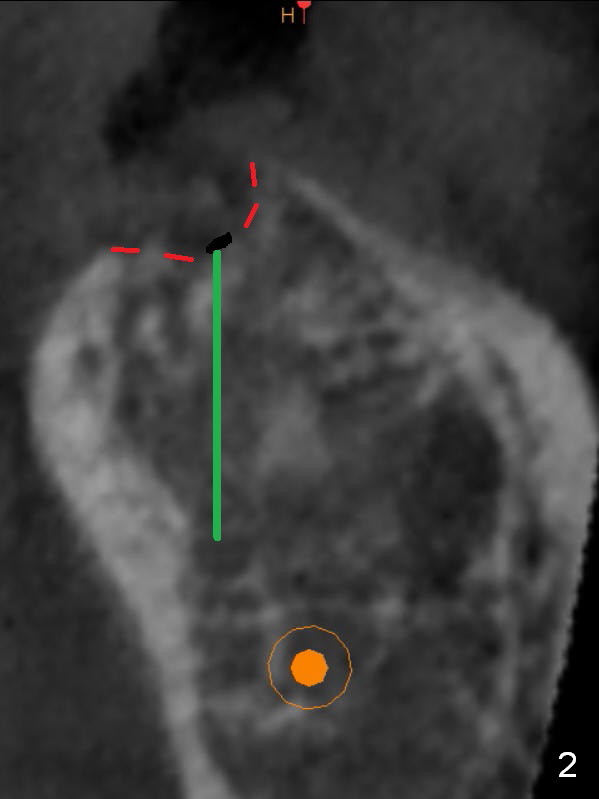
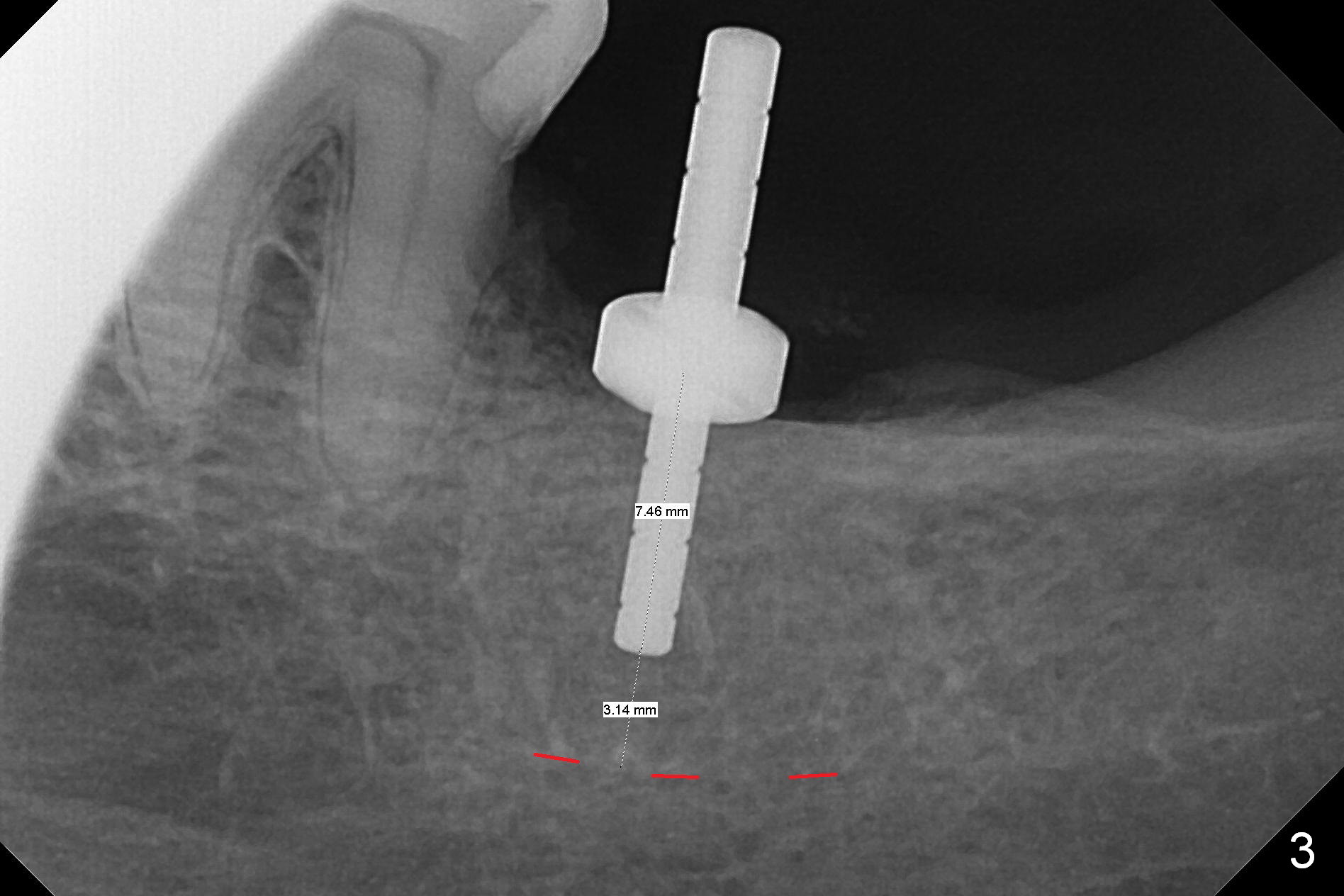
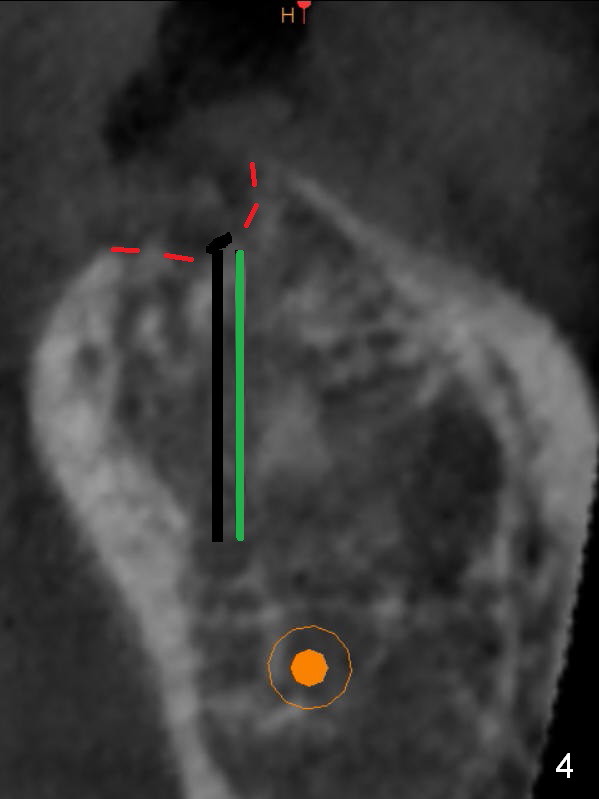
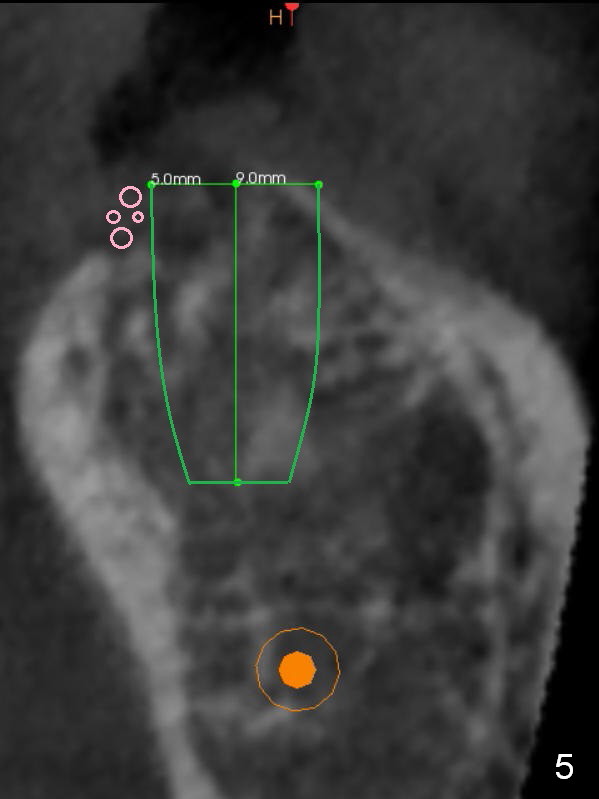
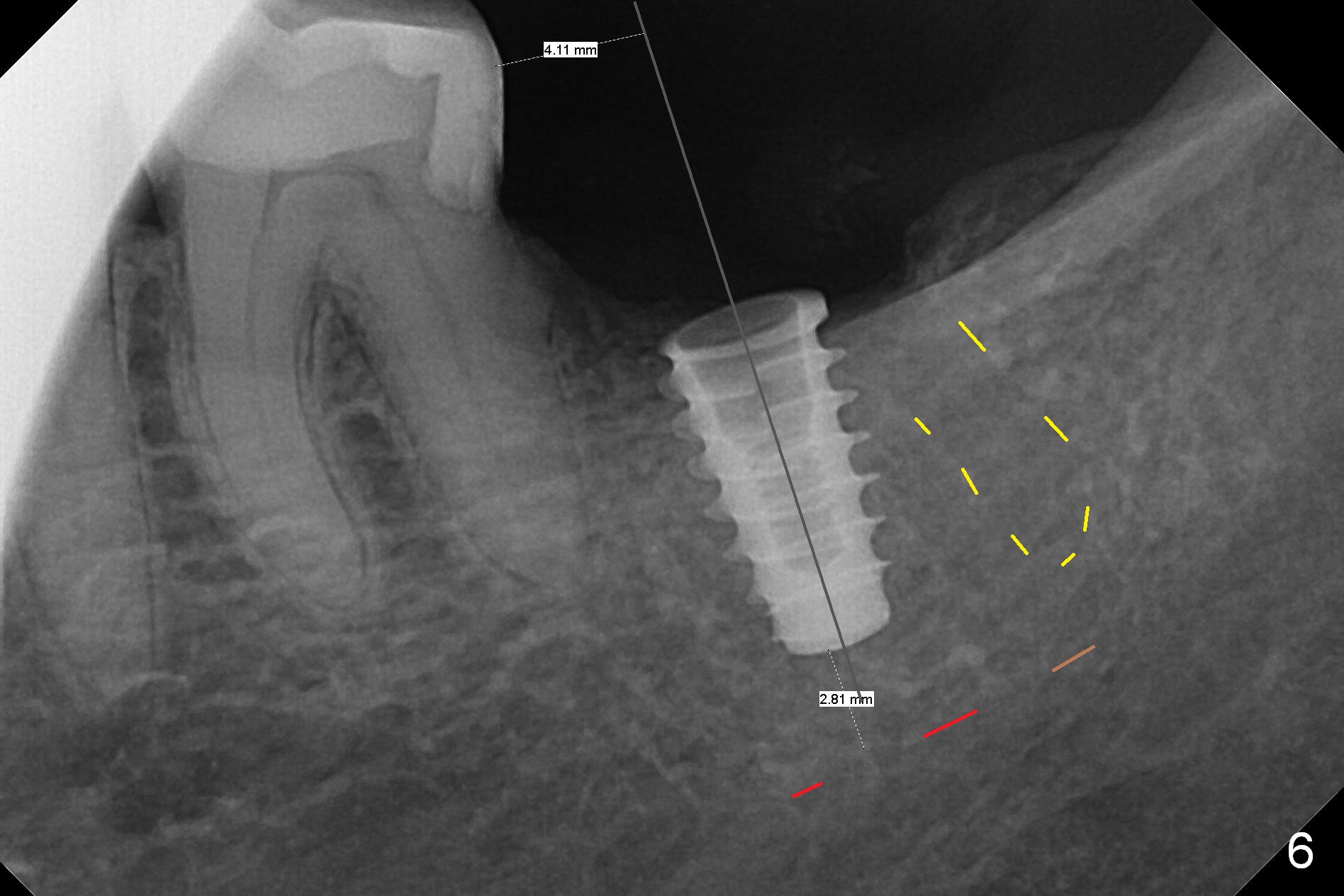
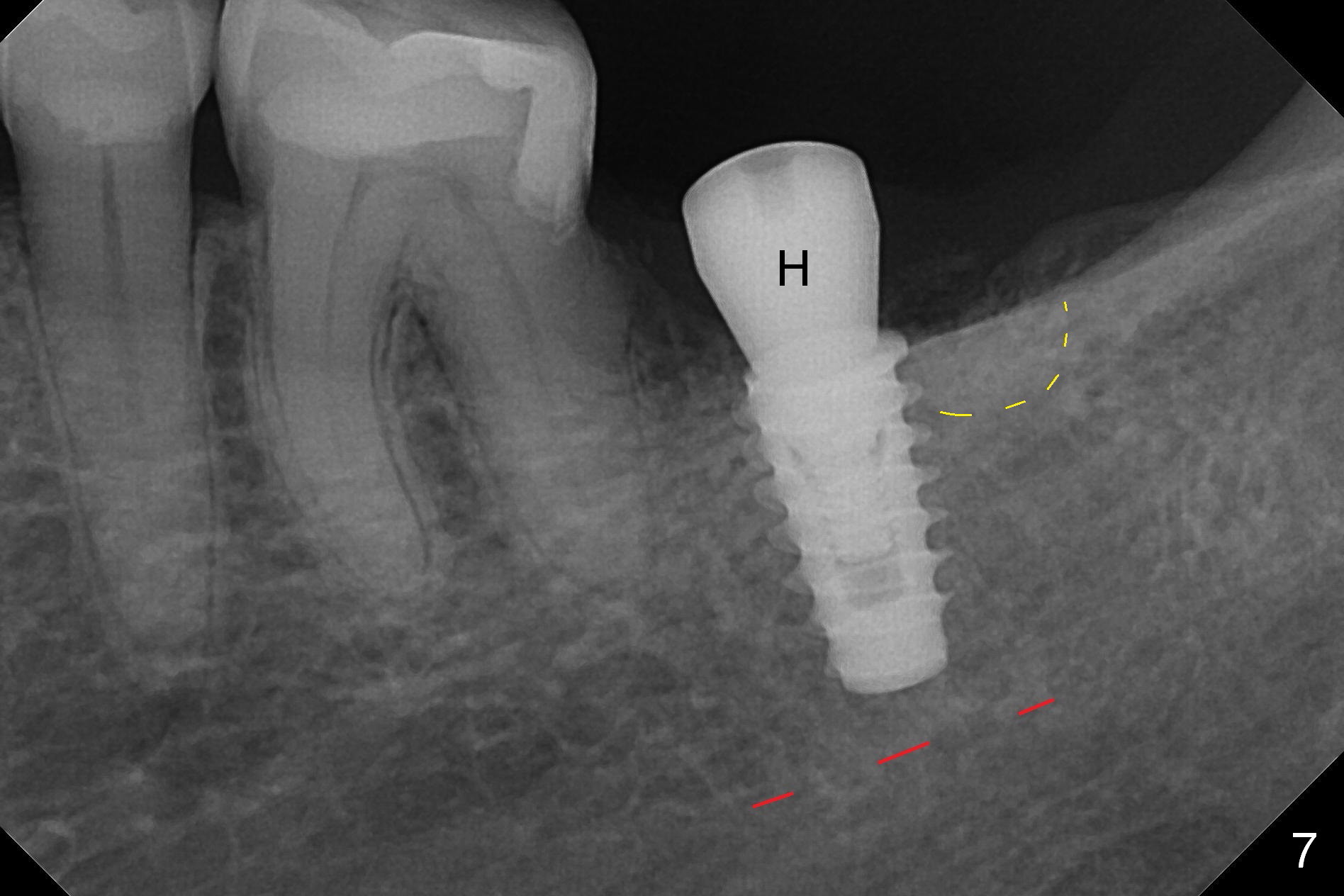
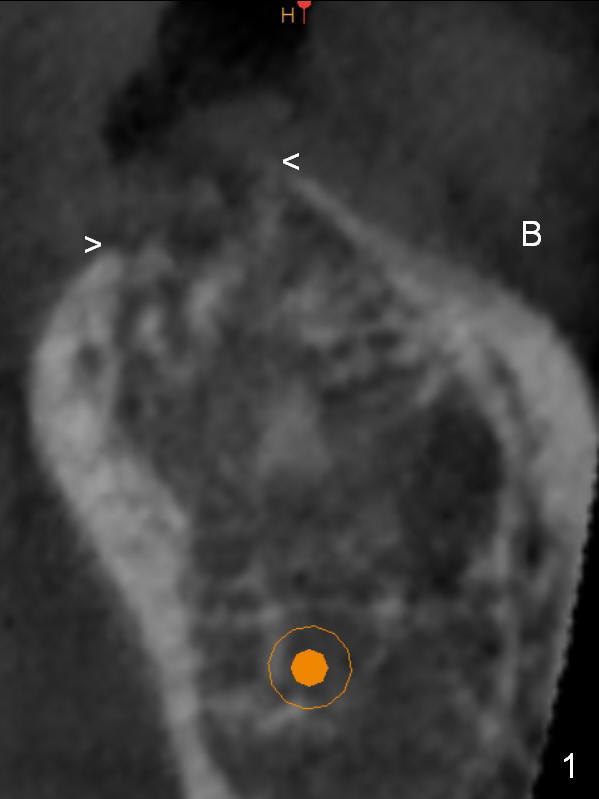
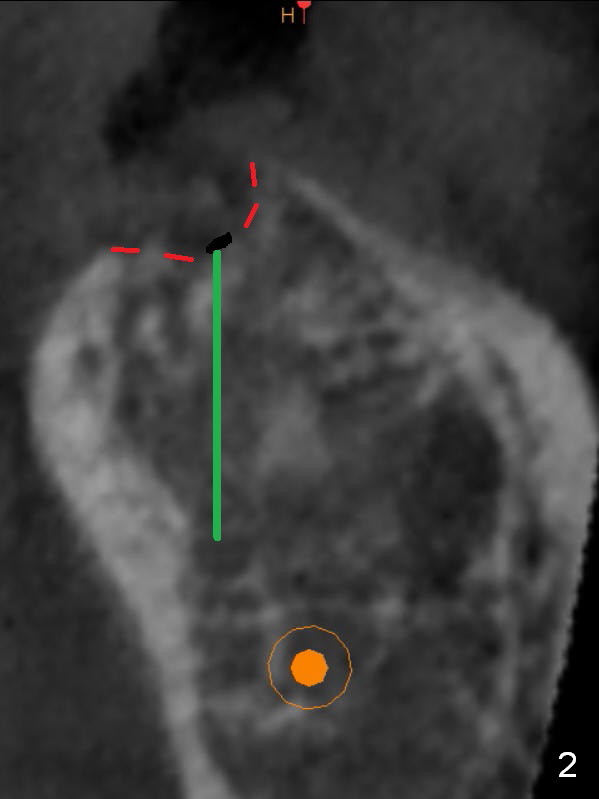
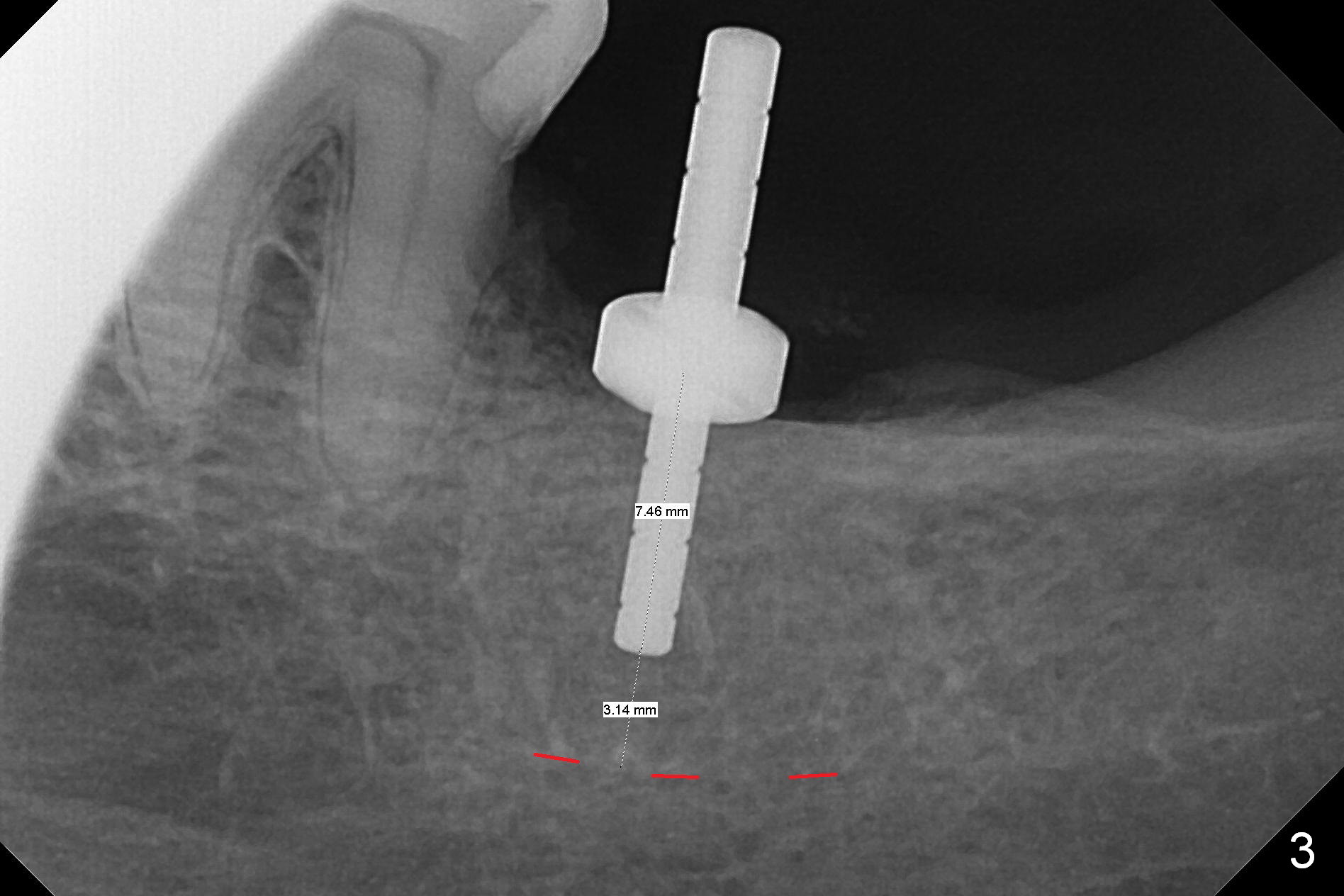
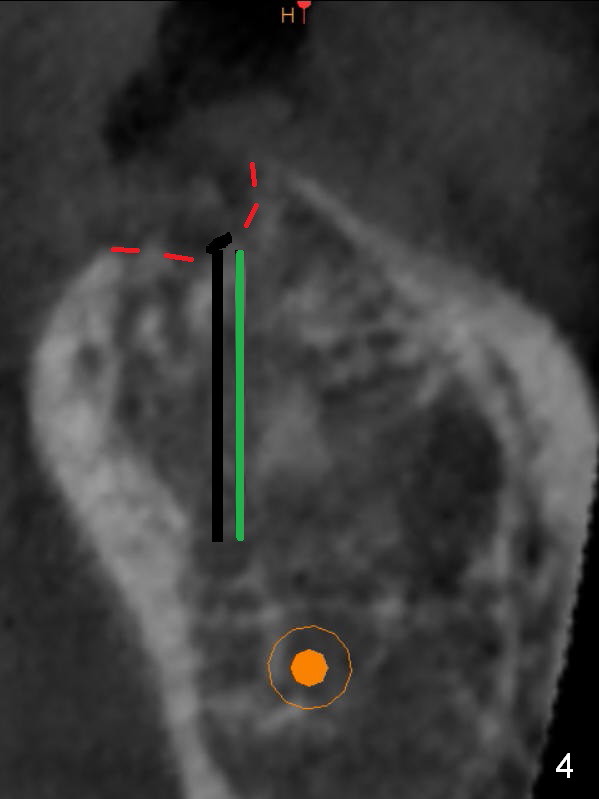
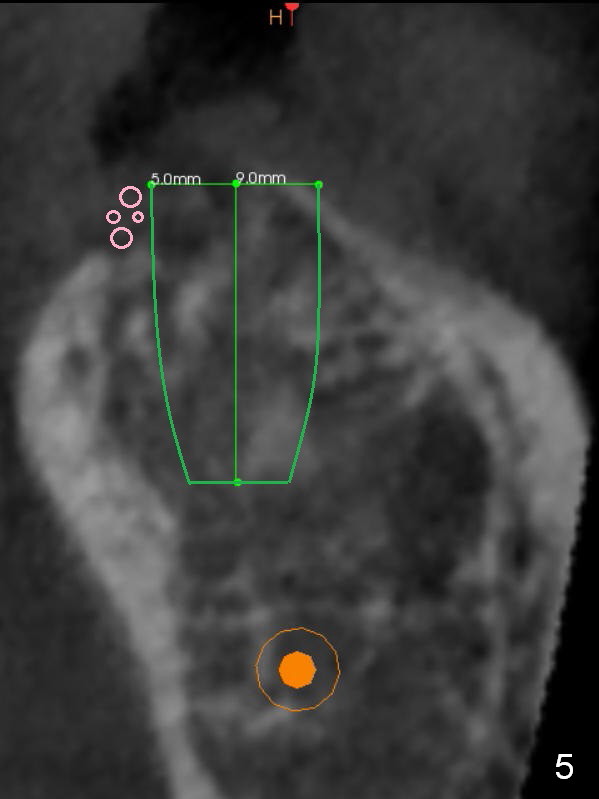
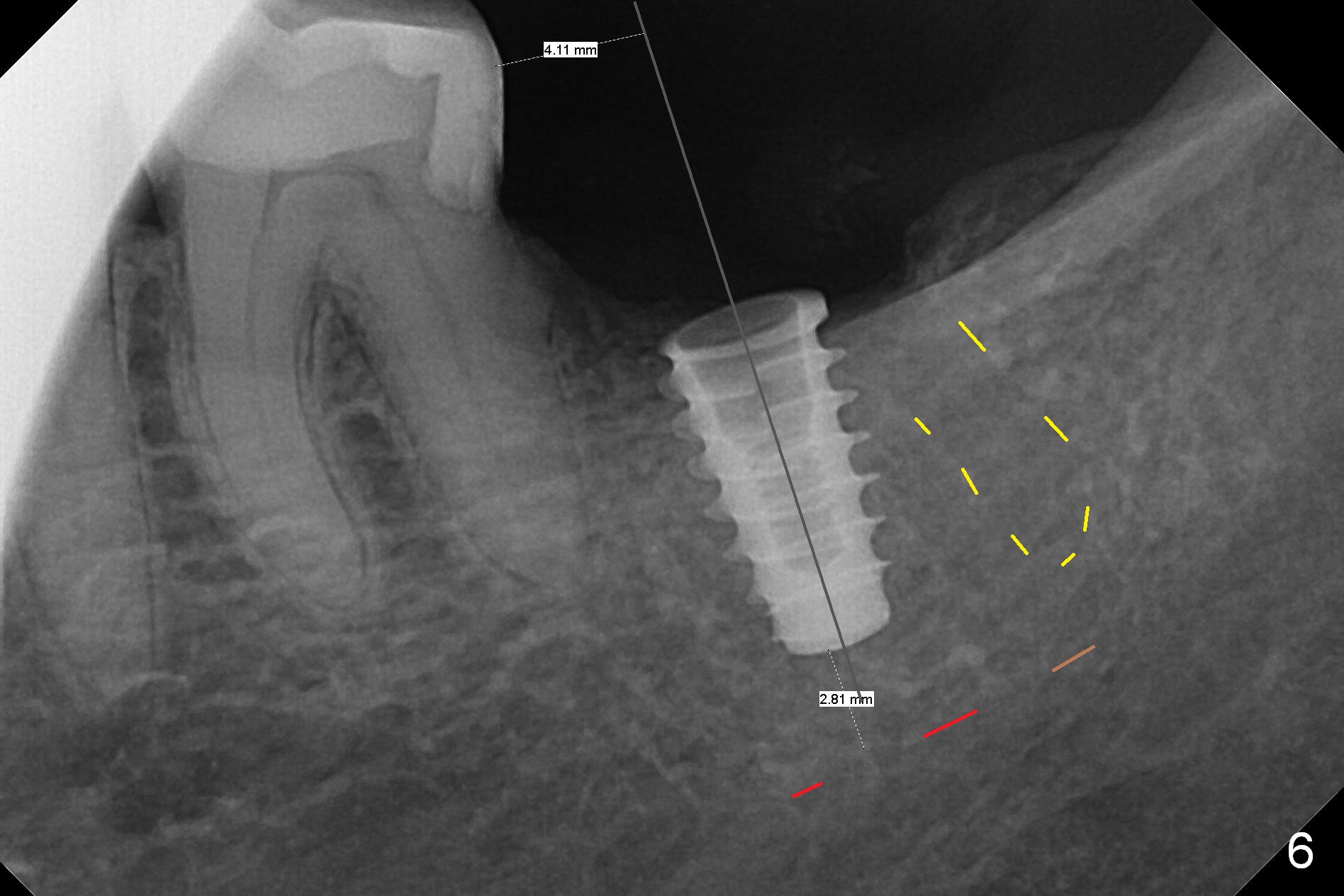
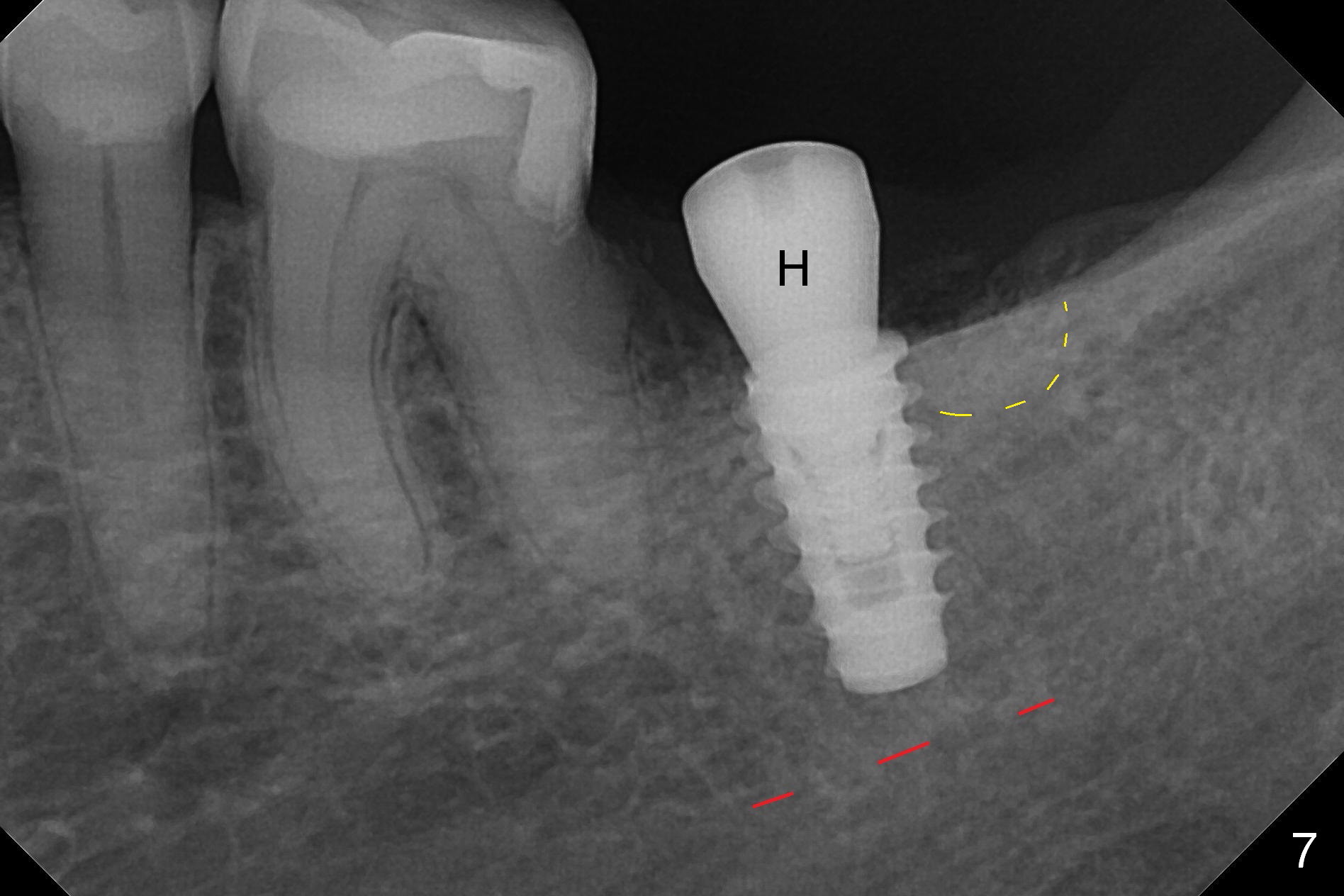
Preop palpation of the edentulous area at #18 does not show the flatness of the ridge top as shown by CBCT. Incision reveals that the ridge is not as wide as CBCT indicates (Fig.1 (coronal section) between arrowheads). In fact the ridge is concave (Fig.2 red dashed line). Osteotomy is initiated in the middle of the concavity (Fig.2 green line) with insertion of 7 mm guide pin (Fig.3). After removal of the pin, the osteotomy is moved buccally (Fig.4). After Marking Bur and 4.3 mm Magic Drill, a 5x9 mm IBS implant is placed with 2.8 mm clearance from the Inferior Alveolar Canal (Fig.6). Following deepening the osteotomy with Final Drill, the implant is placed deeper (Fig.7). The osteotomy happens to be established in the mesial socket, since the distal socket has not completely healed (Fig.6 yellow dashed line). Granulation tissue is removed. Since the lingual crest is lower than the buccal one (Fig.1 B), there is lingual thread exposure after implant placement (Fig.5). The exposed thread is covered by bone graft (autogenous bone, allograft and Osteogen, Fig.5 pink circles). Some of the graft is apparently pushed into the distal socket (Fig.7 yellow dashed line) post GBR and suture. As the implant is placed twice, insertion torque is <10 Ncm (although the implant is stable). A 5x3 mm healing abutment is placed (Fig.7 H).
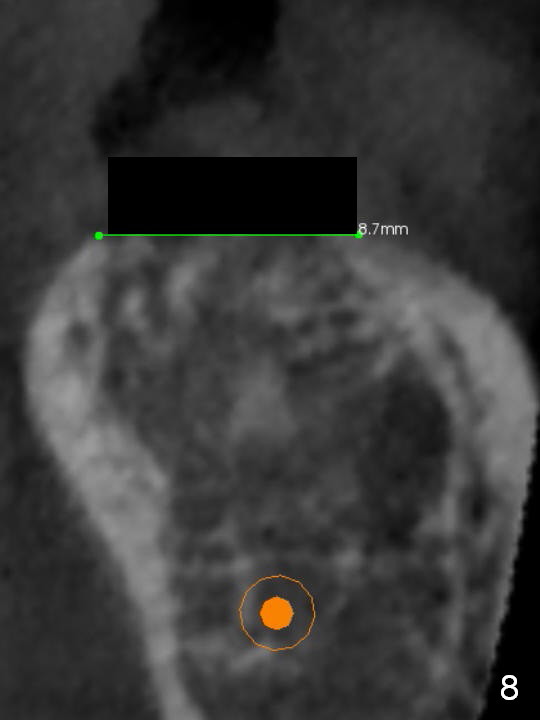
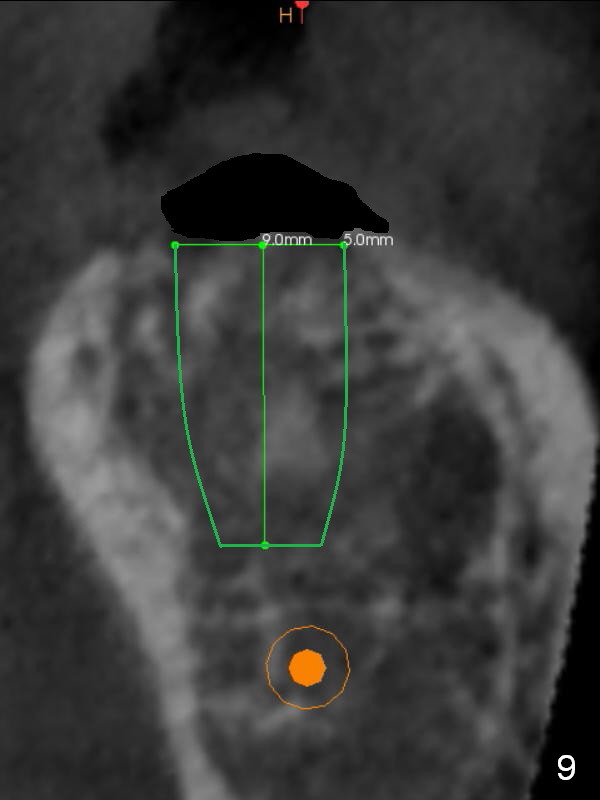
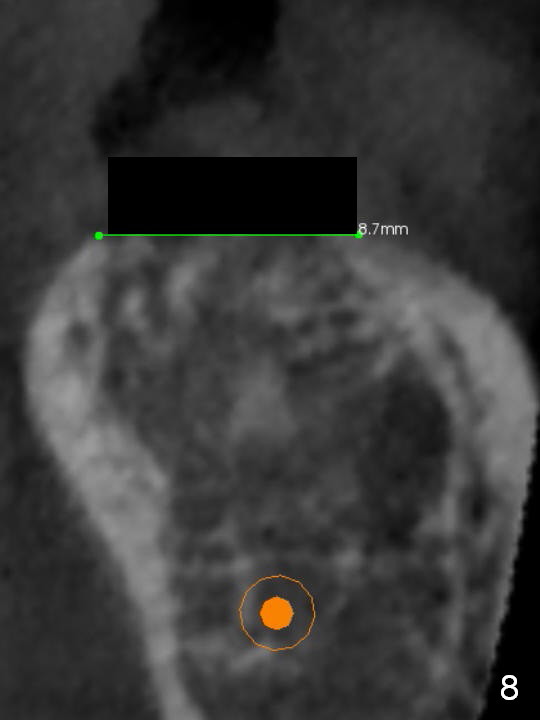
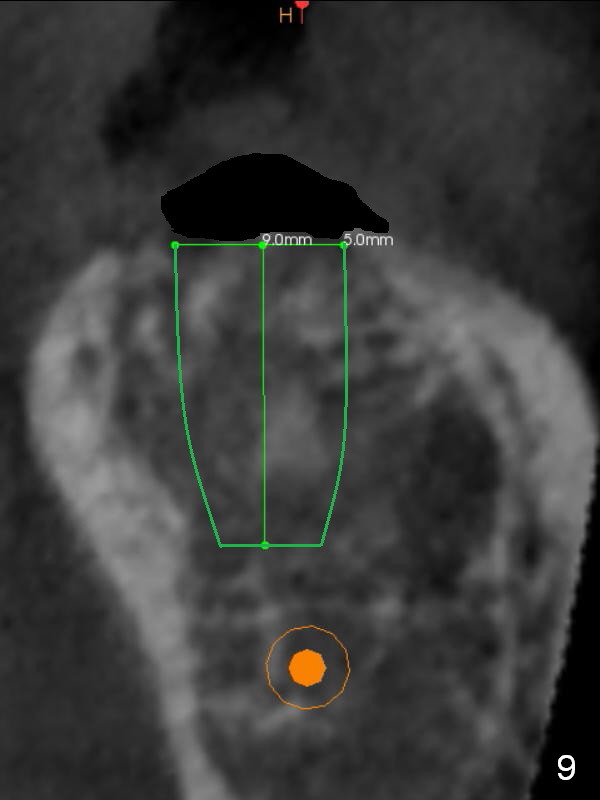
To bury the implant evenly, the ridge should be flattened (Fig.8) prior to osteotomy and implant placement (Fig.9) when bone height is sufficient.
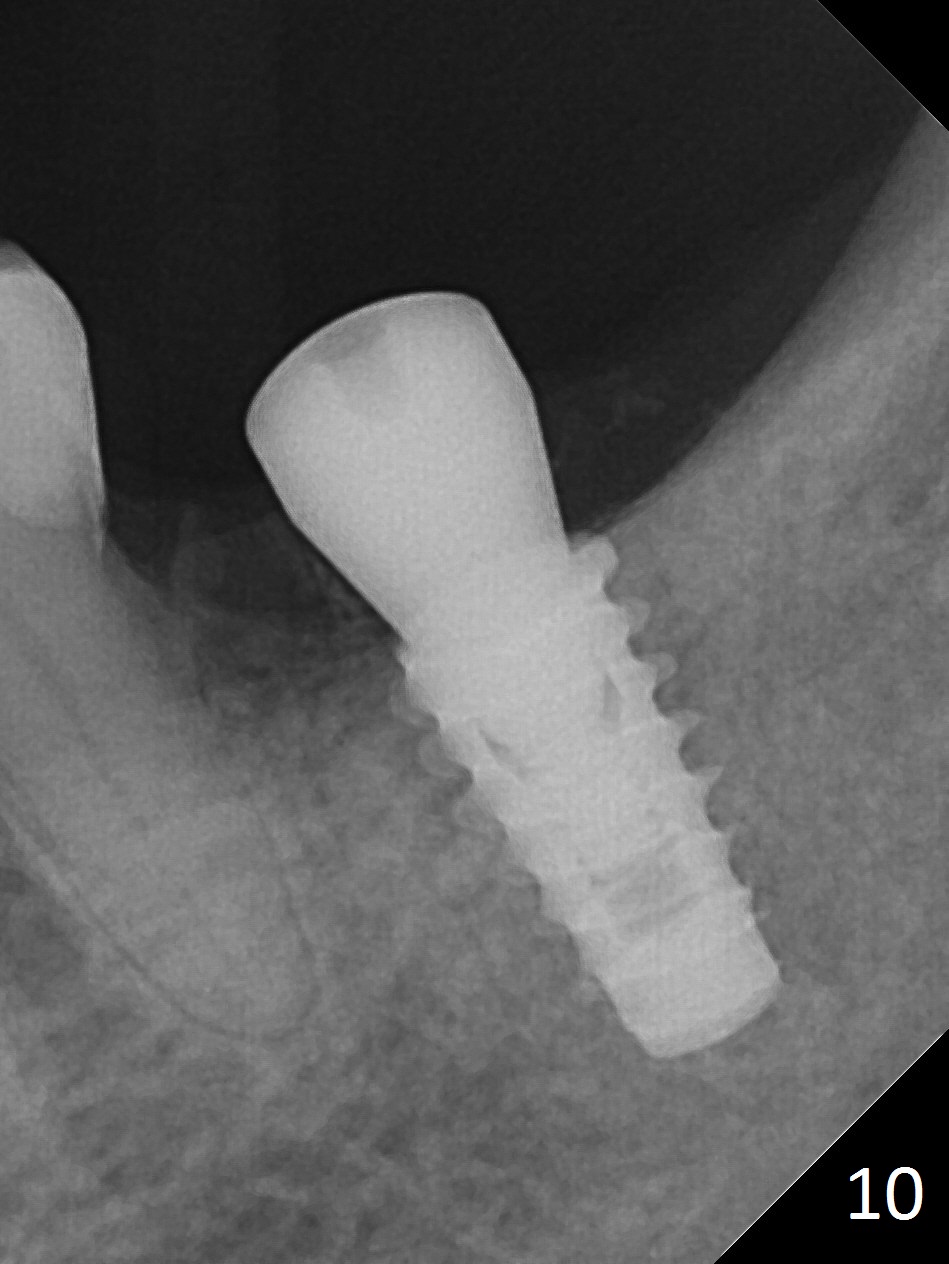
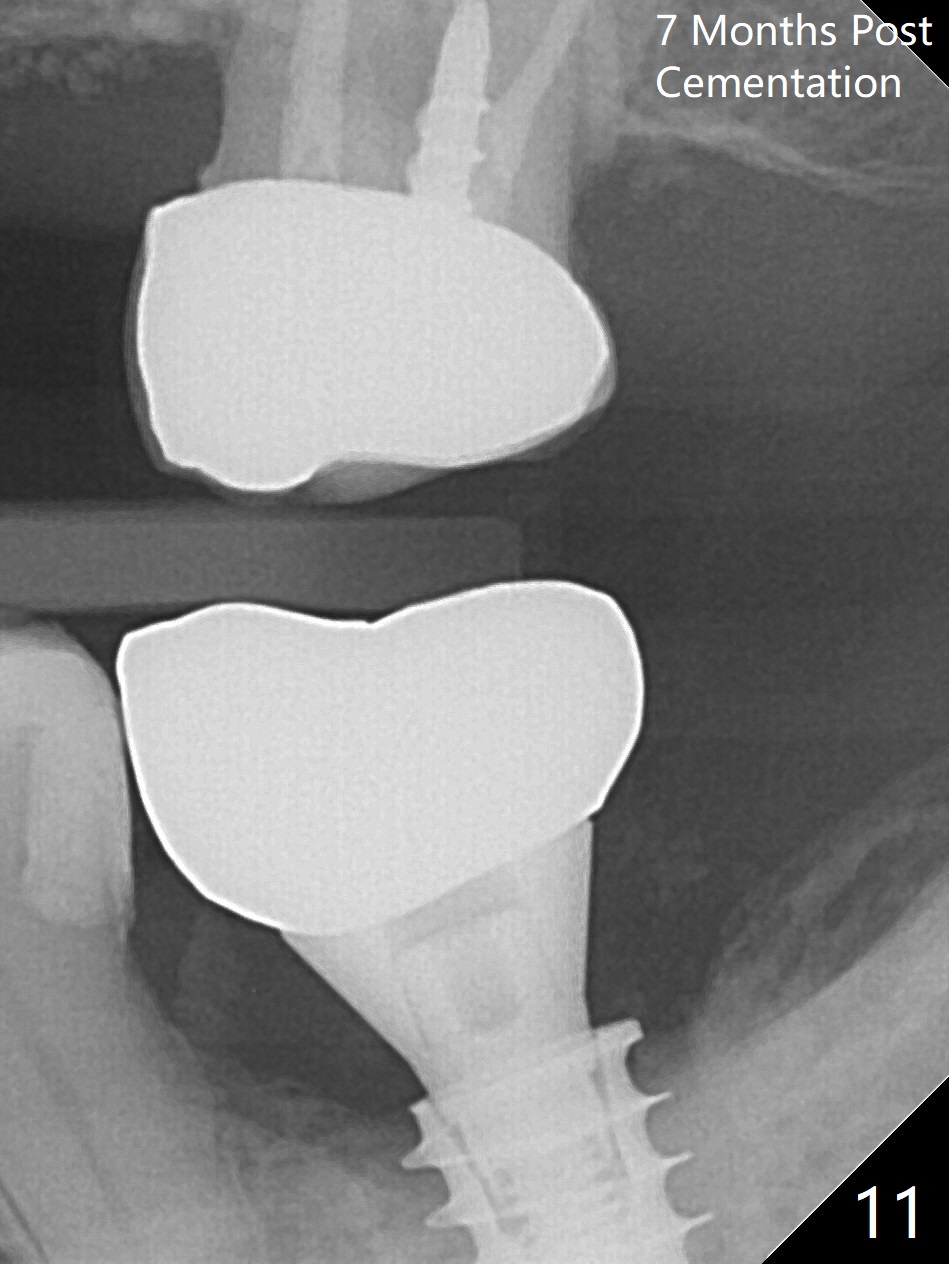
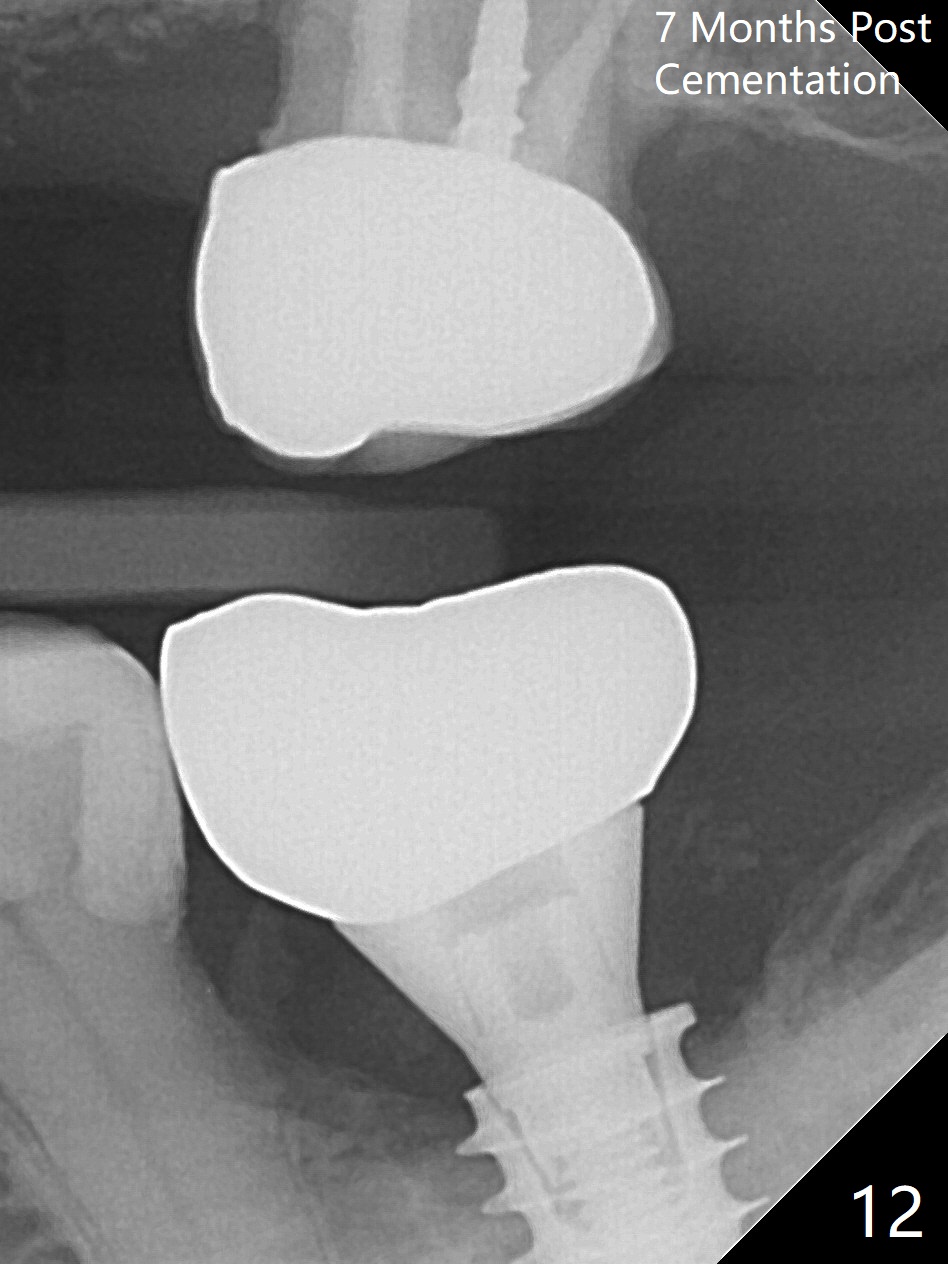
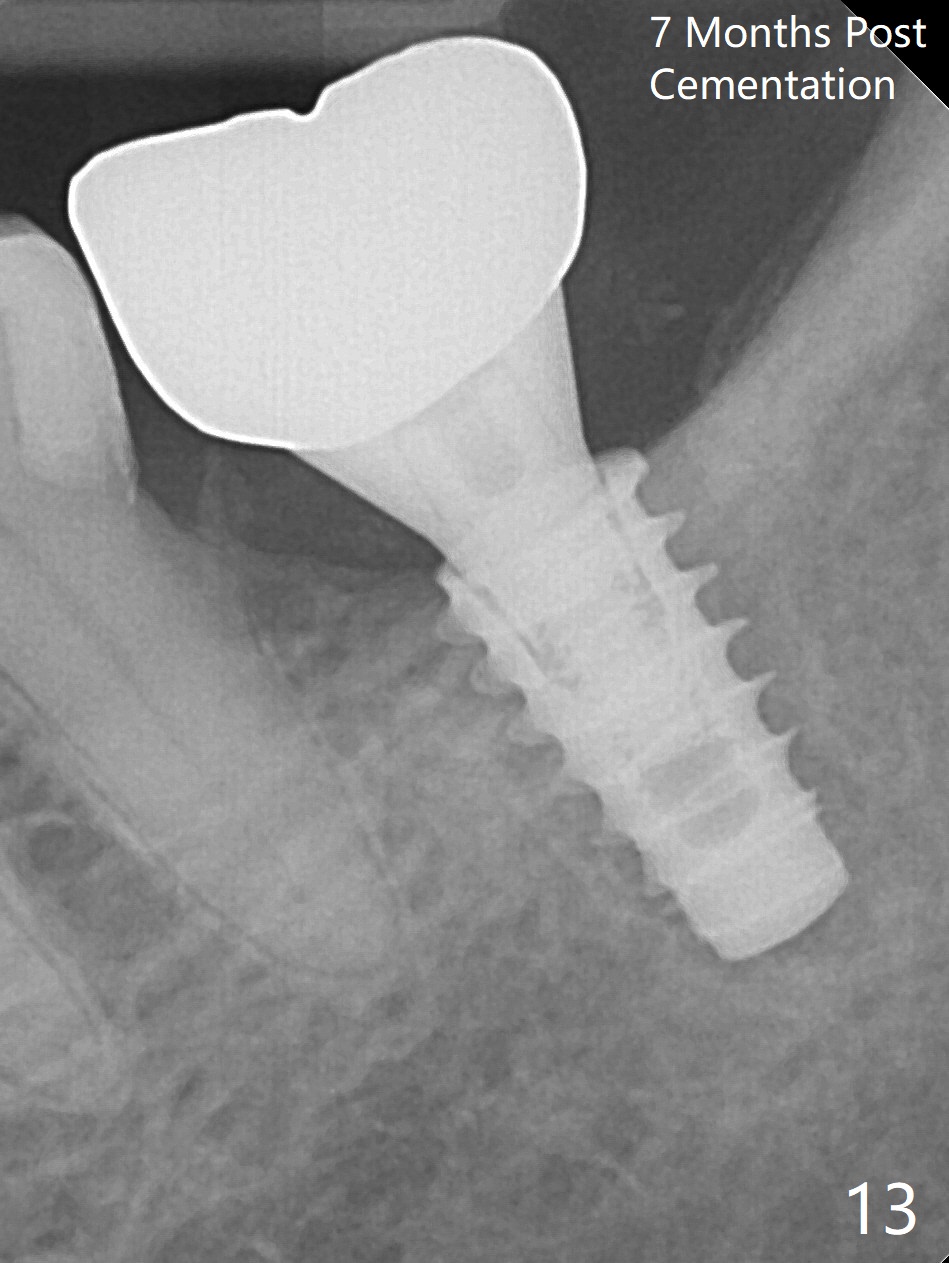
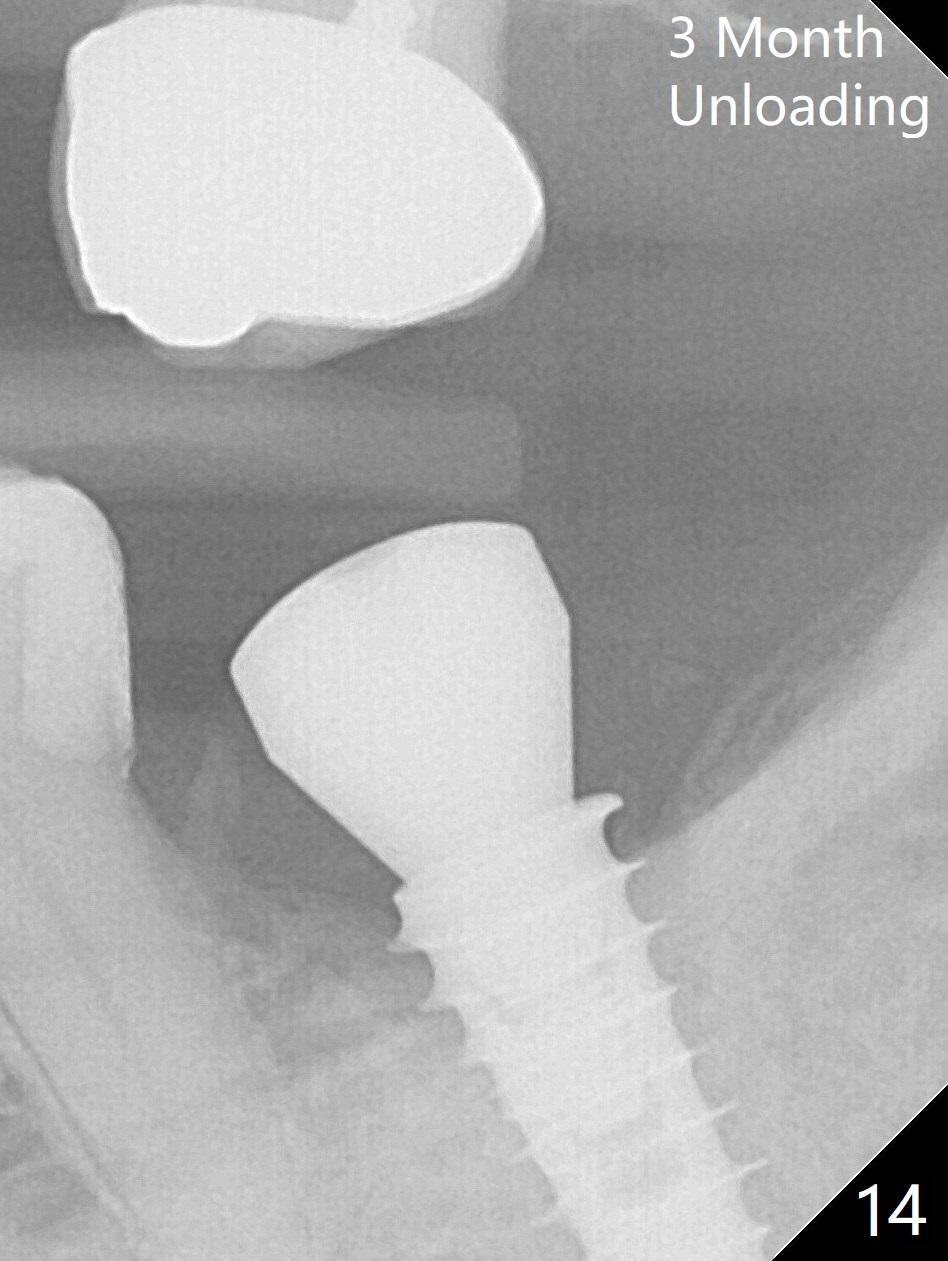
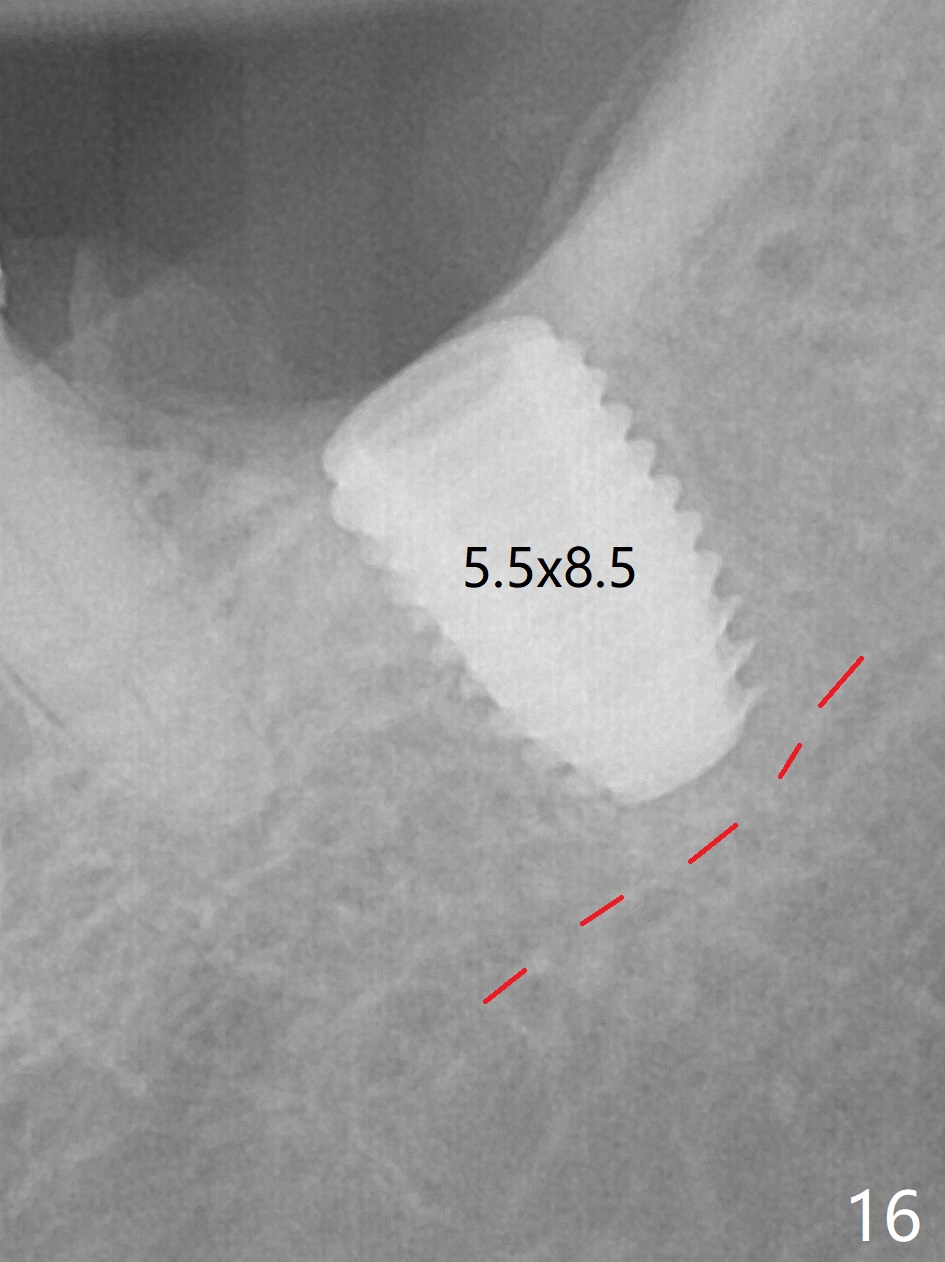
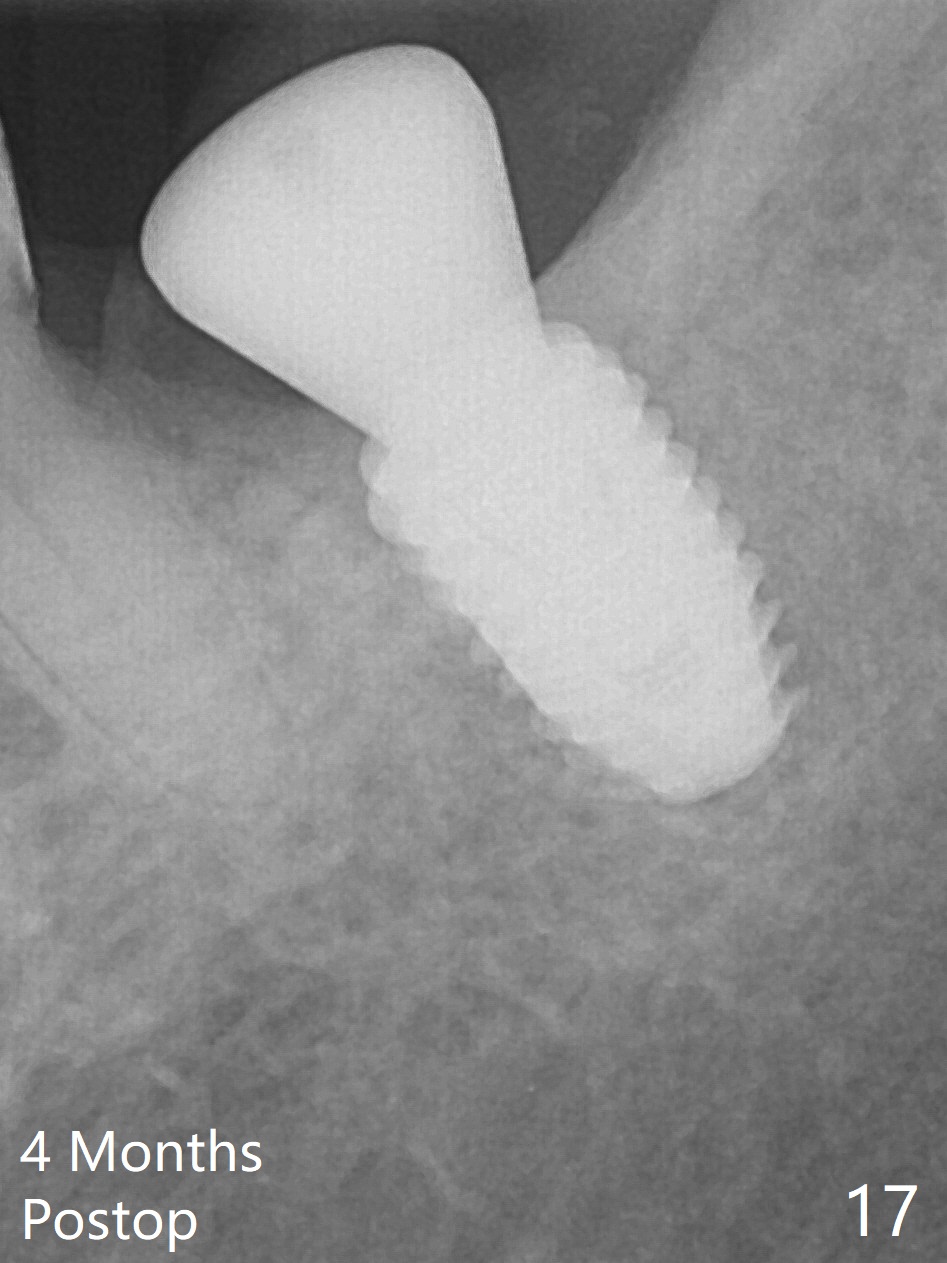
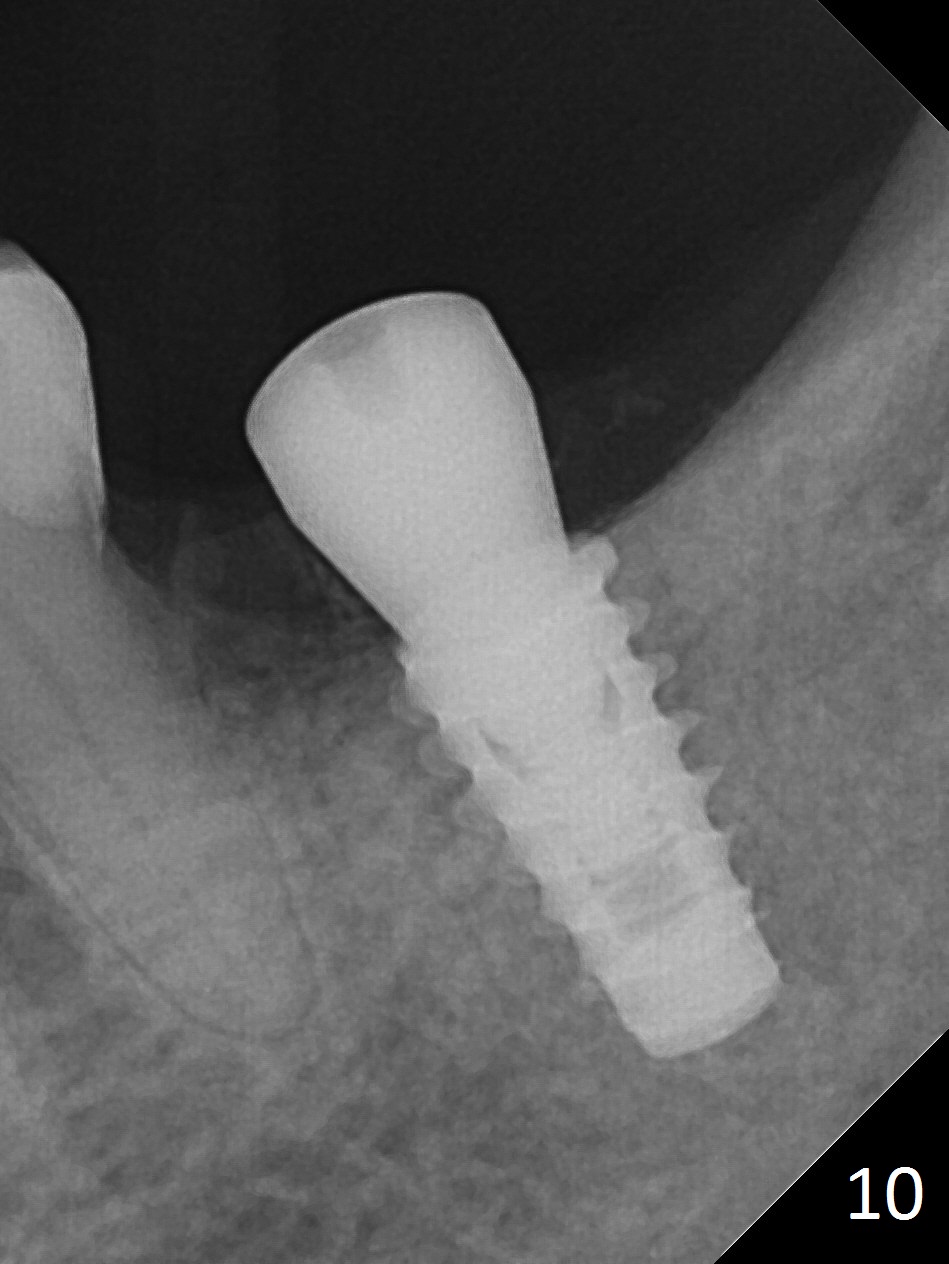
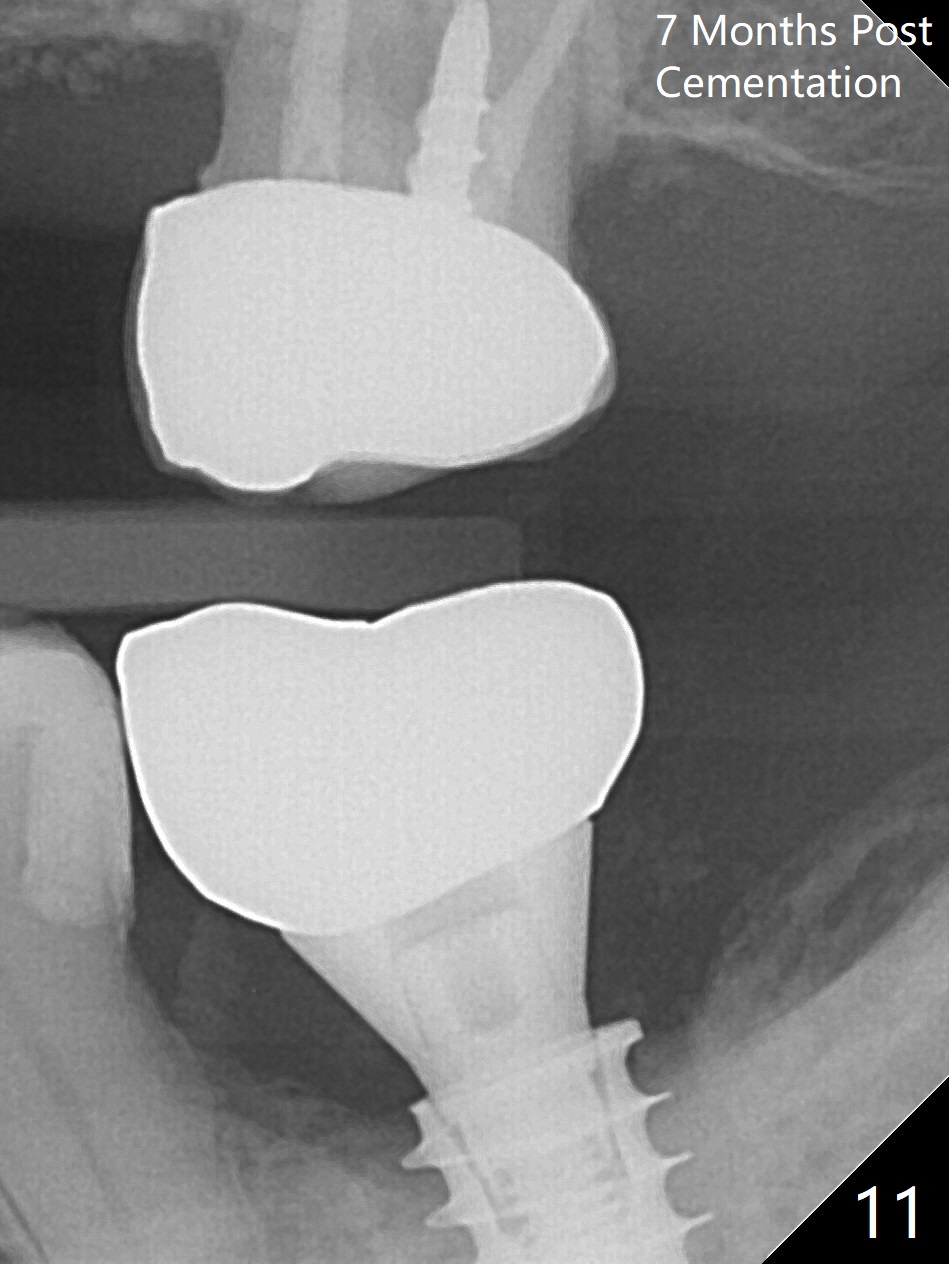
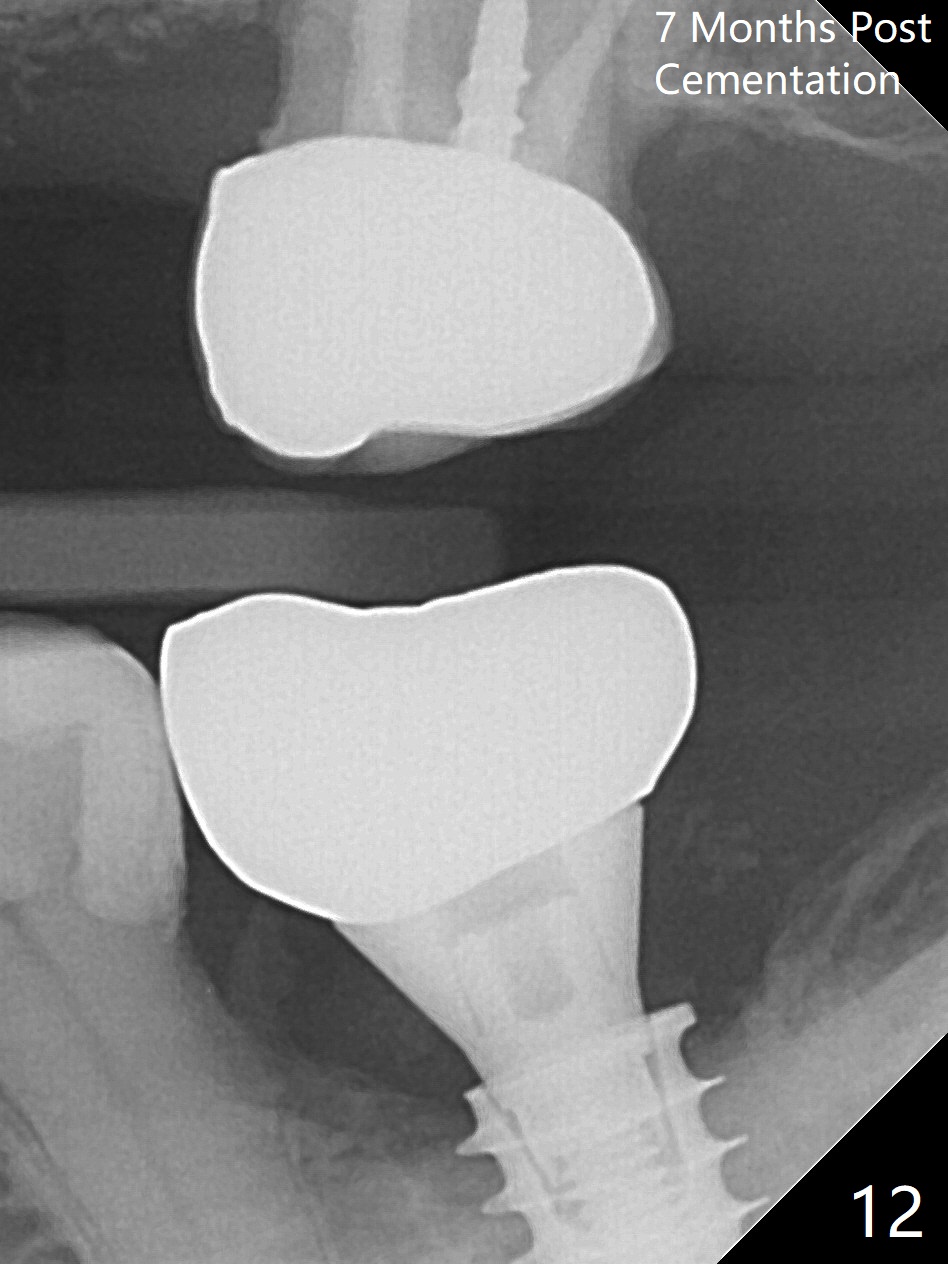
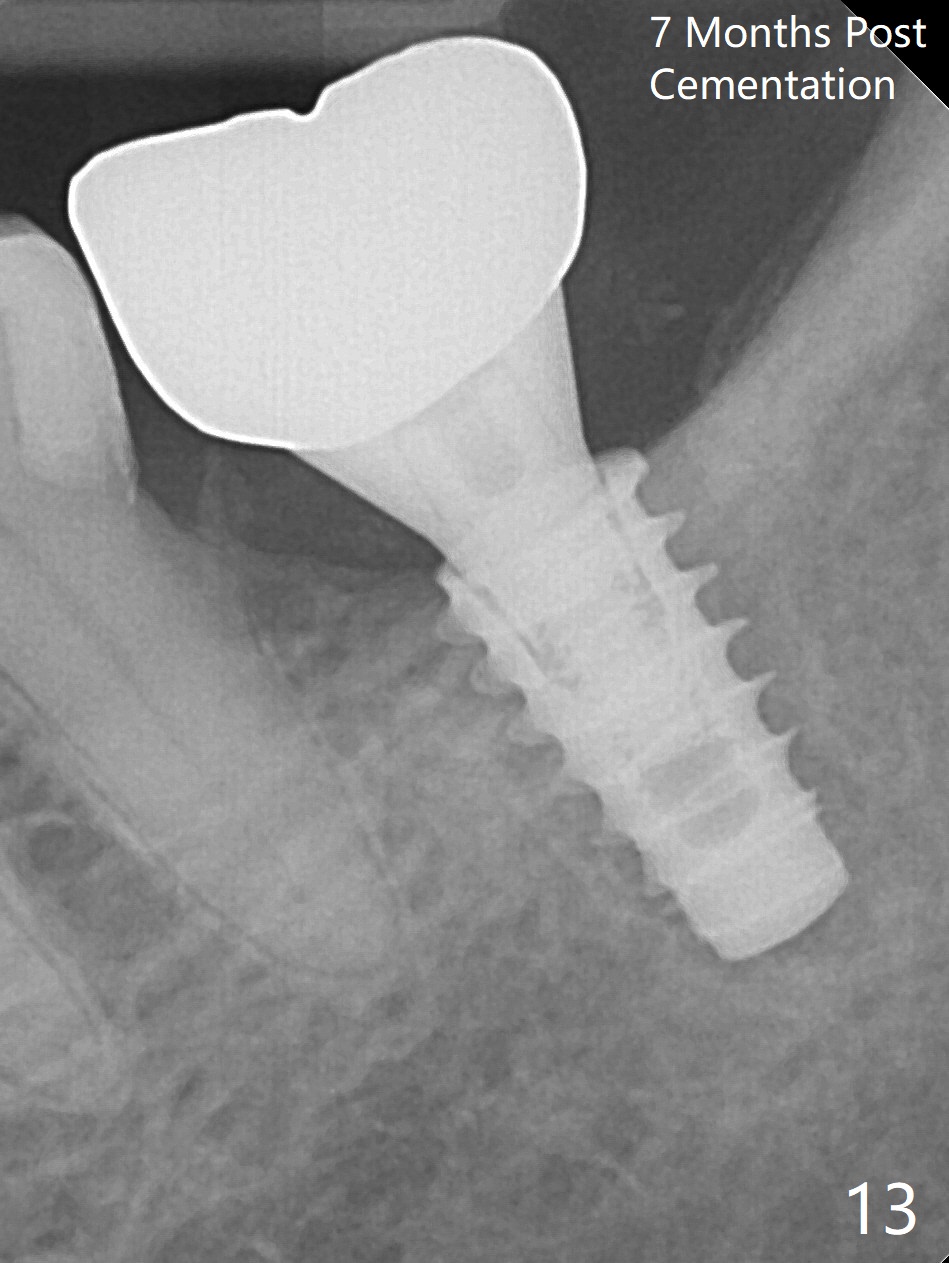
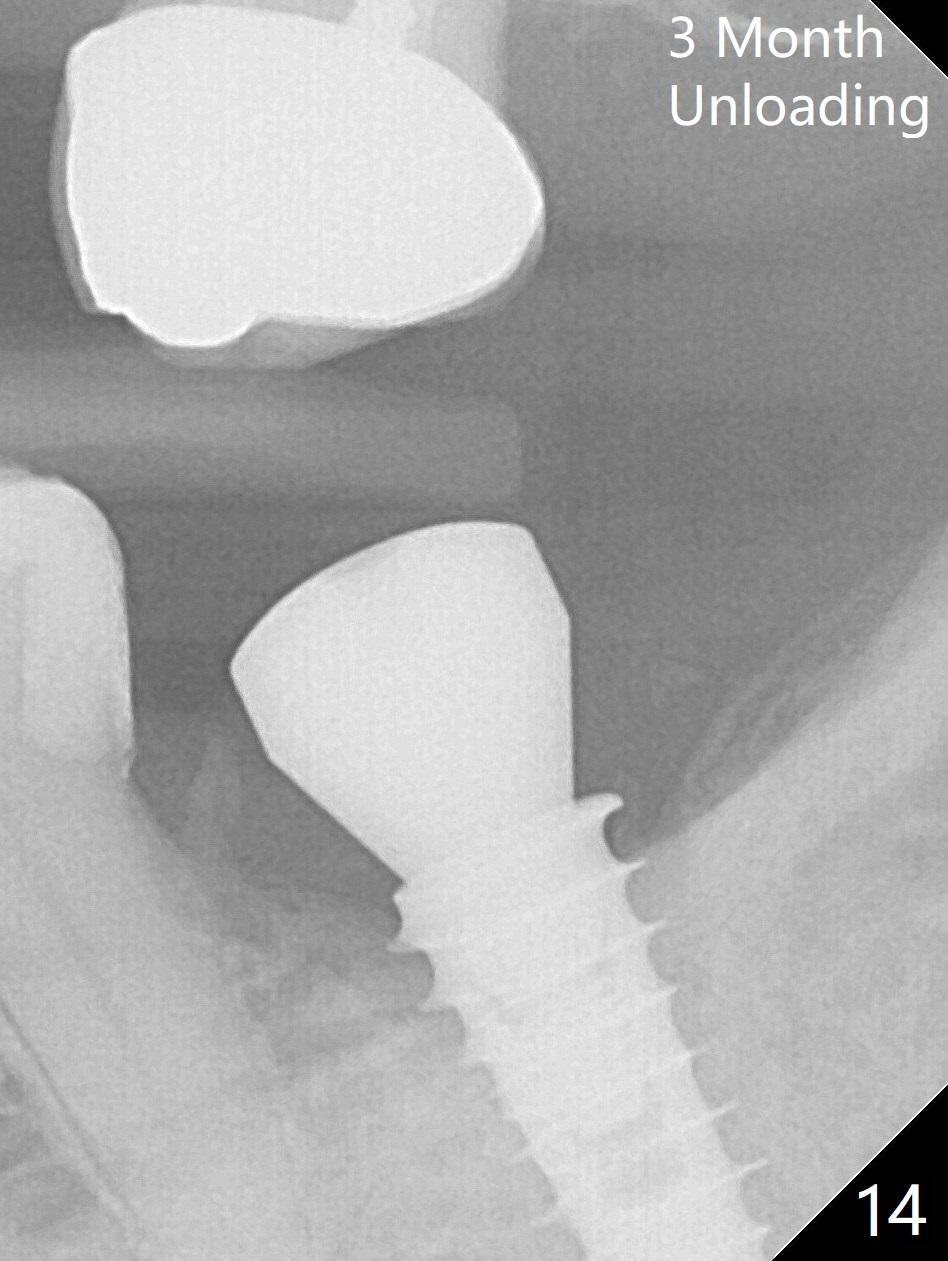
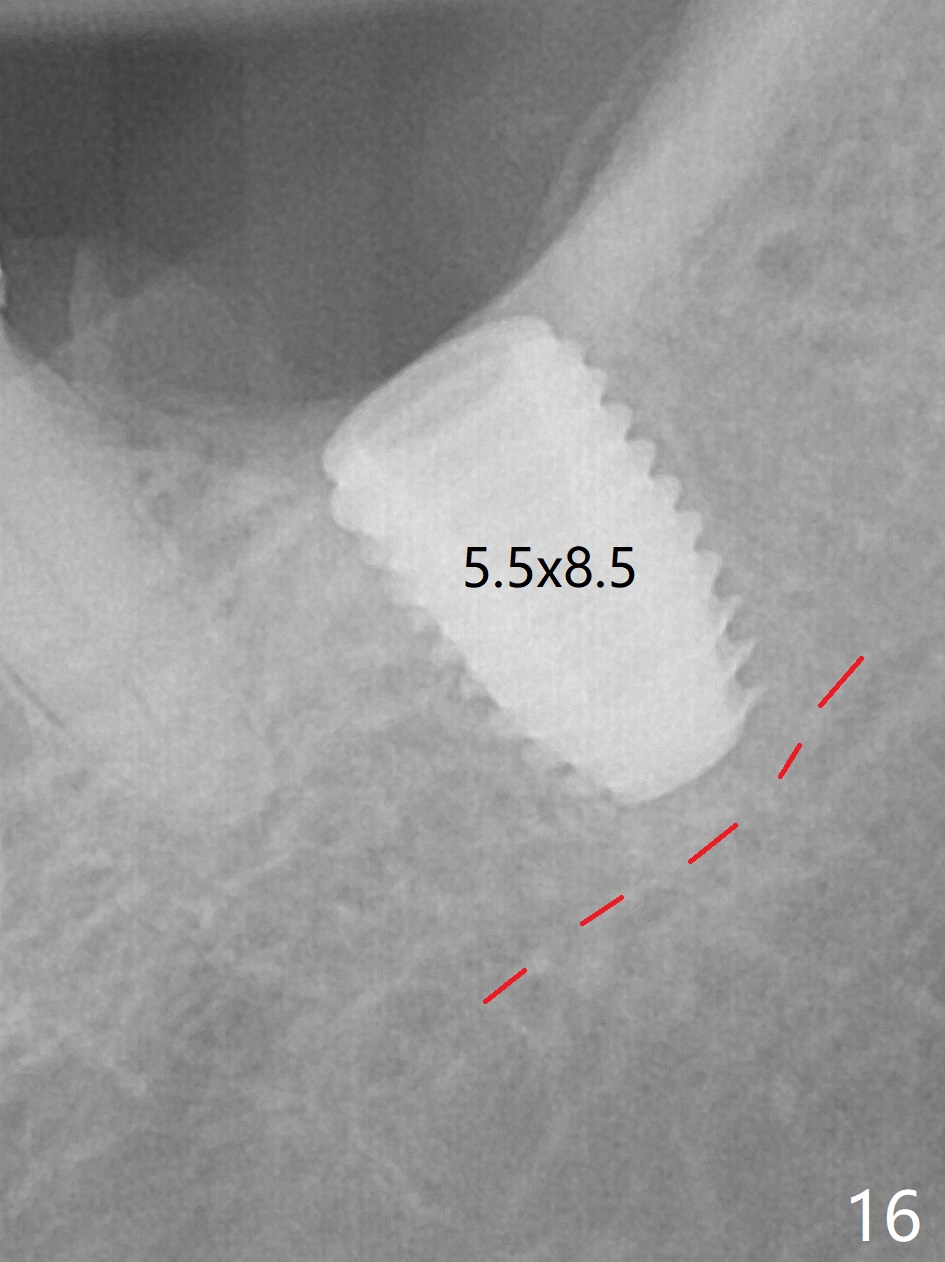
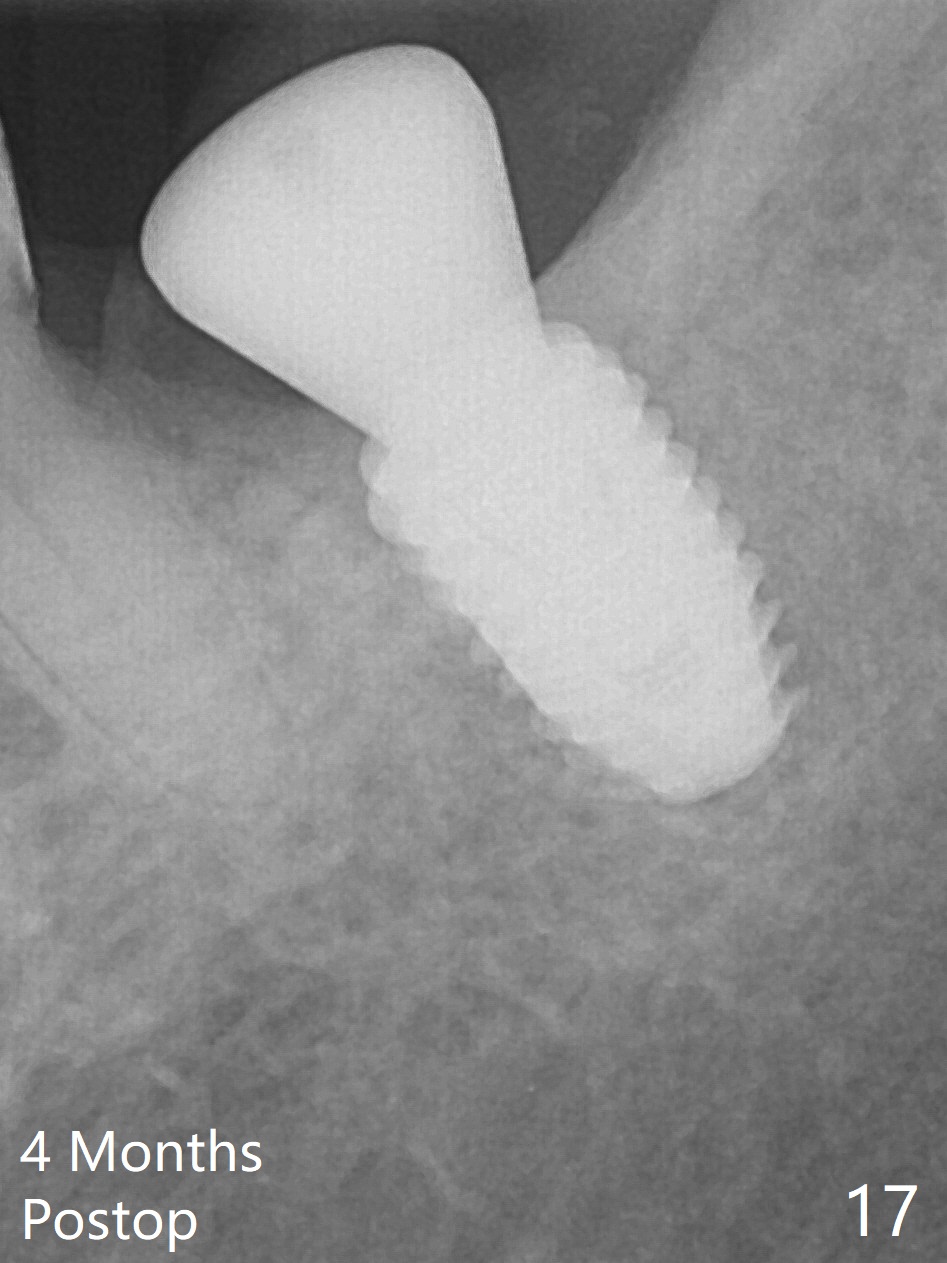
There is no apparent bone loss 4 months postop (Fig.10). There is chewing pain in spite of occlusal adjustment 7 months post cementation (Fig.11-13: increased radiolucency around the implant). The crown/abutment is removed and a healing abutment is placed (6x3 mm); the implant is stable. The patient return for re-evaluation in 3 months (15 months postop); radiolucency appears to reduce (Fig.14). But there is pain when the healing abutment is being removed. After local anesthesia, the implant is removed with a wrench. Following debridement of the osteototomy (intact, although tender), a 5x10 mm dummy implant with SLA surface is placed (Fig.15). After 5.5 mm tap, a 5.5x8.5 mm implant is placed with >50 Ncm (Fig.16). A 6.8x5 mm healing abutment is placed, followed by periodontal dressing. Re-analysis of preop CBCT shows that the bone density at the site is low: 70 units average. Progressive loading is necessary for this case 4-6 months postop. The soft and hard tissues around the implant seem to heal 4 months postop (Fig.17).
Return to
Lower
Molar Immediate Implant
Armaments
Xin Wei, DDS, PhD, MS 1st edition 01/20/2017, last revision 08/30/2018