
,%20better%205.5(3).jpg)
,%20distal%20bone%20growth.jpg)
 |
 |
,%20better%205.5(3).jpg) ,%20distal%20bone%20growth.jpg) |
 |
Slow Osteotomy Reduces Pain M
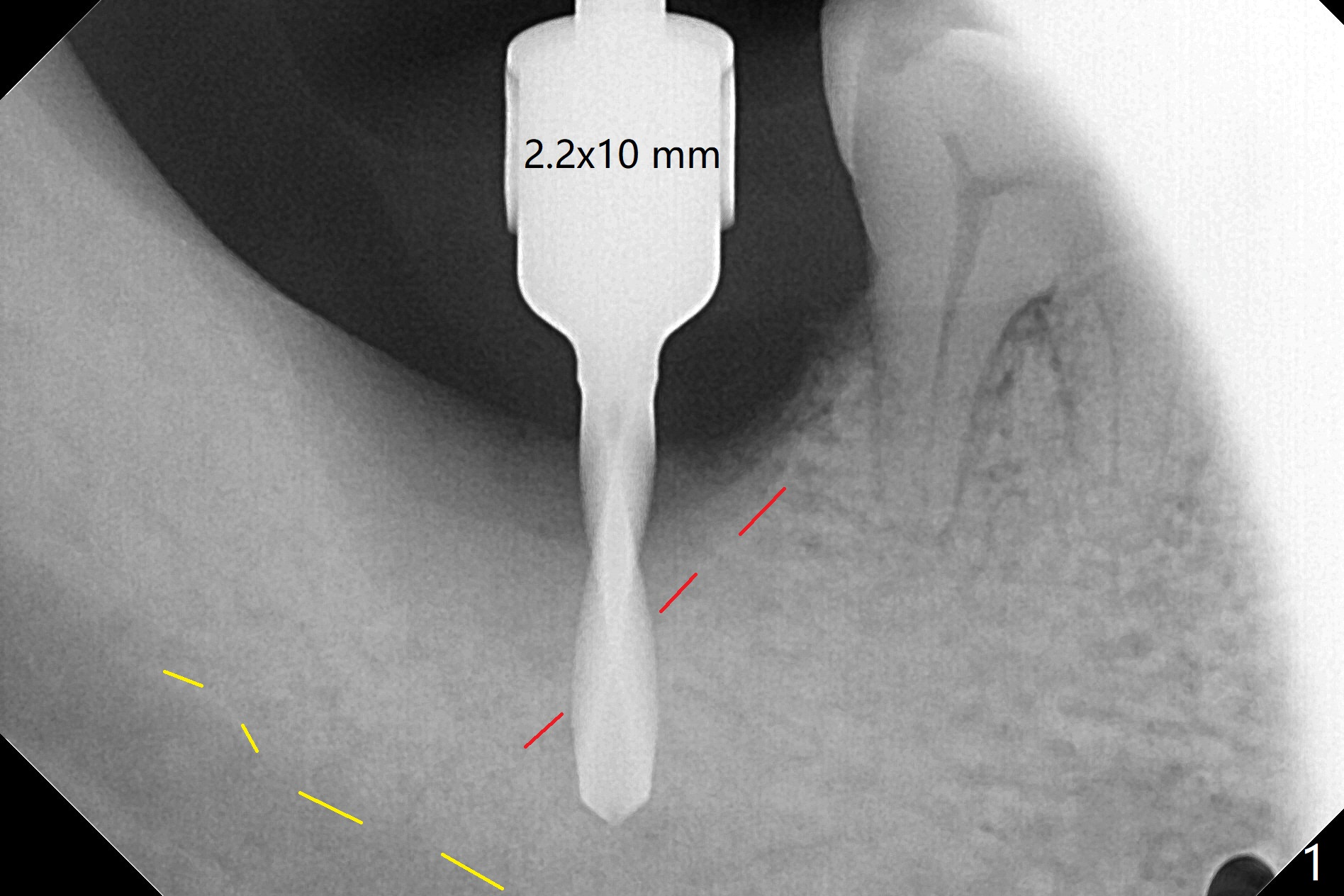
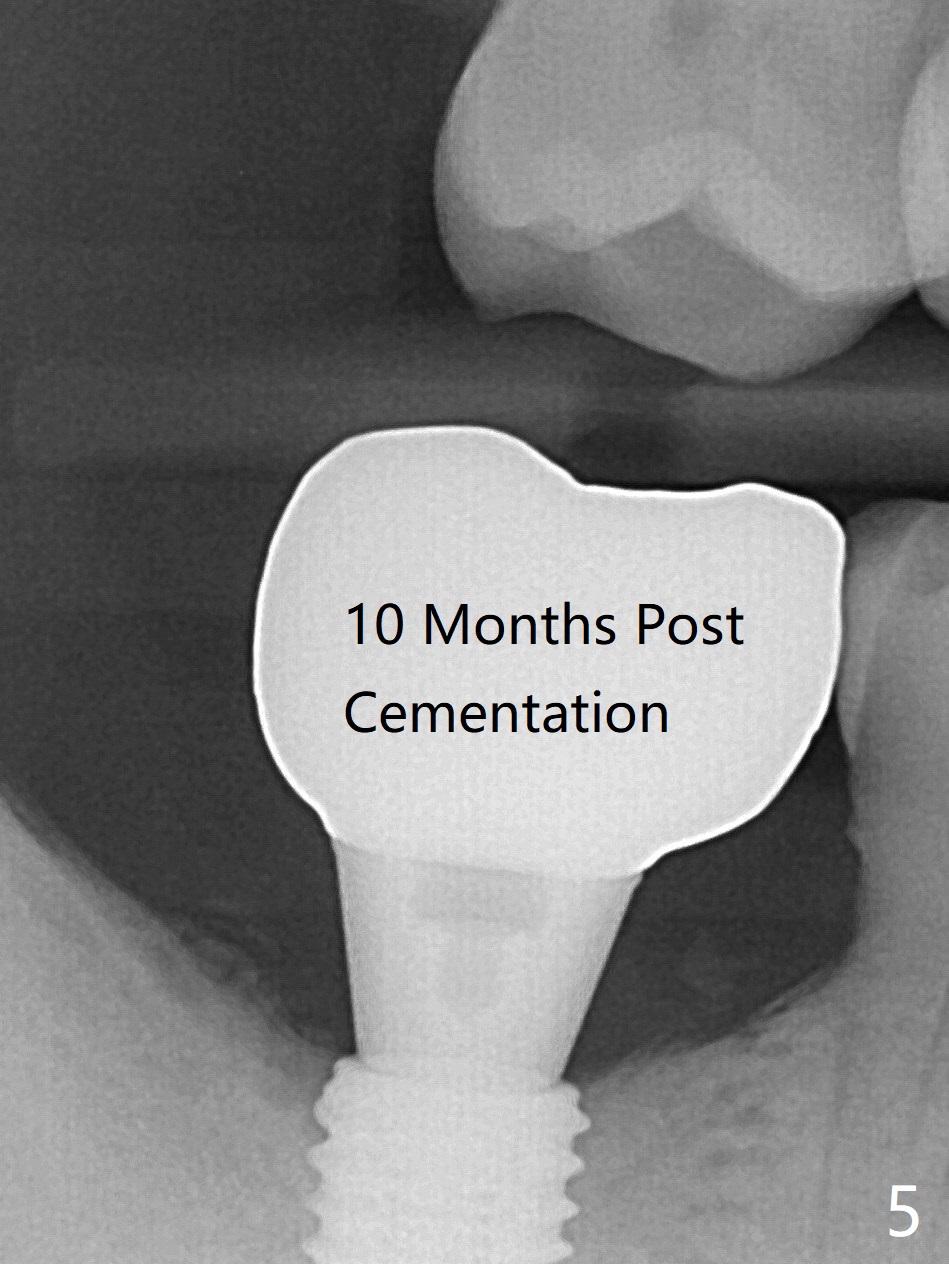
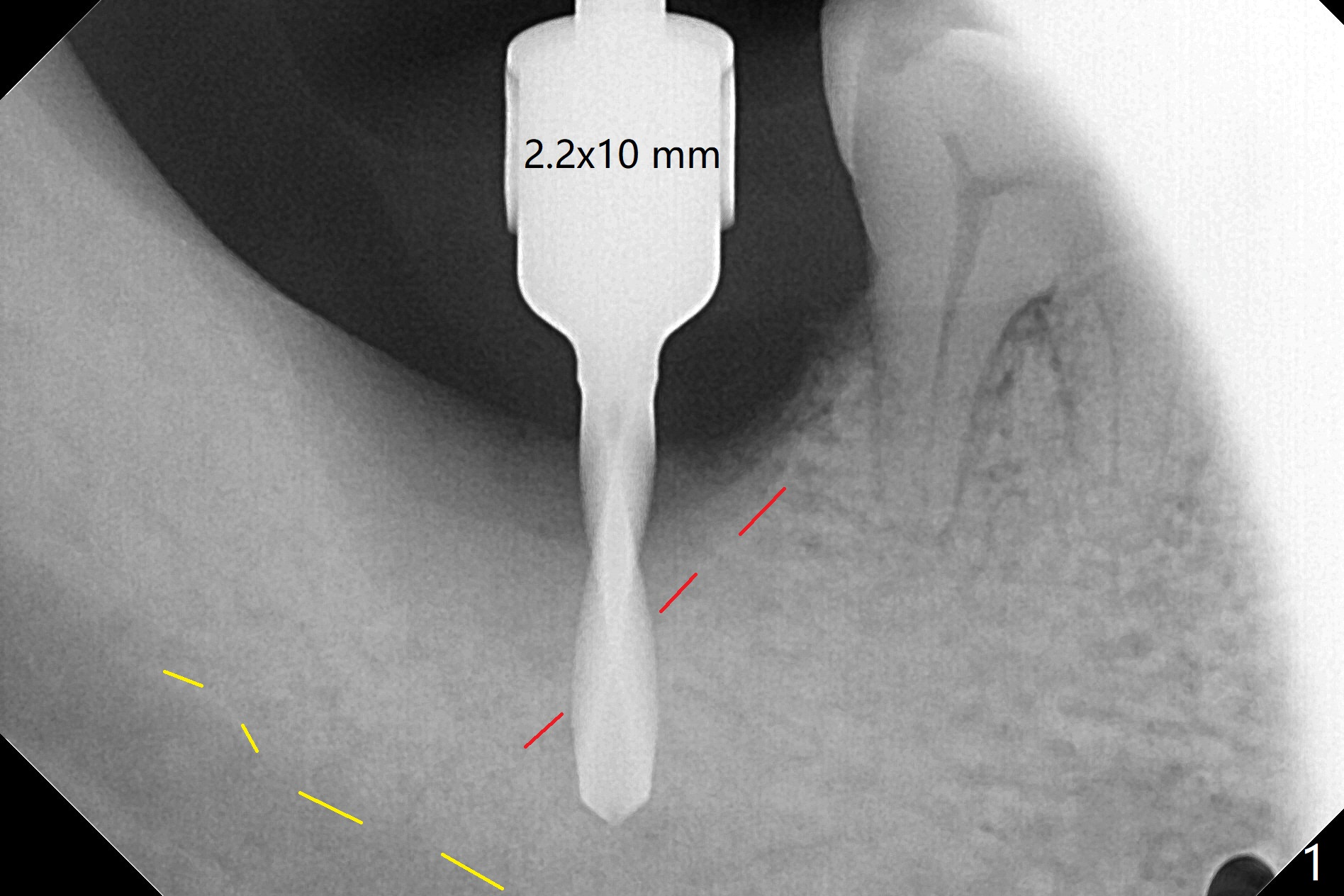
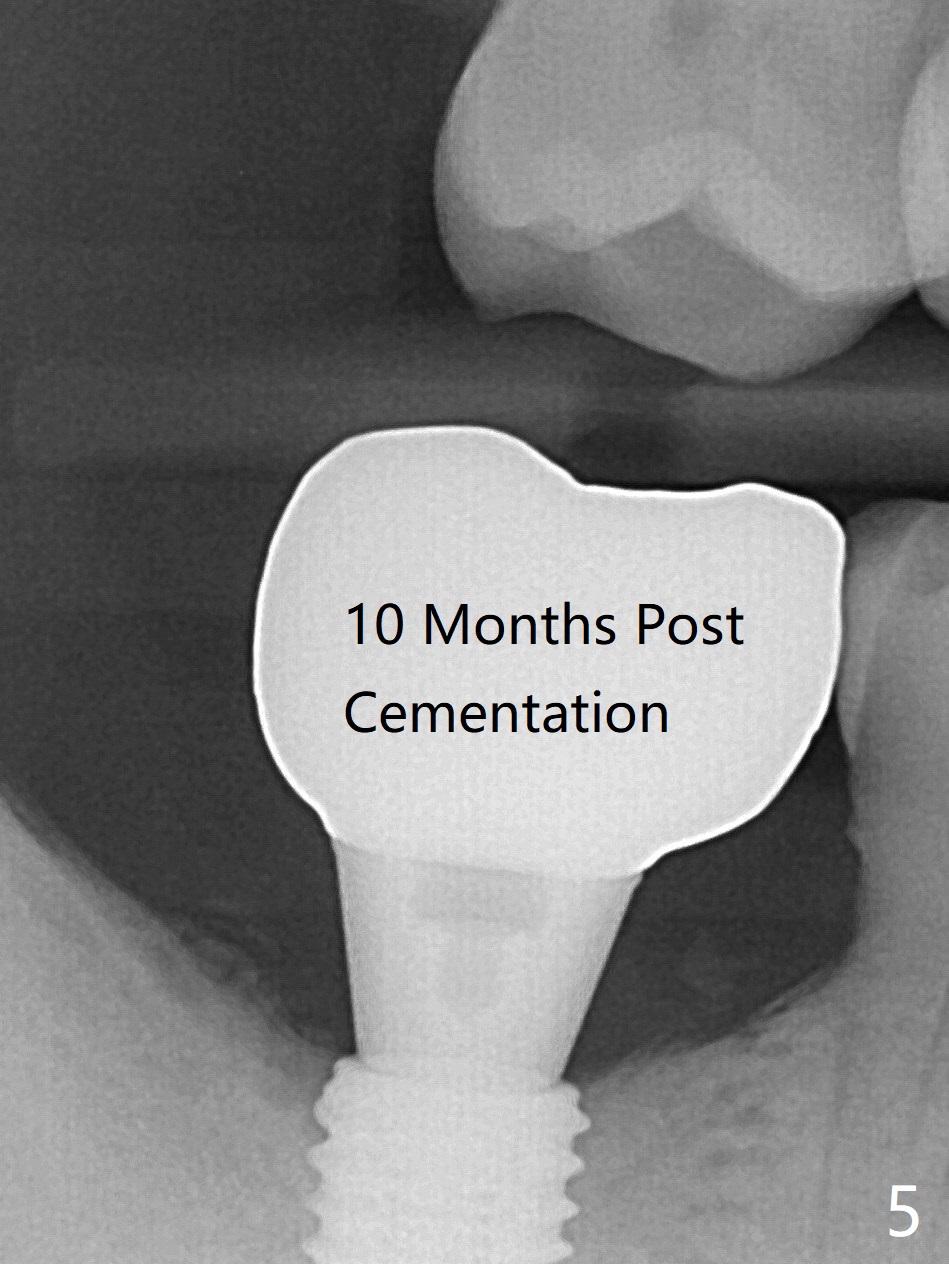
The morning case shows that to avoid Inferior Alveolar Neuropathy associated with 2nd molar implant placement, three measures should be adopted, no block anesthesia, no pressure on the distal end of the distal end guide and no over deep placement. In fact pain control is difficult with severe chronic periodontitis at #31. After repeated infiltration injection, the most effective step of anesthesia is slow speed of osteotomy with gentle pressure. The 1st intraop PA is taken when the depth is reached with a 2.2 mm pilot drill (Fig.1 (yellow dashed line: superior border of the Inferior Alveolar Canal)). The 2nd purpose of the PA is to make sure that the osteotomy is establish in the mesial slope of the socket (red dashed line). As drills increase in diameter, the patient experiences pain. Since the bone density is high, it is hard to place 5x10 mm implant to the lowest space (Fig.2 *, ~ 60 Ncm). For compensation, bone graft (Fig.3 *) is packed securely around the implant before and after abutment insertion. After fabrication of an immediate provisional, periodontal dressing is applied around the provisional and socket to prevent graft leakage. Smoke cessation/reduction is encouraged. In fact the patient returns 11 months postop (the 1st time postop), partly due to coronavirus. The immediate provisional is lost, but the distal defect has apparently been repaired (Fig.4*). A 4 mm cuff abutment is changed to due to enough occlusal clearance. The abutment is completely seated. Oral hygiene is poor with 1/2 ppd of smoke. SRP was done in the lower right quadrant when the implant was placed. When the crown is delivered 1 year postop, the patient mentions #18 mobility. SRP is done in the lower left quadrant. The bone is stable 10 months post cementation (Fig.5).
Return to Lower Molar Immediate Implant, Prevent Molar Periimplantitis (Protocols, Table), Trajectory II 18 第二磨牙即种
Xin Wei, DDS, PhD, MS 1st edition 07/30/2019, last revision 05/12/2021