

.jpg)
.jpg)

 |
 |
 |
.jpg) |
 |
 |
 |
|
 |
.jpg) 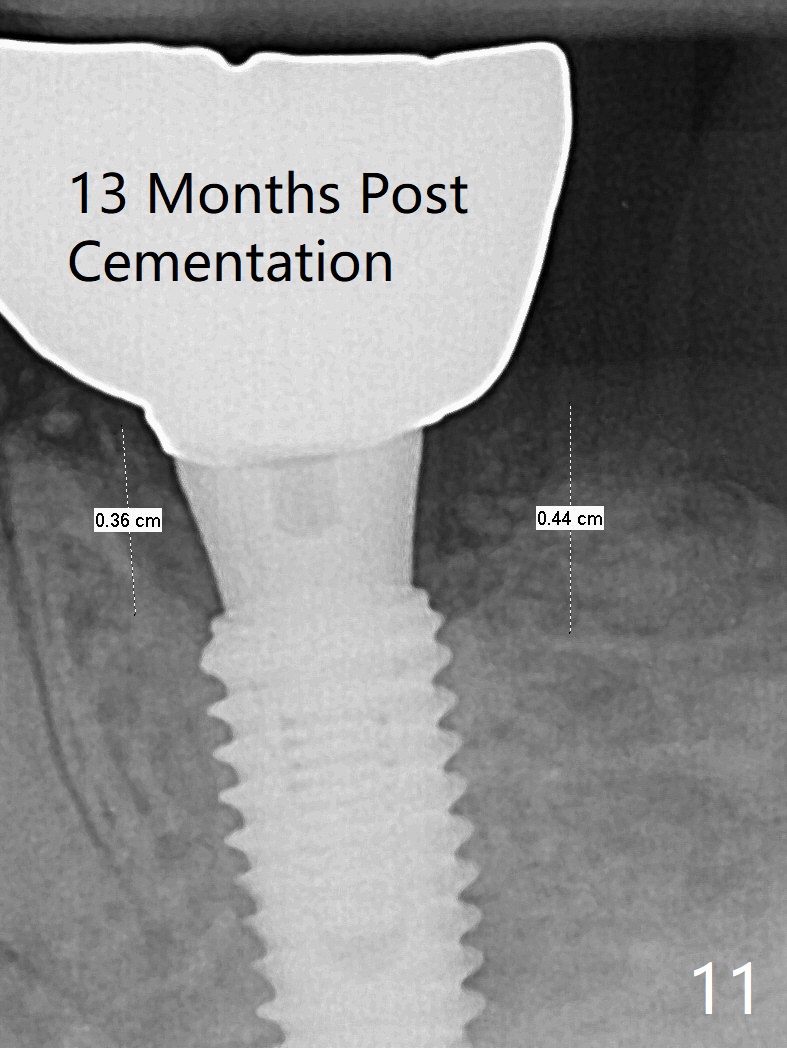 |
 |
|
More Secure Graft Retention M
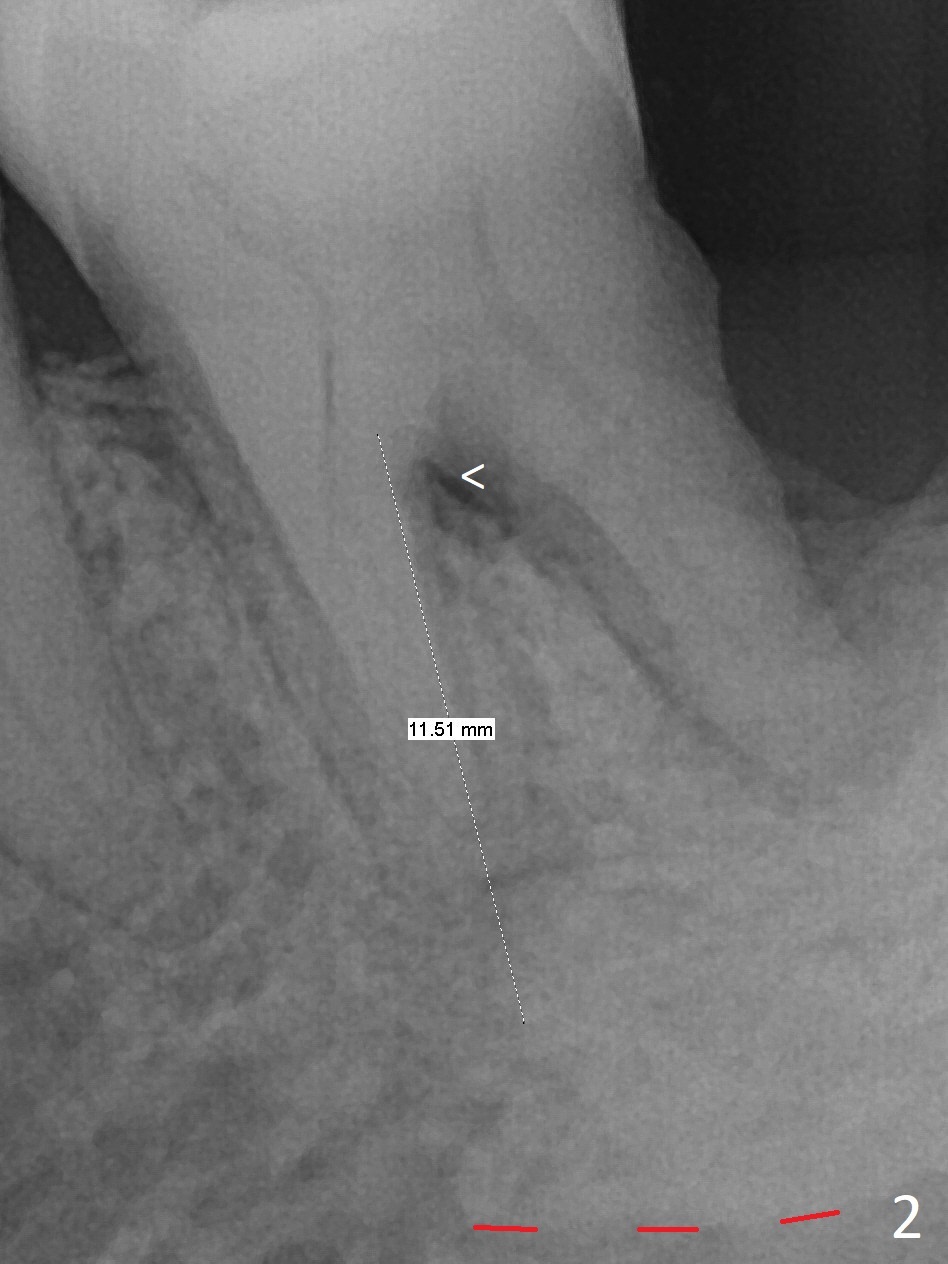
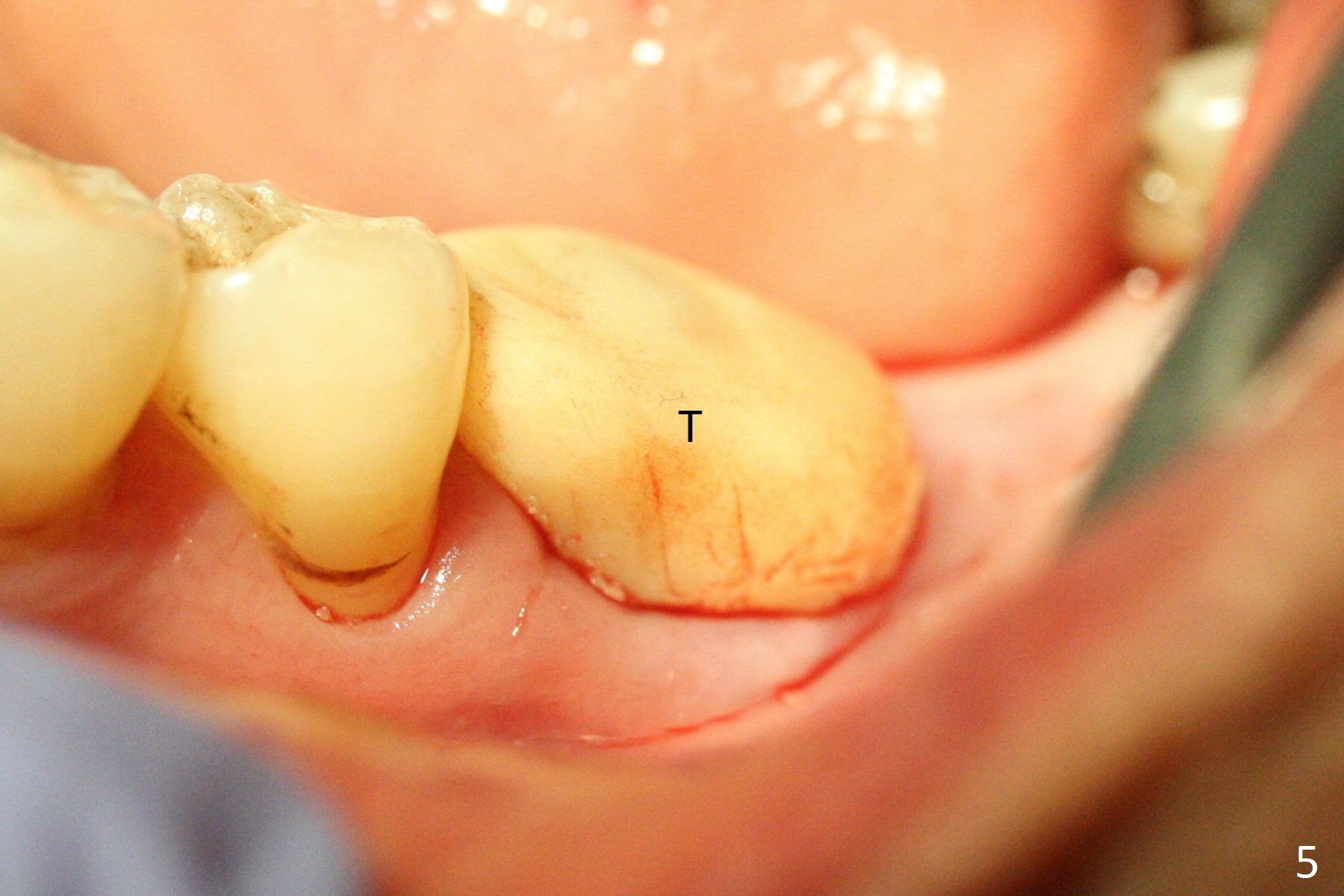
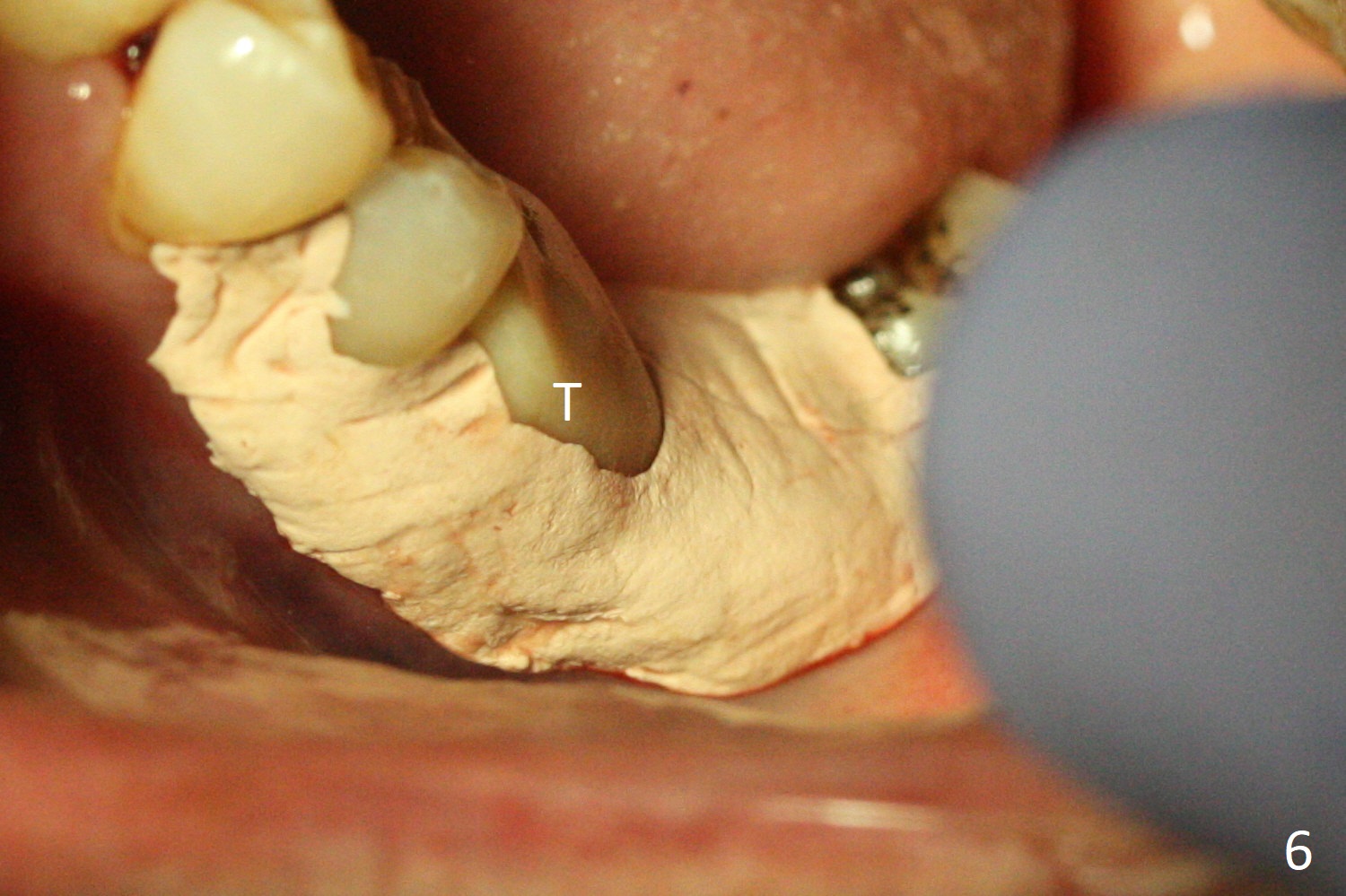
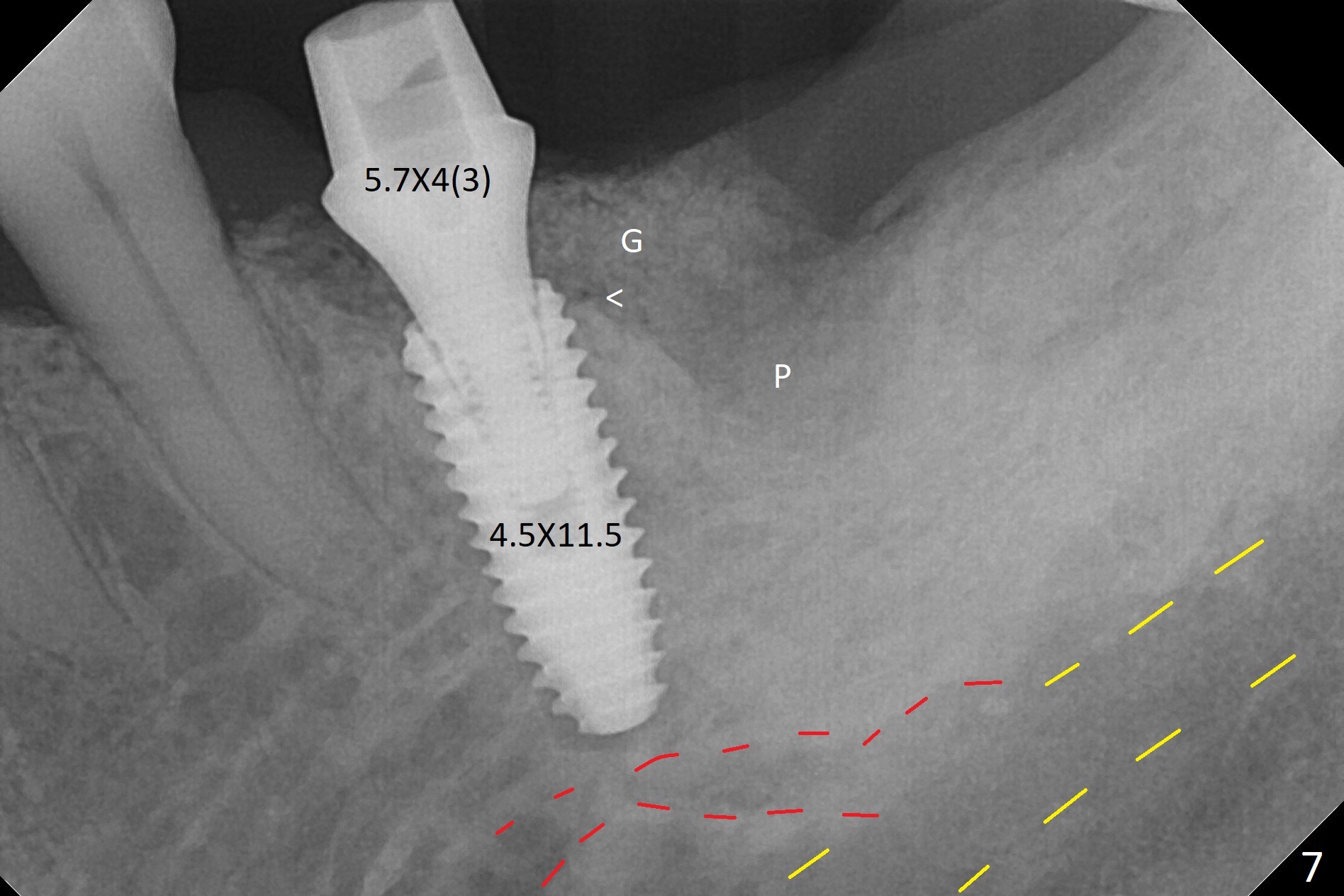
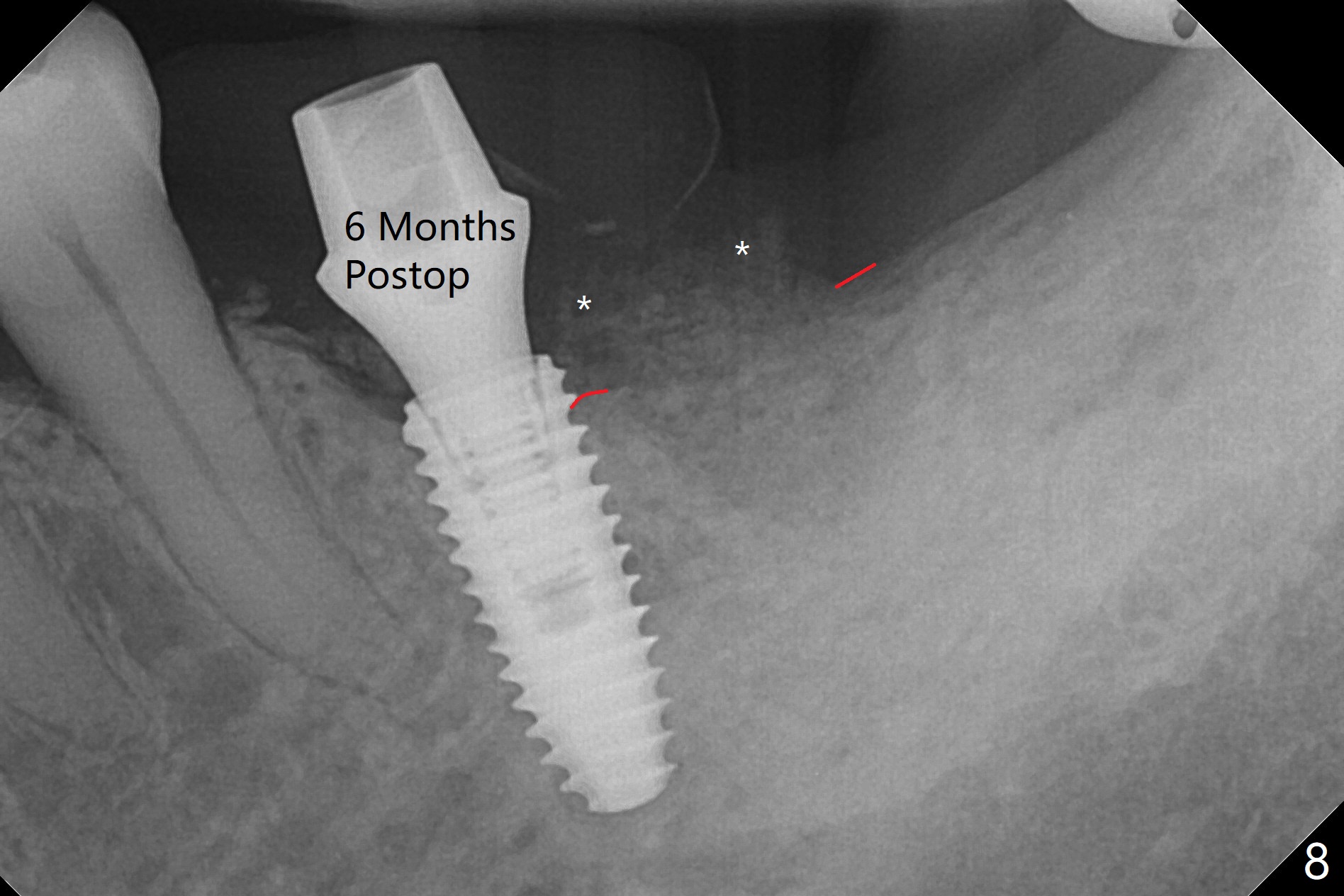
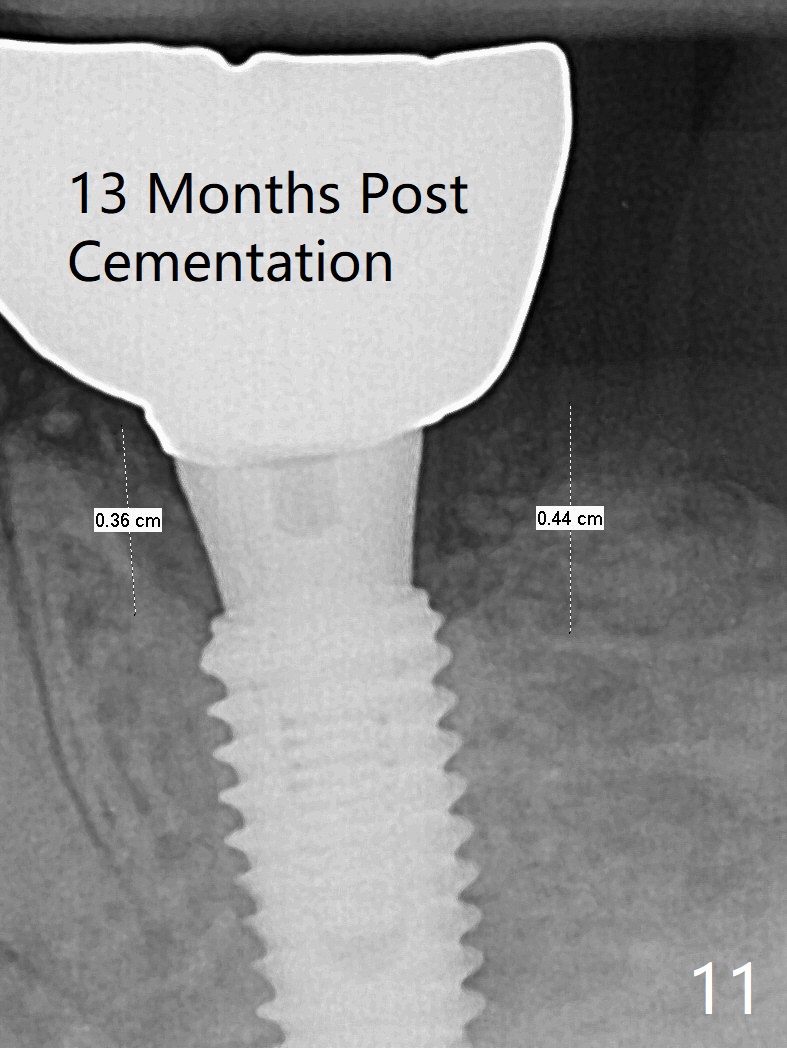
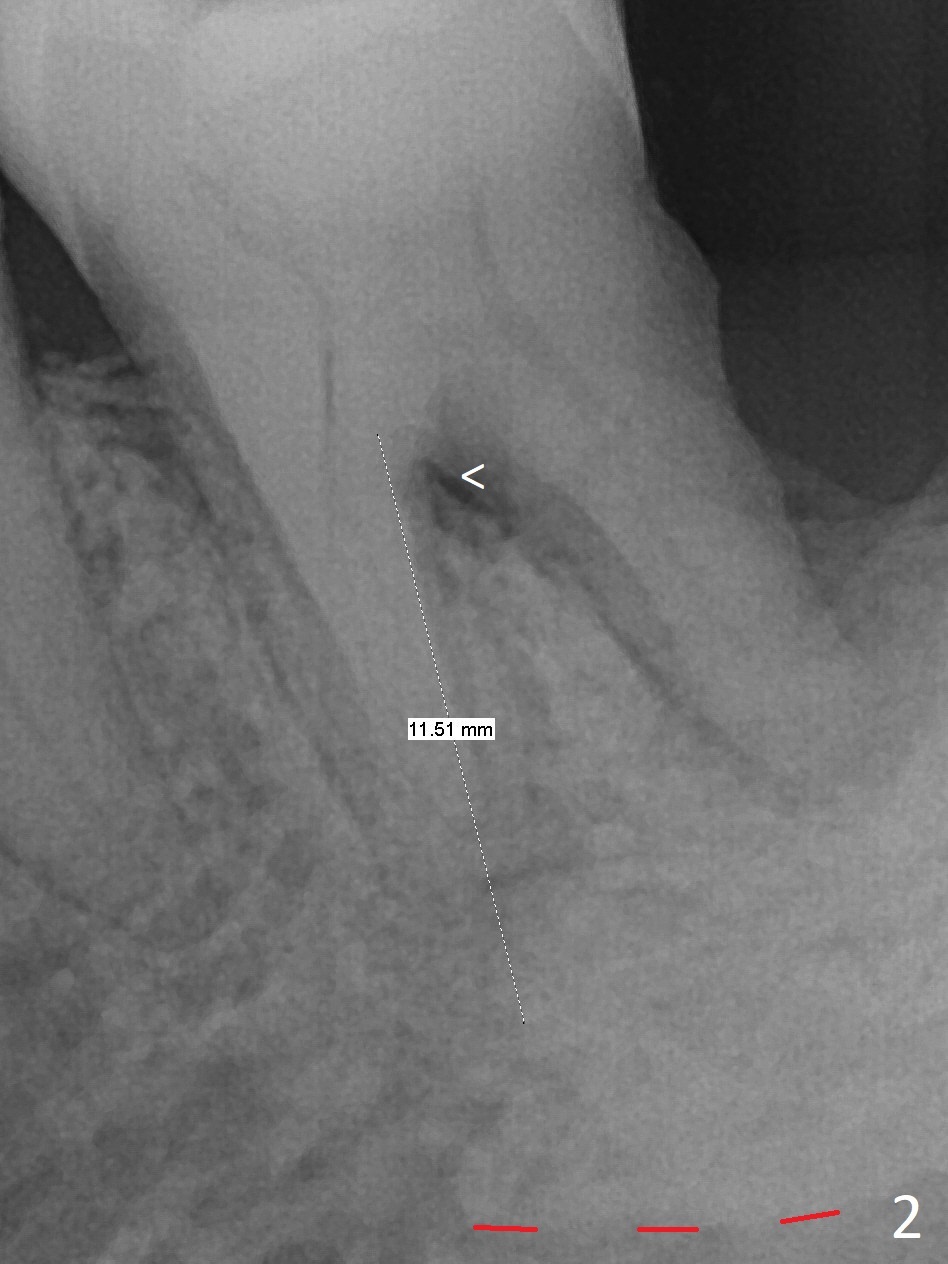
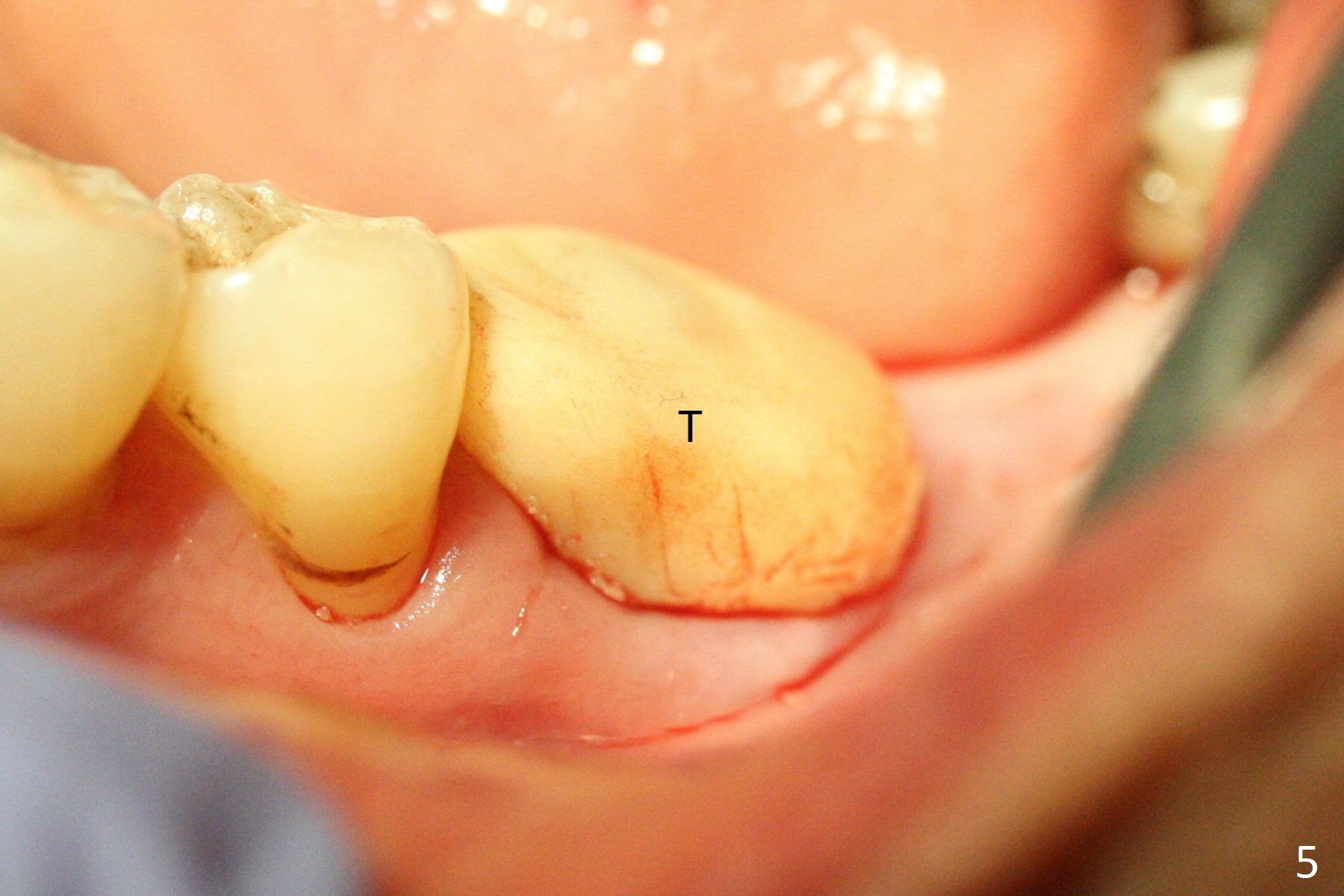
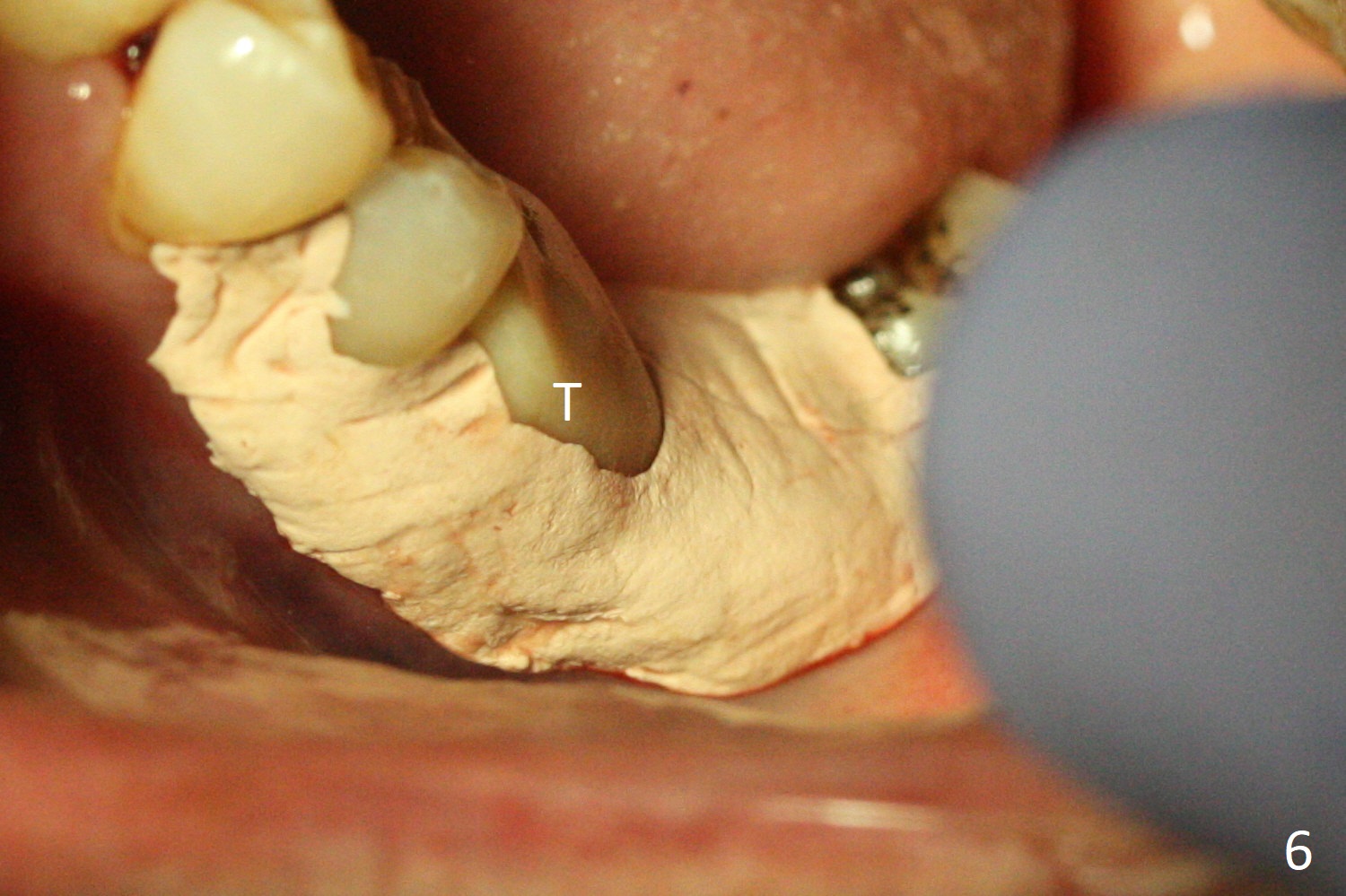
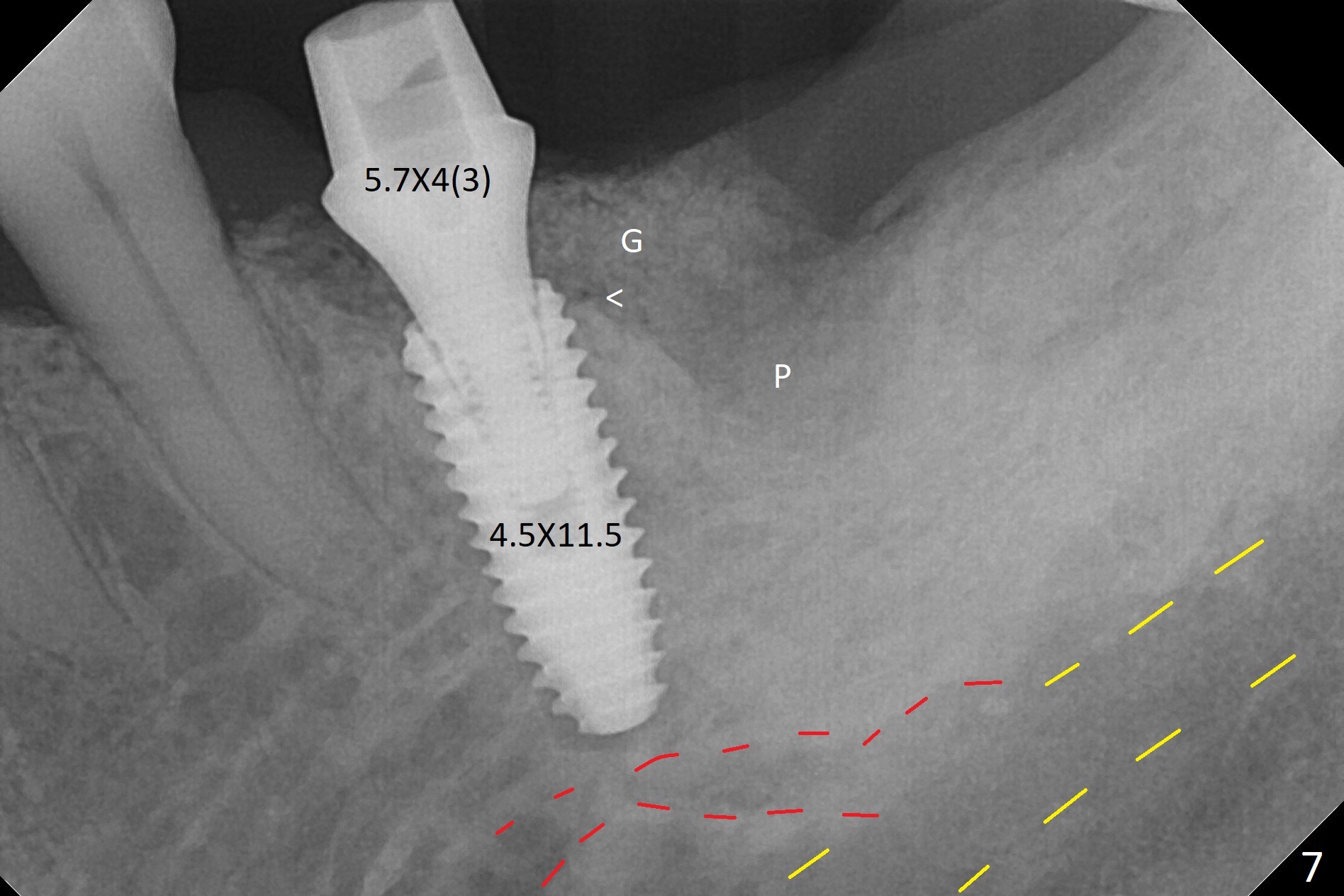
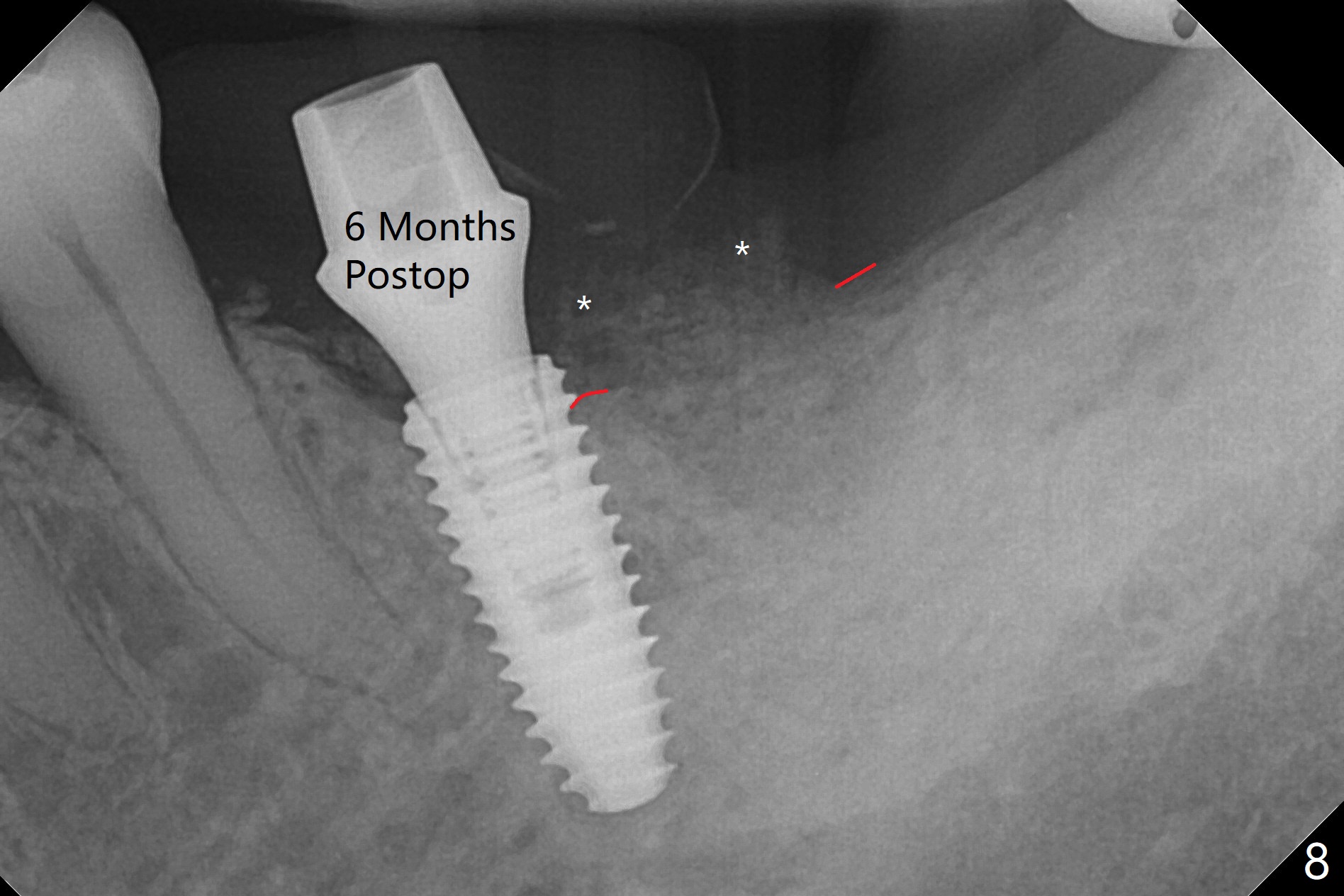
A 68-year-old man returns for extraction of the tooth #19 with distal root periodontal-endodontic lesion (Fig.1 *). After discussion, he agrees immediate implant. A 4.5x11.5 mm implant will be placed in the mesial socket (Fig.2 (red line: superior border of Inferior Alveolar Canal)); the plateau level with the septal crest (<). Osteotomy is initiated in the lingual slope of the mesial socket; the depth is controlled with stopper (Fig.3 S). The implant is placed at the level as expected (Fig.4 <) with insertion torque ~30 Ncm; after placement of 5.7x4(3) mm abutment and Osteogen plug (P) in the apical half of the distal socket, bone graft (G) is placed in the remaining socket gaps, mainly distal and buccal. An immediate provisional is fabricated to keep the graft in place (Fig.5 T). The graft may be lost if the gingival margin recedes in healing. Periodontal dressing is applied for additional security (Fig.6). There is no postop paresthesia. The upper border of the Inferior Alveolar Canal in Fig.3,4 seems to be high. In fact it may be a branch of the Inferior Alveolar Canal (Fig.7 yellow line, as compared to Fig.4). With all of measures taken (including periodontal dressing), the distal bone graft (Fig.8 *) is ~ 2 mm coronal to the crestal bone (red line) 6 months postop. The temporary crown is perforated. The gingival cuff is erythematous. A 6.8x5 mm healing abutment is installed. When the patient returns for impression, a 4.5x5.5(3) mm abutment is fully seated (Fig.9 <). The distal height increases by 4 mm because of immediate implant (support). The mesial papilla remains normal in height and shape immediate post cementation (Fig.10), as related to the mesial socket implant placement without mesial crestal bone loss. The mesial and distal crestal height is maintained 13 months post cementation (Fig.11, weight lifter).
Return to Lower Molar Immediate Implant, Prevent Molar Periimplantitis (Protocols, Table), Trajectory, Metronidazole Next Case 牙周敷料 Xin Wei, DDS, PhD, MS 1st edition 06/28/2019, last revision 03/17/2021