
,%20then%203.3x13,%20final%20drill.jpg)

 |
 |
 |
|
,%20then%203.3x13,%20final%20drill.jpg) |
 |
 |
|
 |
 |
||
Flap Surgery for Bone Graft M
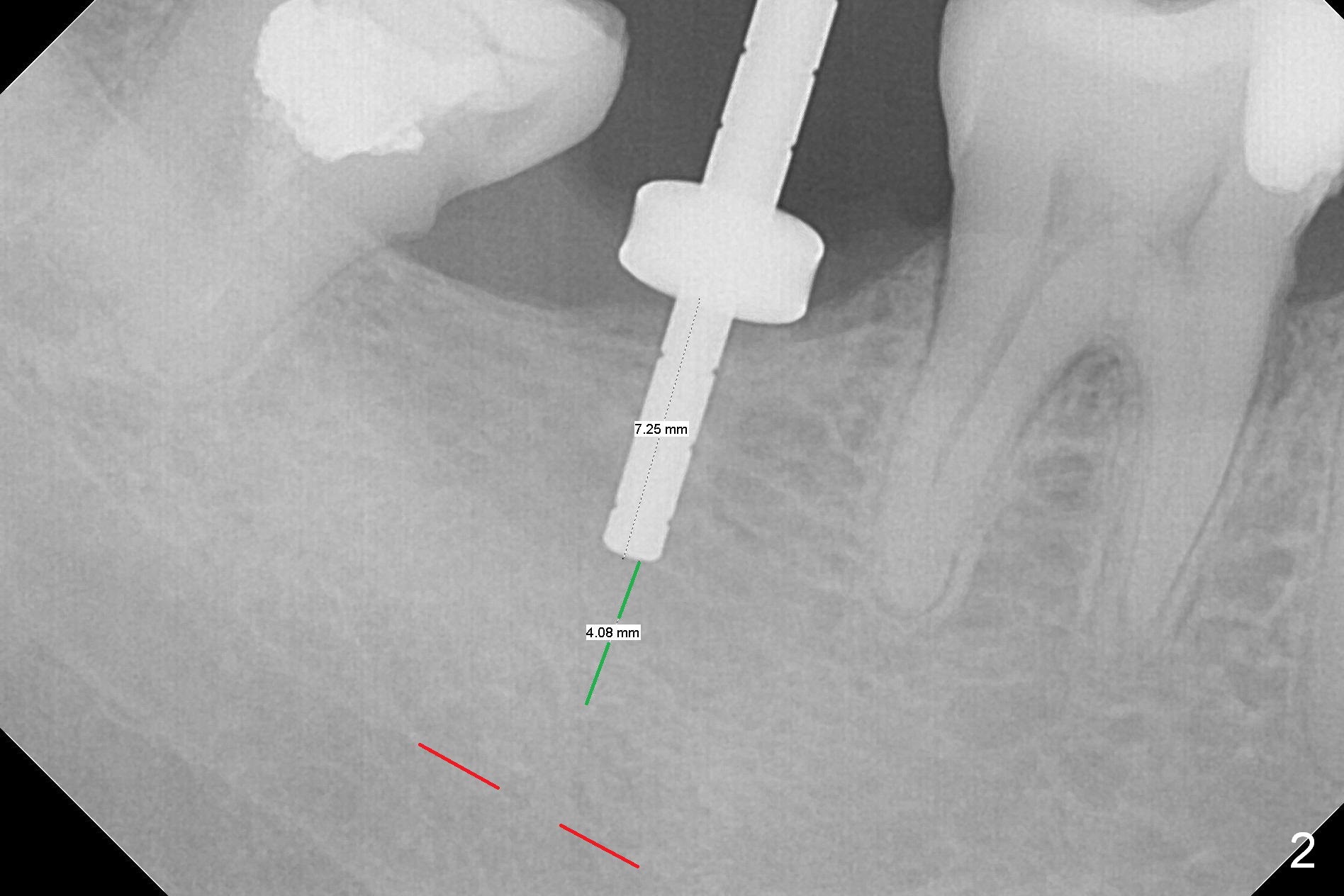
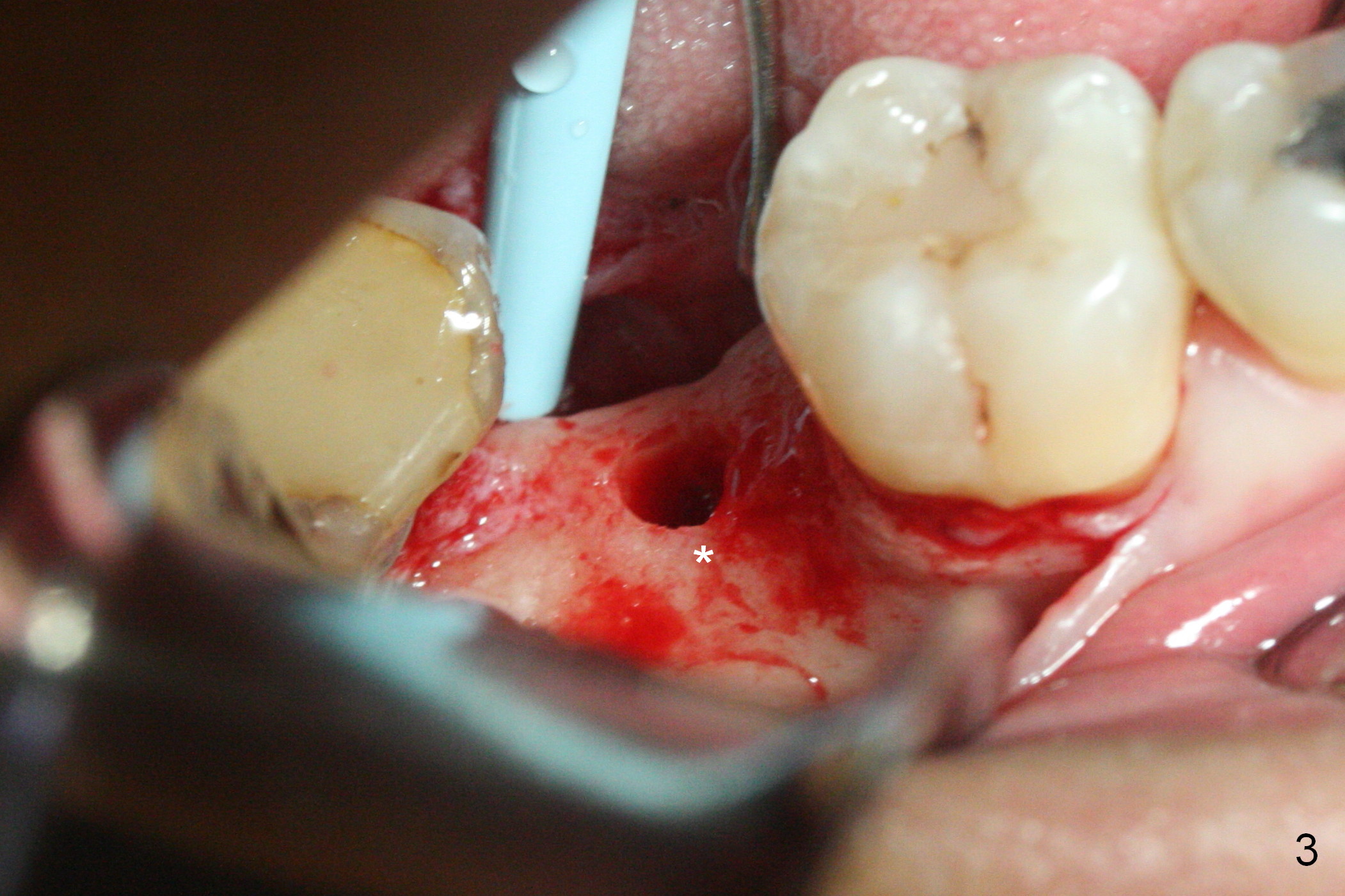
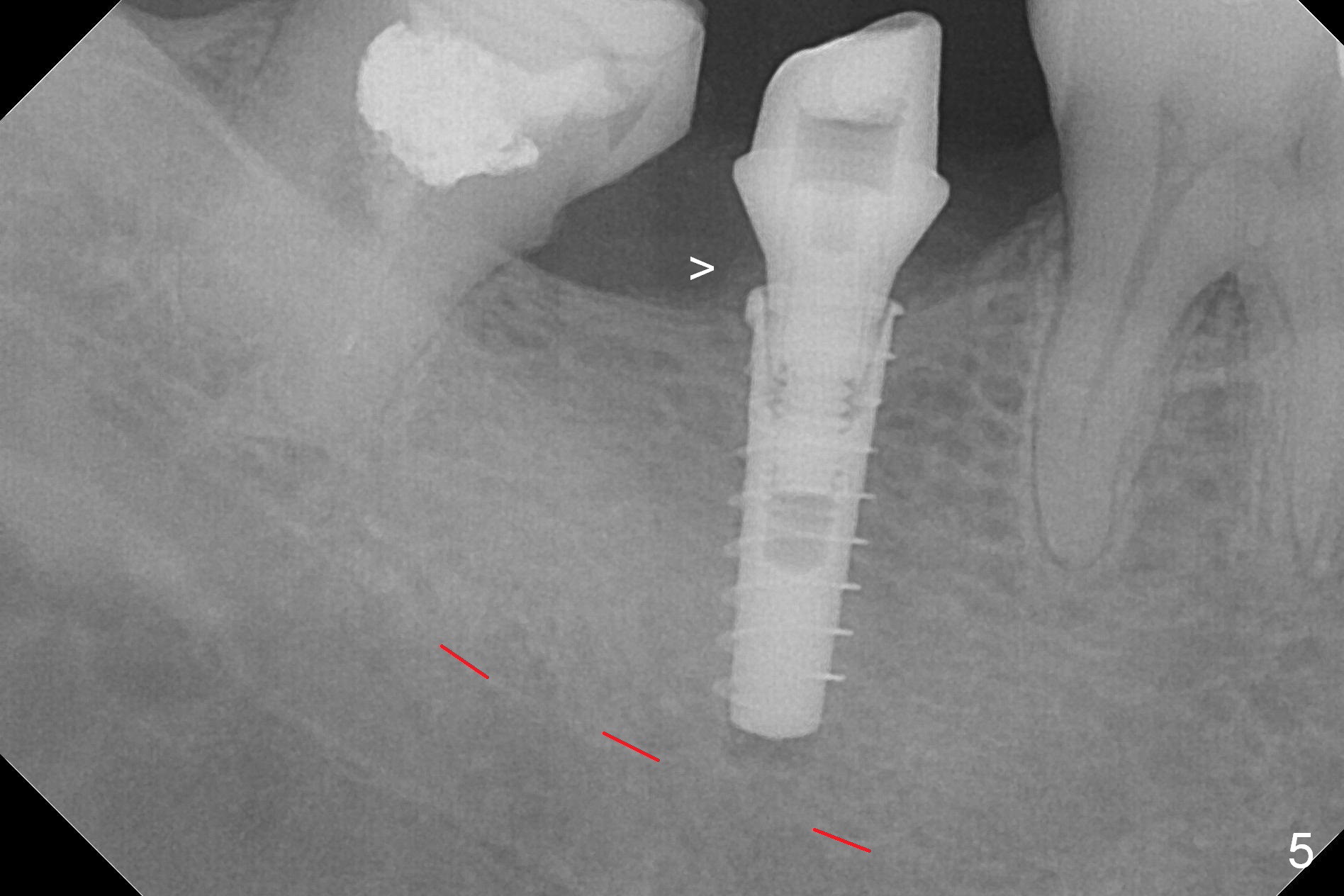
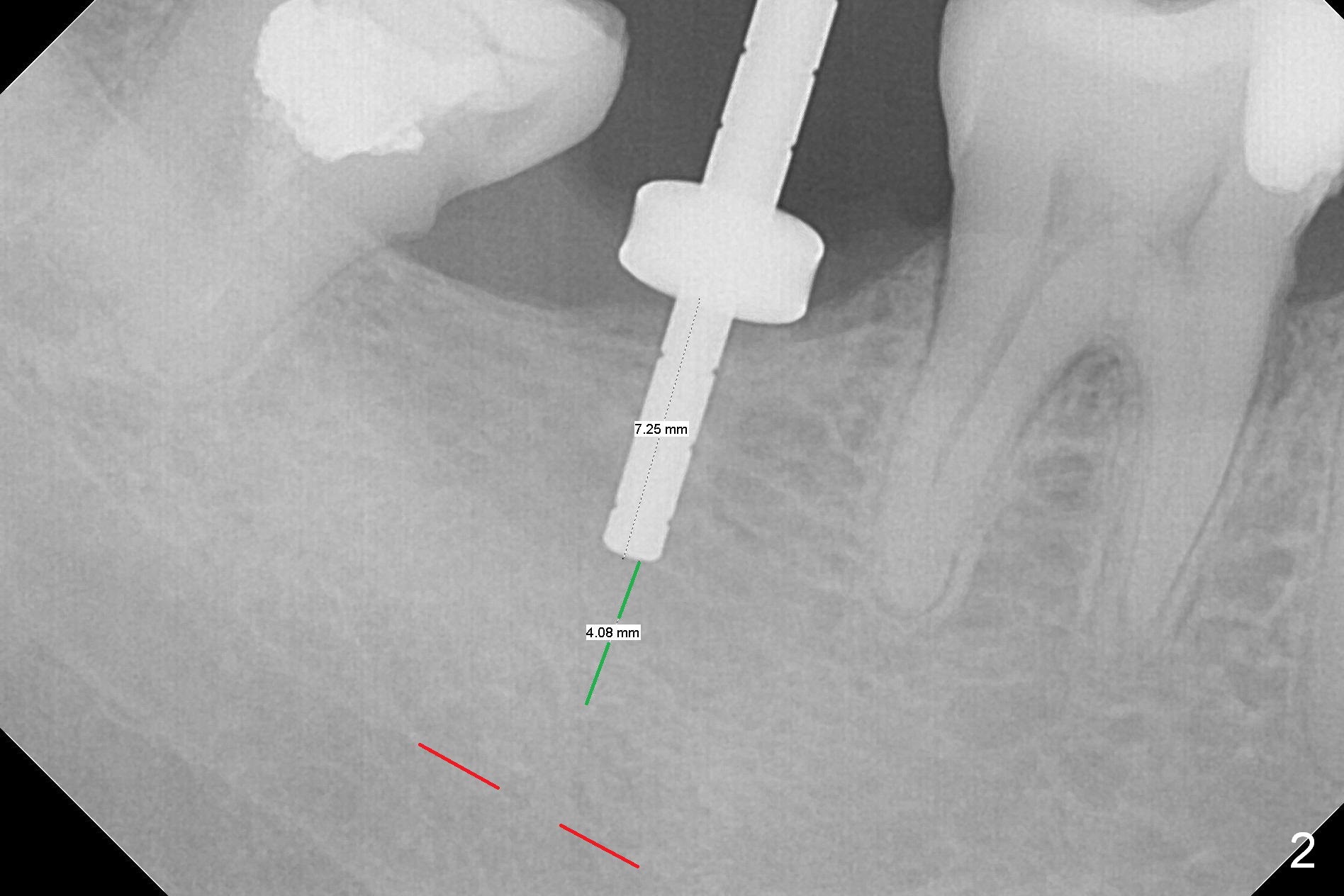
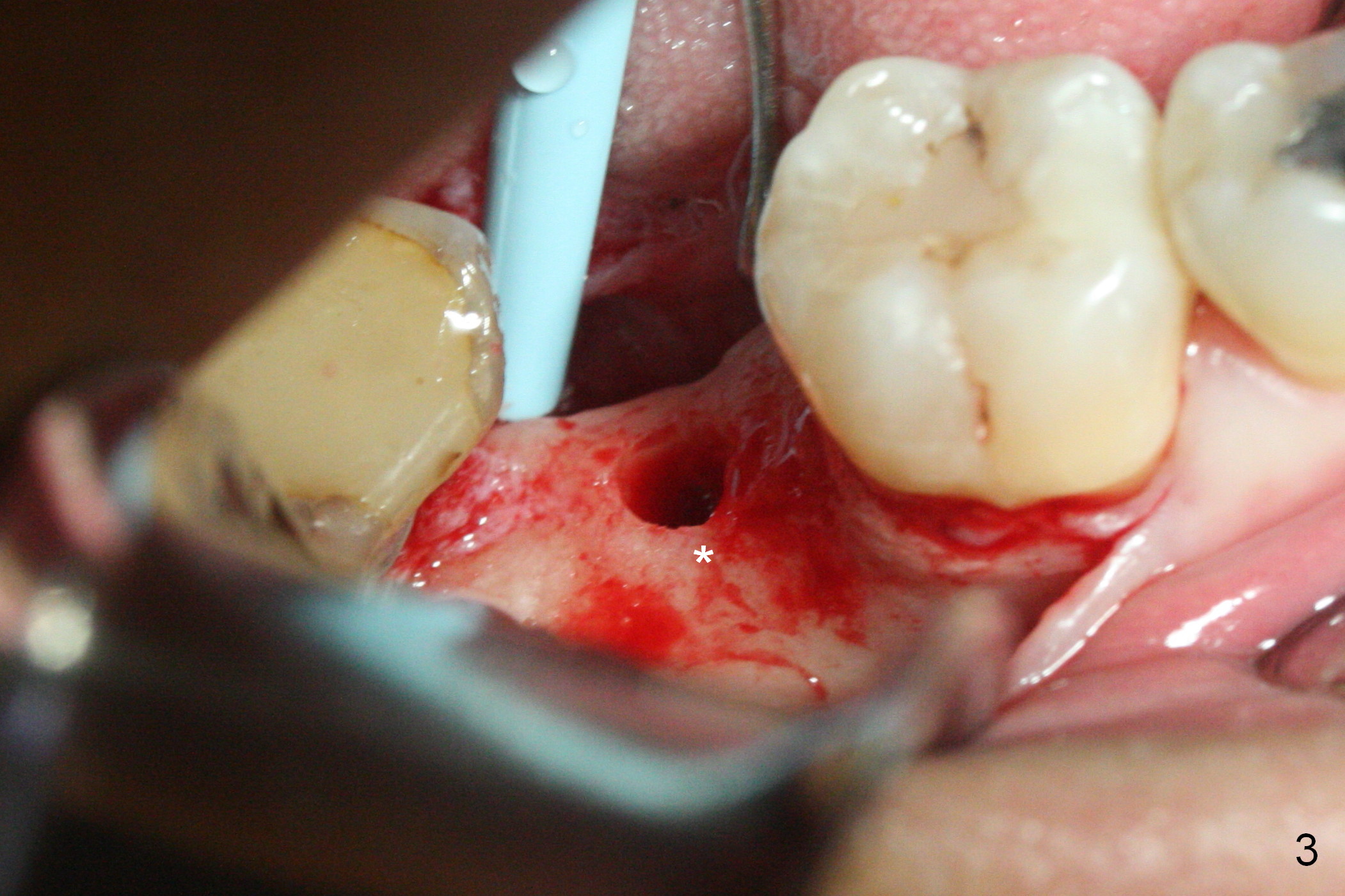
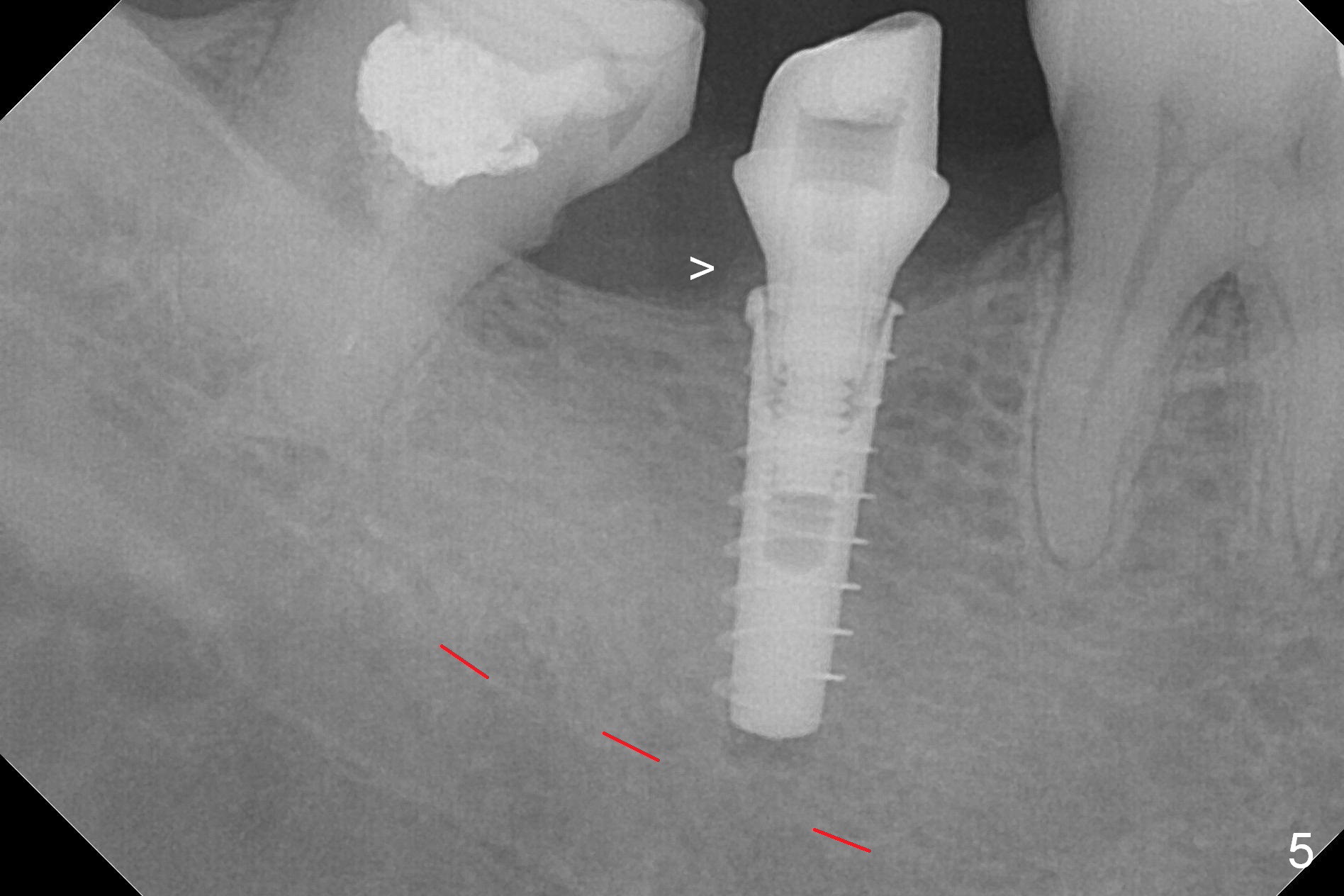
The ridge at #31 is also narrow buccolingually (Fig.1 *). After incision and 1.6 mm pilot drill, a guide pin with 7 mm length is inserted to confirm trajectory and depth; it appears that 11 mm osteotomy has enough clearance from the superior border of the Inferior Alveolar Canal (IAC, Fig.2 red dashed line). Following Marking Bur, 3.3 mm Magic Drill and final drill, the buccal plate seems to be thin (Fig.3 *). When a 4x11 mm IBS implant and 5x4(2) mm pair abutment are placed, the distal thread is exposed (Fig.4 >), the abutment contacts the opposing tooth (data not shown) and there is 2.7 mm clearance from IAC. After increasing the osteotomy 1-2 mm, the implant is placed deeper; the autogenous bone with Osteogen is placed around the plateau of the implant (Fig.5 >), particularly buccally, followed by collagen membrane. When sutures are placed around the abutment, the buccal ridge looks bulkier (Fig.6) than preop (Fig.1). It may remains so long term. The flap surgery makes it possible for simultaneous GBR and reduction in possibility of peri-implantitis. Last, periodontal dressing is applied.
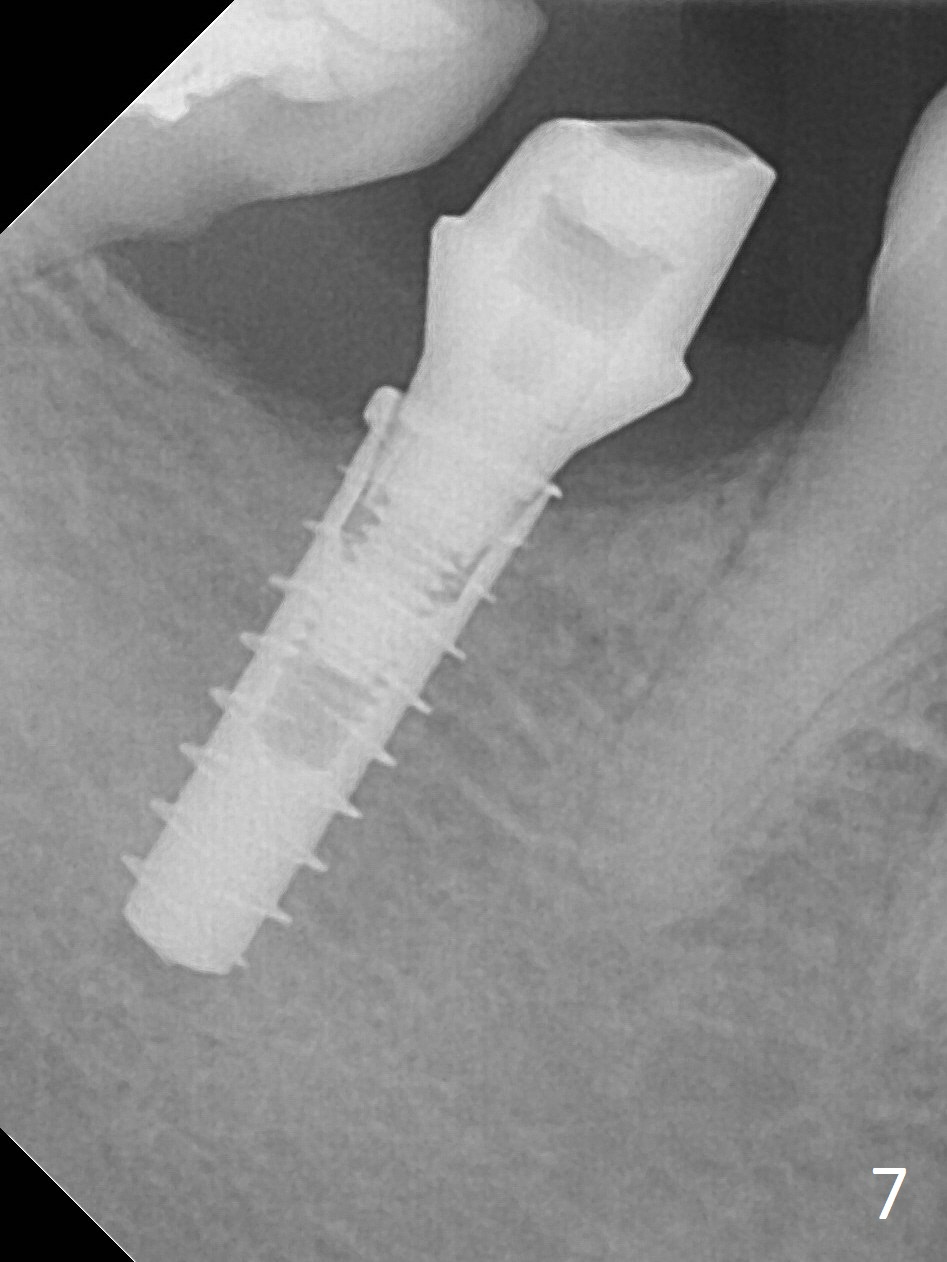
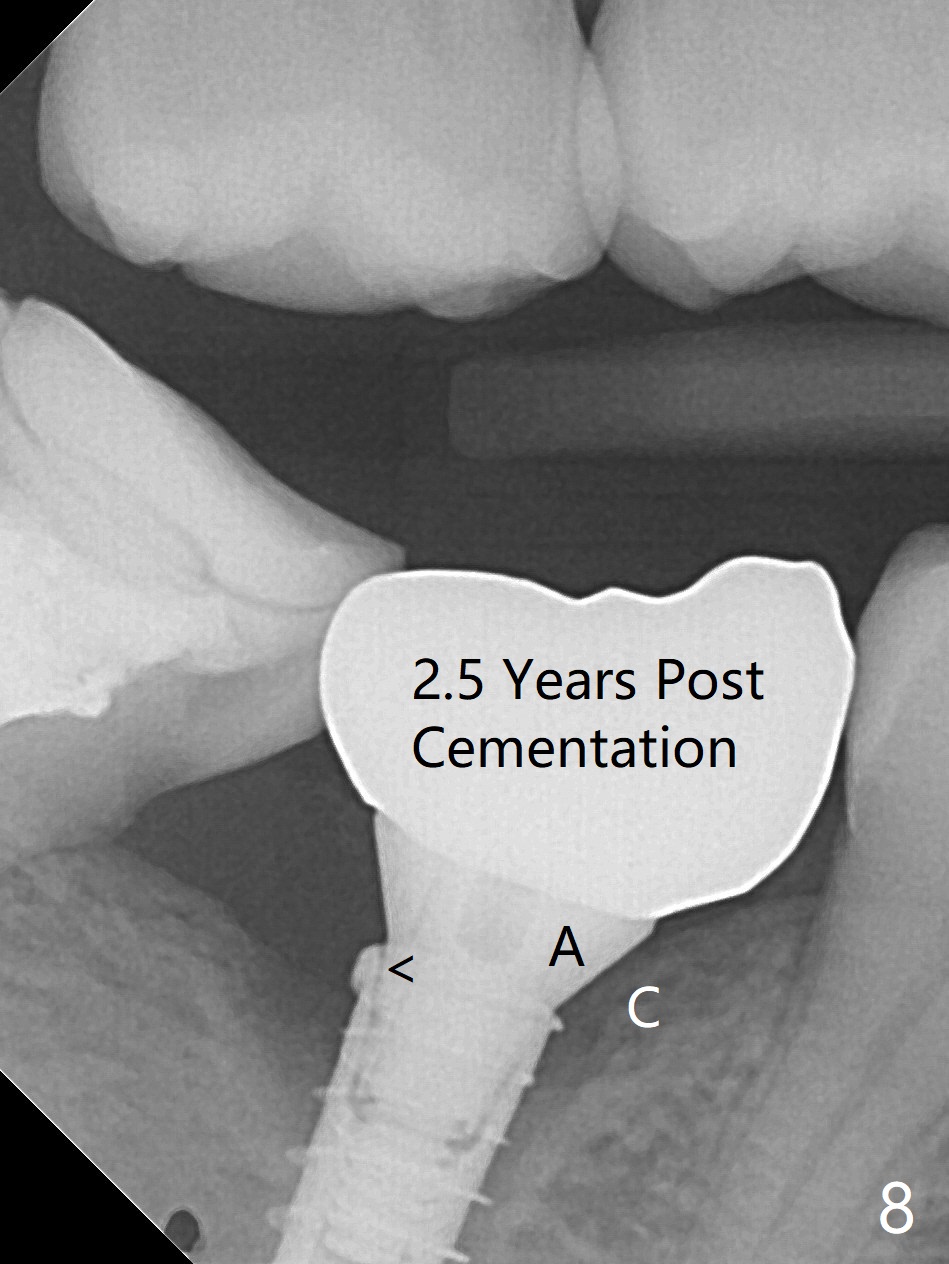
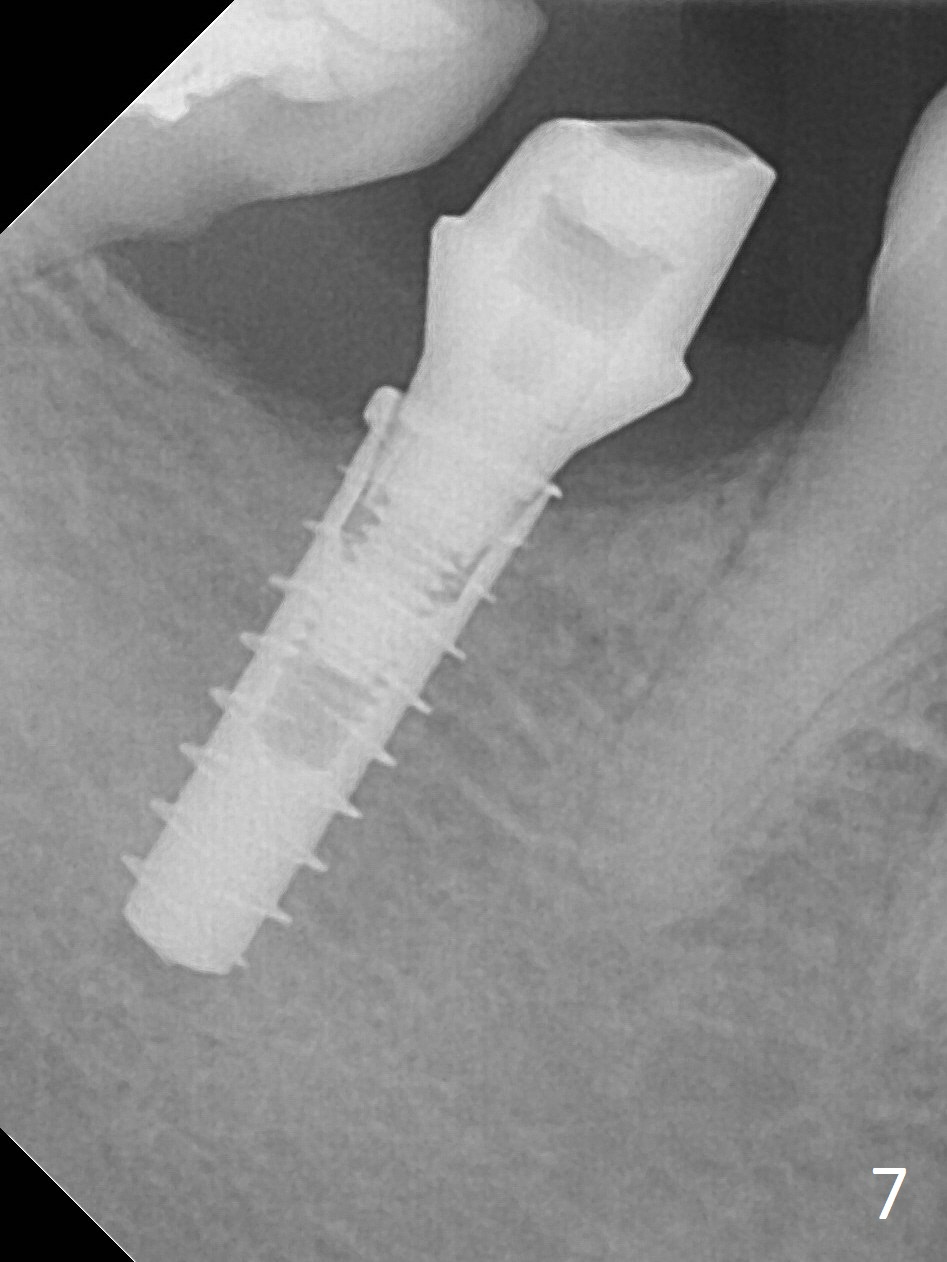
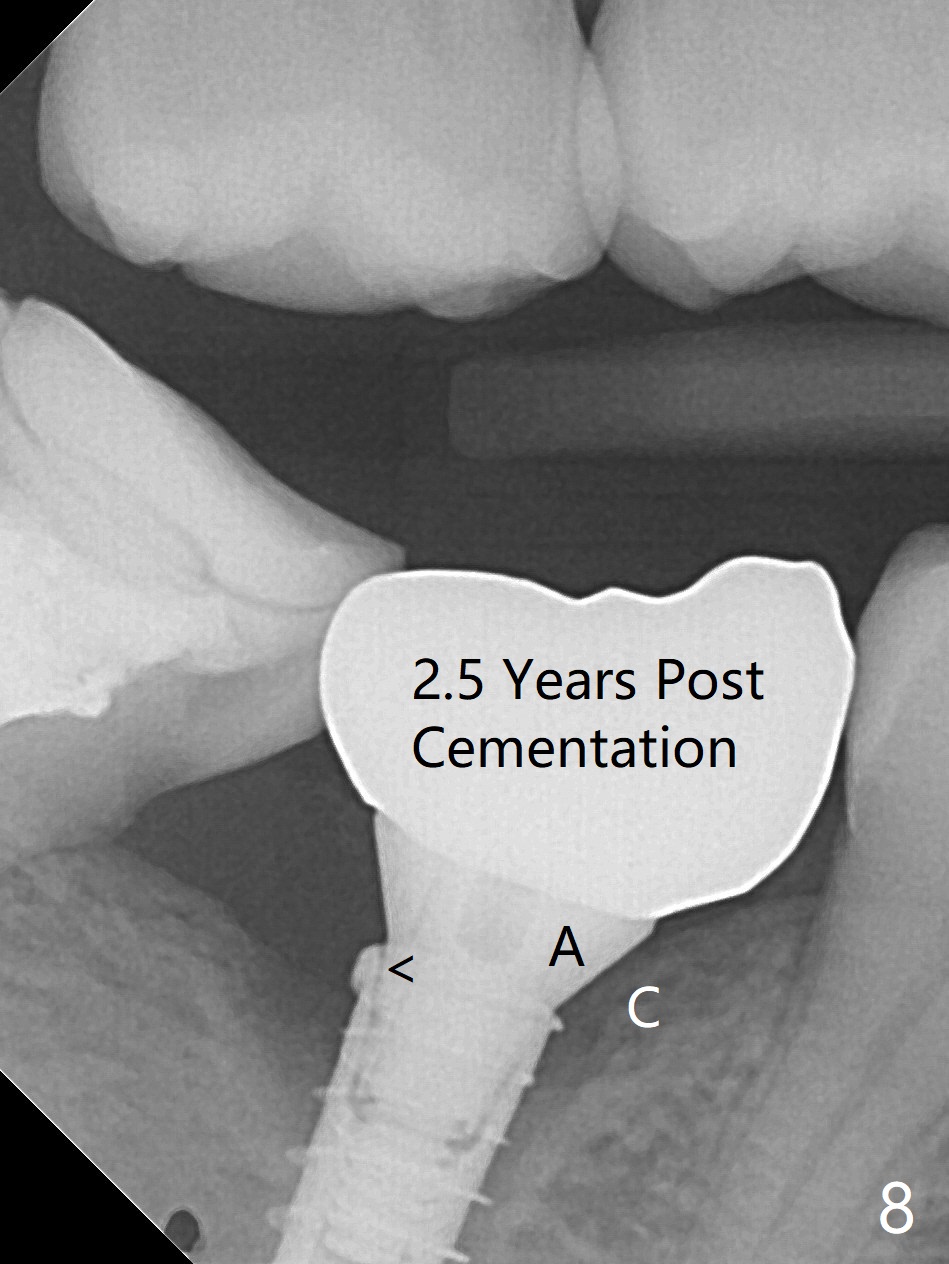
There is no apparent bone loss 4 months postop (Fig.7), related to the advantage of the narrow implant (less traumatic). The crown/abutment is loose 2.5 years post cementation due to incomplete abutment seating (Fig.8 < (no clearance between the abutment (A) and the mesial crest (C))). A 6x3 mm healing abutment is placed. When the patient returns, try in the smallest abutment with 2 mm cuff in the Planning Kit and place probably a 4x4(3) mm pair abutment from 5x4(2) mm existing one. Torque and take PA with sensor 1 to confirm seating before impression. Or use 5.5 mm profile drill before reseating the crown/abutment.
Lower Molar Immediate Implant
Xin Wei, DDS, PhD, MS 1st edition 01/19/2017, last revision 01/12/2020