


 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
Immediate Implant Placed in the Molar Socket with Large Buccal Defect
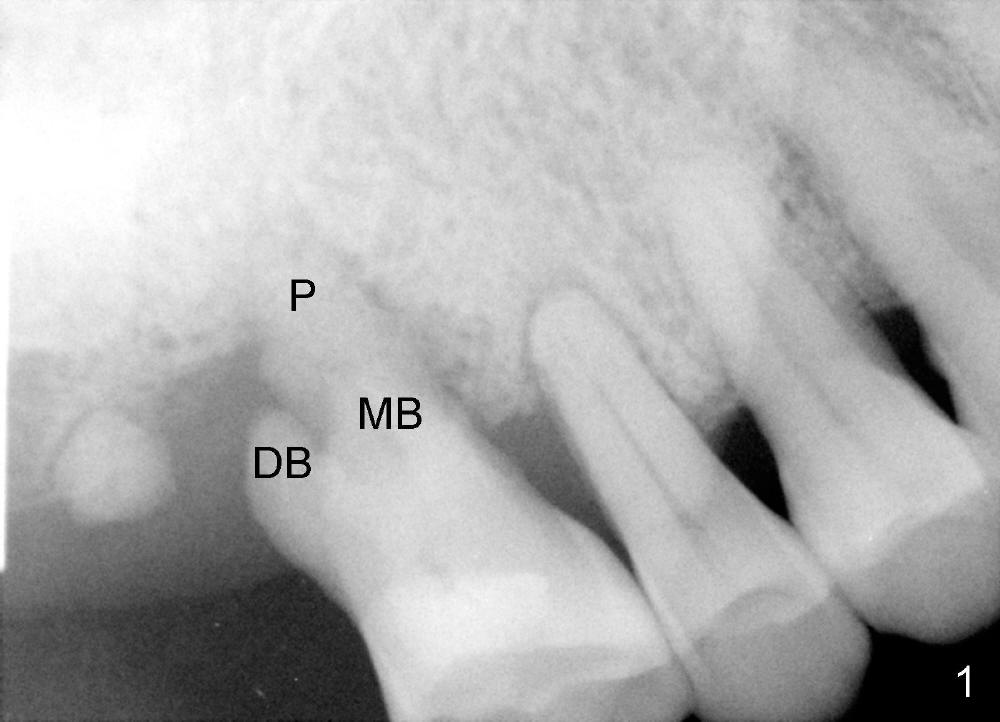
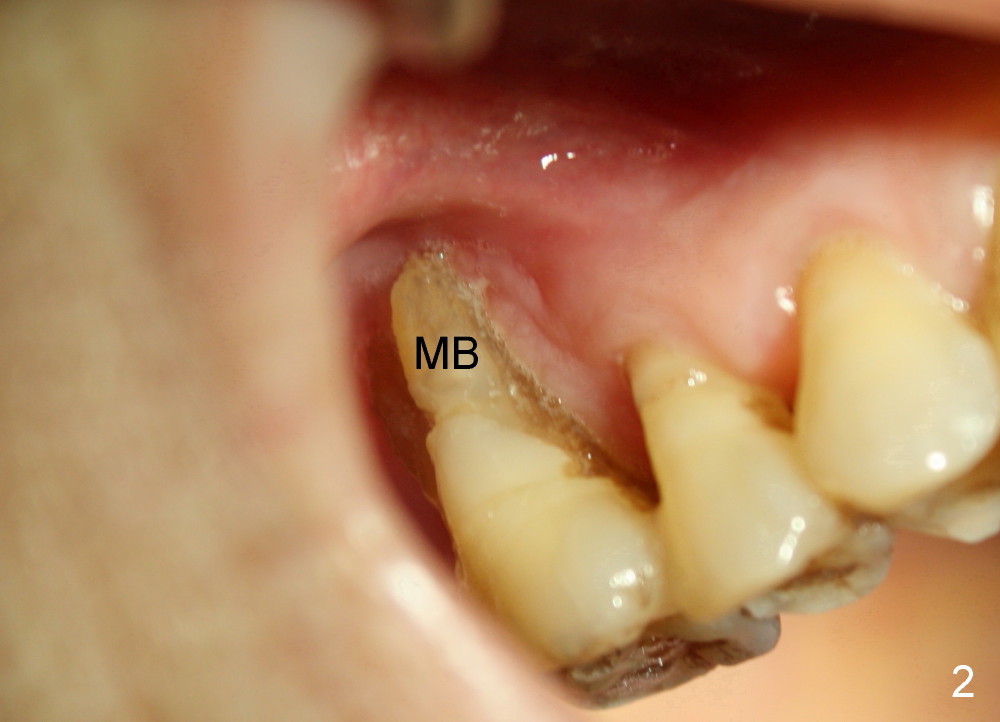
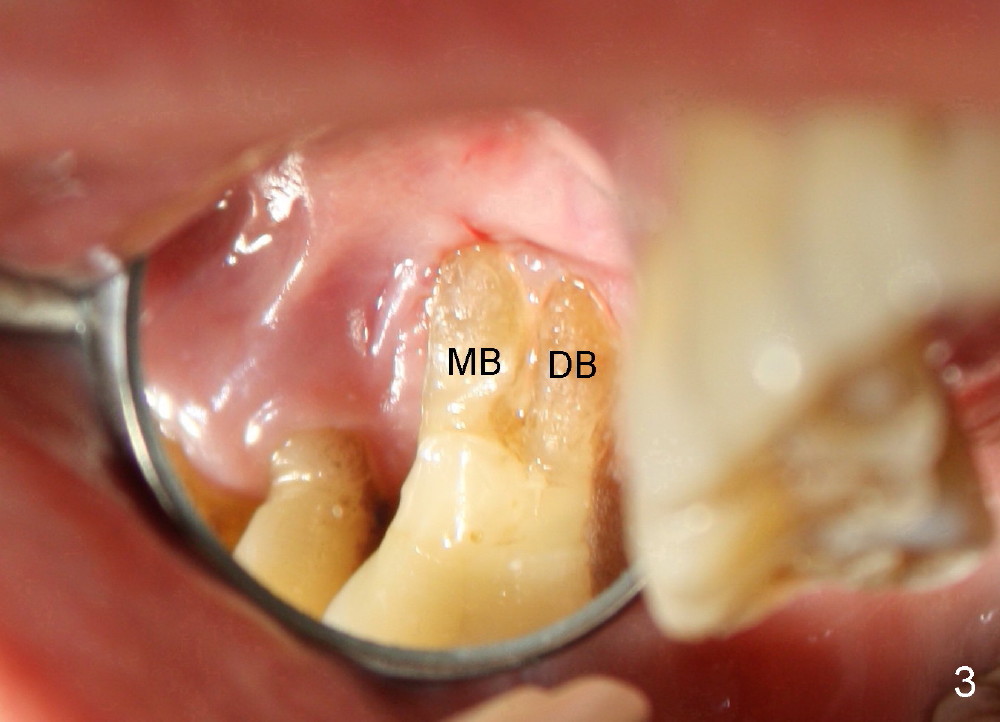
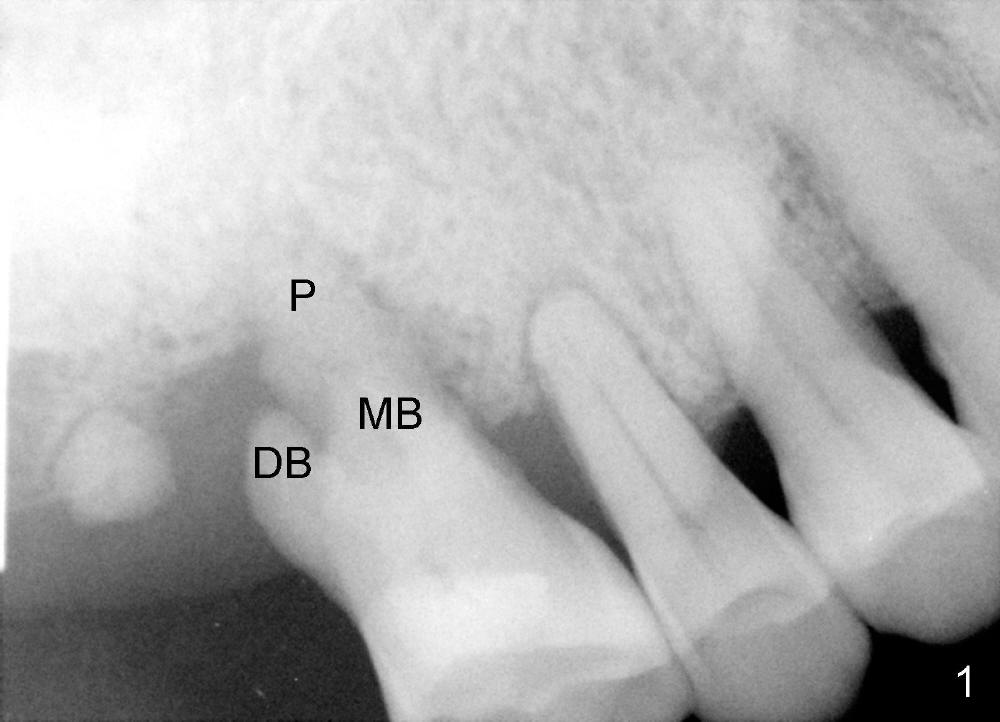
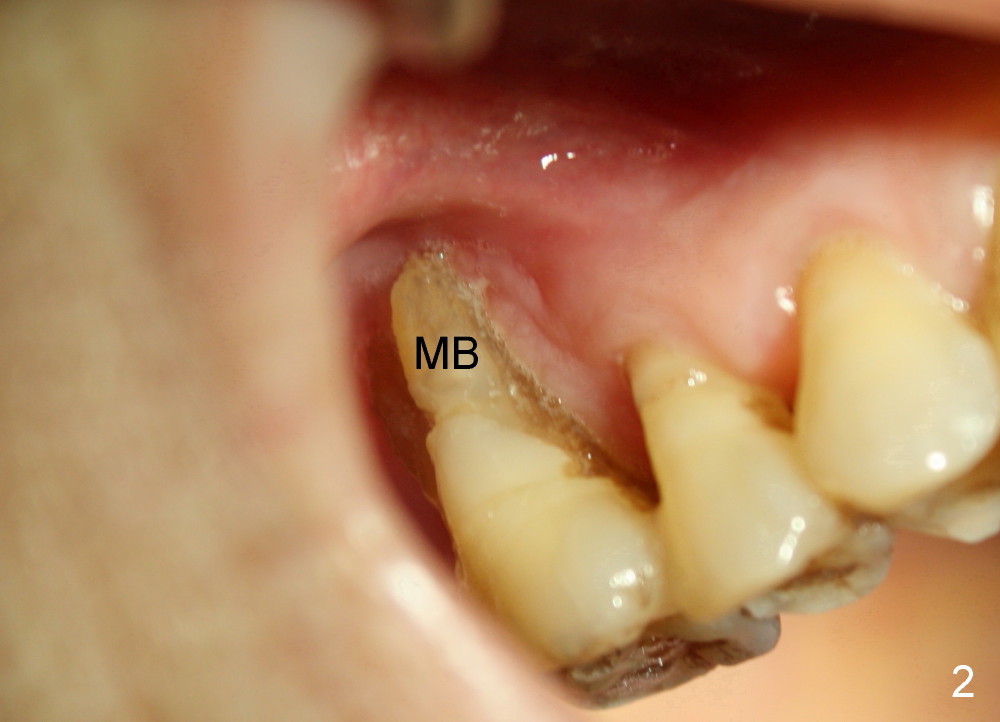
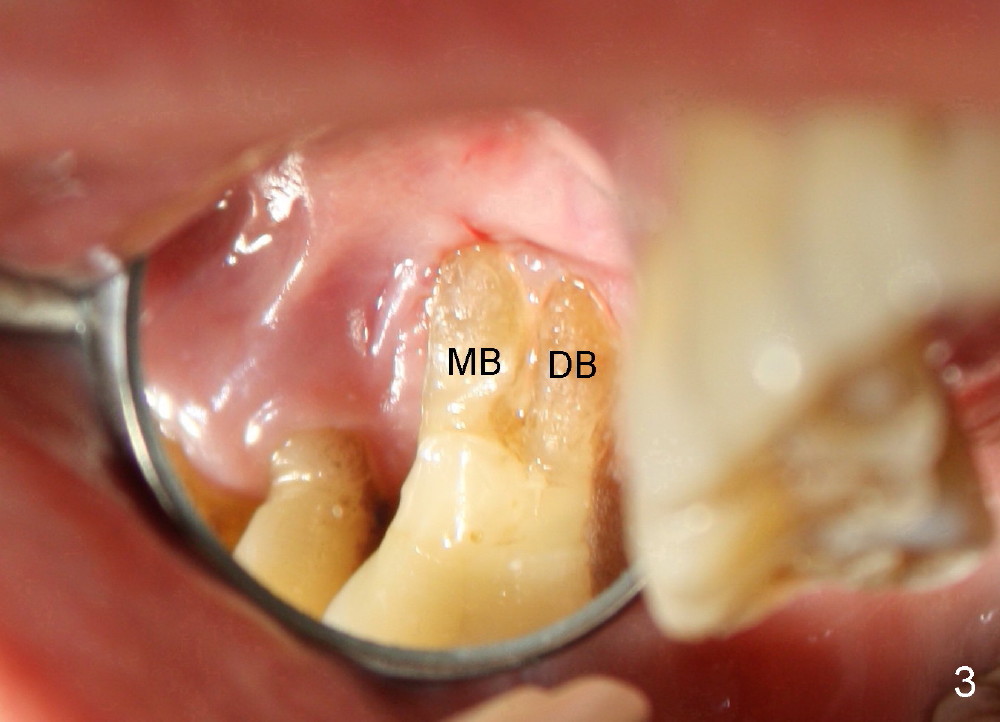
A 68-year-old lady presents to clinic with chief complaint of upper right pain. The tooth #3 has advanced periodontitis, compounded by occlusal trauma (Fig.1). There is severe bone loss, especially around the buccal roots, MB and DB. The latter are exposed (Fig.2,3).
Fig.4 shows the defect post extraction after debridement of infected granulation tissue. Apparently healthy tissue remains undisturbed and attaches to the septum (S).
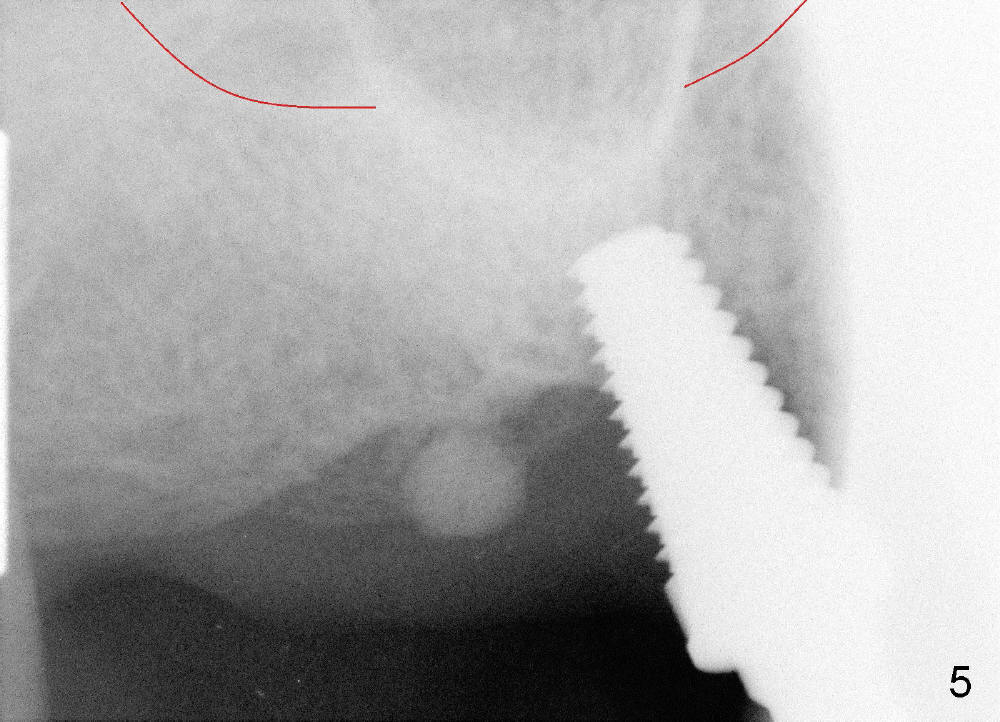
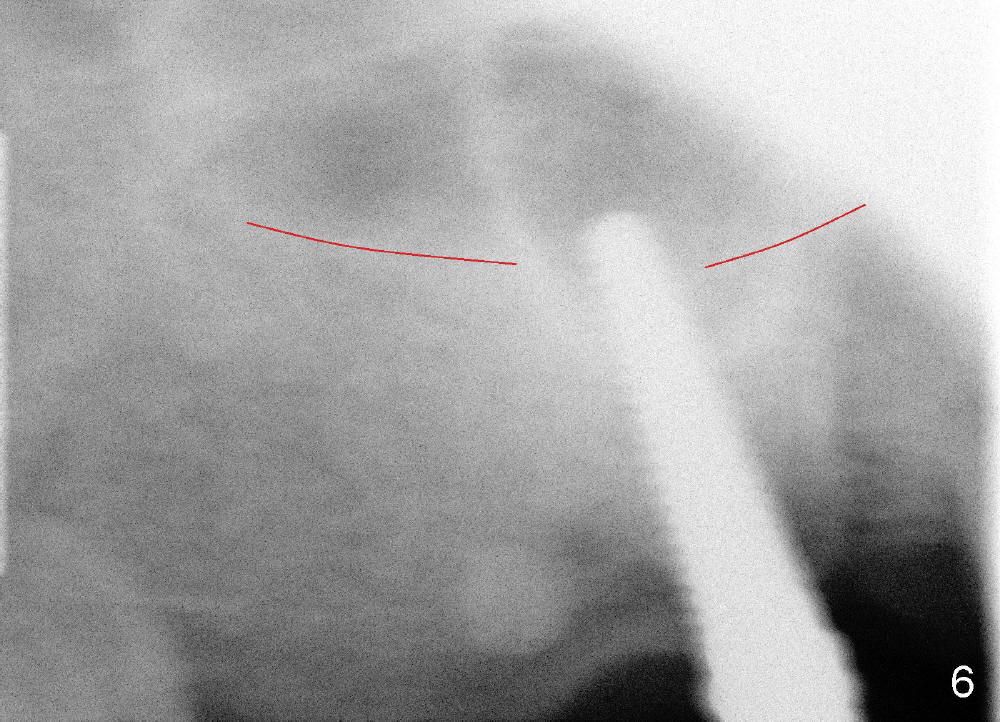
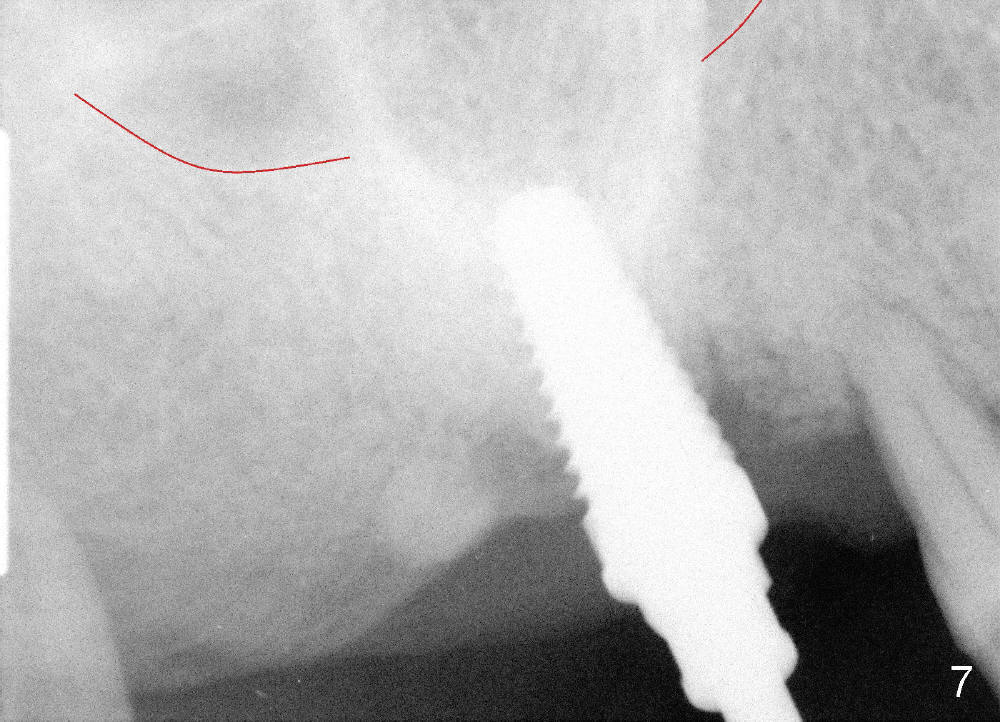
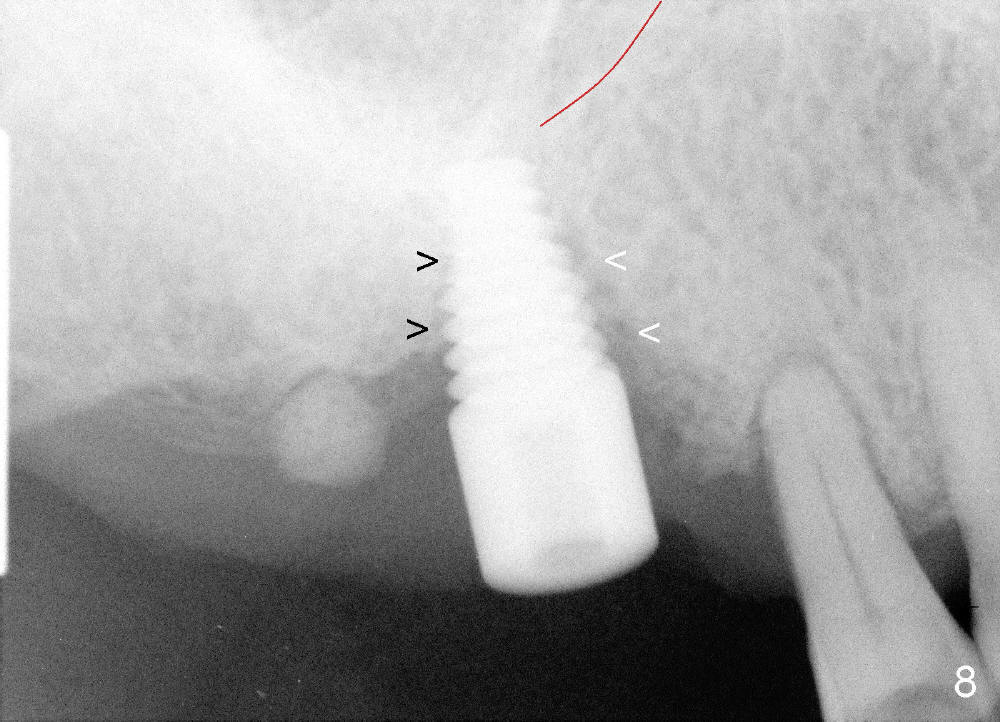
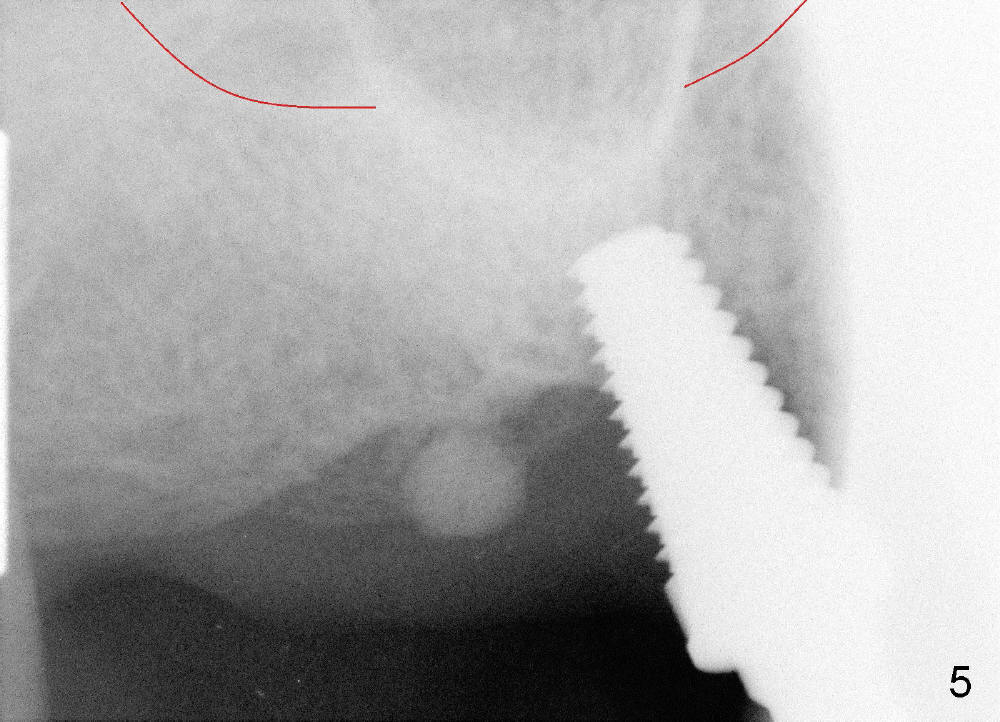
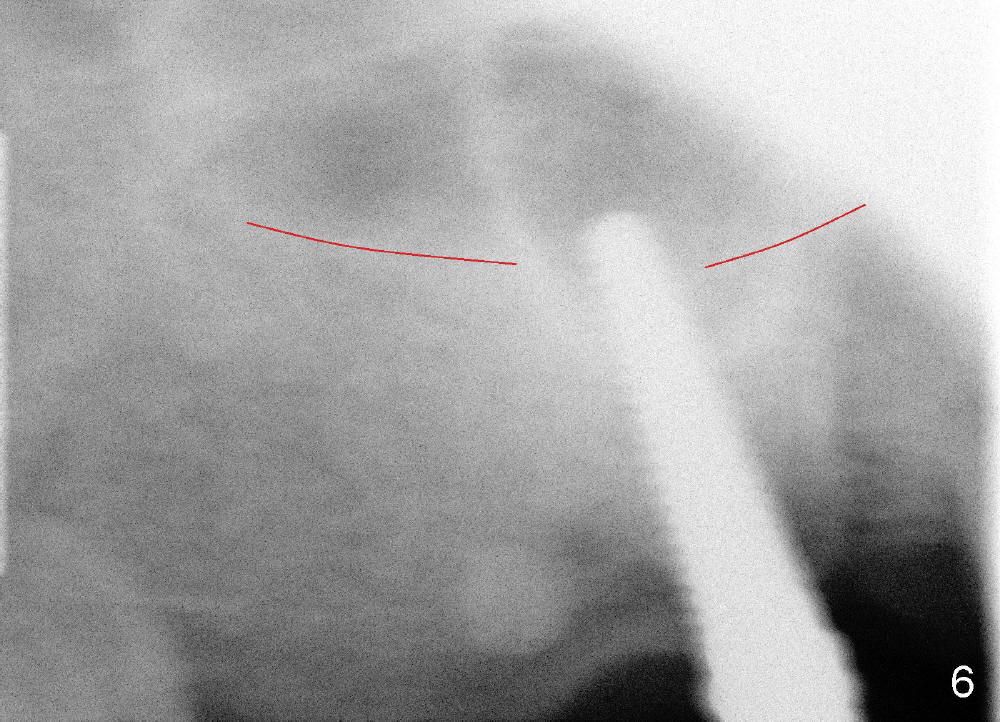
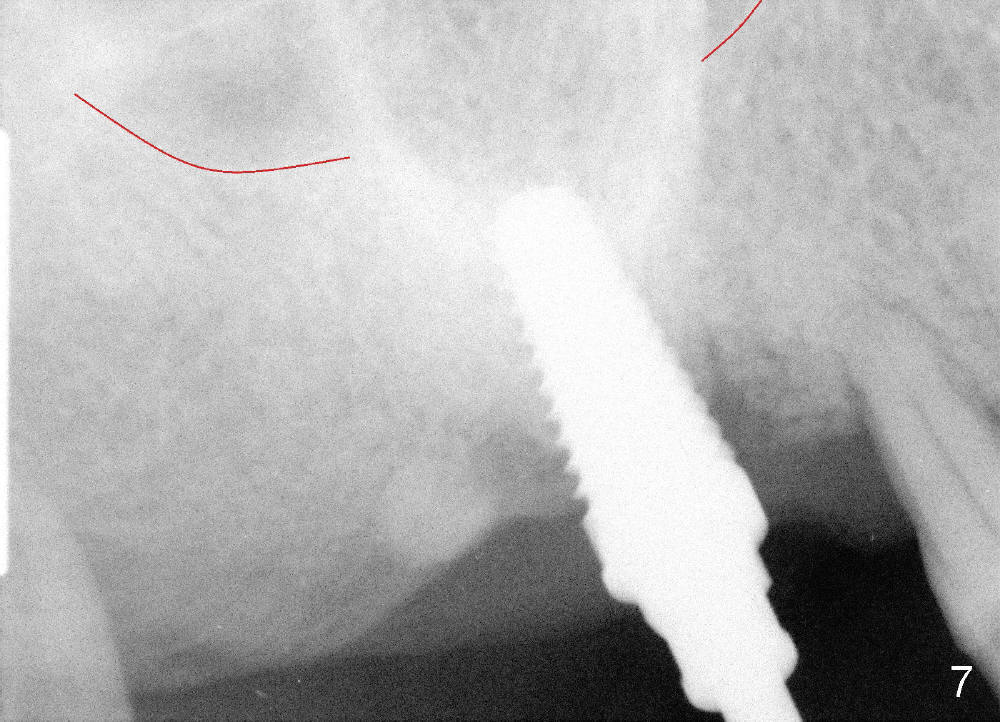
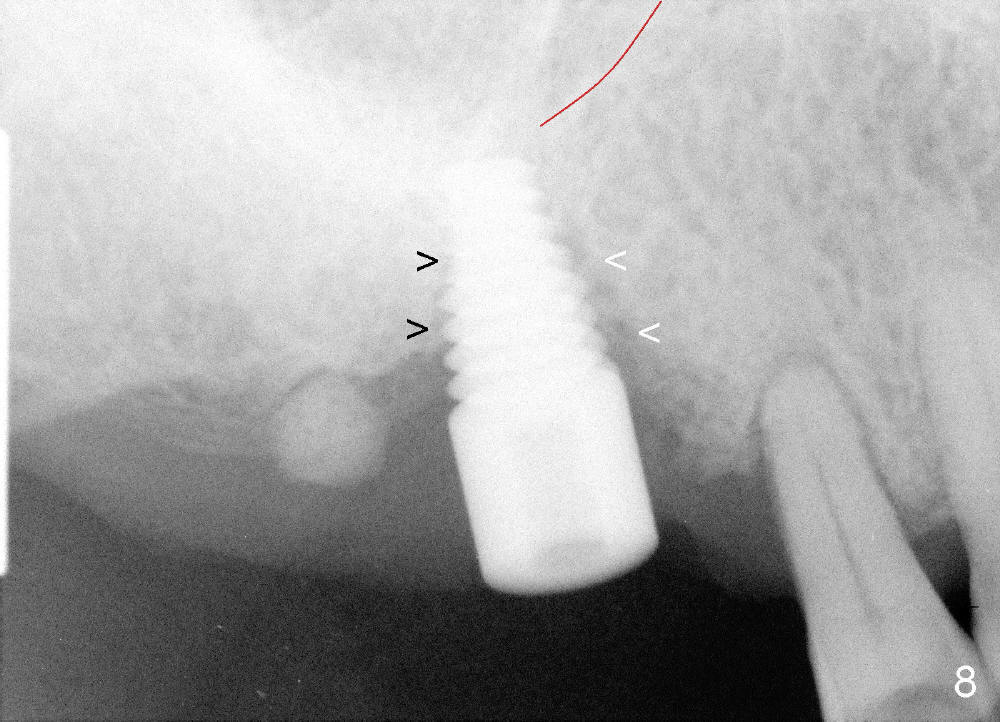
Osteotomy can be done in the palatal socket or the septum in this case to avoid implant thread exposure. Initial osteotomy is created in the palatal socket by using series of tap drills (4.5,5,6,7x17 mm) without stability or enough length (Fig.5; red line: sinus floor). The second osteotomy is made in the septum by using series of tapered osteotomes (2,3,4x17 mm), followed by 4.5x20 mm tap at depth of 17 mm with satisfactory binding (Fig.6). To avoid further sinus penetration and close the socket as much as possible, 5 and 6x17 mm taps are used at 14 mm deep (Fig.7). Nasal blowing reveals air leaking after the last tap. A 6x14 mm tapered implant is placed with insertion torque >60 Ncm (Fig.8). No bone graft is placed. The implant is surrounded by gingiva proximally and lingually and coagulation buccally. The wound is covered by perio dressing.
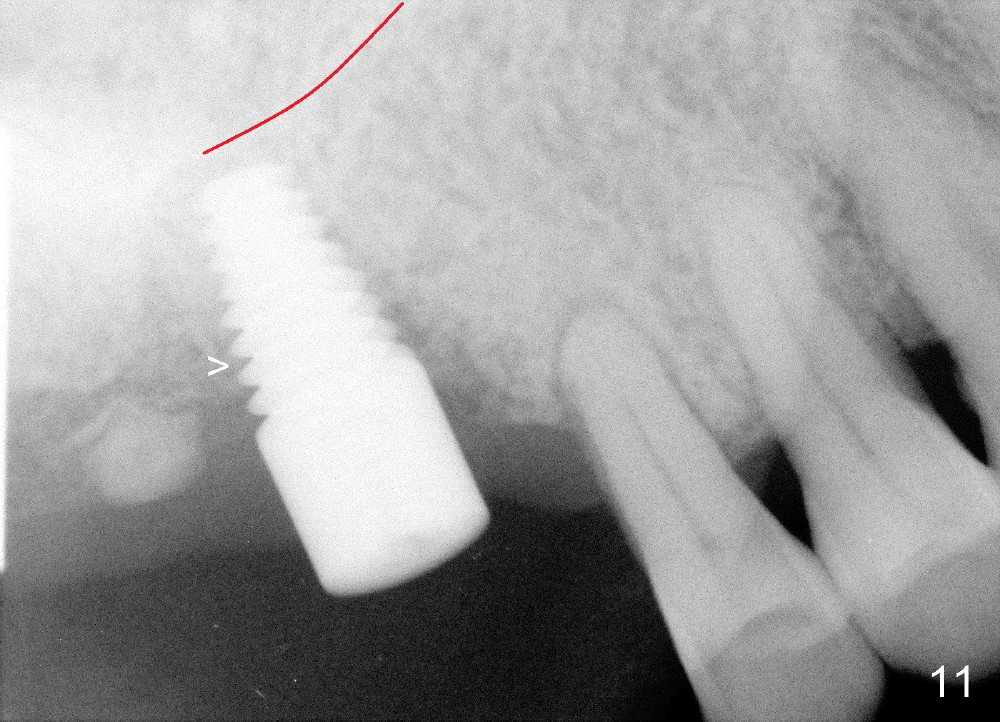
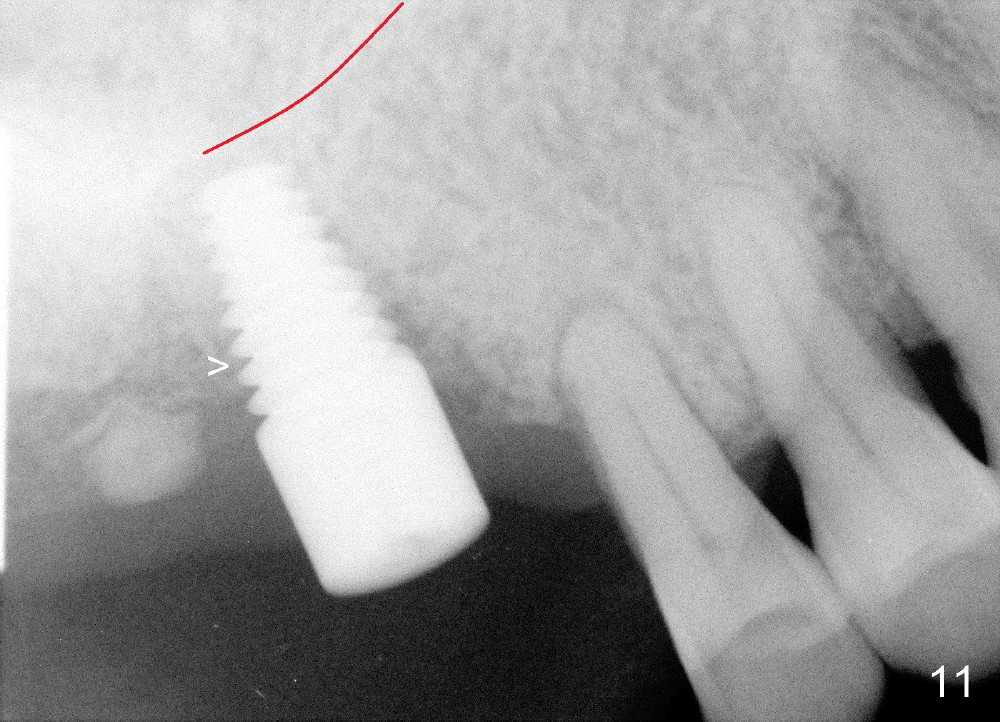
There is no nasal hemorrhage intra or postop. The implant is covered buccally by healing gingiva 7 days postop (Fig.9). It appears that the gingiva has strong regenerative potential. The buccal gingiva looks normal 3 months postop (Fig.10 healing cuff is placed over the implant). The implant appears to have osteointegrated (Fig.11).
Immediate implant not only saves time, but also avoids soft and hard tissue graft procedures in some cases.
Hard and Soft Tissue Defects, Introduction to Immediate Implant
Xin Wei, DDS, PhD, MS 1st edition 12/29/2013, last revision 04/22/2018