








 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
Advantage of Immediate Implant
Once an osteotomy is formed in a healed site, the trajectory is difficulty to change. In contrast, the trajectory of immediate implant is still changeable post osteotomy. This is the advantage of immediate implant.
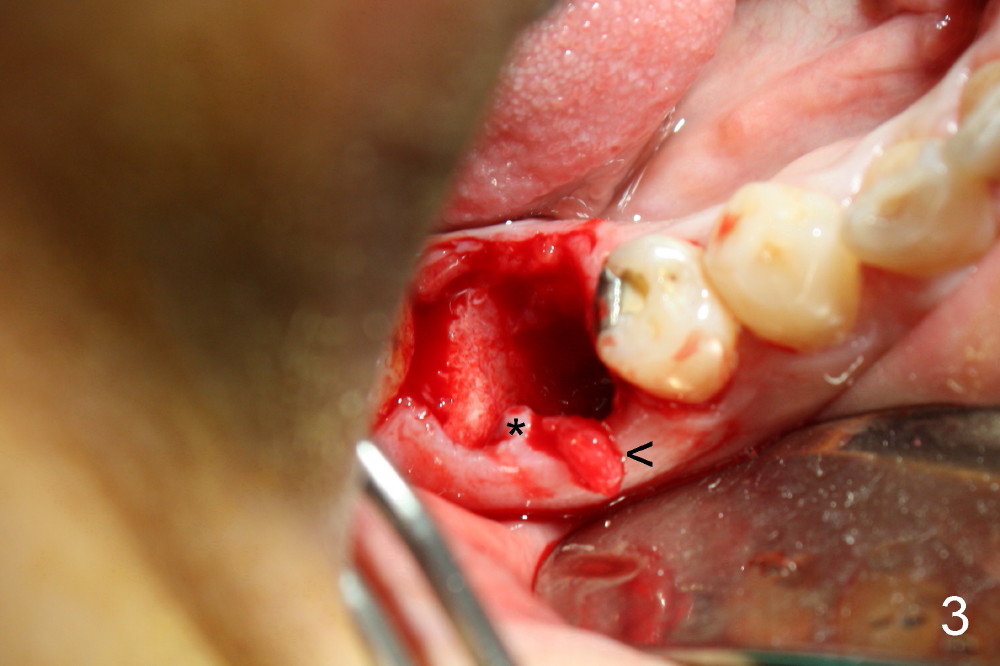
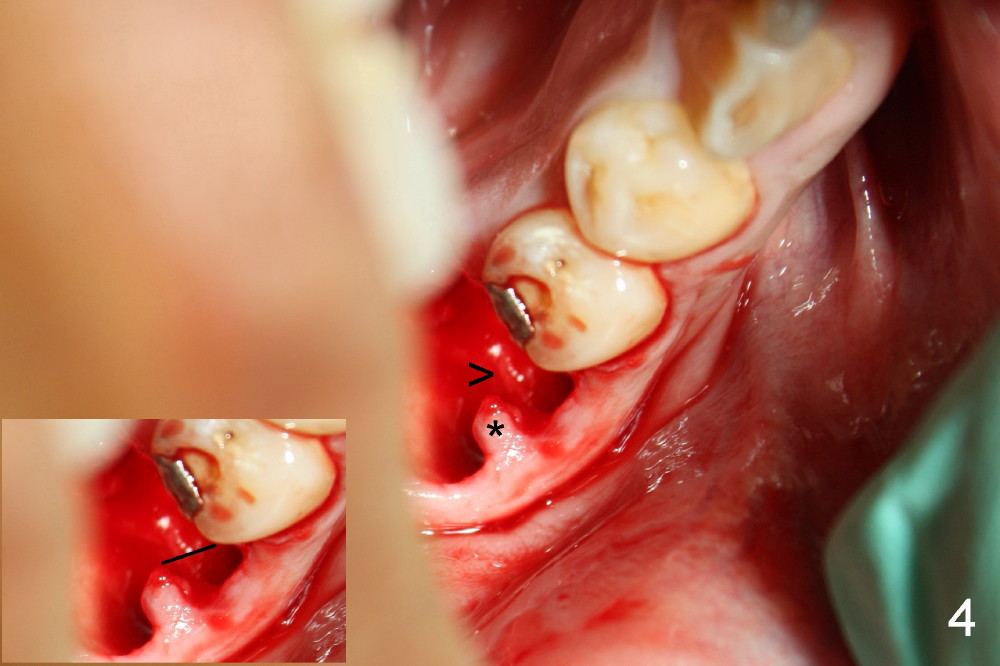
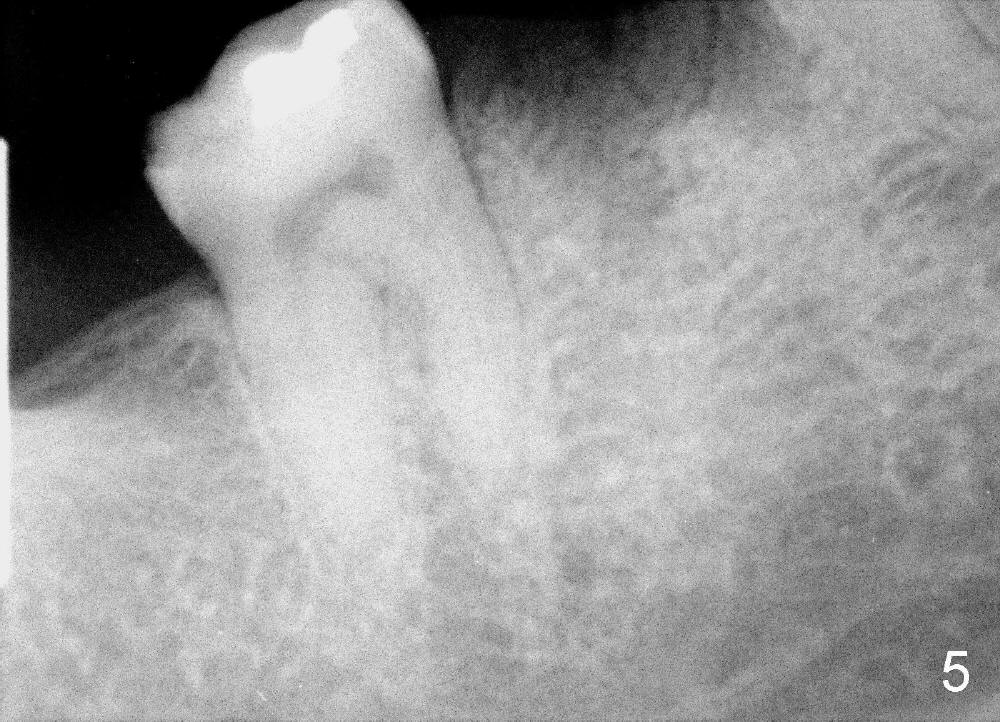
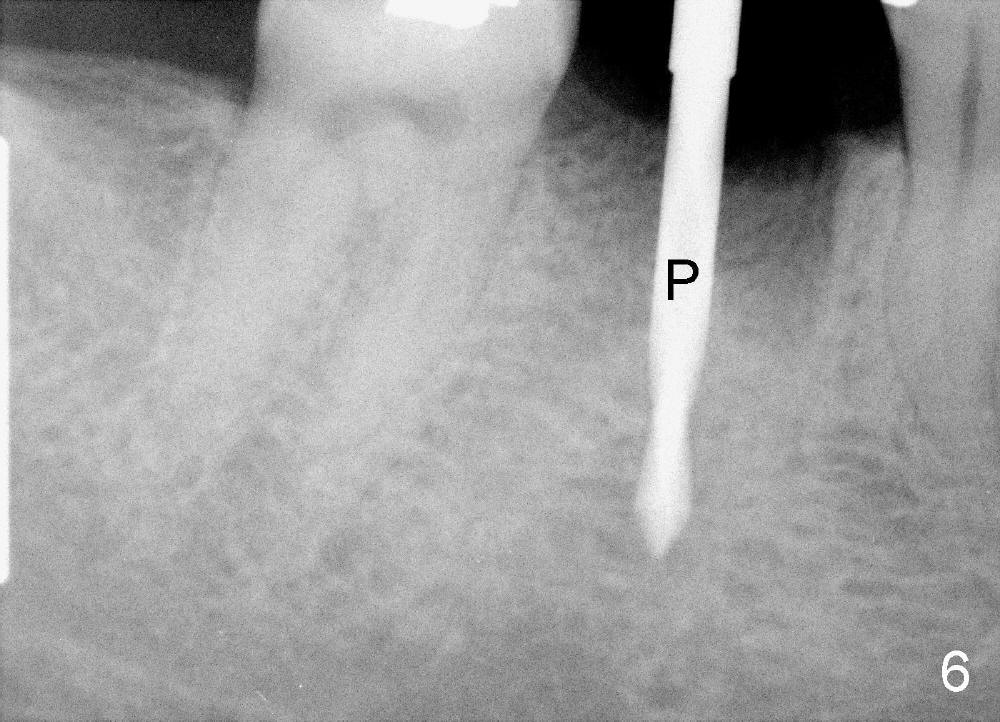
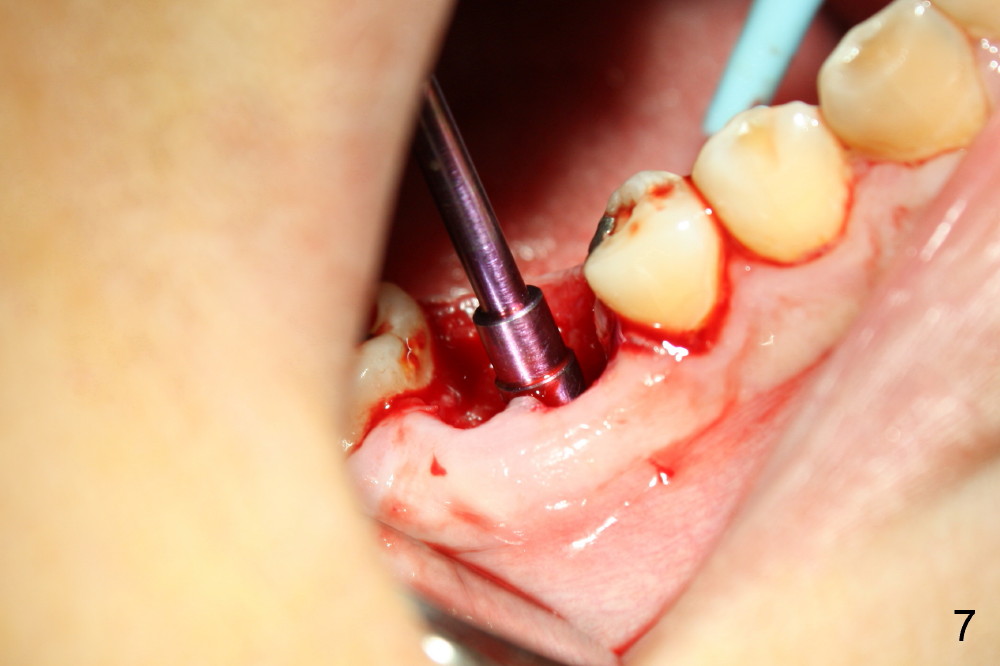
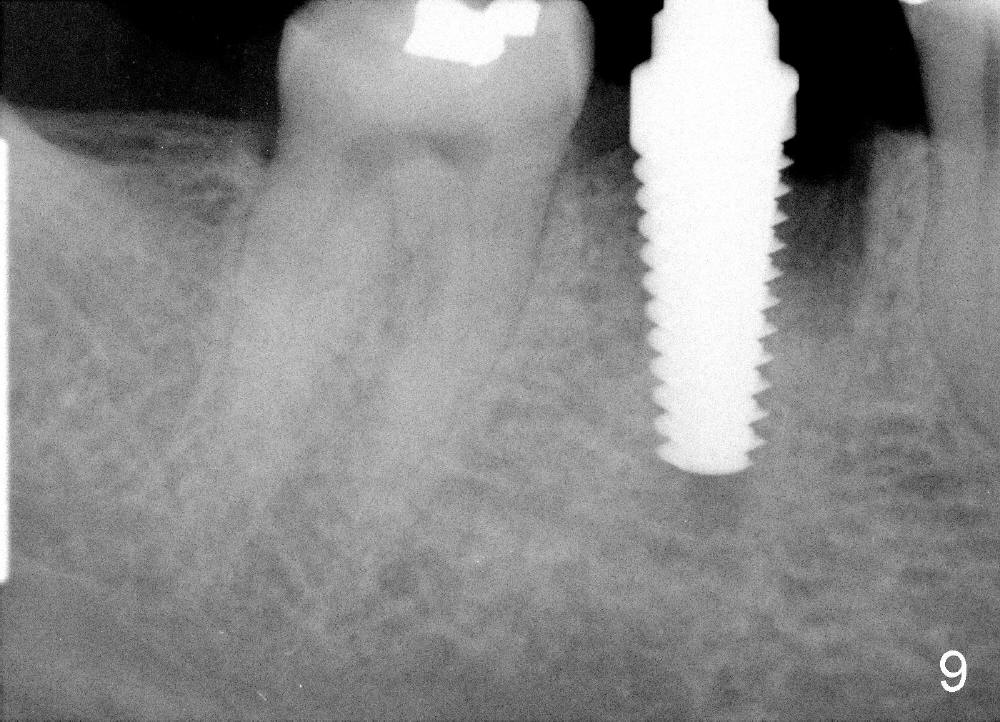
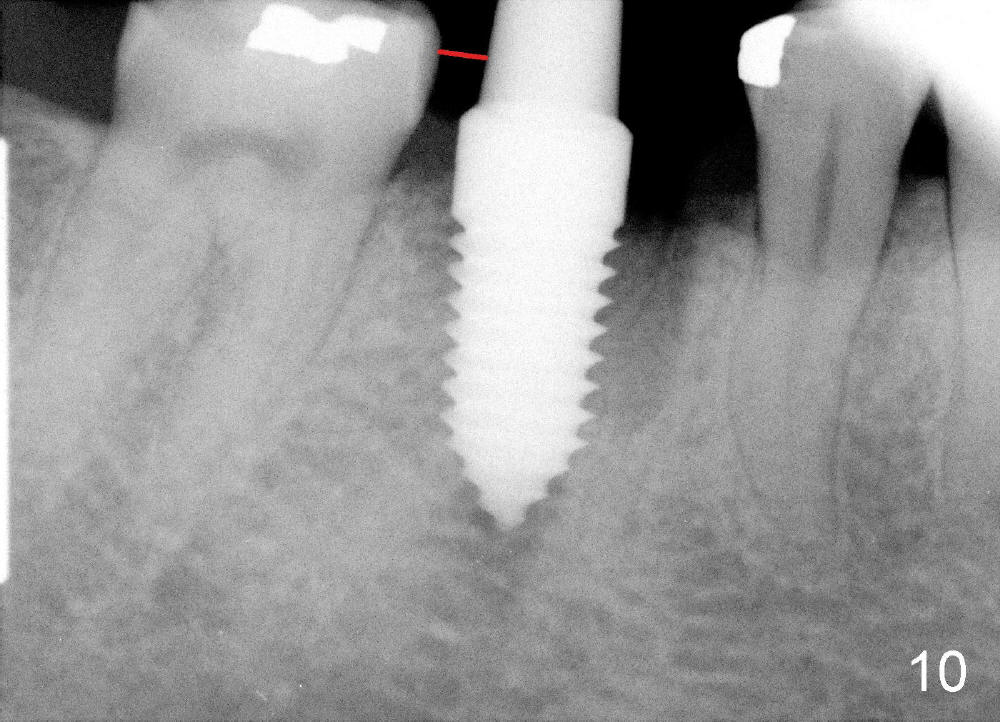
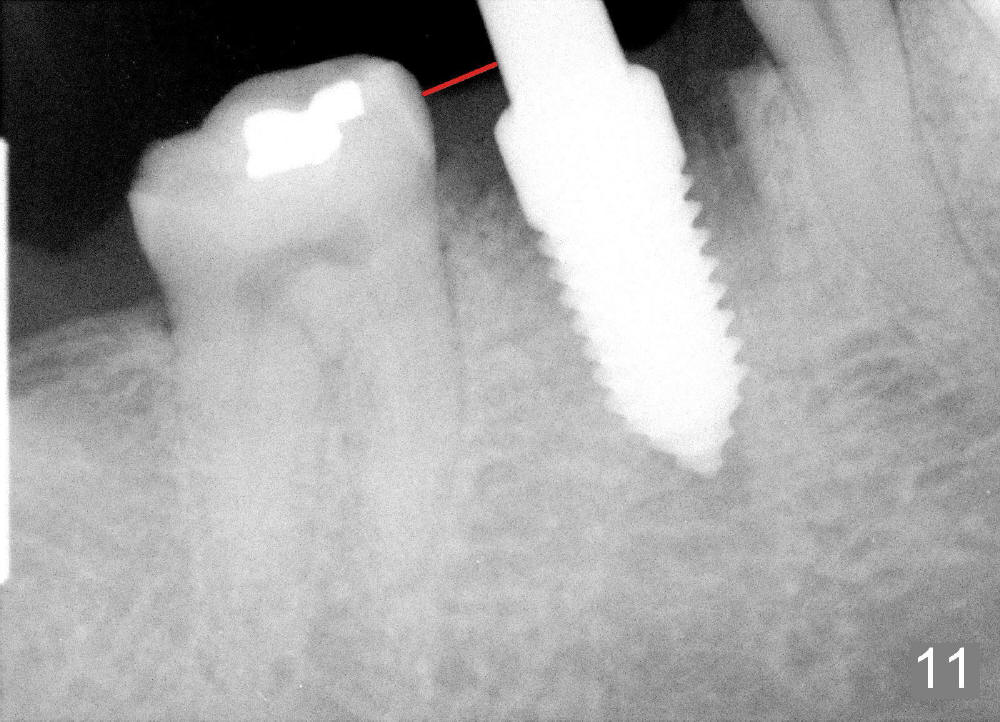
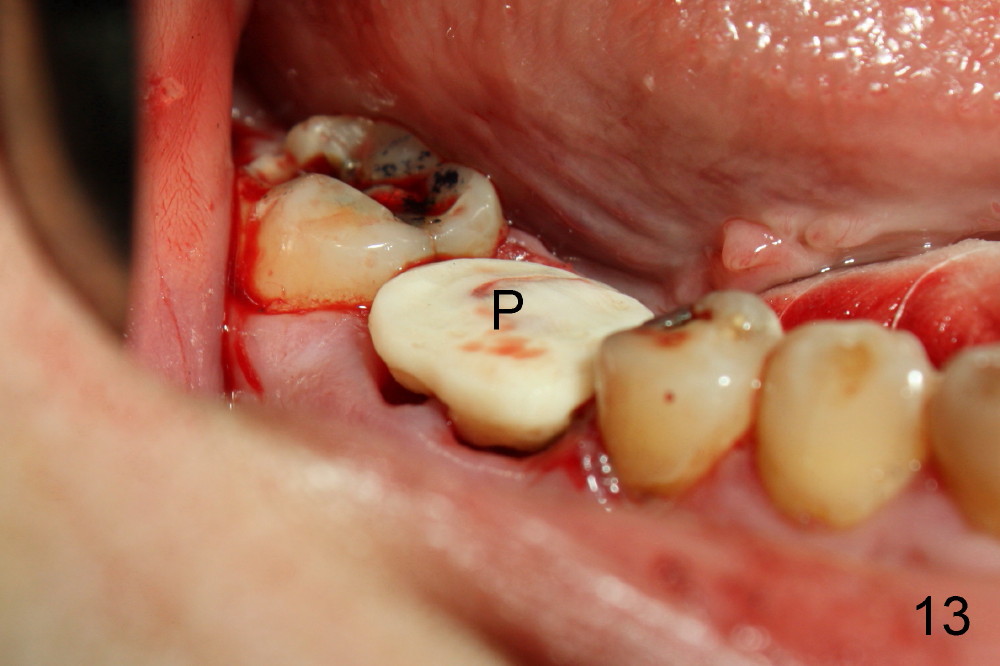
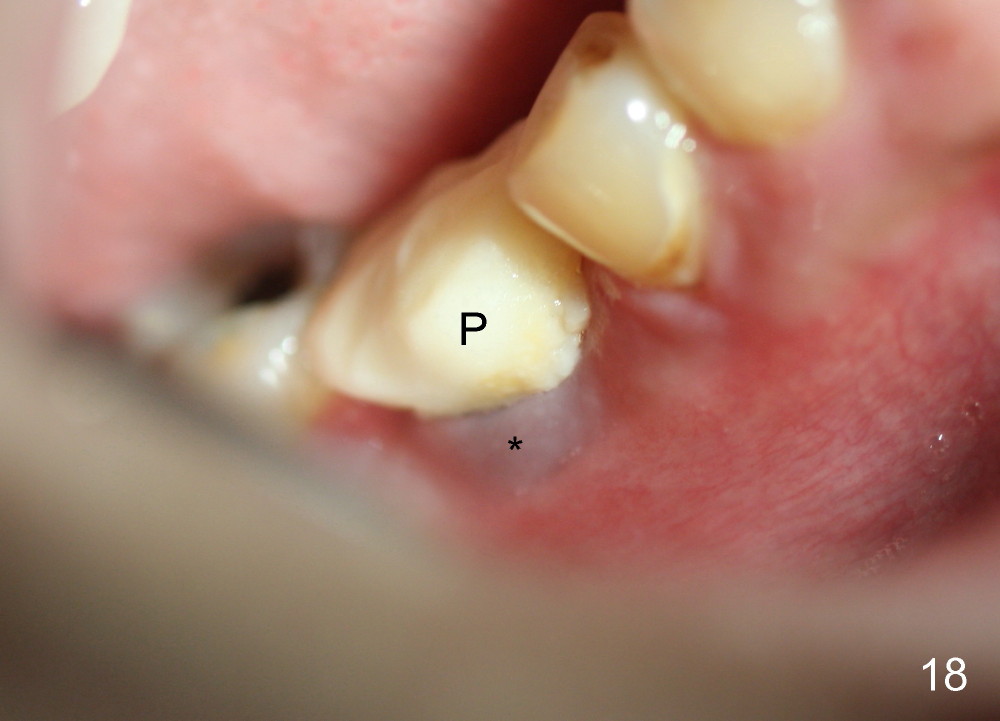
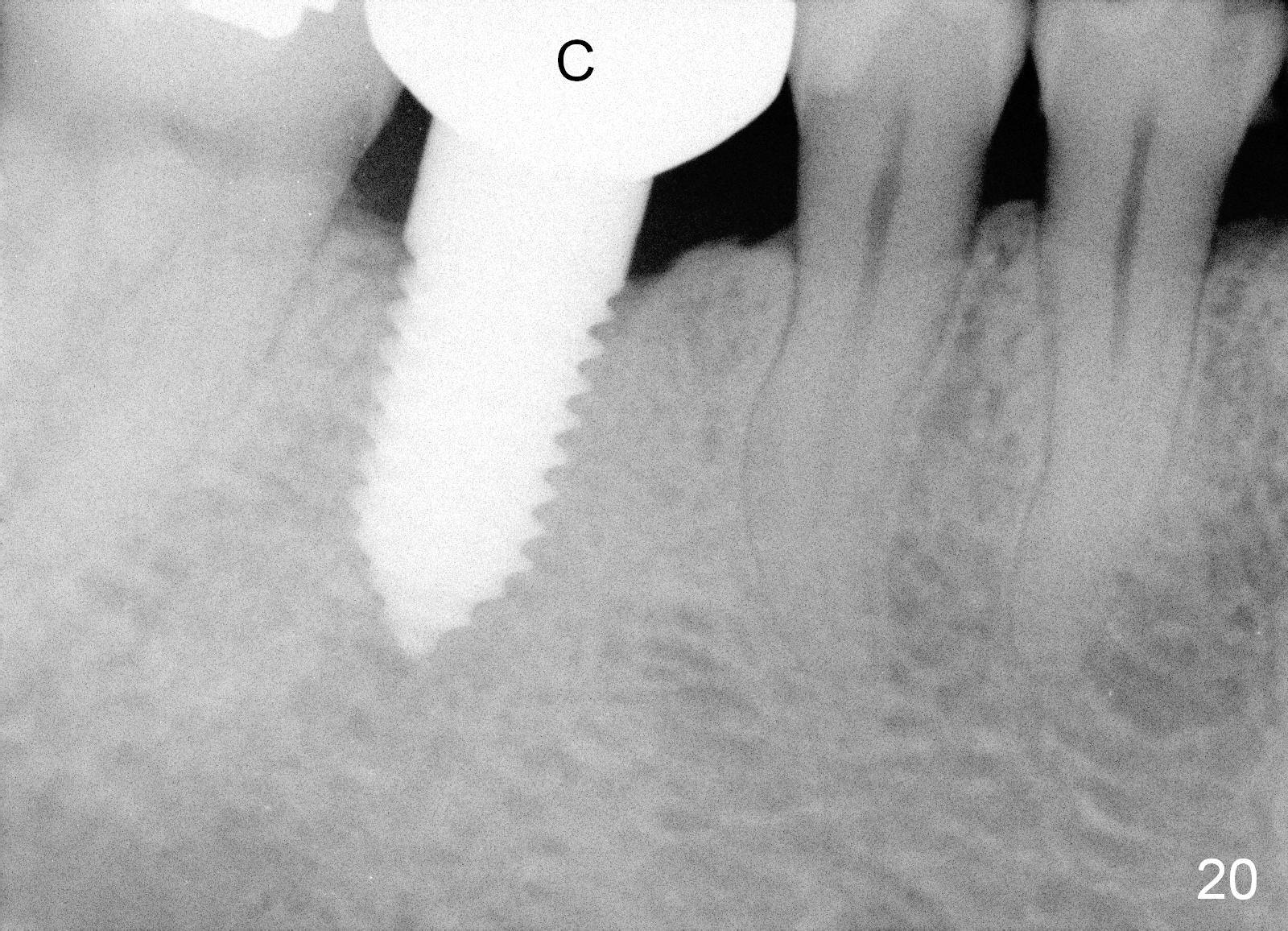
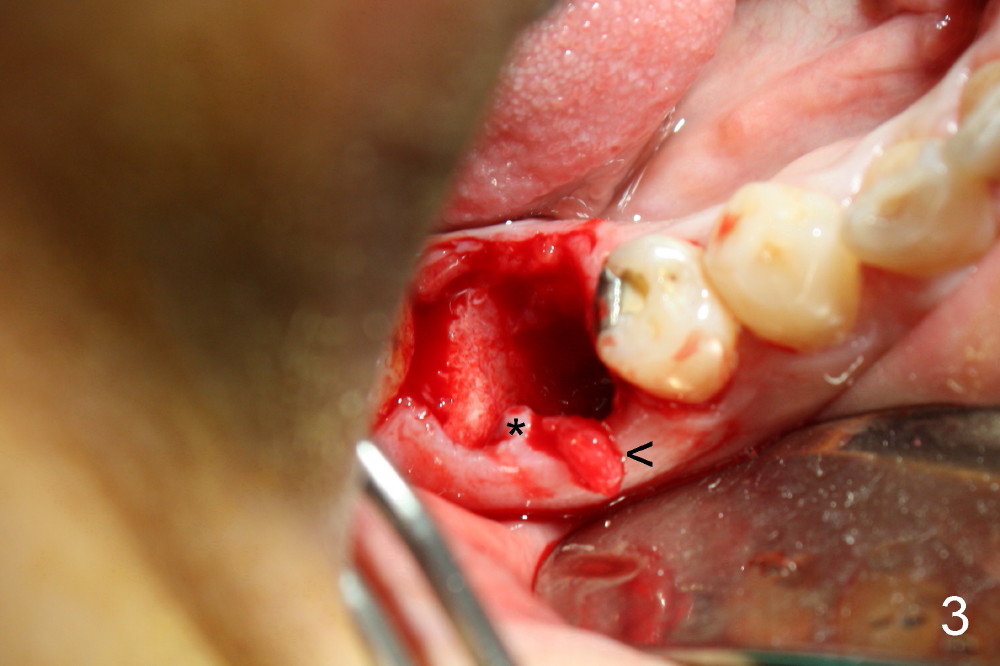
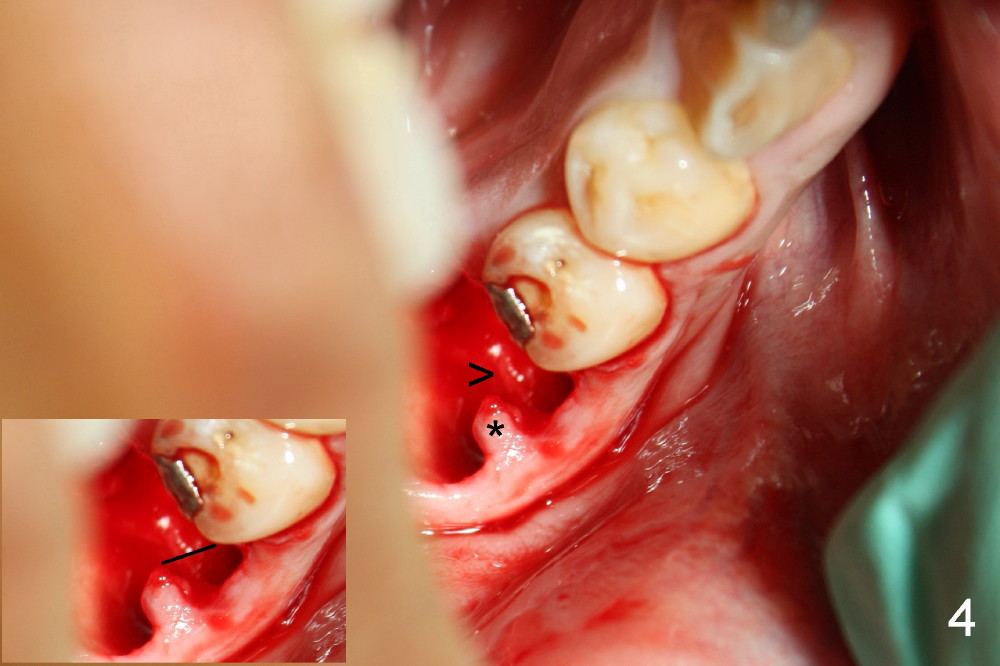
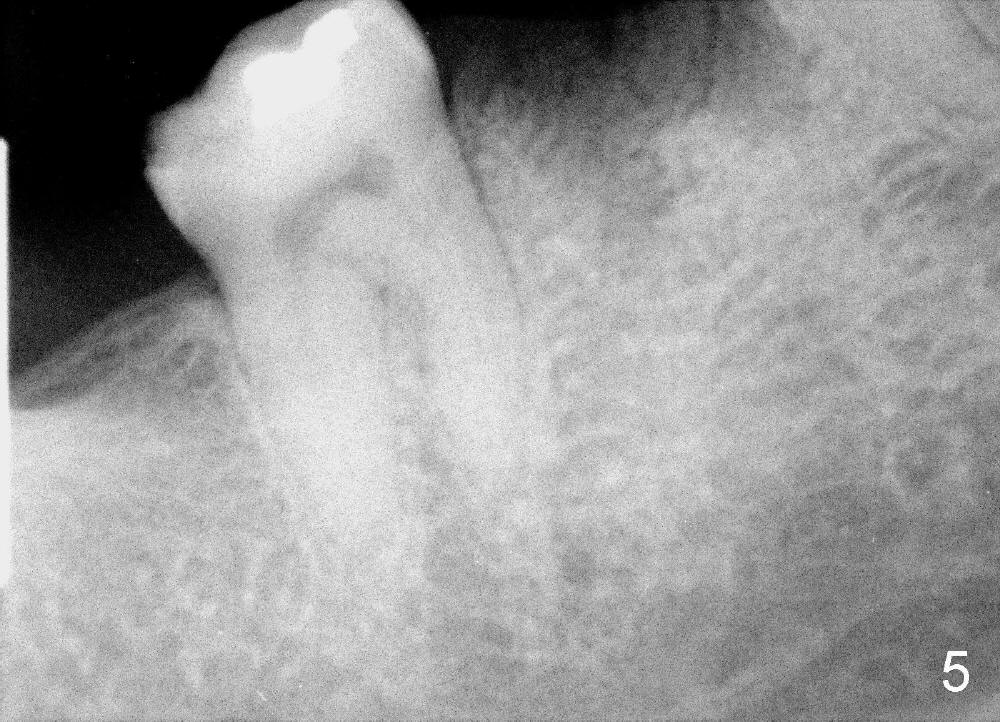
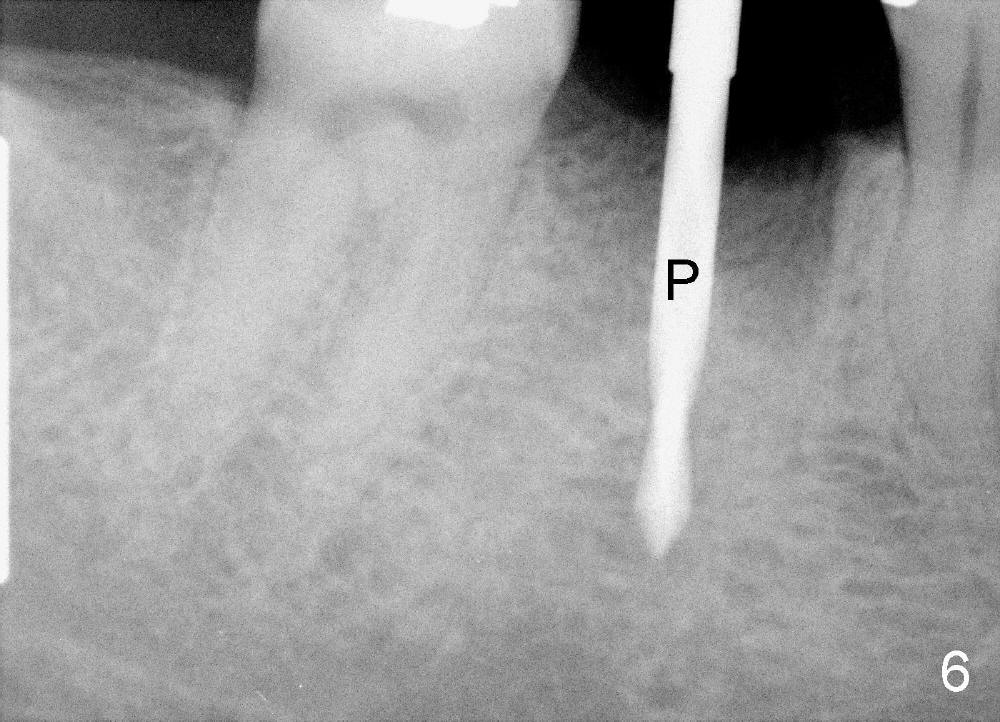
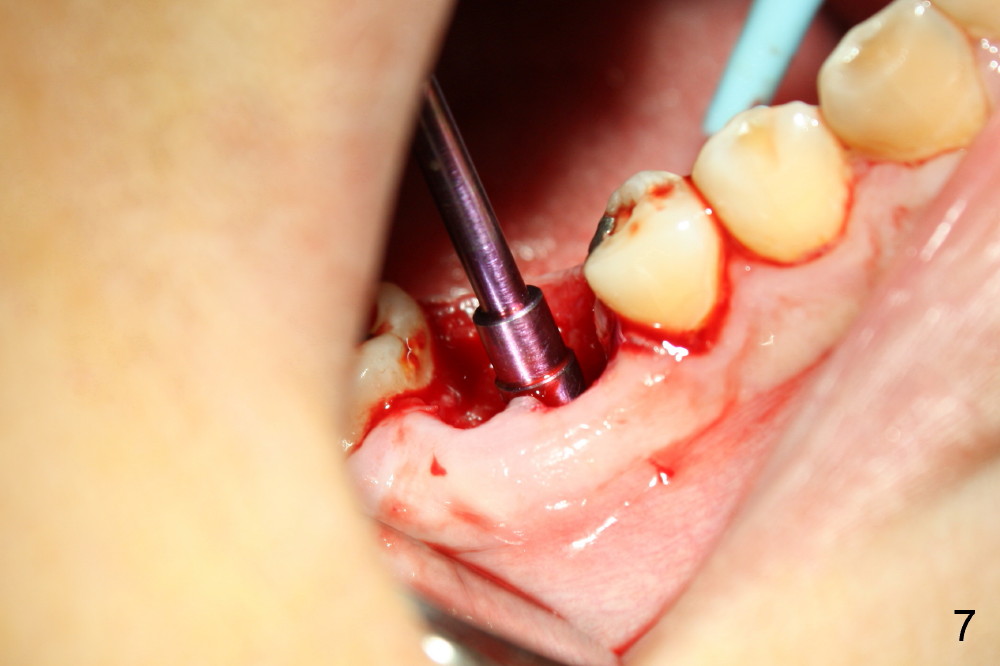
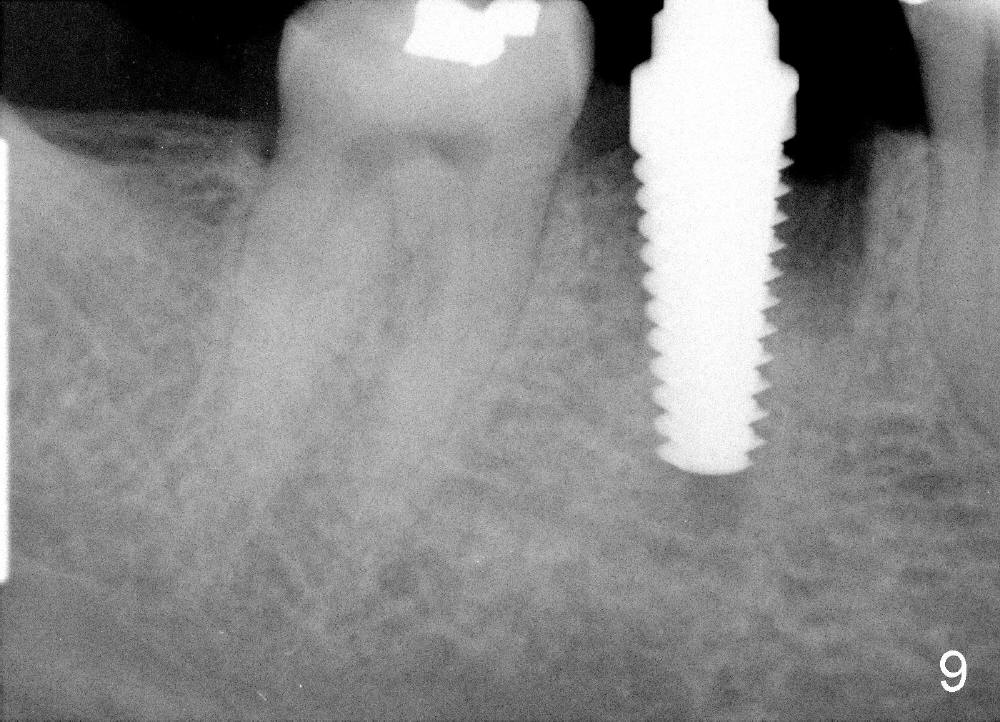
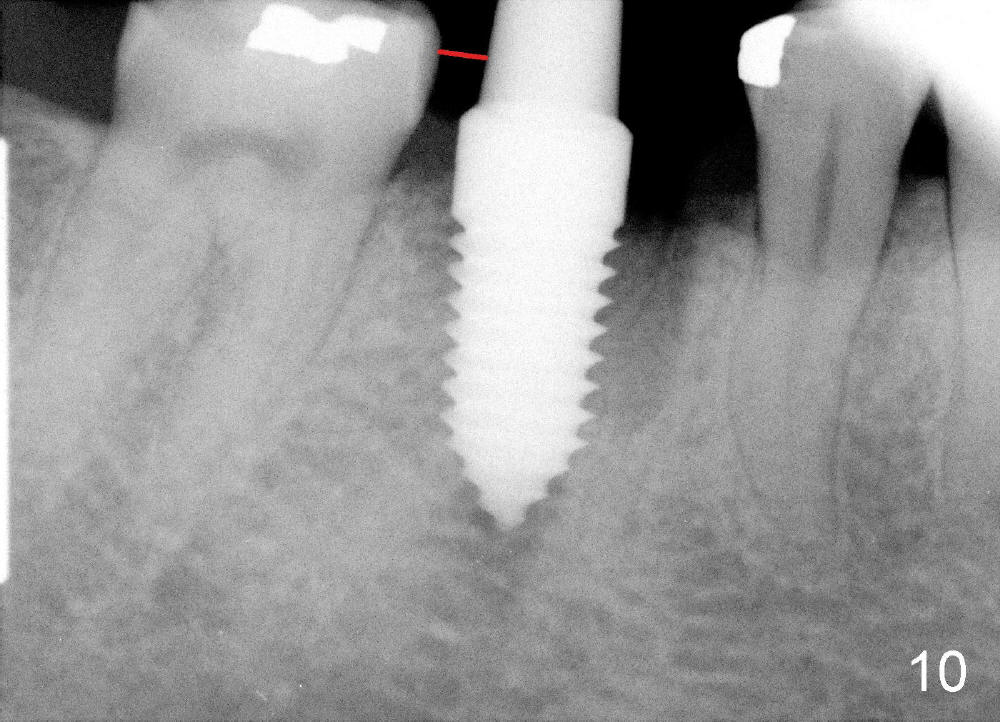
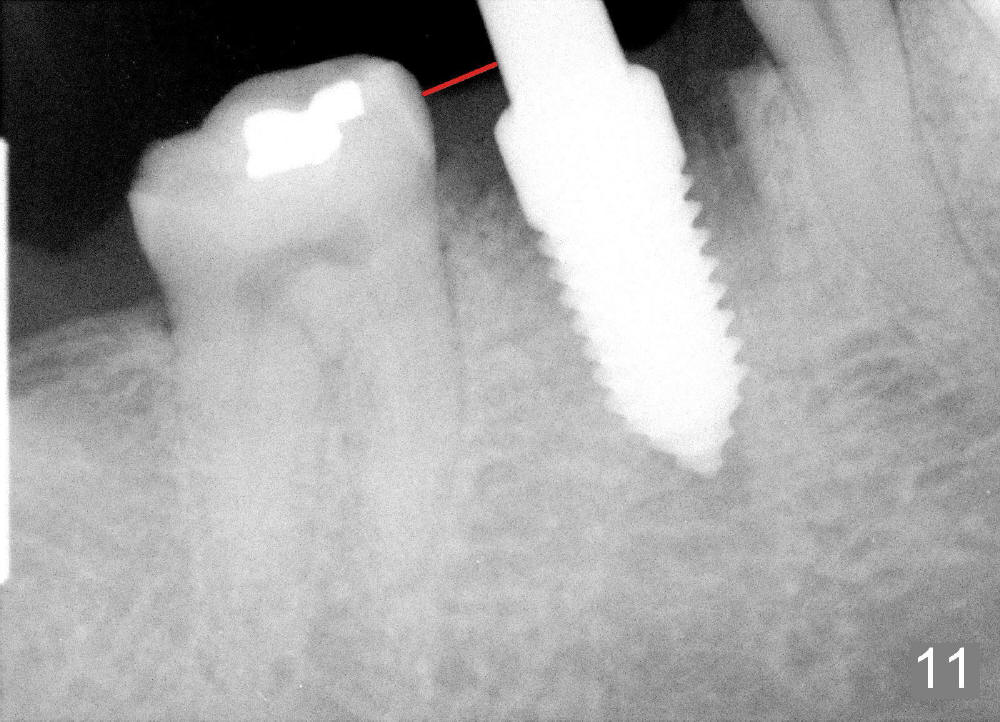
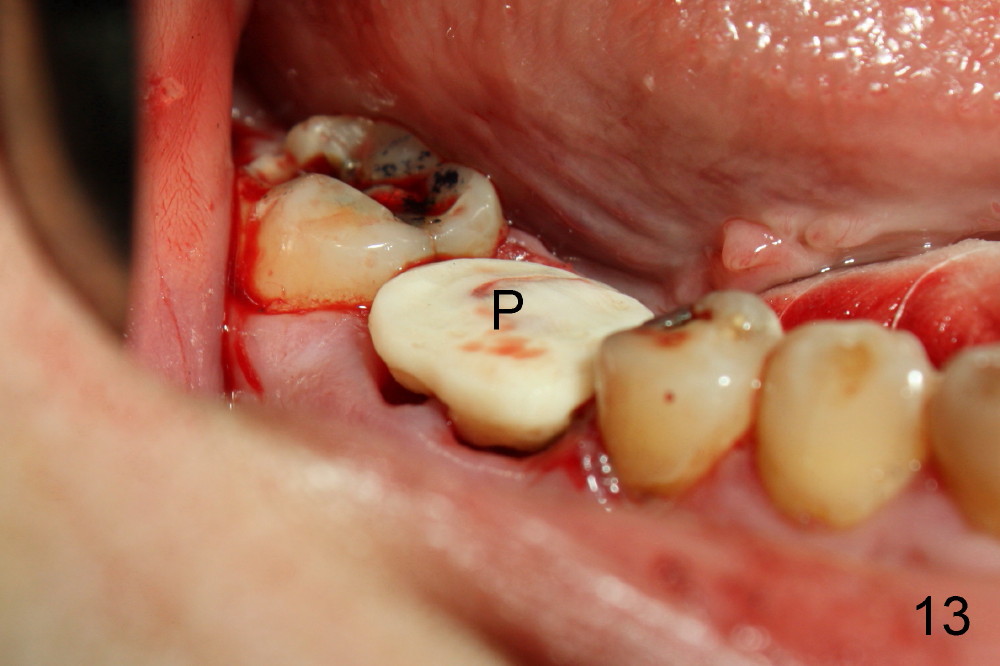
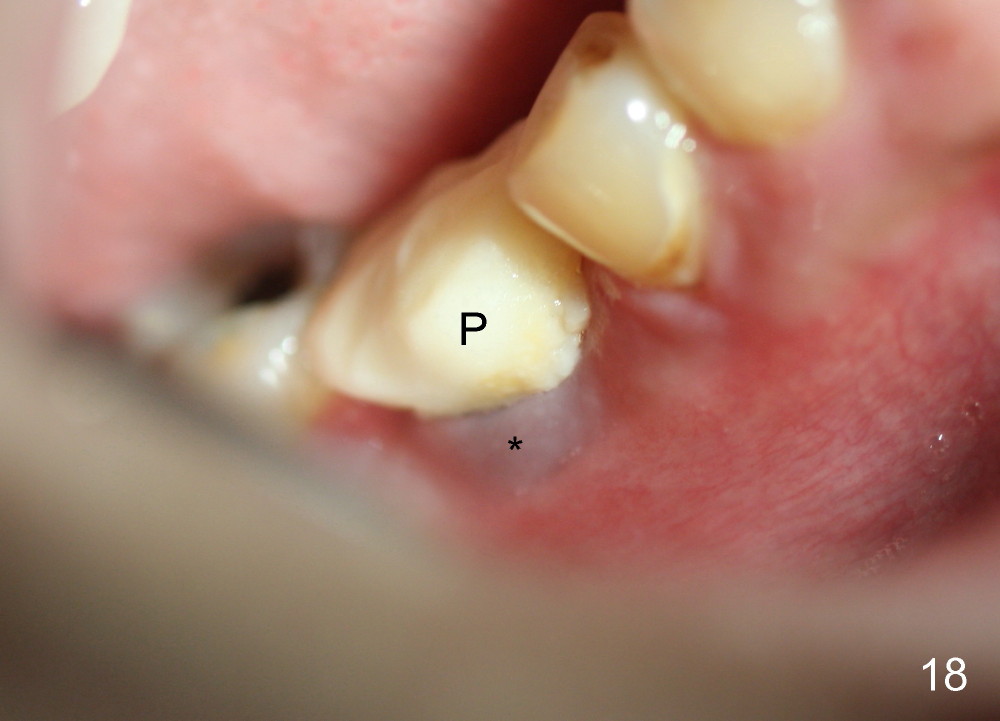
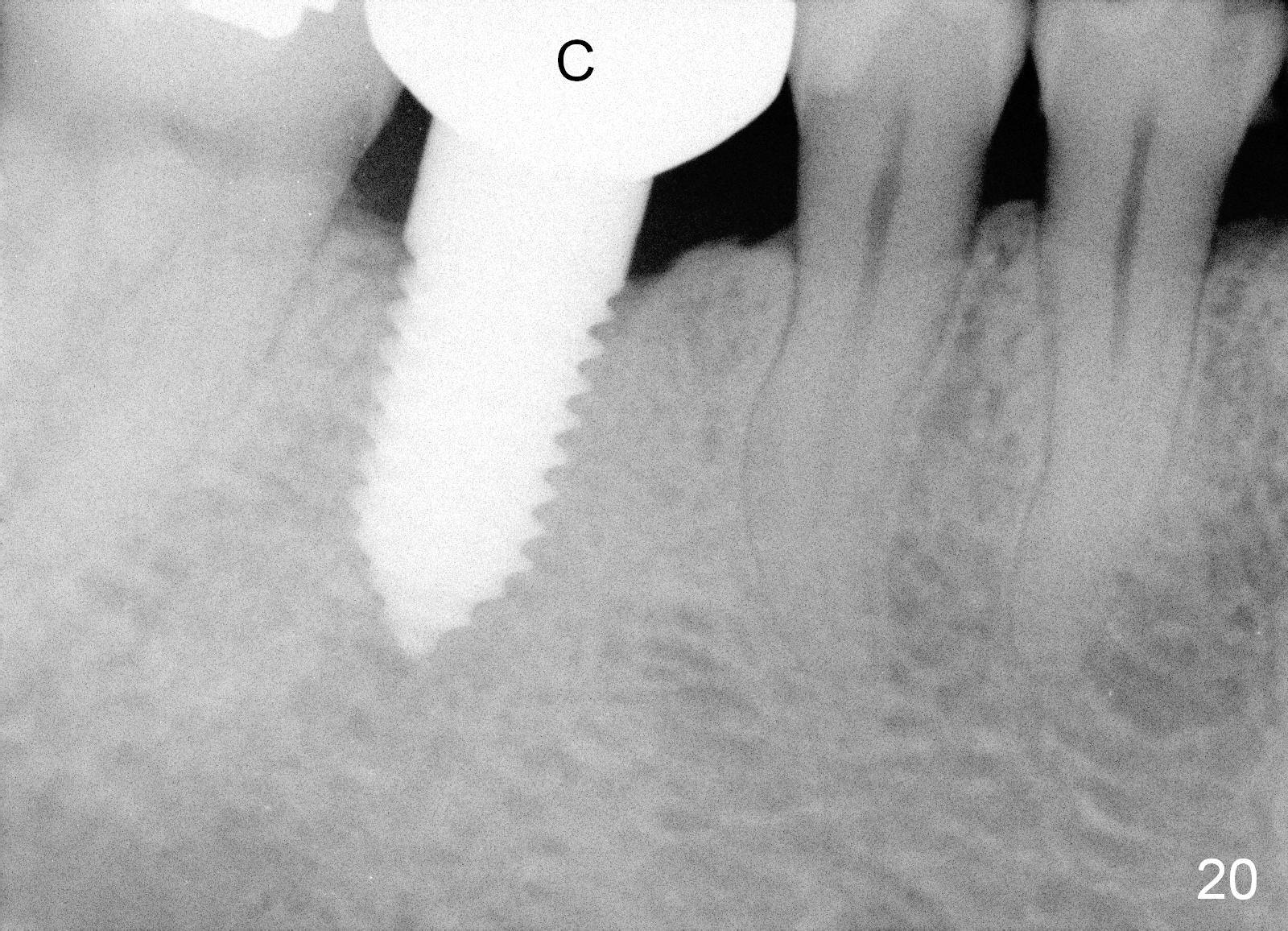
A 38-year-old lady agrees to have implant placement 7 years after loss of the crown of the lower right first molar (Fig.1,2). When the tooth is extracted, the septum is found to be low (Fig.3,4). To confirm it, a PA is taken (Fig.5). To initiate an osteotomy in the septum, it is trans-sectioned with thin osteotomes as shown in Fig.4 insert (black line). A 2 mm pilot drill is placed in the septum (Fig.6: P). The osteotomy is enlarged by 2.5-4.0 mm reamers (Fig.7,8), followed by insertion of 6x17 mm tapered tap at the depth 14 mm (Fig.9). The osteotomy is further enlarged by 4.5 and 5.0 mm reamers. A 6.0x14 mm one piece implant is placed initially. The trajectory is not ideal. A 6.0x14 mm one piece implant is placed initially. The trajectory is not ideal. The implant is removed from the osteotomy partially and reinserted with improved trajectory (Fig.11, compare to Fig.10 (red line)). Primary stability is high. There is not much bone mesiodistally so that the trajectory is easily changed in that direction. After abutment preparation, mixture of autogenous bone (harvested from reamers) and allograft is placed in the residual mesial and distal sockets (Fig.12). To contain the bone graft, an immediate provisional is placed (Fig.13 P). The occlusal plane of the provisional is significantly lower than that of the adjacent teeth to avoid micromovement of the implant. The patient is advised to eat soft food on the left side. Six days postop, the patient returns for prophy. The provisional is removed; the bone graft appears to be incorporating into the socket (Fig.14). After recementation, the provisional remains in place for 3.5 months; PA shows increased bone density in the mesial and distal sockets (Fig.15, compare to Fig.5,11). Due to insurance coverage, the patient defers fabrication of definitive restoration for at least 7 months. The immediate provisional is finally lost 8.5 months postop: the gingiva attaches to the 1-piece implant (Fig.16), while the density of the mesial socket increases (Fig.17 *) with formation of the cortex (lamina dura) coronally (v). Before the provisional (Fig.18 P) is removed for cementation of the definitive restoration, black shadow (*) is noted over the buccal gingiva. It is partially due to buccal placement (Fig.19) and partially due to buccal atrophy over a period of 10.5 months postop. How to prevent buccal placement? Positioning the first pilot drill in the septum buccolingually is a key. Eleven months post crown (Fig.20 C) cementation, the black shadow remains, but there is no tenderness. If the implant threads are immediately underneath the periosteum, there is tenderness.
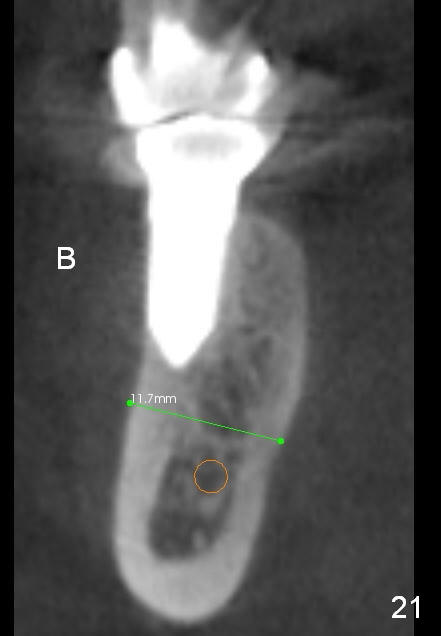
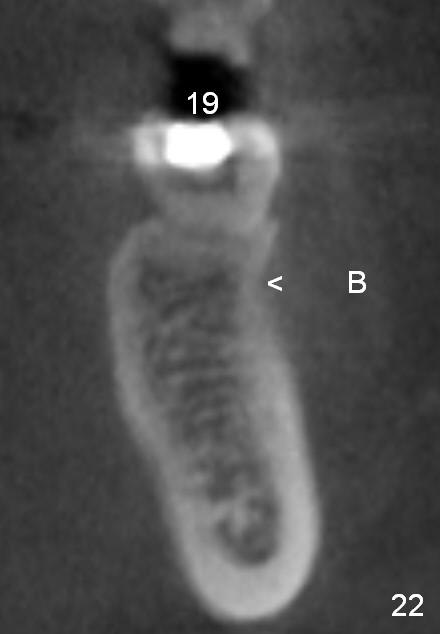
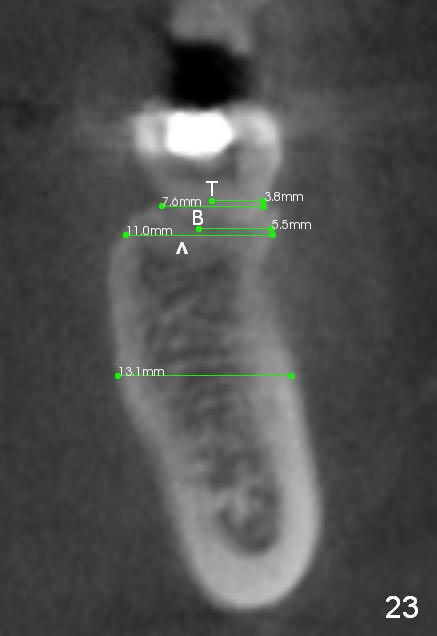
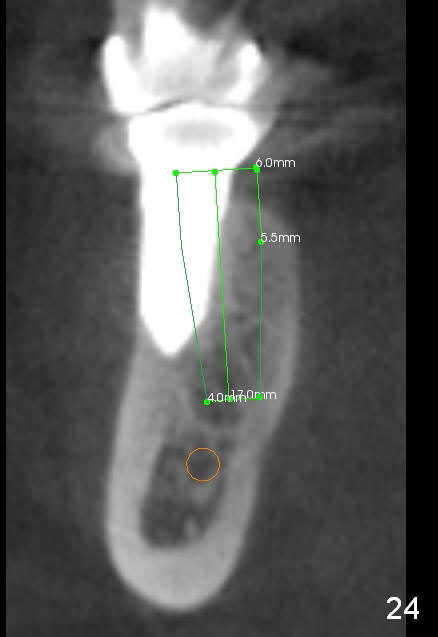
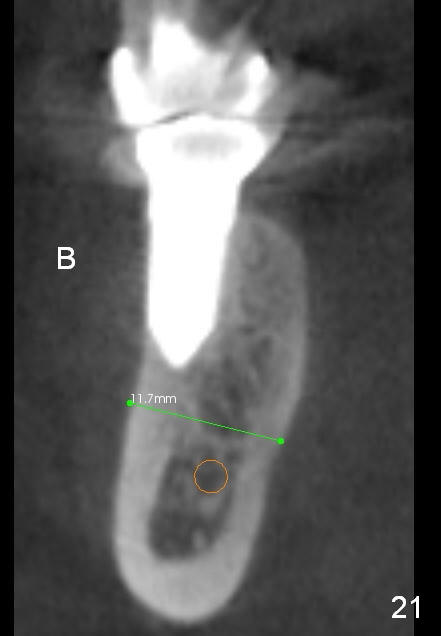
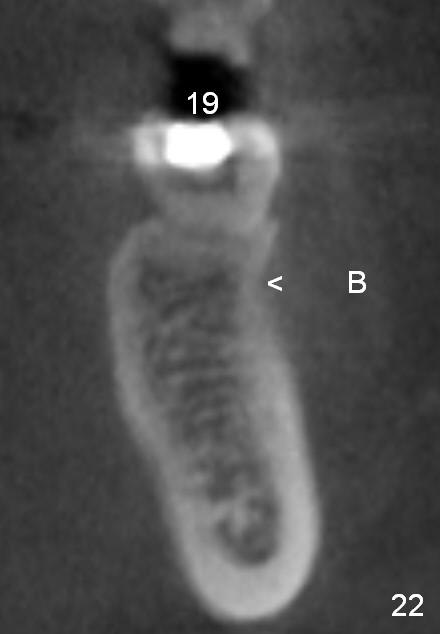
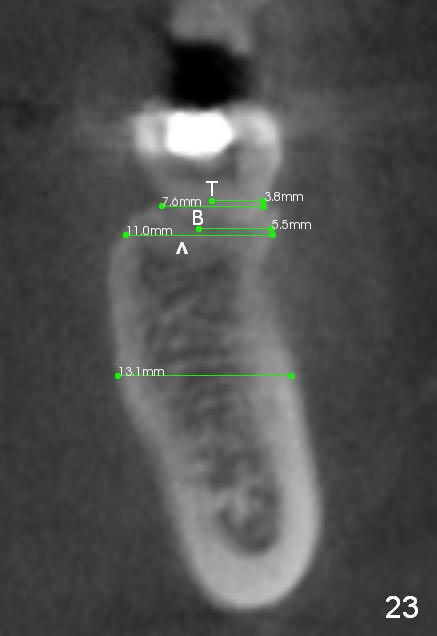
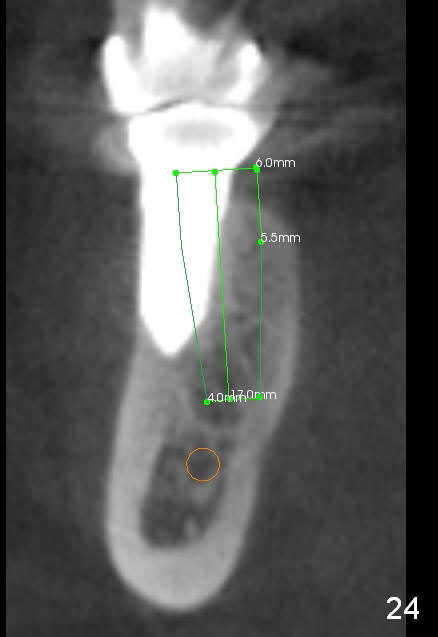
CBCT taken 15 months post cementation shows that the implant is buccally placed (Fig.21 B), associated with possible postop buccal plate resorption (as compared to Fig.23 (coronal section of the site of #19). The buccal plate is not only thinner than the lingual one, but also concave (Fig.22 <). The tooth center (i.e., septum; Fig.23 T) is more buccally located than the center of the basal bone (B). Considering the denser bone lingually, the initial osteotomy should be more lingually (^). If the implant develops infection, it will be replaced by a more lingually placed implant (Fig.24 green).
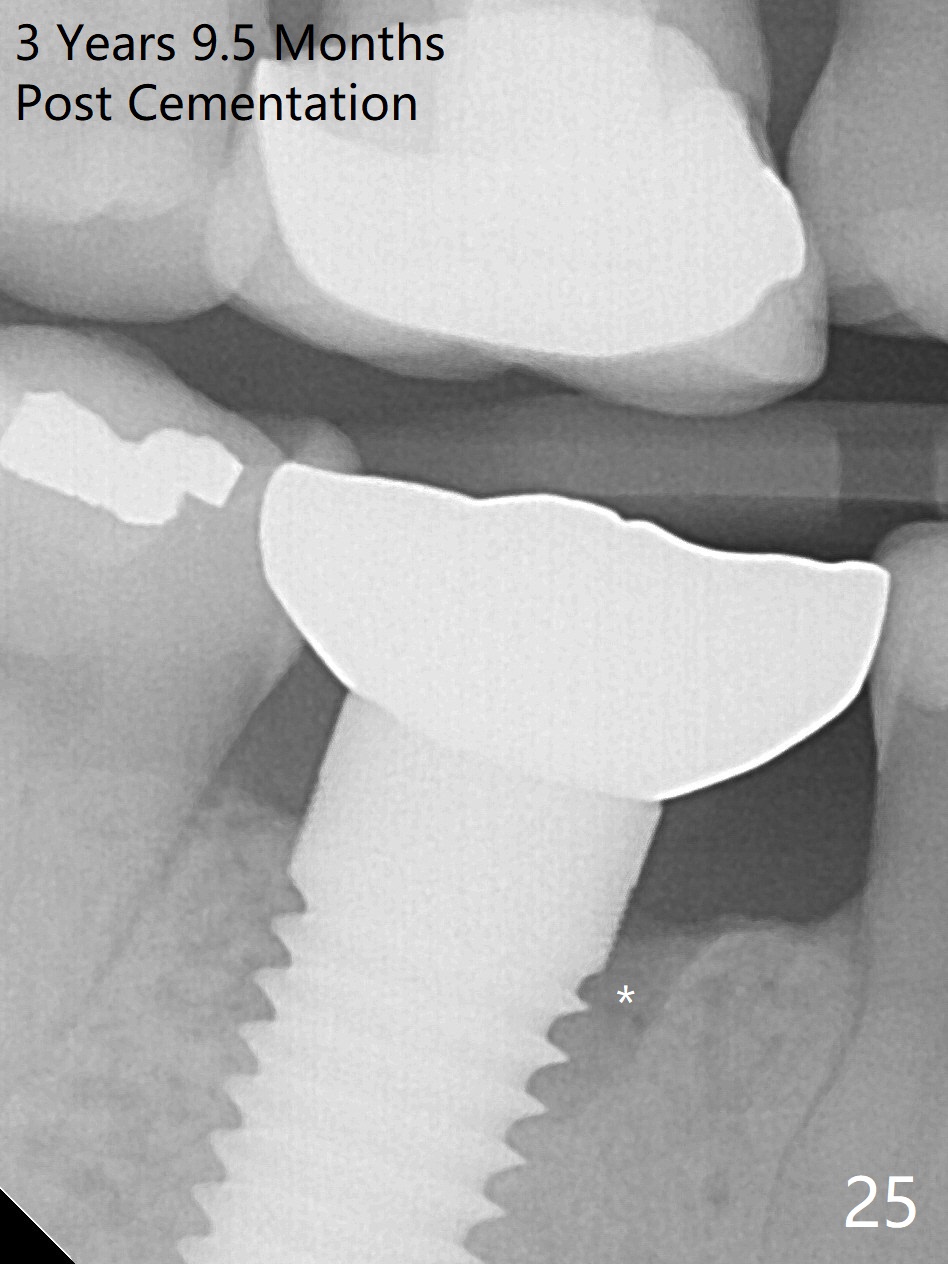
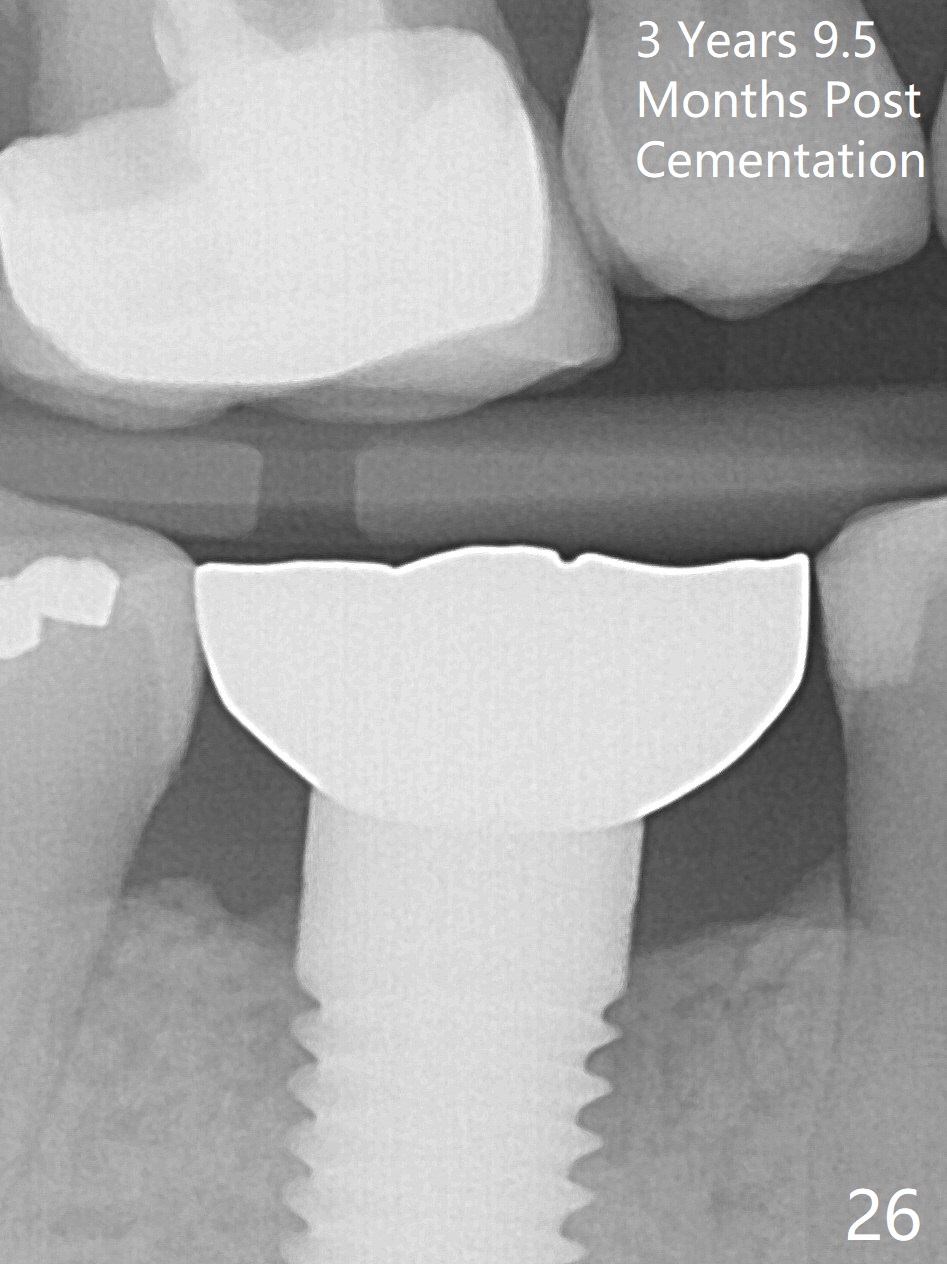
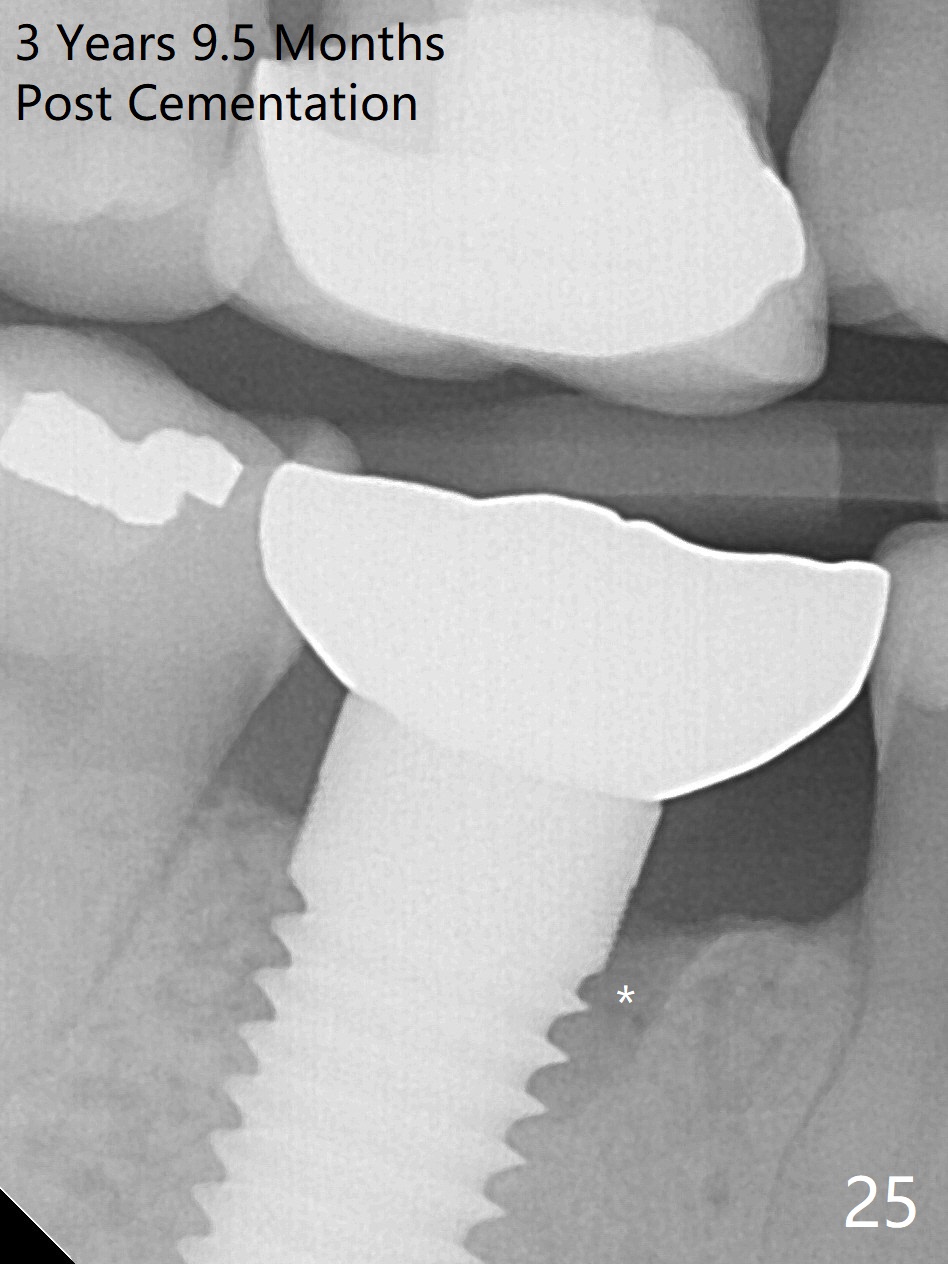
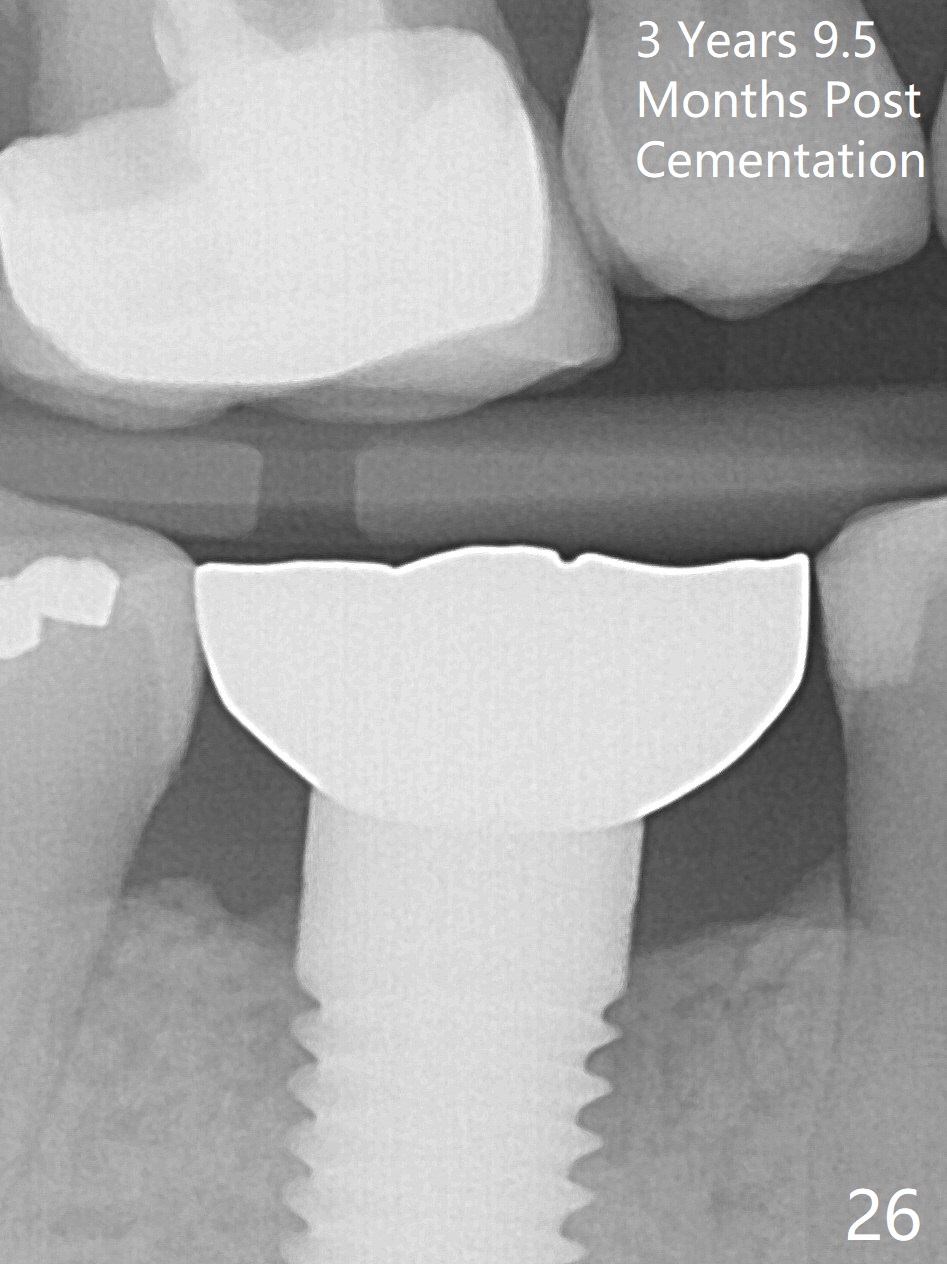
The patient will return for immediate implant at #14. Do not forget placing an implant as palatal as possible. There is no sign of infection at #30 three years 9.5 months post cementation because of water pik for #3 endo failure (Fig.25,26).
Return to
Lower Molar Immediate Implant,
Posterior Immediate Provisional,
1-Piece
Xin Wei, DDS, PhD, MS 1st edition 03/01/2014, last revision 11/04/2018