.jpg)












.jpg) |
 |
 |
 |
 |
 |
 |
 |
 |
 |
  |
 |
 |
Hard Bone
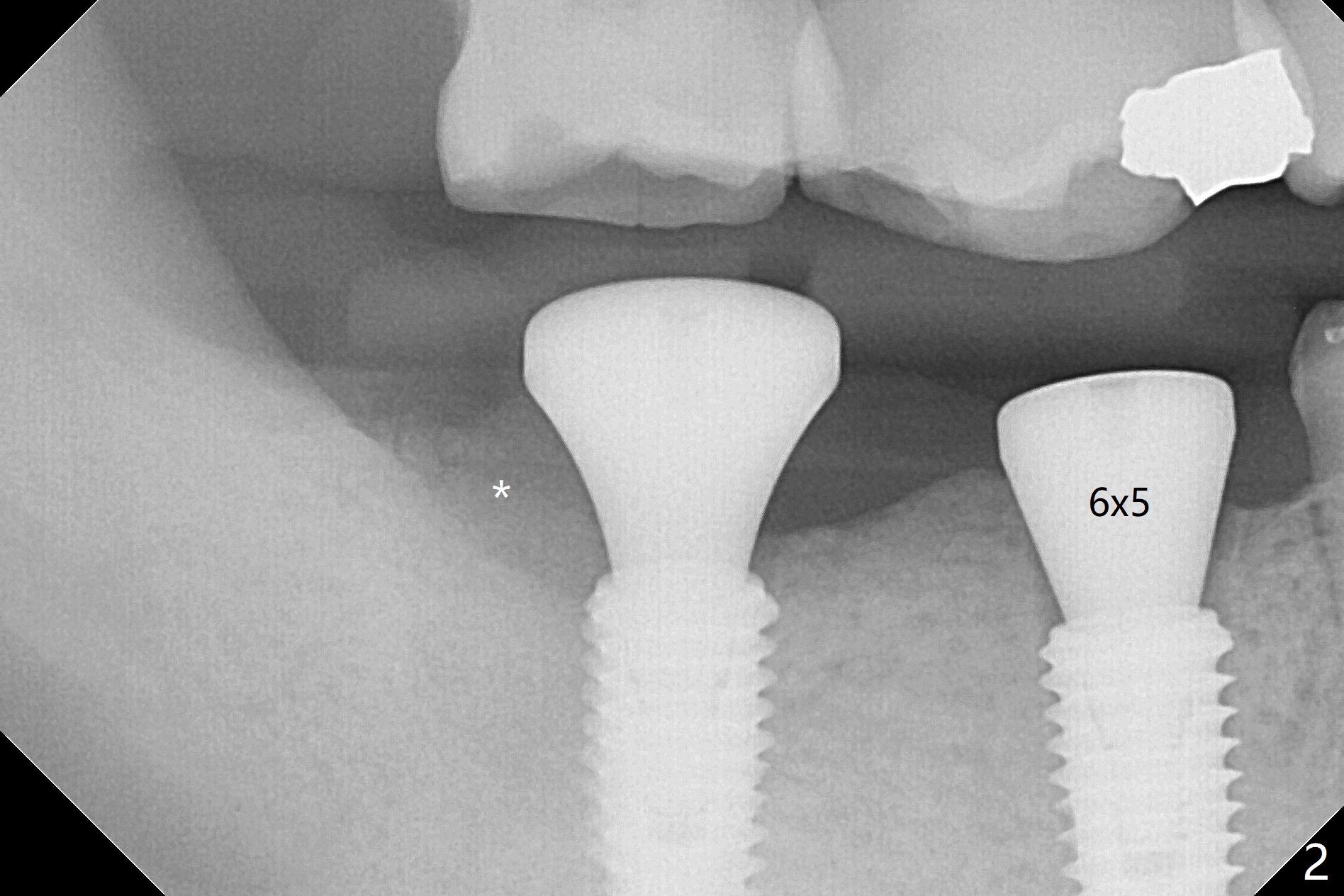
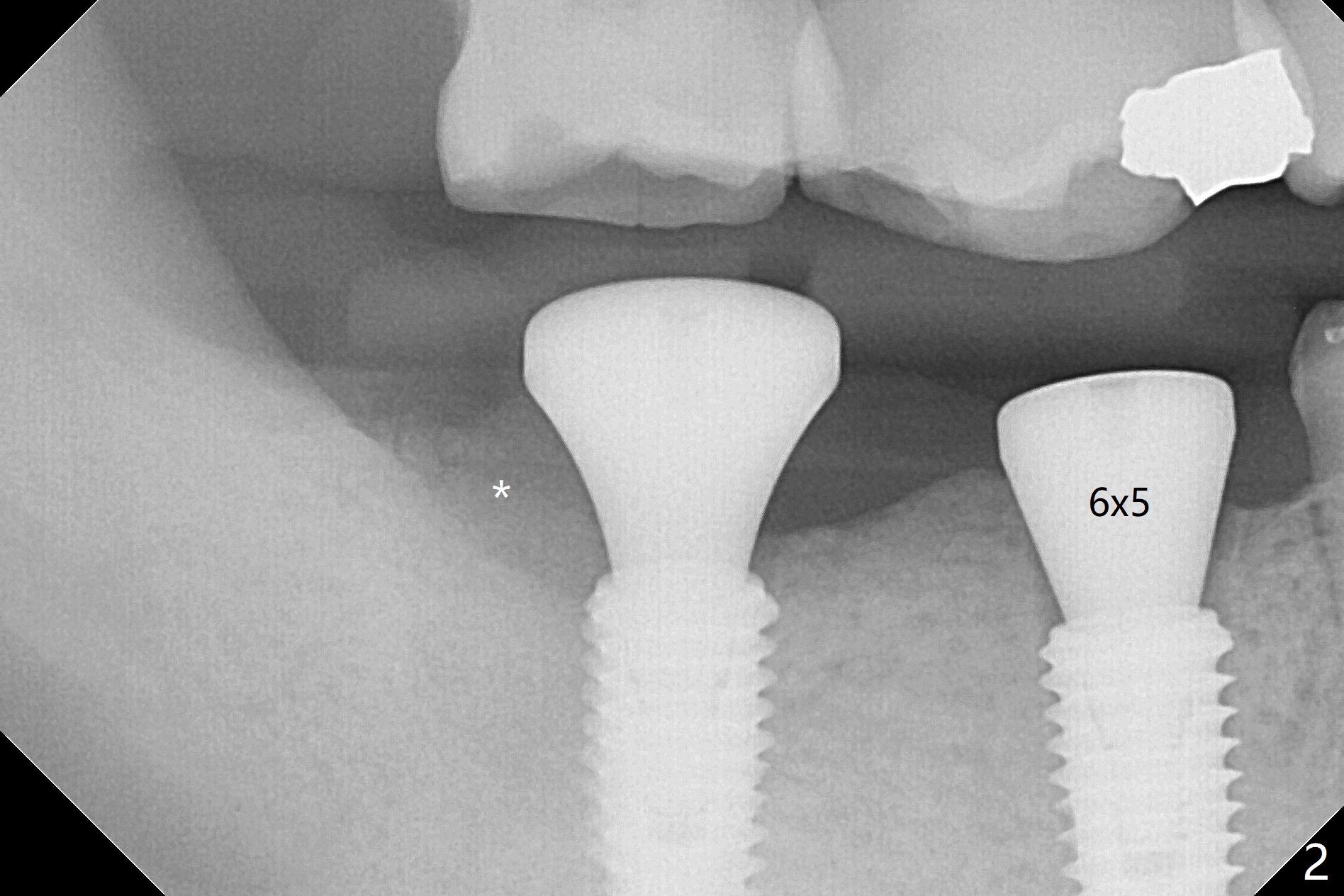
An endodontist refuses RCT retreatment at #29 because of short root. The patient is hesitant about apicoectomy. After discussion of advantages and disadvantages of the latter vs. extraction and implant, the patient chooses the extraction. The latter turns out to be smooth with socket preservation (Fig.4, 5 *). Immediately postop PA shows bone loss at #30 and minor degree around the apex of #31 implant (Fig.4 <), which is probably related with hard bone and bone necrosis due to heat. The headache disappears 1 week postop (Fig.6). The patient does not take pain medication. There is no percussion at #30 (Fig.7). The healing abutments are stable. The patient will return for #30 and 31 restoration nearly 4 months postop and 2 months post #29 extraction. Splinted provisional will be placed if the implants heal. Impression will be taken for #29 guide 4 months post socket preservation. After re-analysis of CT, it appears that a long implant (4x15 mm to gain 3.9 mm fixation in the native bone) will be placed free hand at #29 four months post socket preservation (Fig.8). The bone loss around the implants at #30 and 31 persists 3.5 month postop, while the socket heals at #29 2 months post socket preservation (Fig.9). When the healing abutments with plaque are removed, there is granulation tissue around the gingival cuffs with tenderness. The abutments with heavy plaque (similar to that in Fig.7) are reloaded after cleaning with OHI. The patient returns for CT and impression for #29 guide 3.5 months post socket preservation and 5 months post implant placement. While bone necrosis remains severe at #30, the socket at #29 seems to have healed (Fig.10). Oral hygiene improves with healthy gingiva, but there is tenderness when a cementation abutment is placed. Implant design before and after extraction at #29 (Fig.11,12). Gingiva becomes inflamed at #31 when a splinted provisional is being worn to intrude the opposing supraerupted teeth; bone resorption remains severe in the previous distal socket and the mesial necrotic area (Fig.13 S, N). Pain persists after placement of a healing screw. In spite of severe bone loss, especially distal, the buccal plate is present. When the implant at #31 is removed, there is a large defect with granulation tissue apicobuccal to the buccal plate, corresponding to the presumptive mesial necrotic area (Fig.13,14 N). Vanilla graft mixed with PRF ("sticky bone" too rigid) is placed in the defect, followed by a piece of PRF membrane and 6-month one. The pain appears not to reduce and nearly 1 month later transfers to the buccal of #30.
Return to Lower Molar Immediate Implant, Prevent Molar Periimplantitis (Protocols, Table), Armaments, 2nd Immediate with Guide Xin Wei, DDS, PhD, MS 1st edition 08/24/2018, last revision 06/16/2019