
.jpg)






%20heavy%20palatal%20reduction.jpg)

 |
 |
 |
 |
||
 |
.jpg) |
 |
 |
||
 |
 |
 |
 |
 |
|
 |
 |
 |
 |
||
 |
 |
 |
 |
||
 |
 |
%20heavy%20palatal%20reduction.jpg) |
 |
||
 |
 |
||||
Repair Apical Buccal Plate M
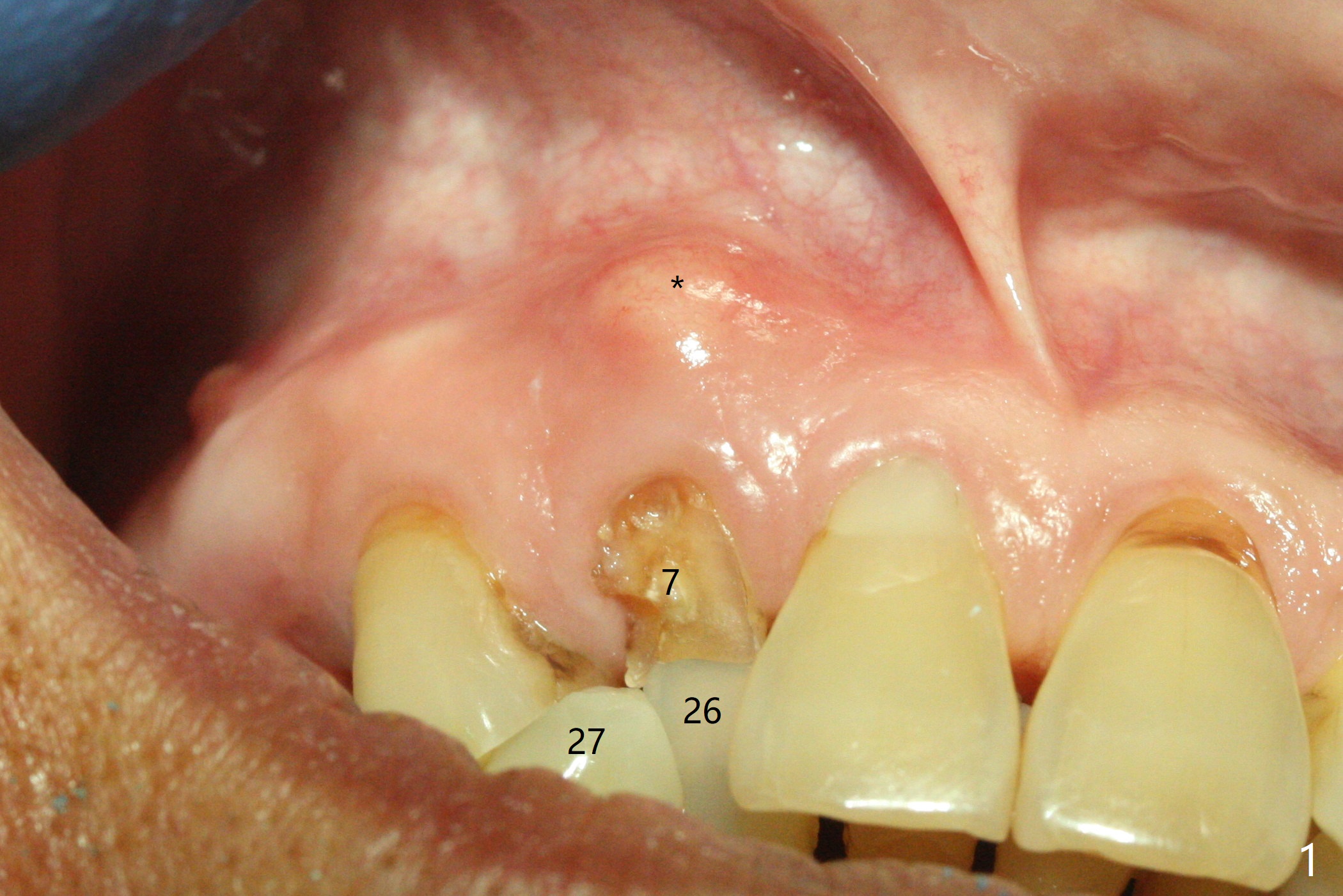
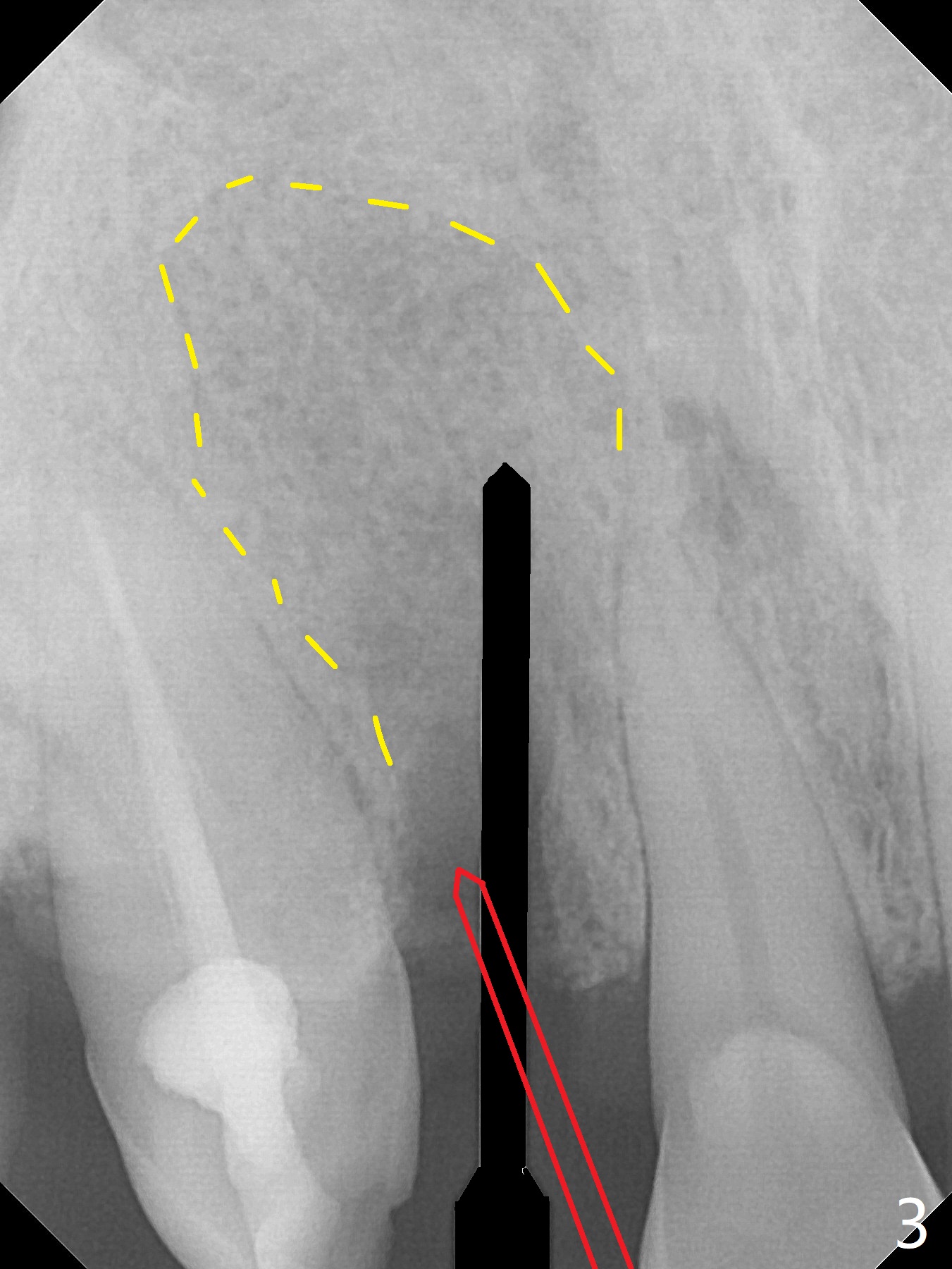
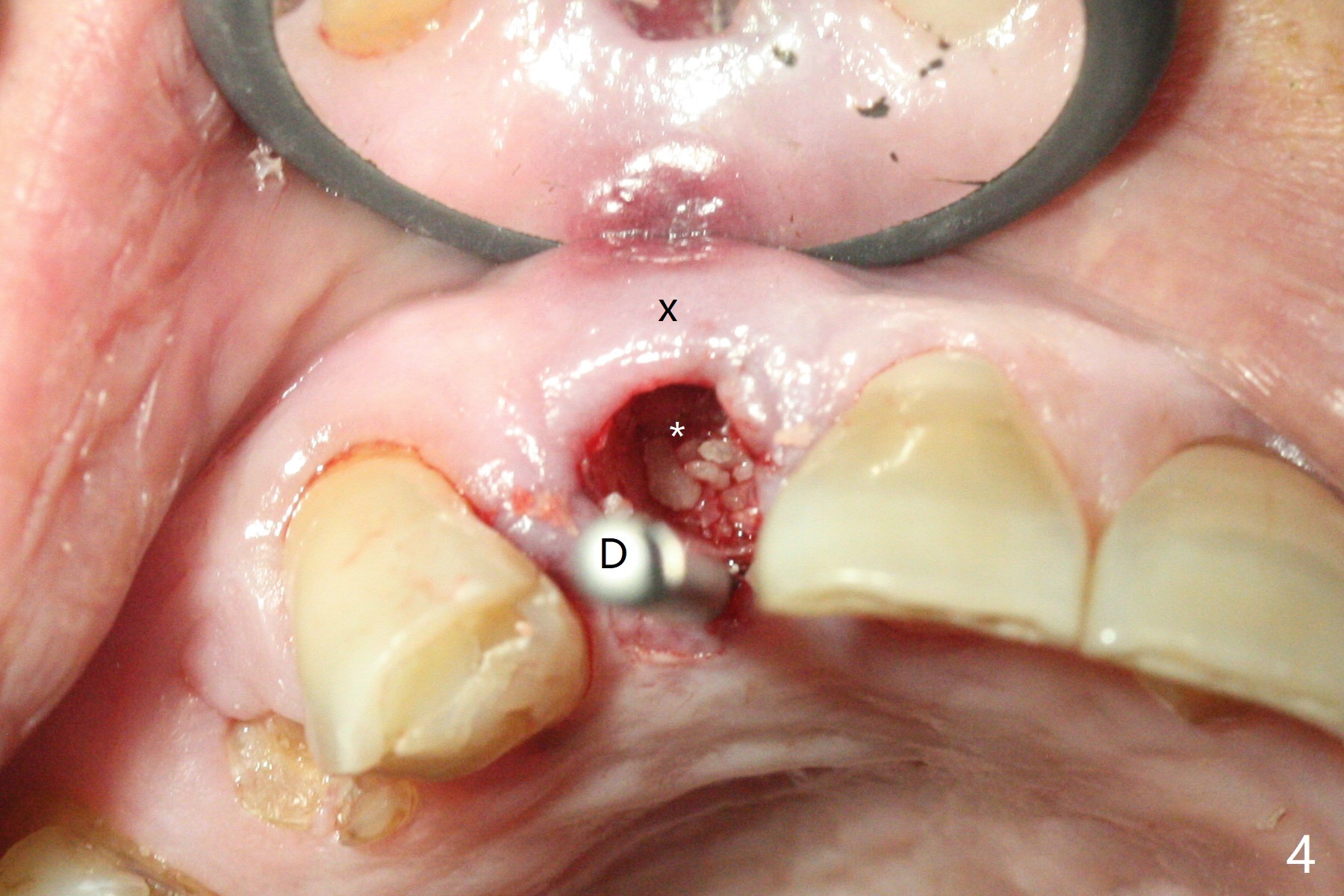
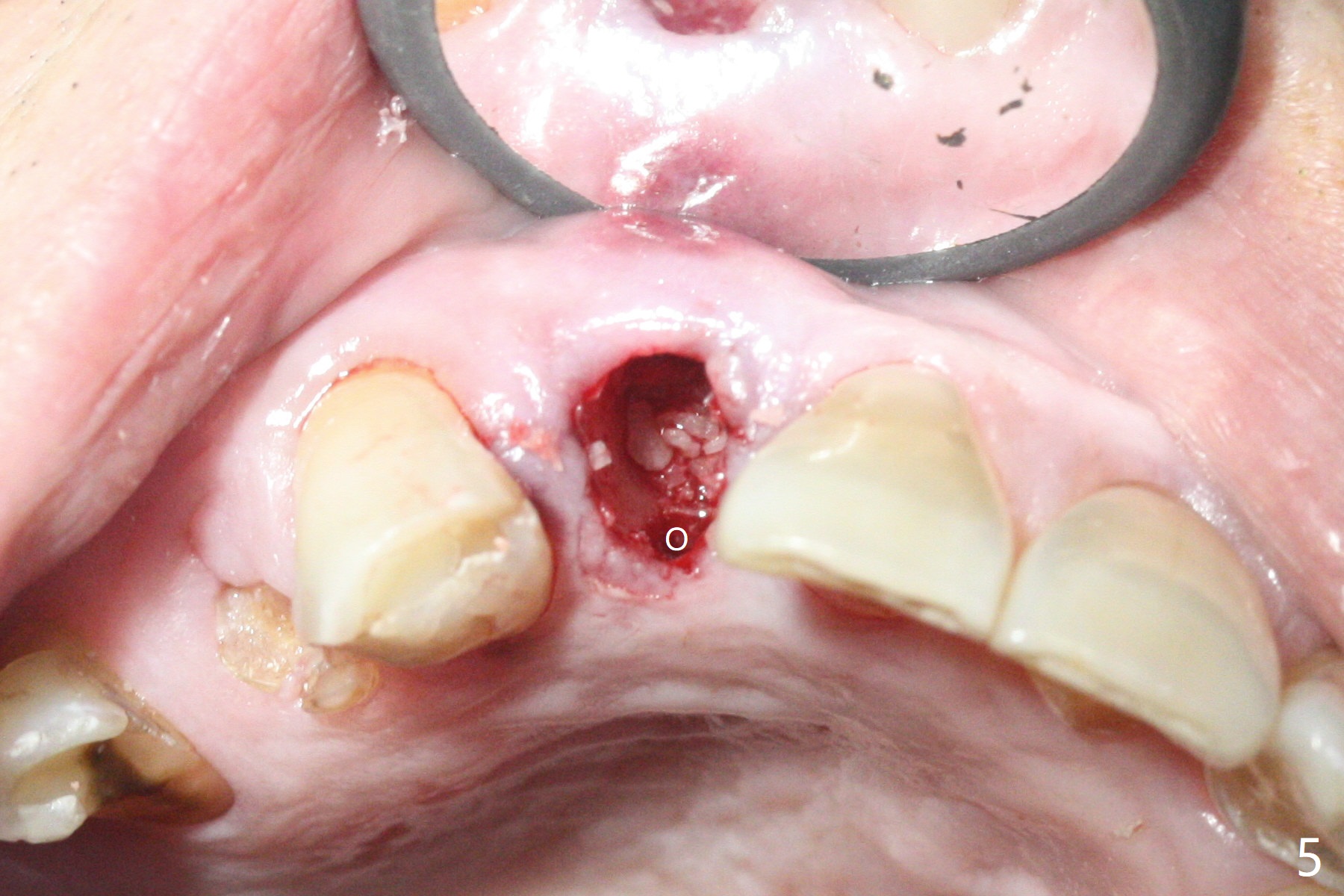
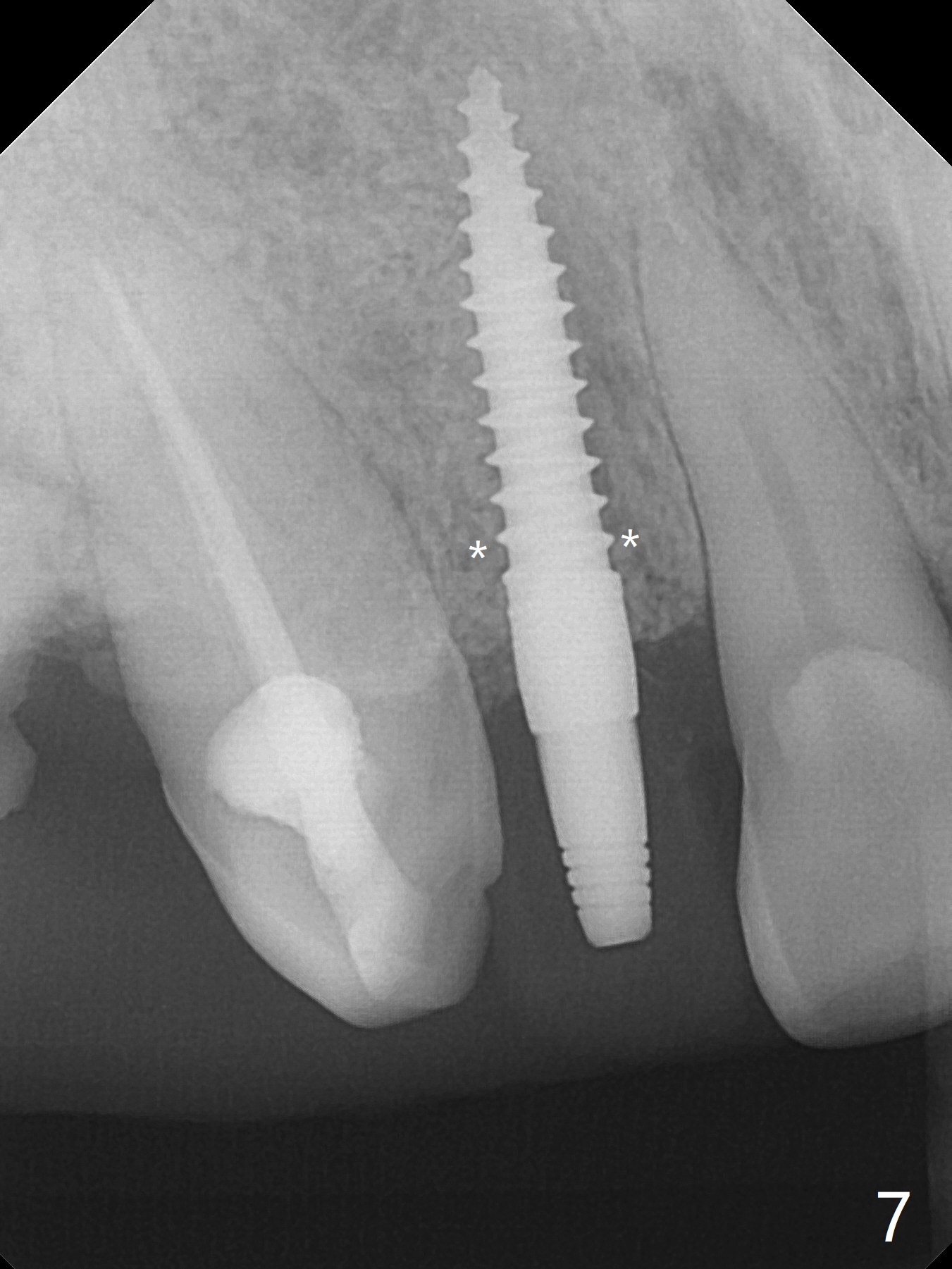
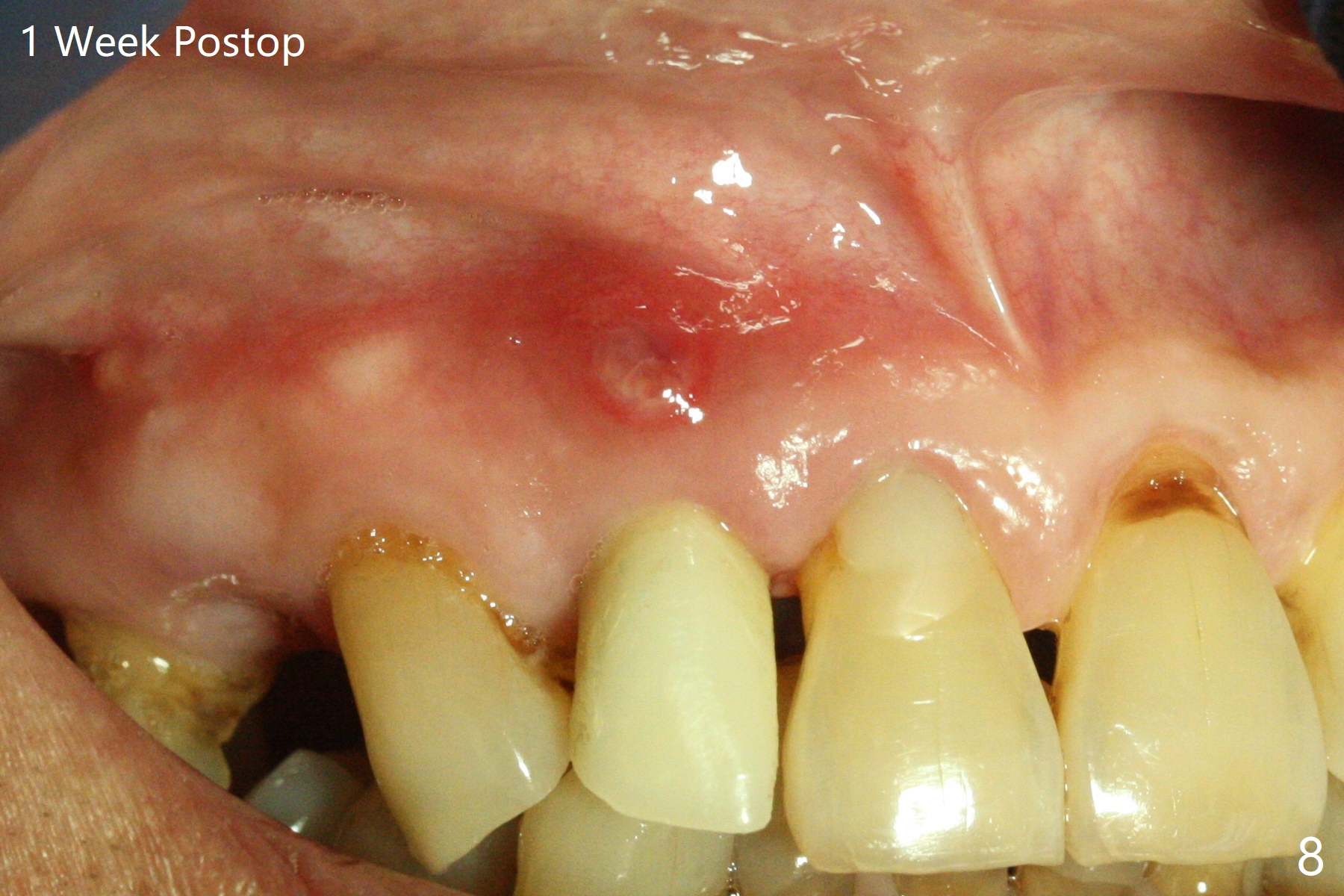
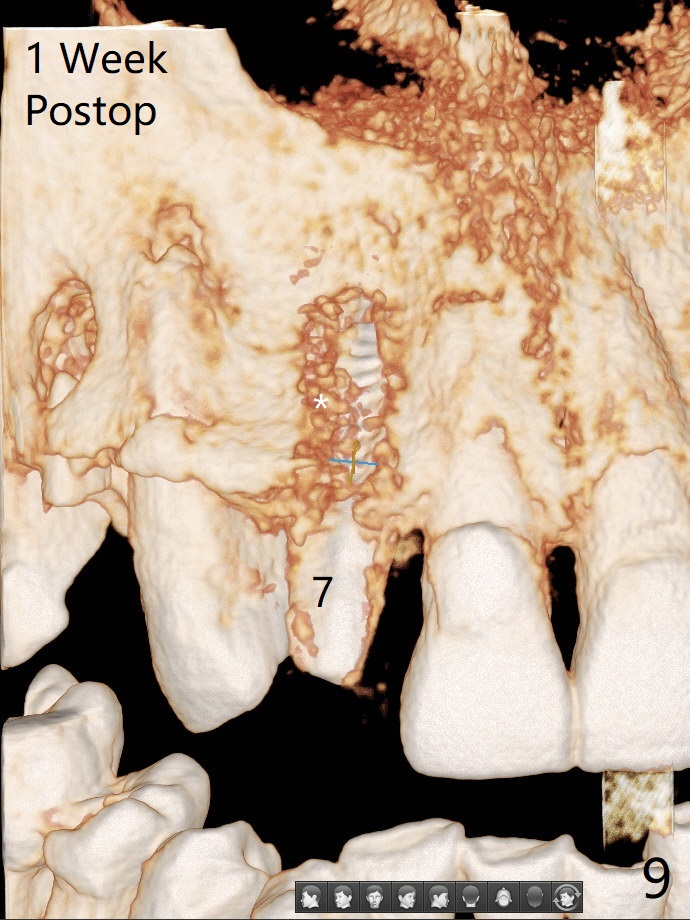
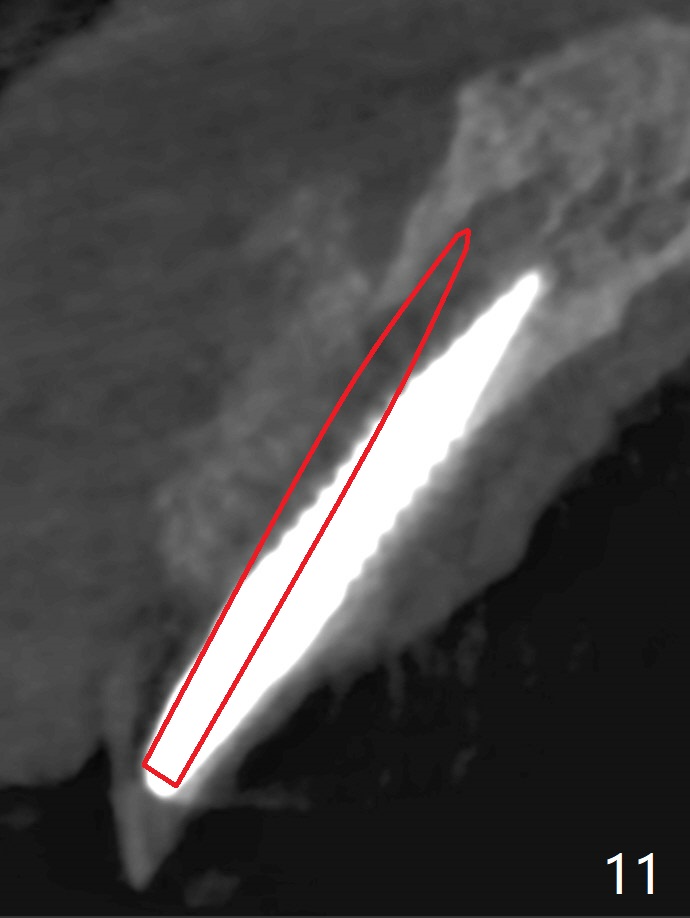
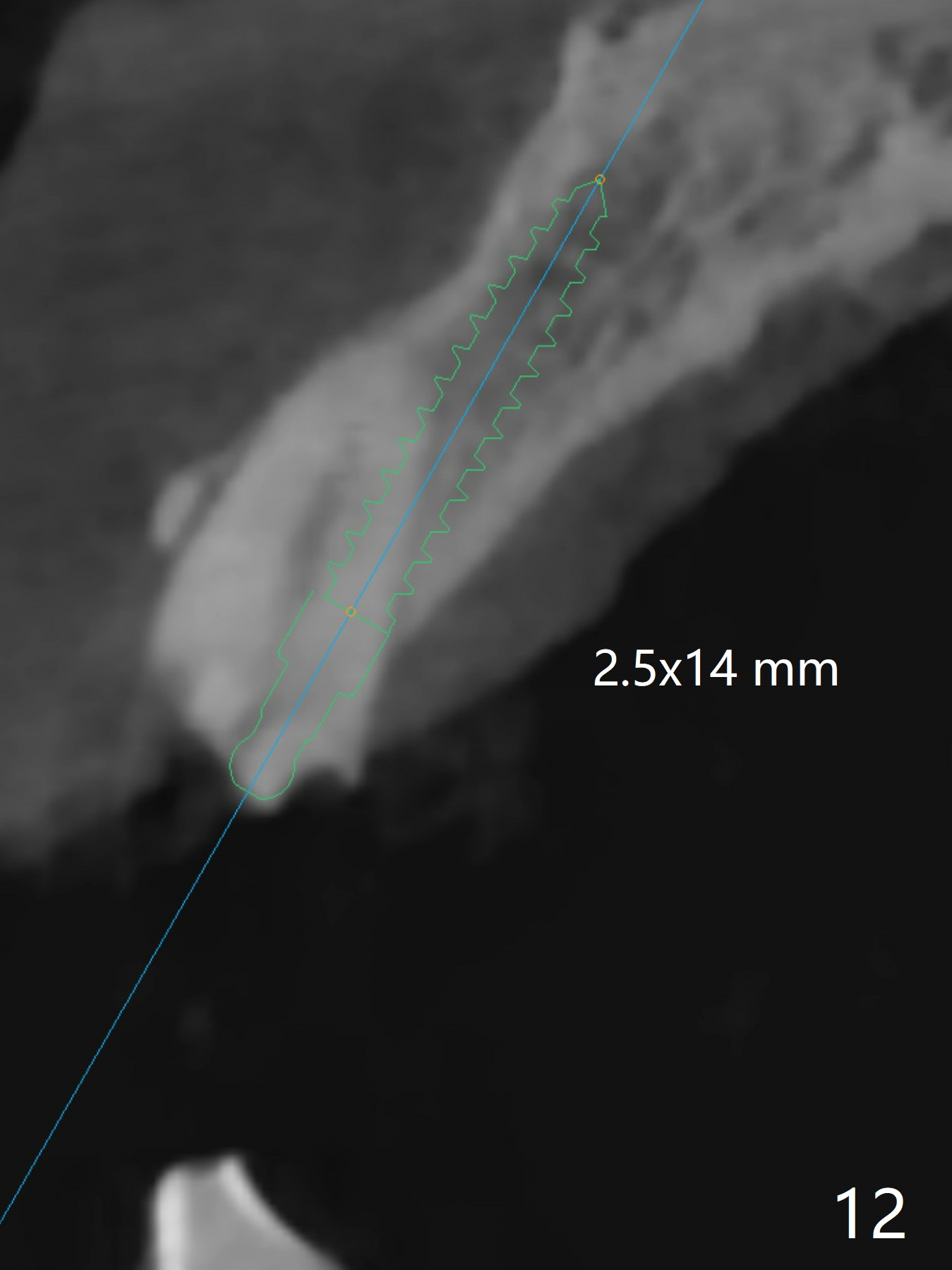
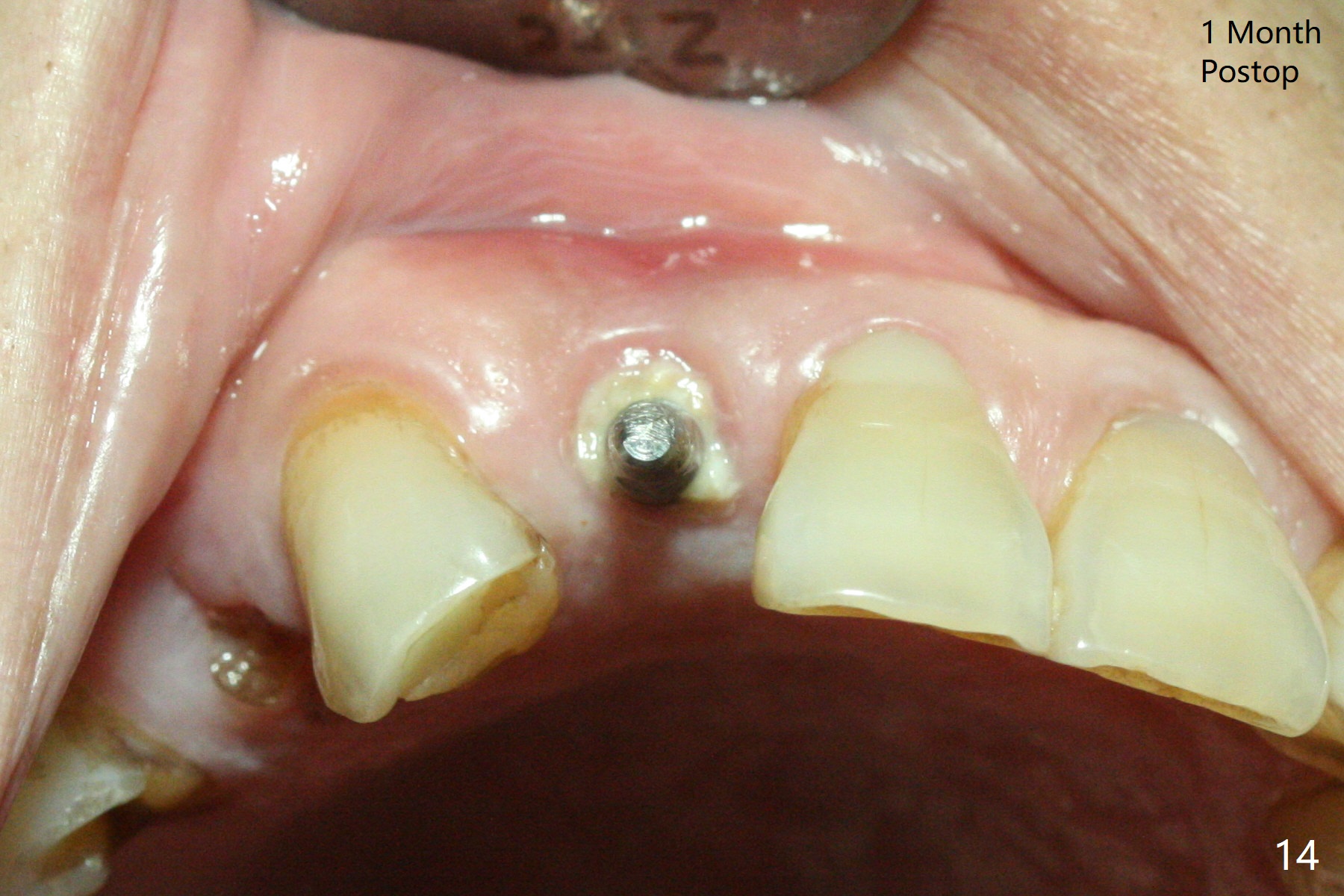
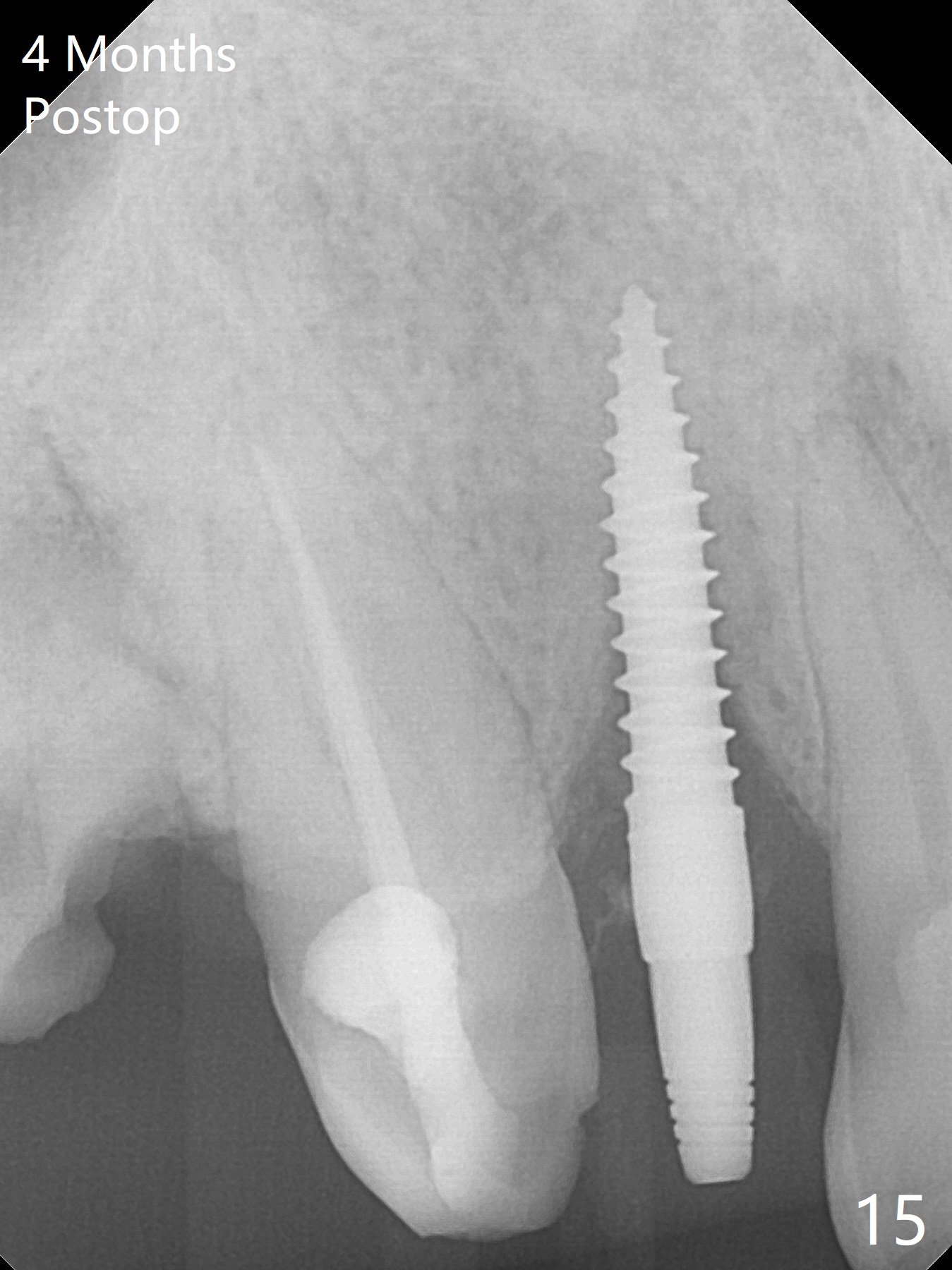
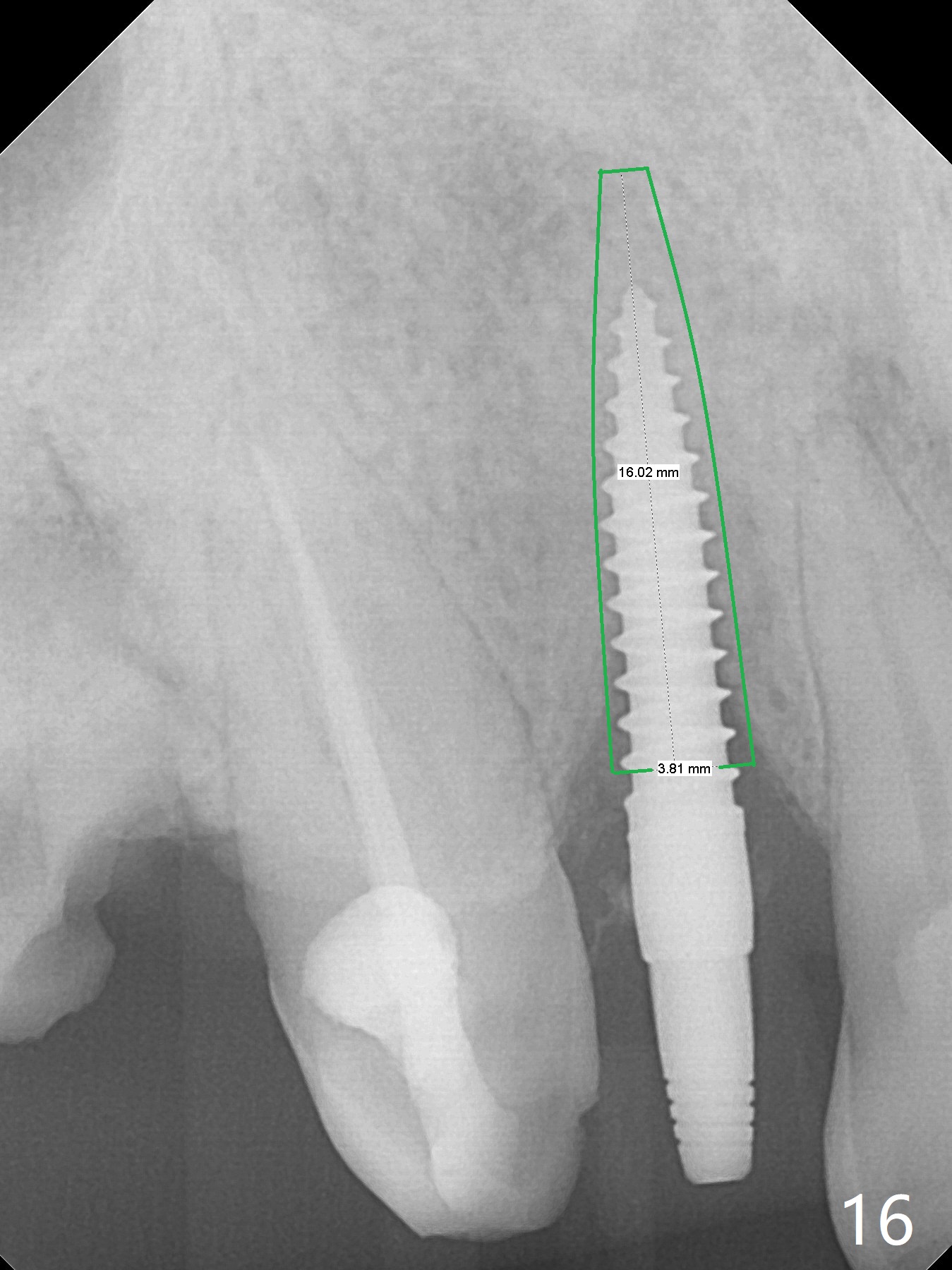
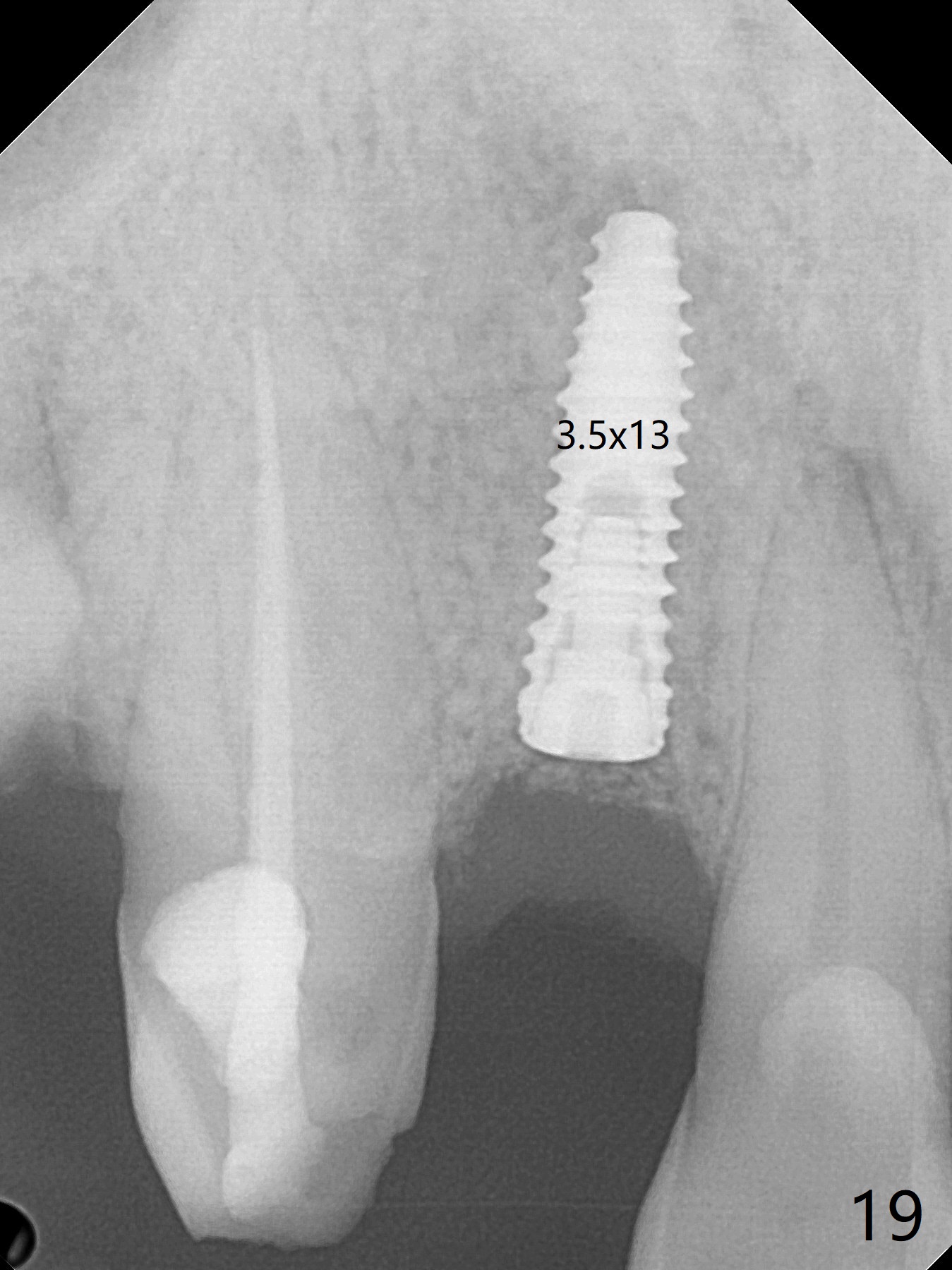
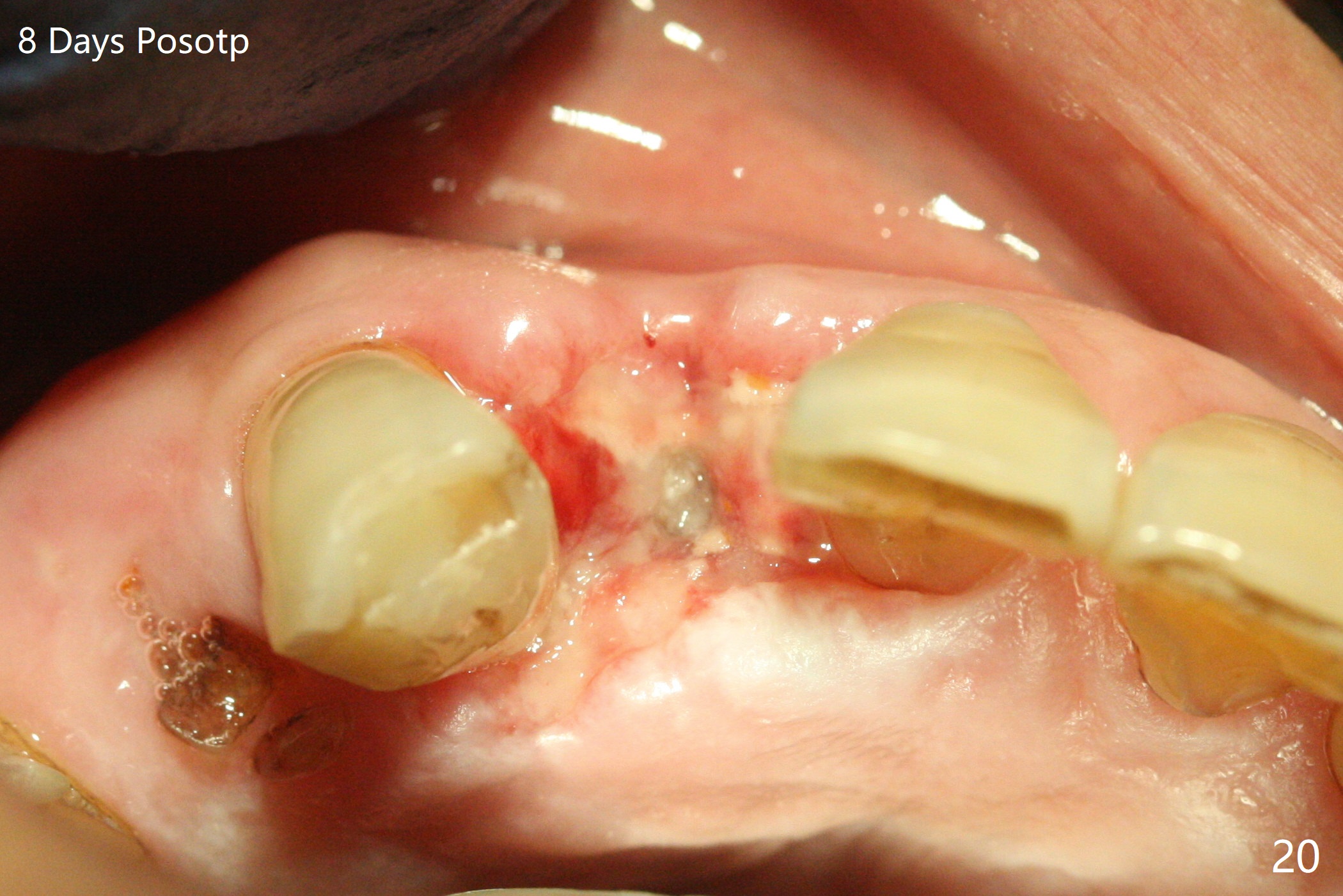
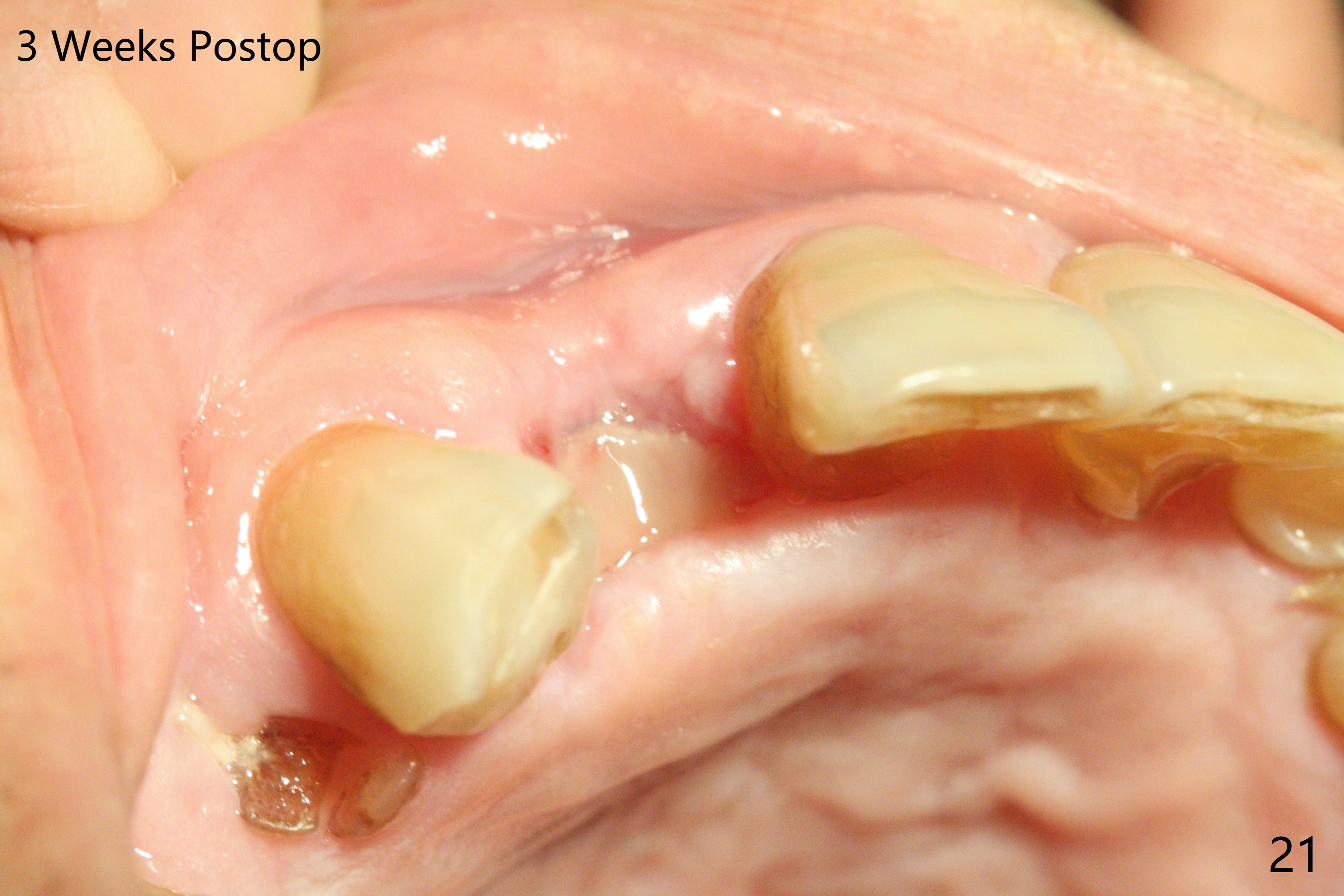
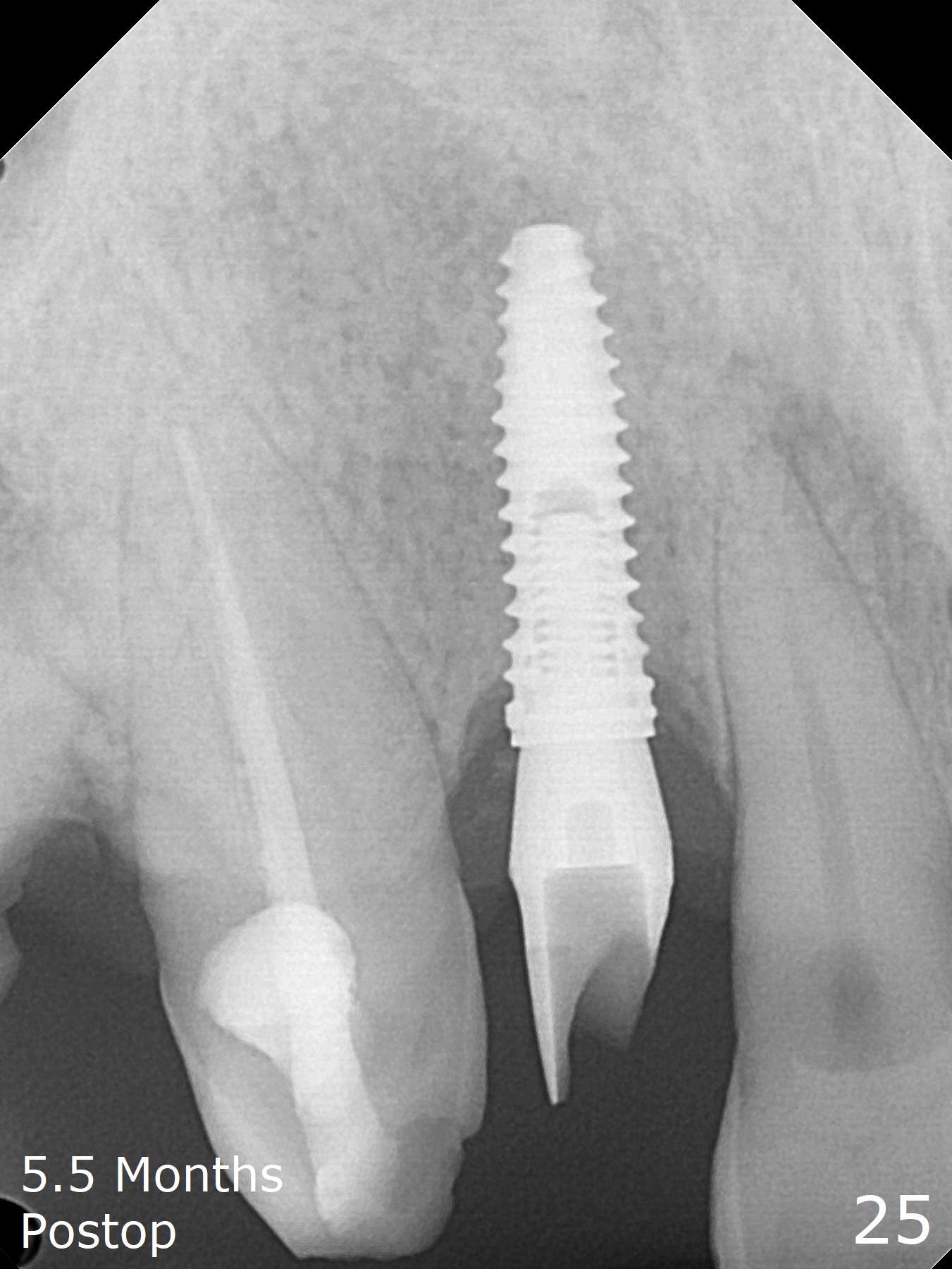
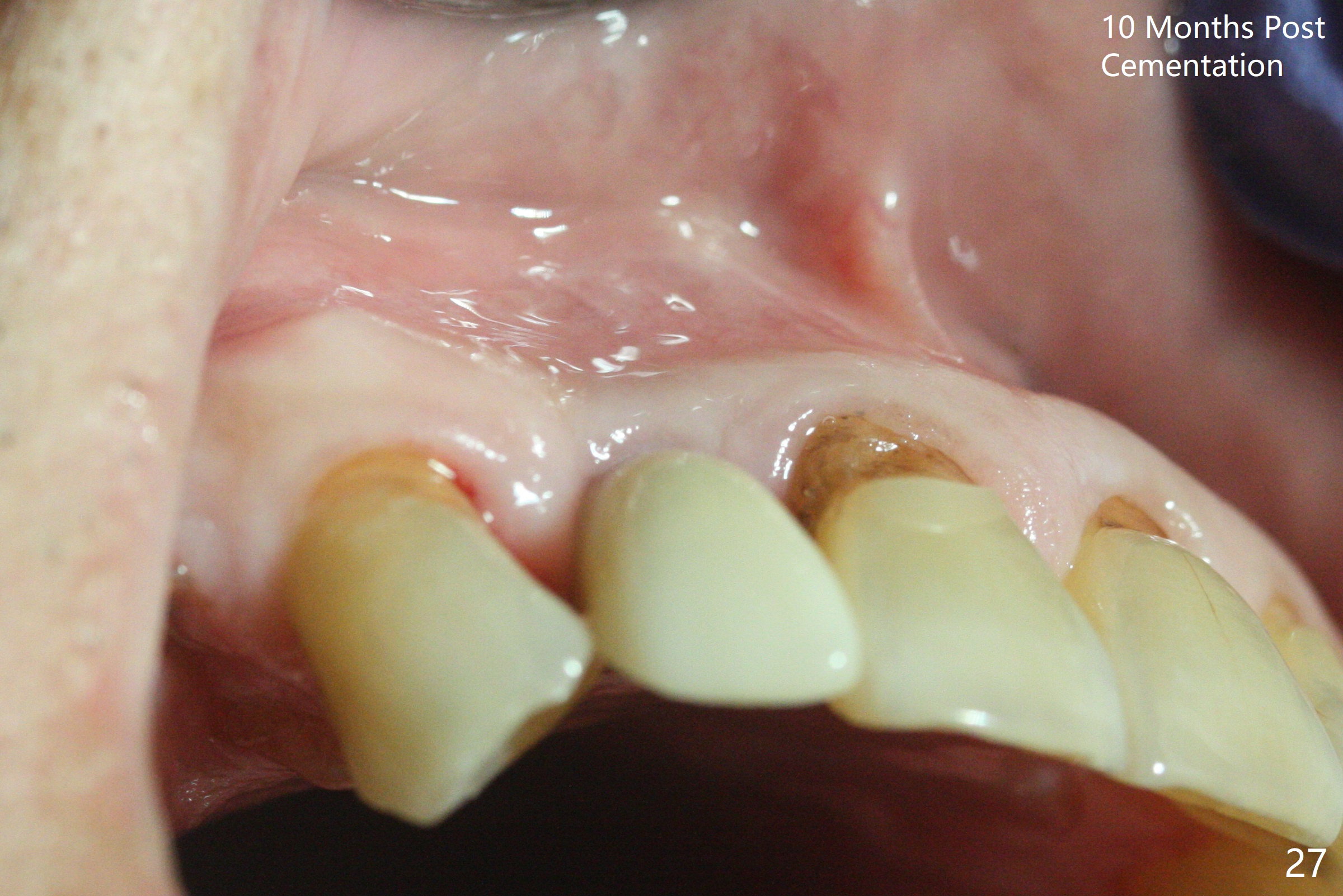
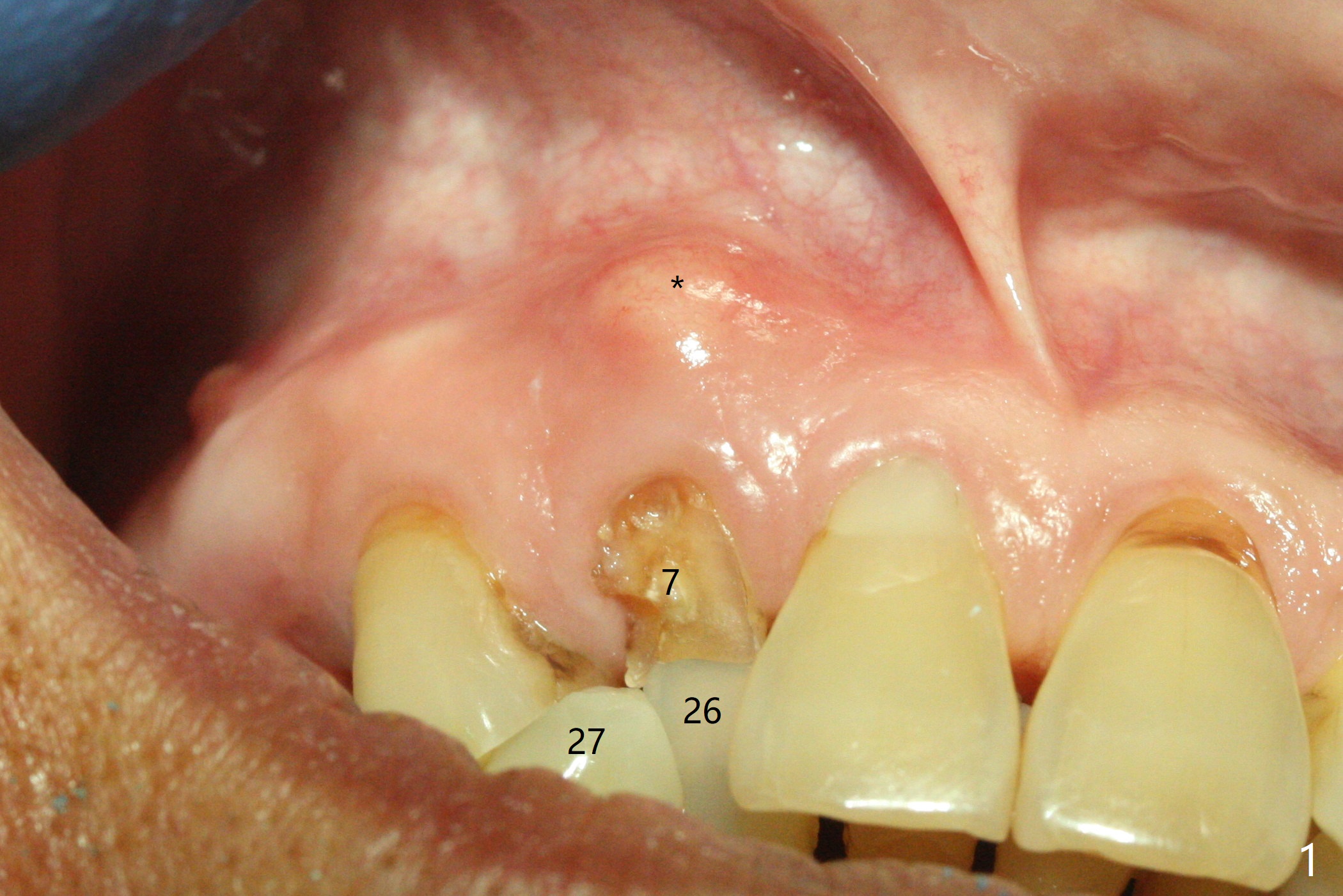
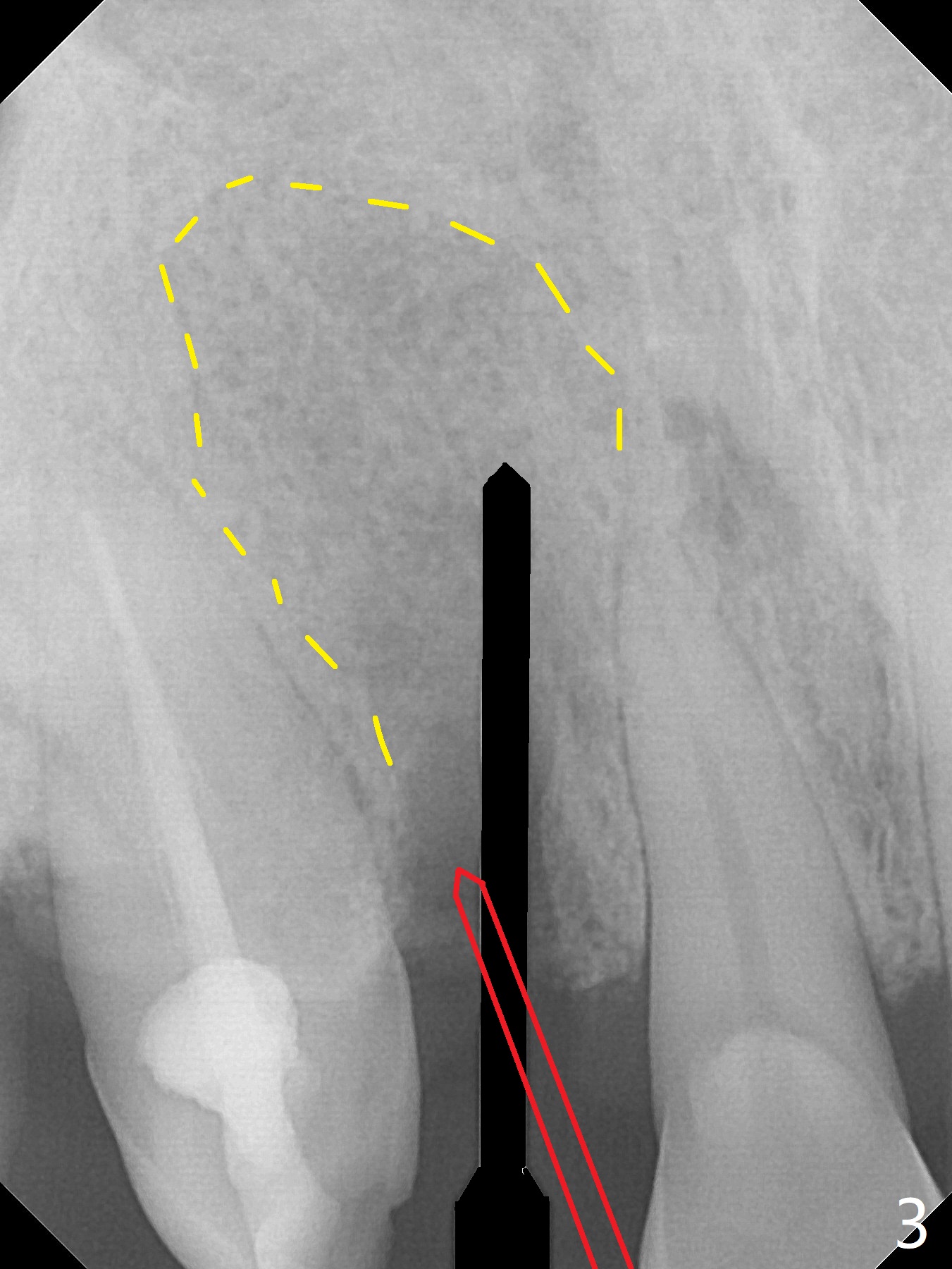
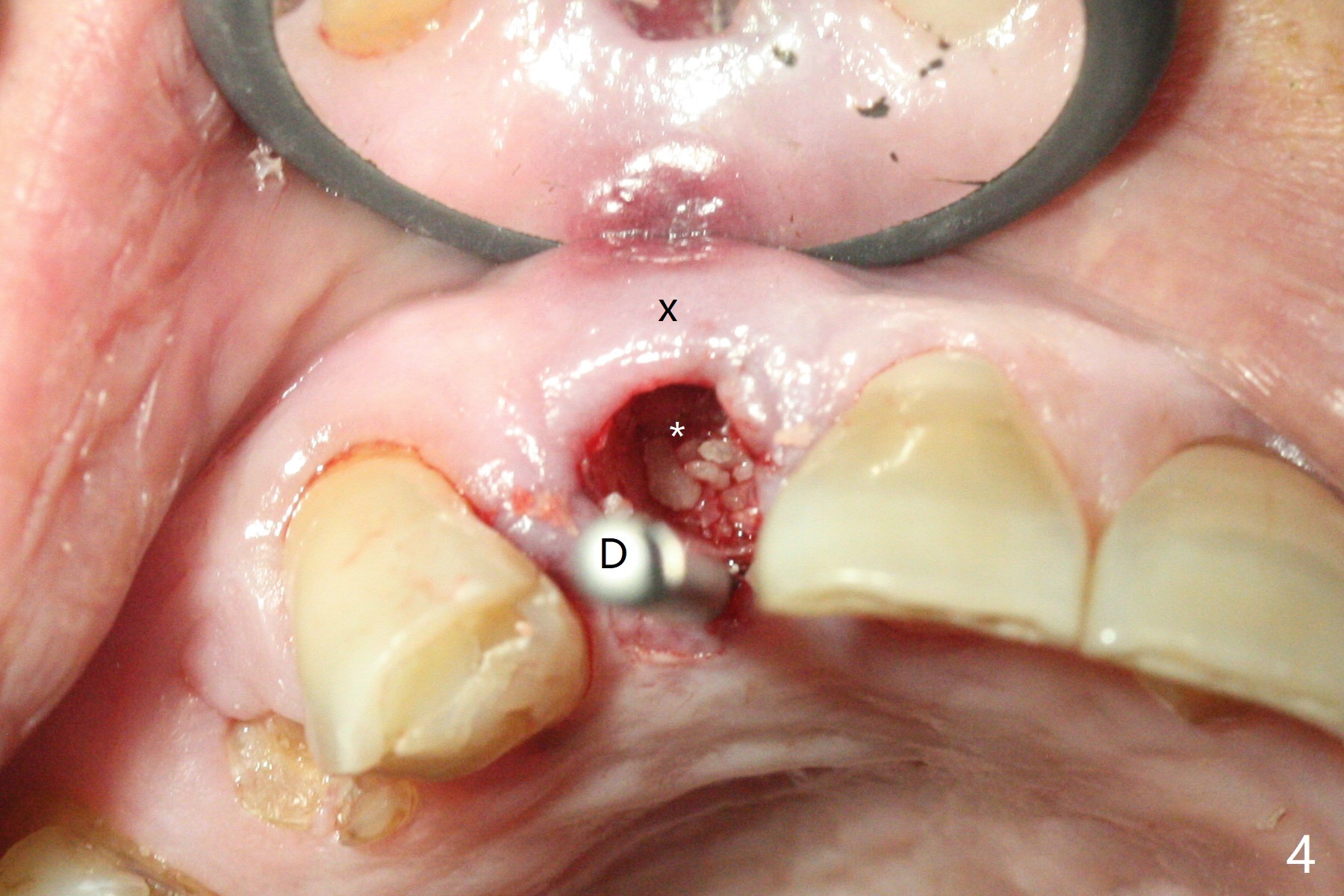
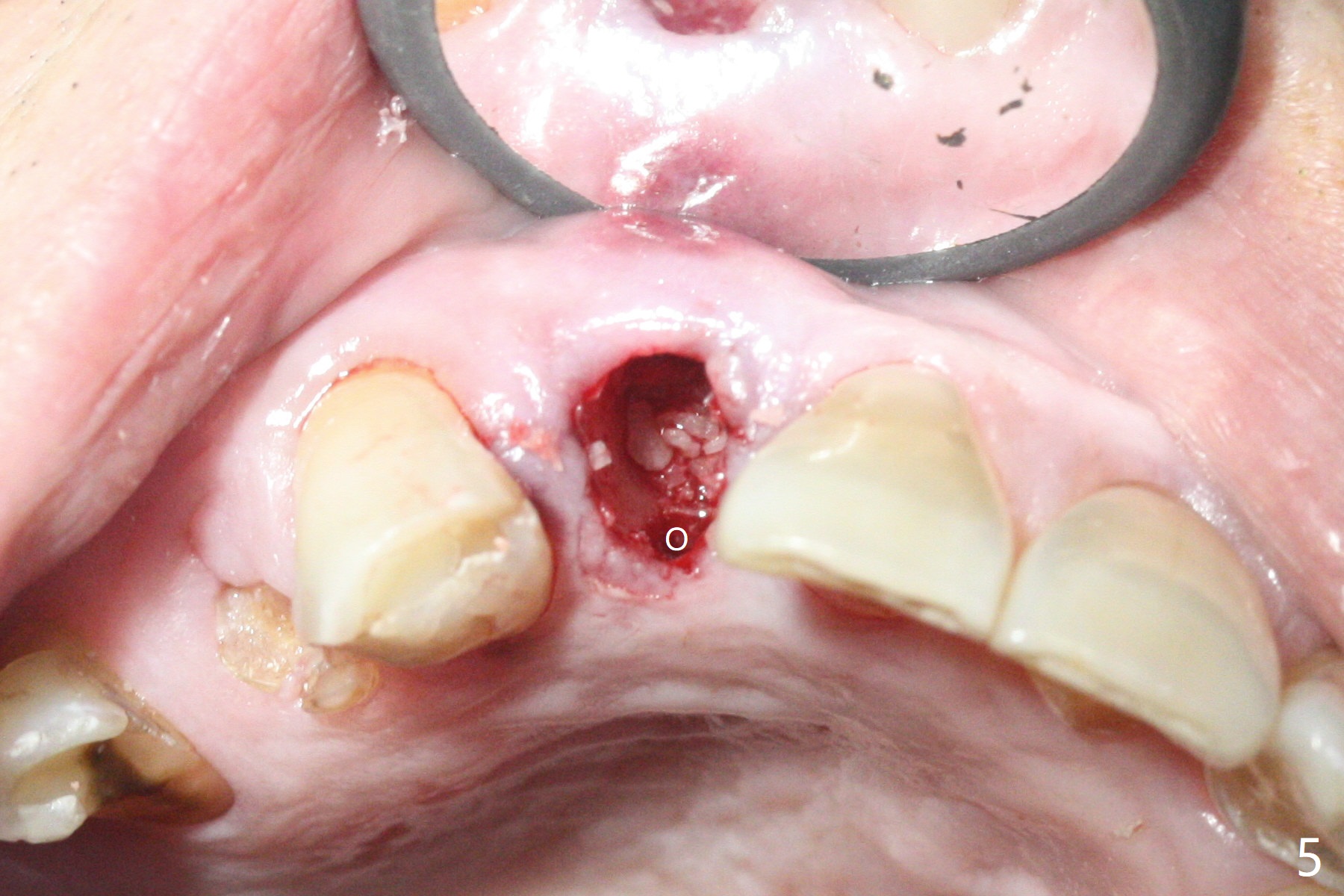
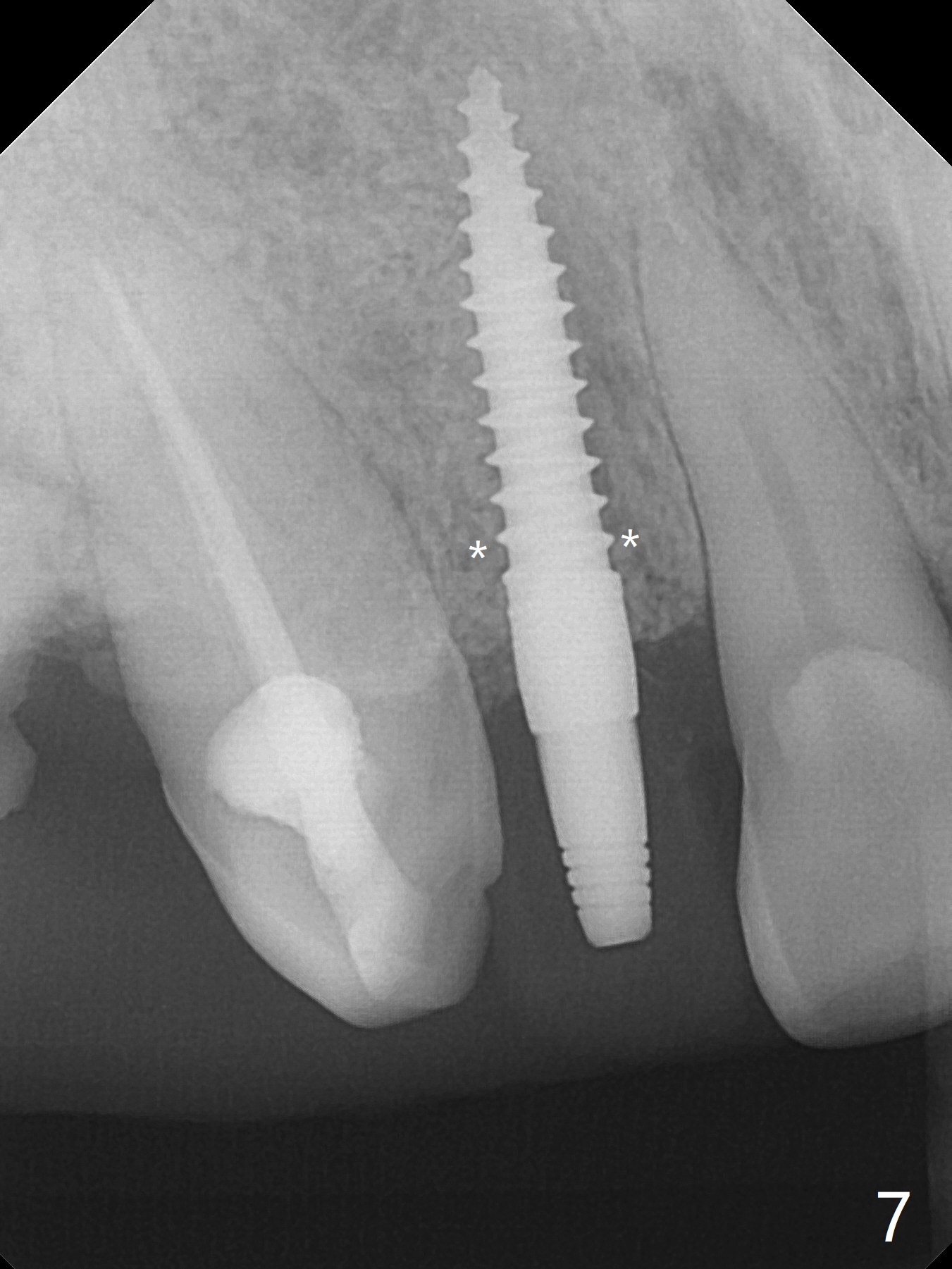
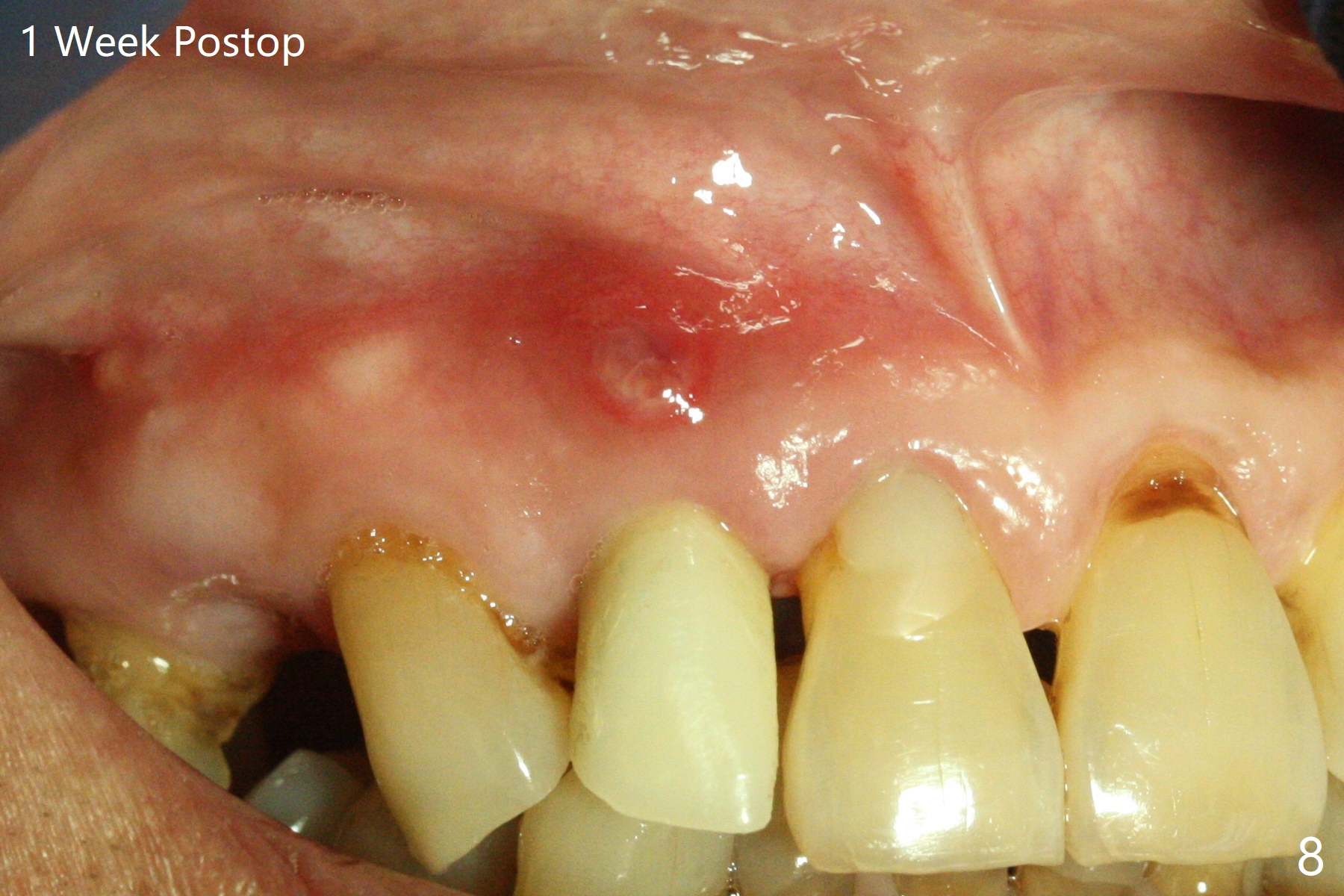
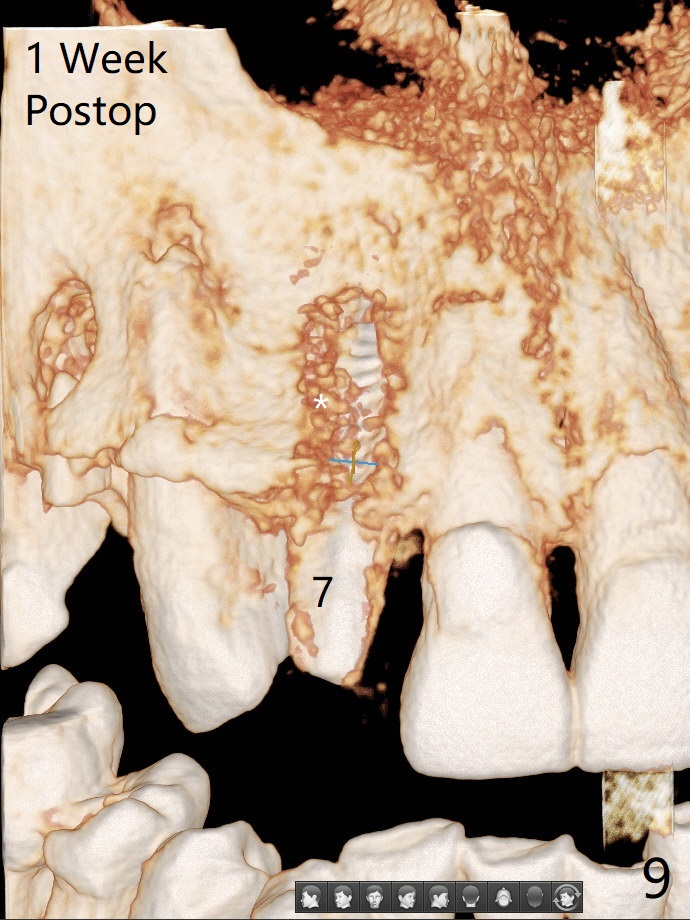
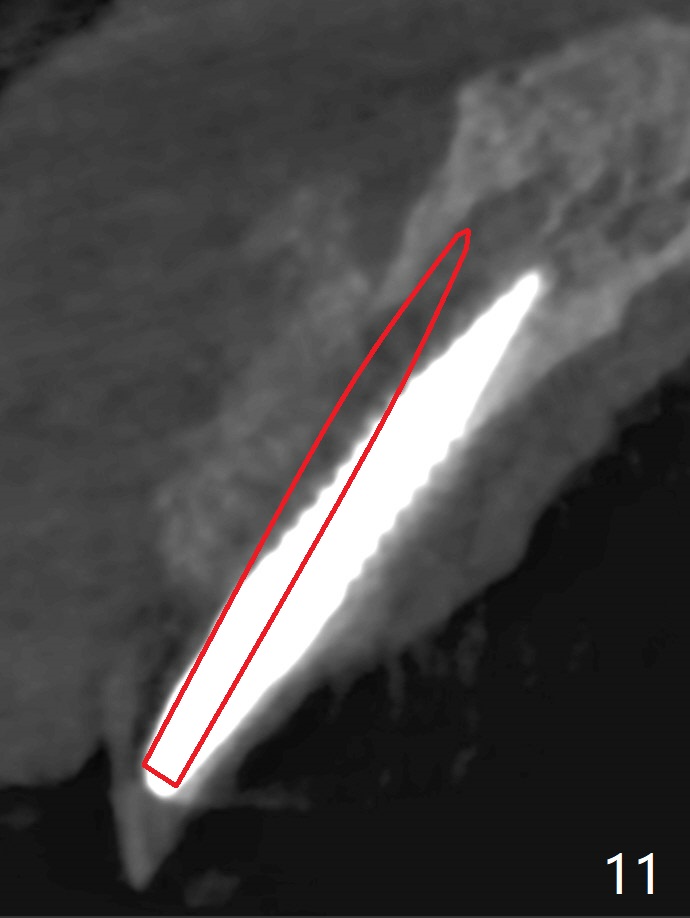
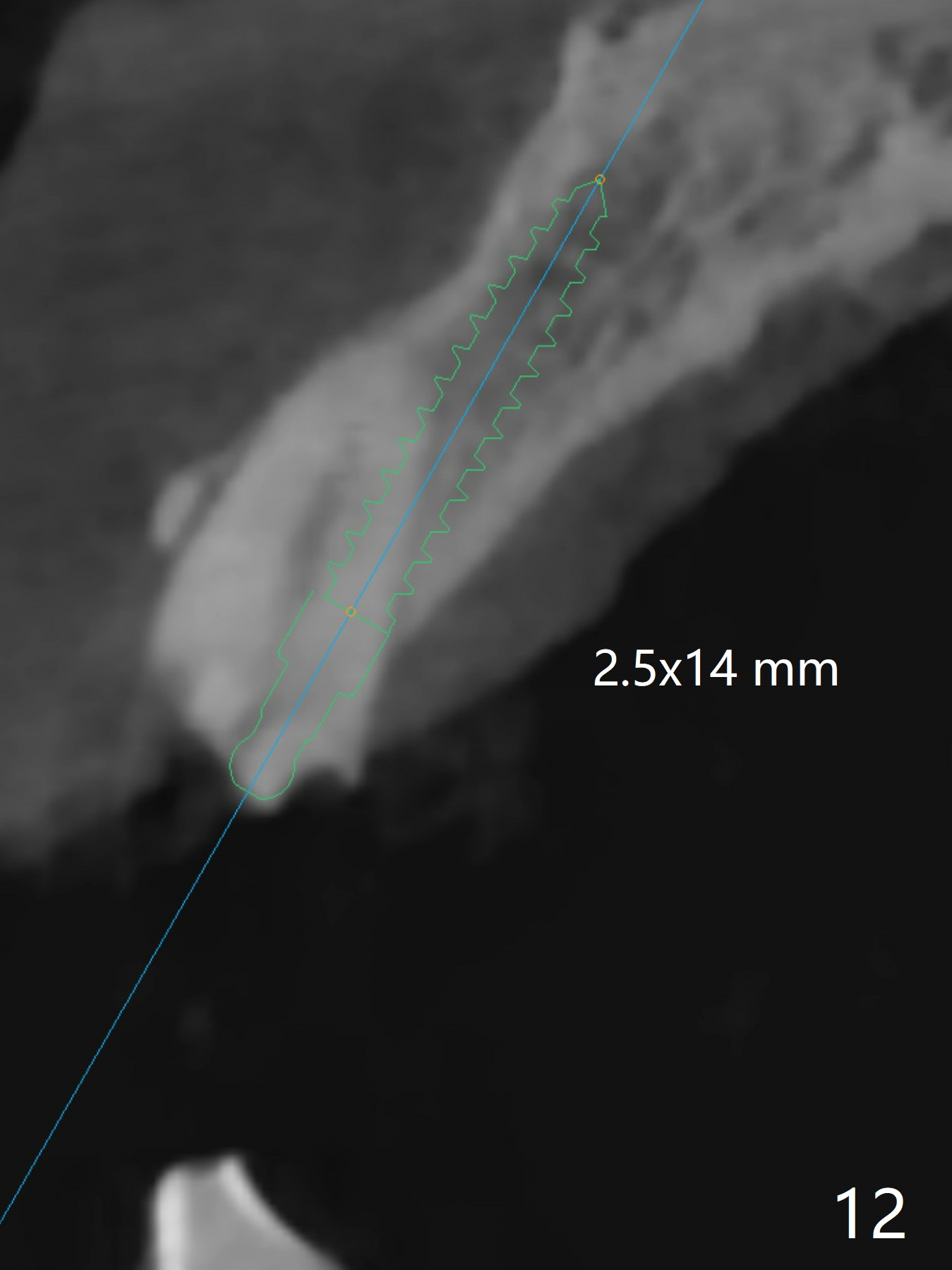
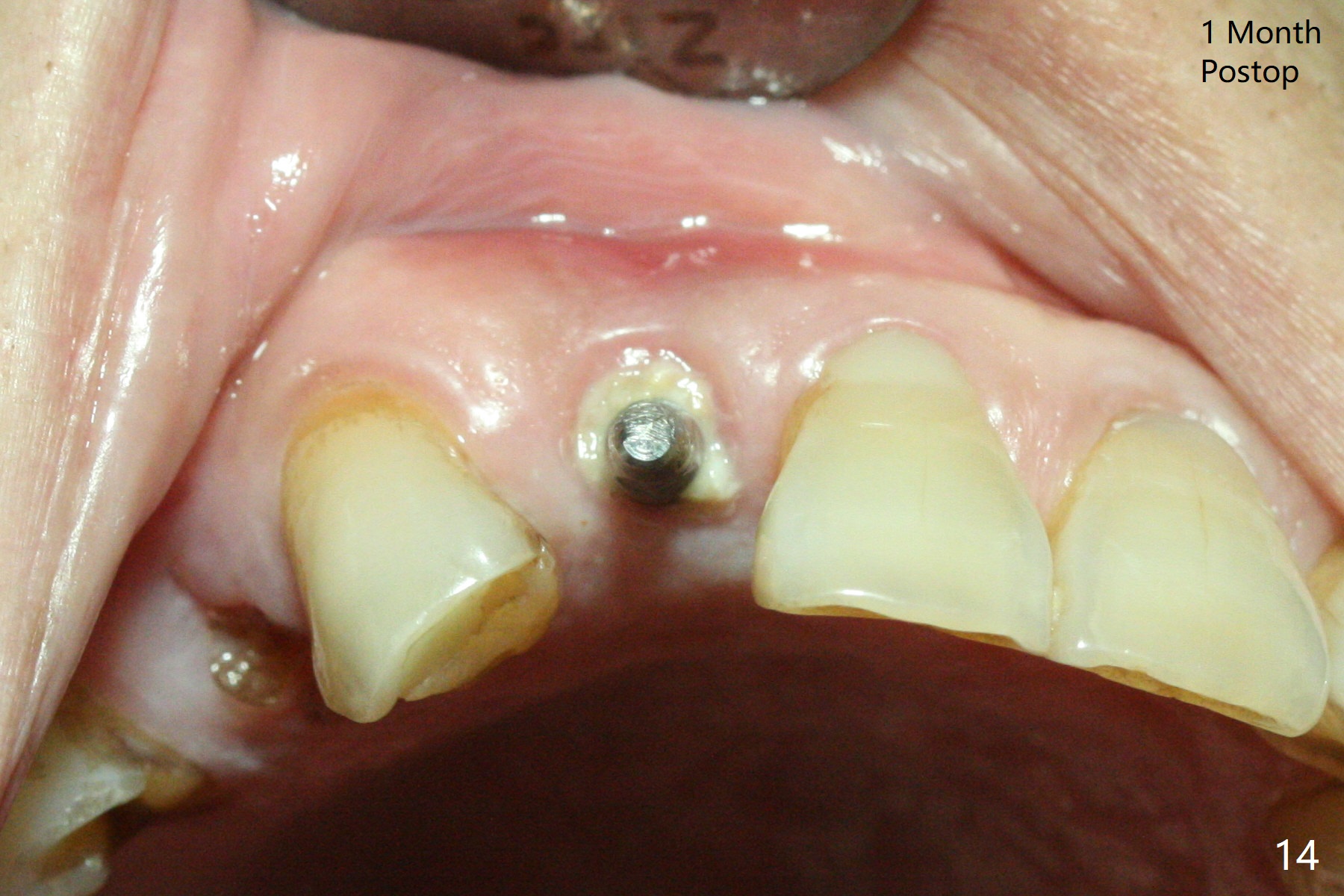
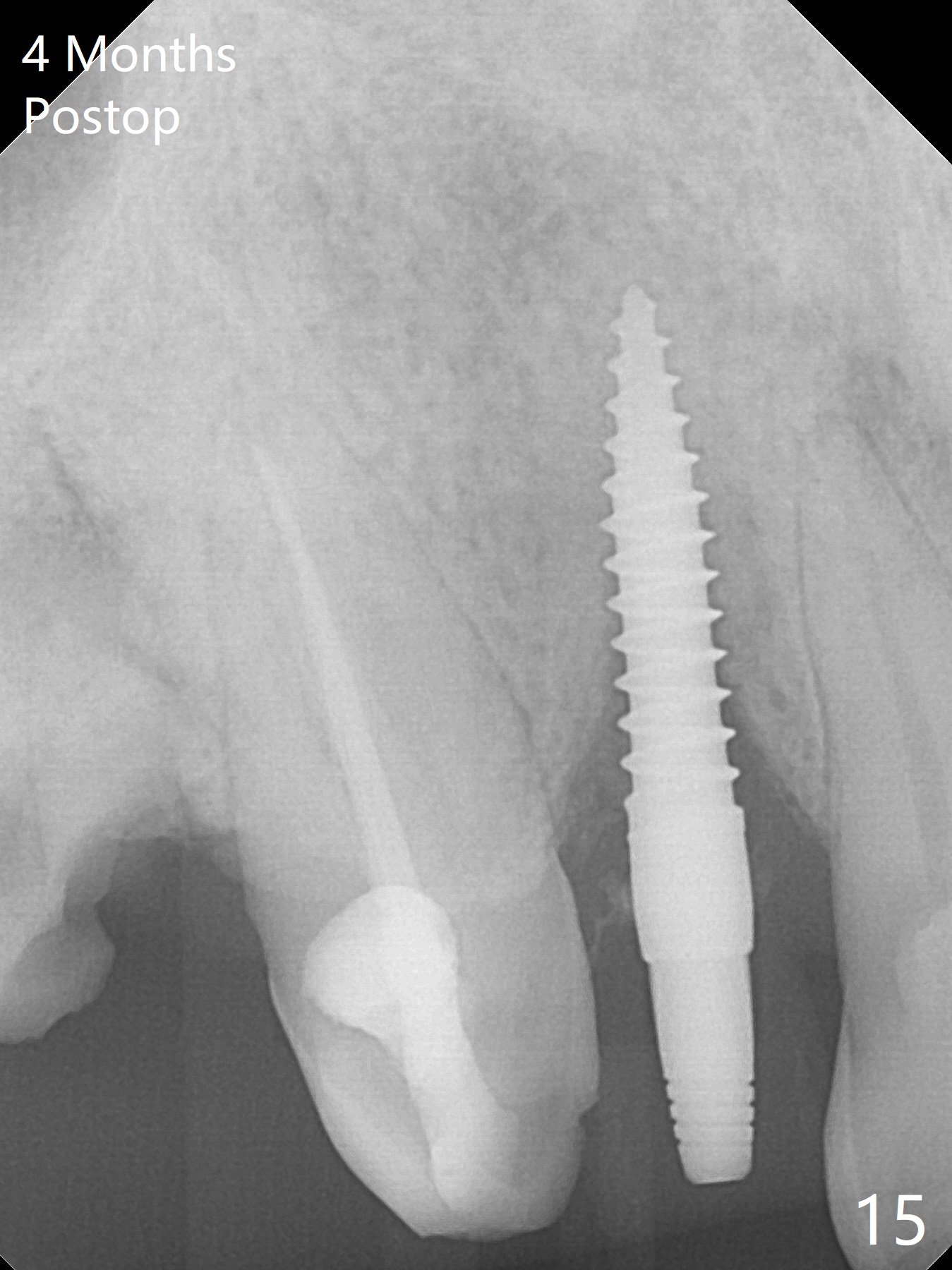
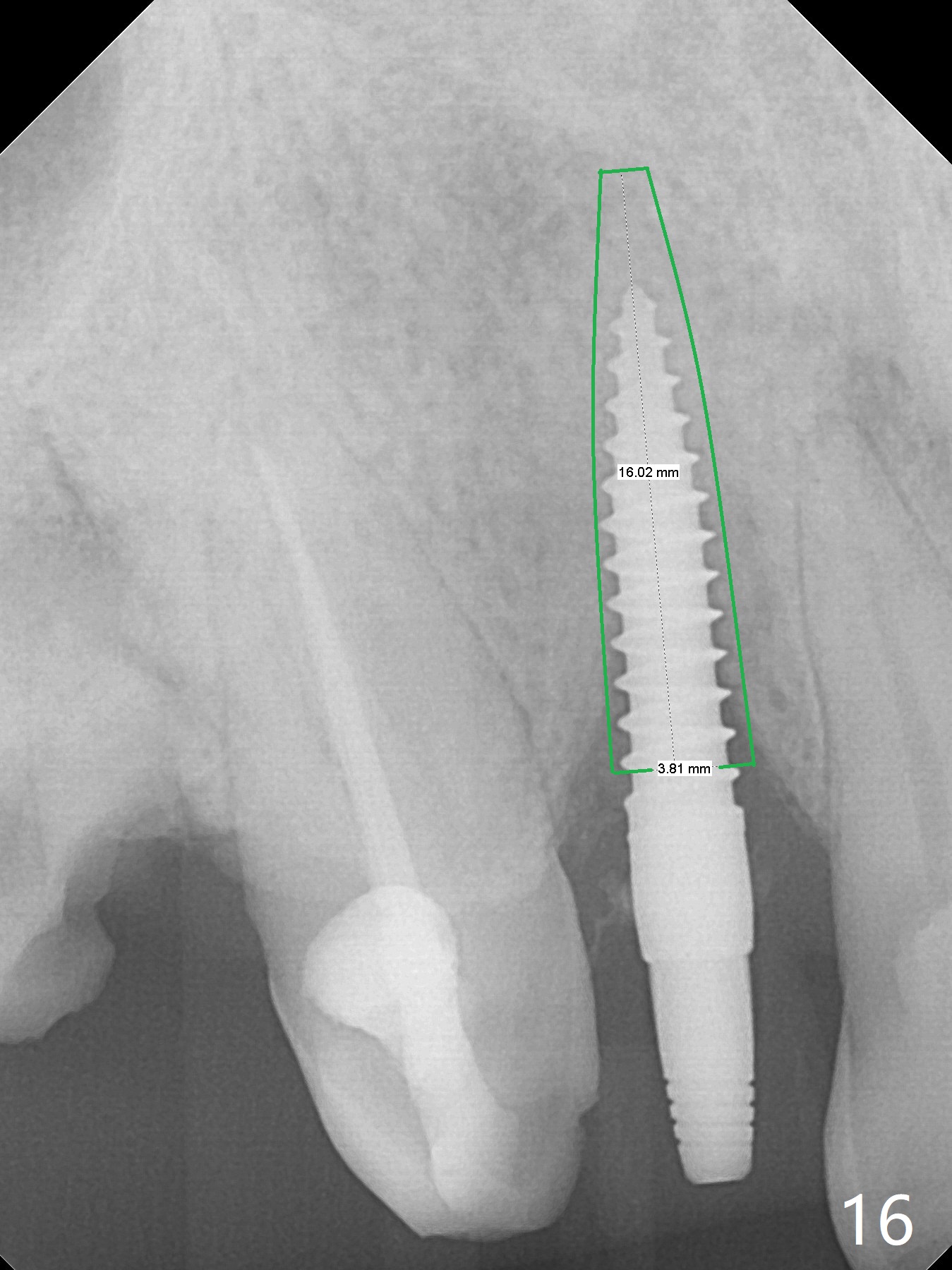
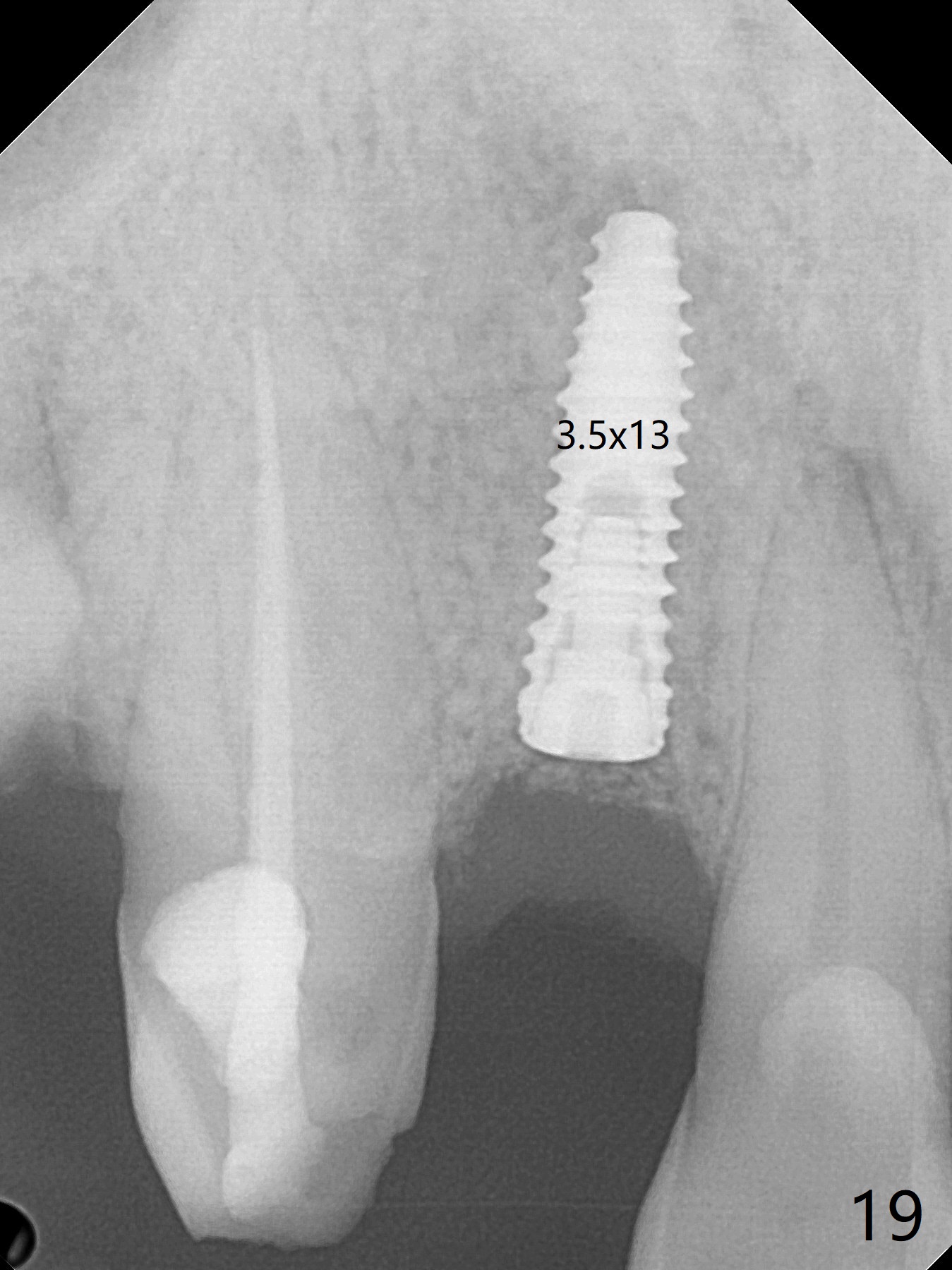
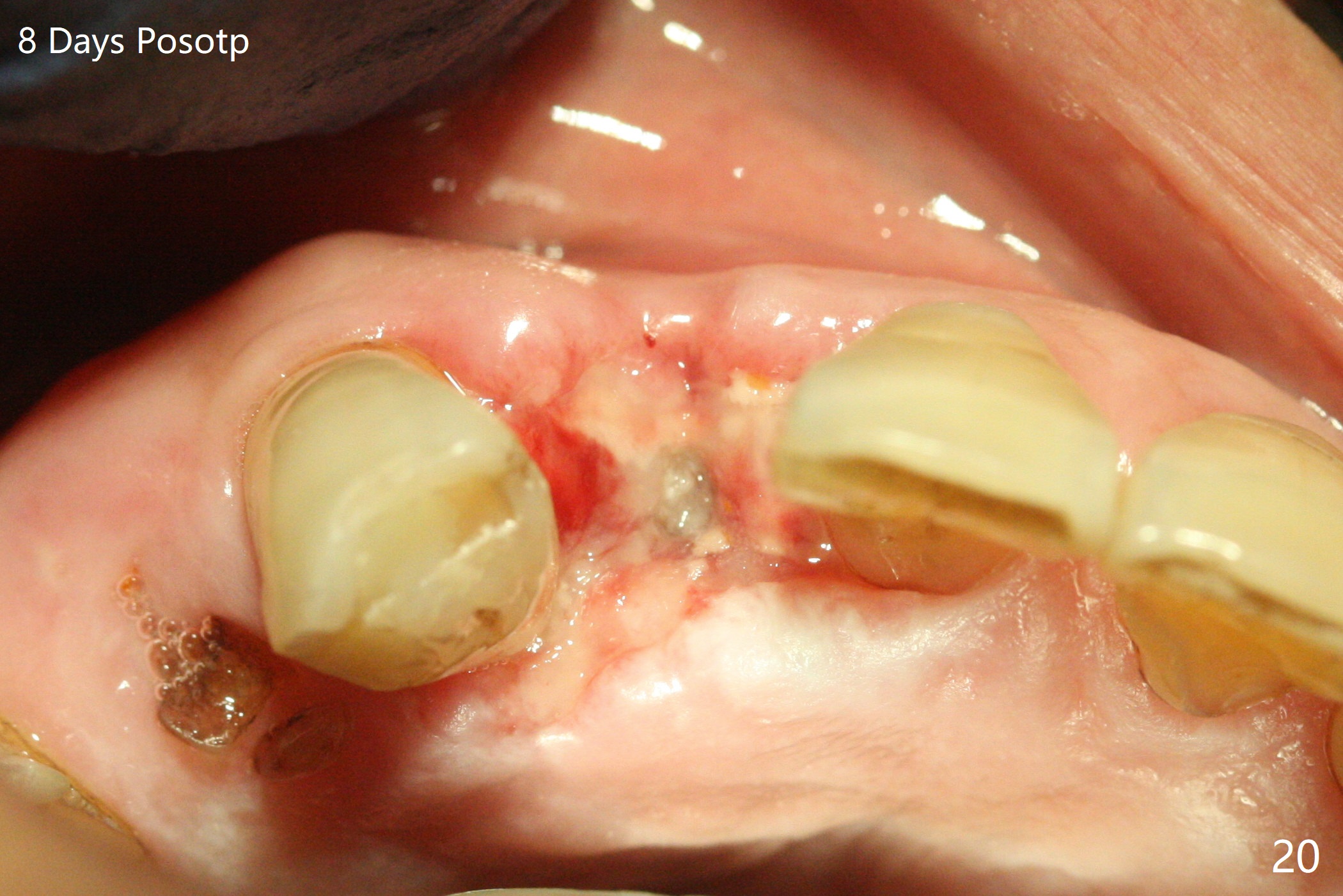
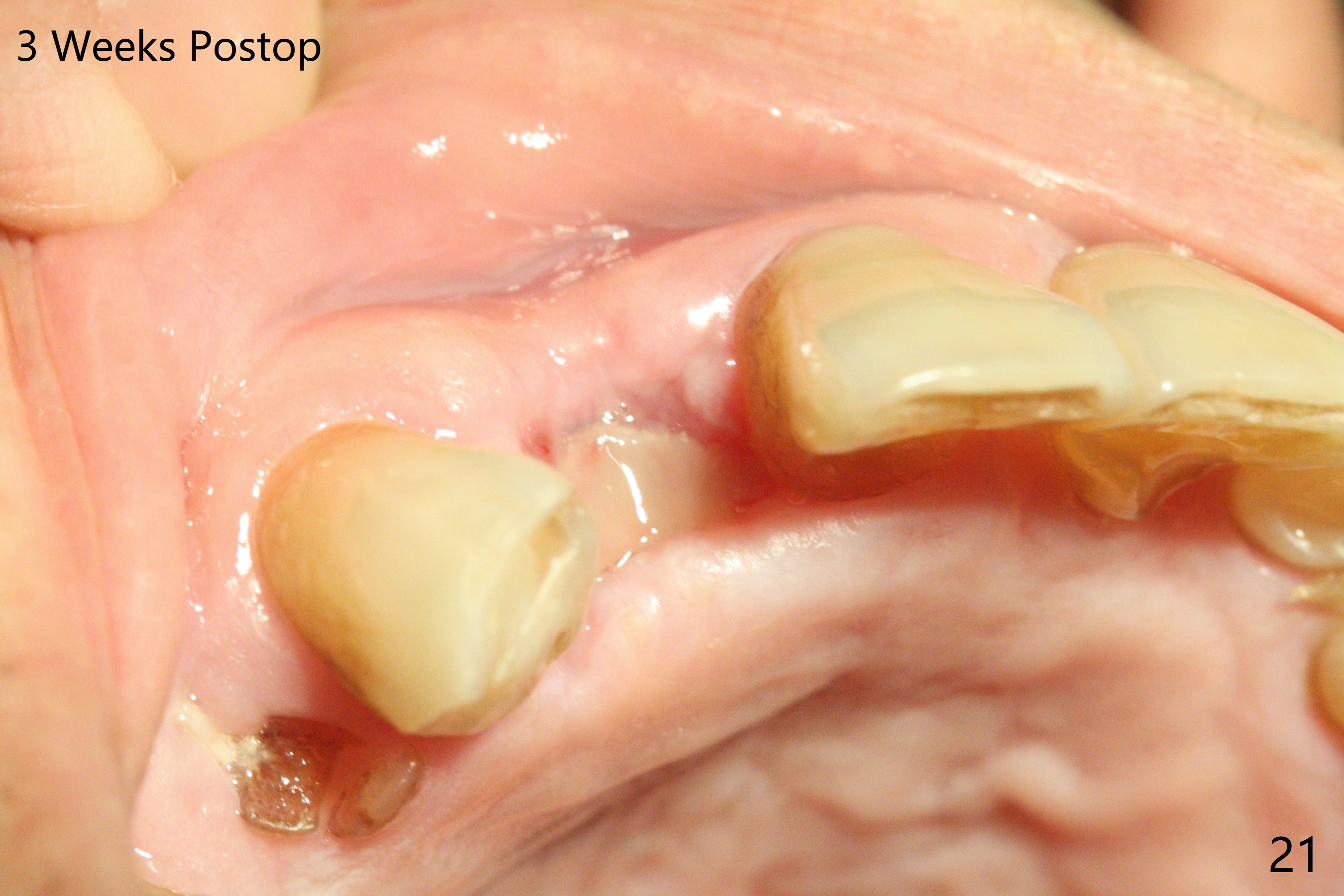
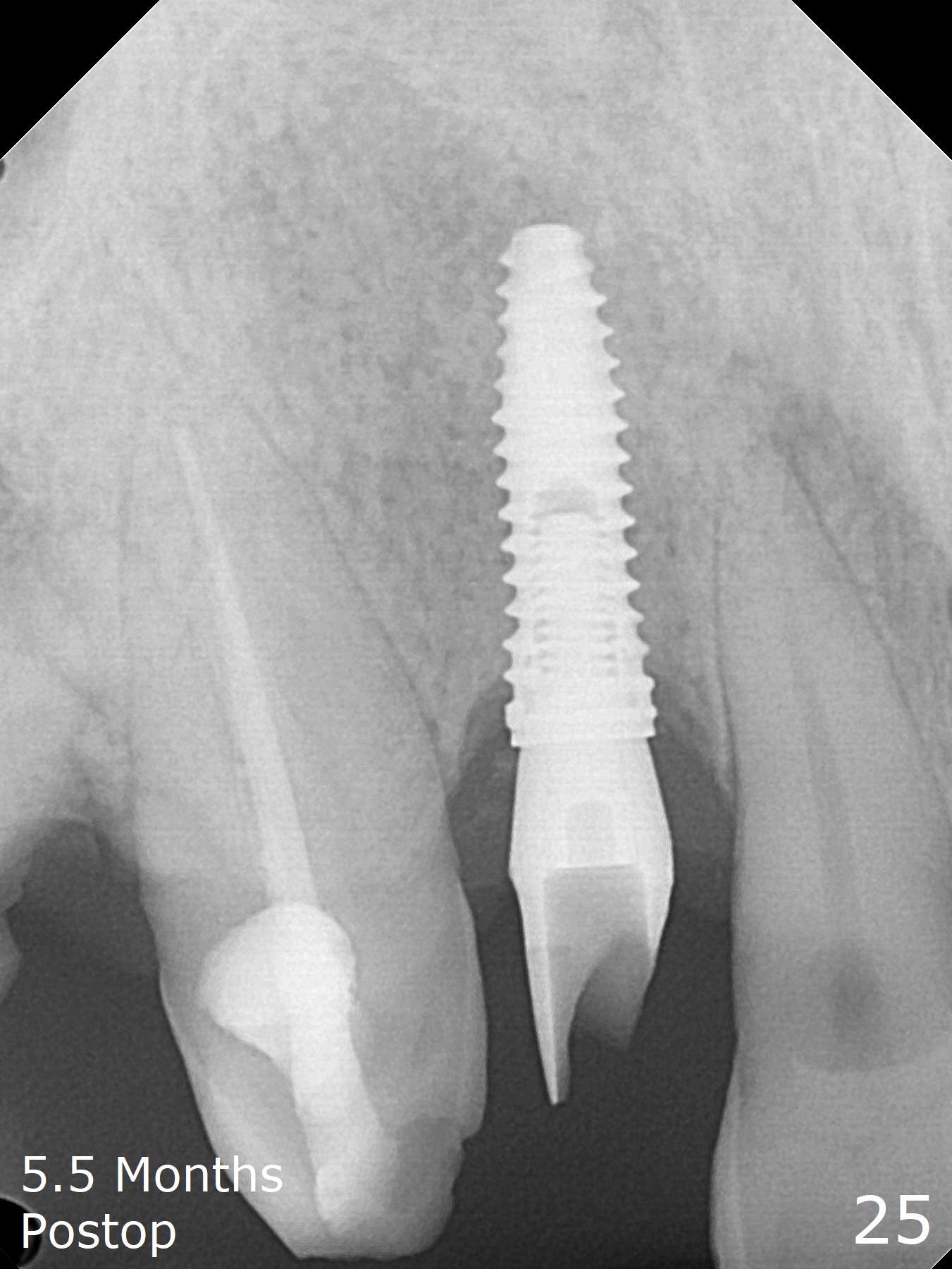
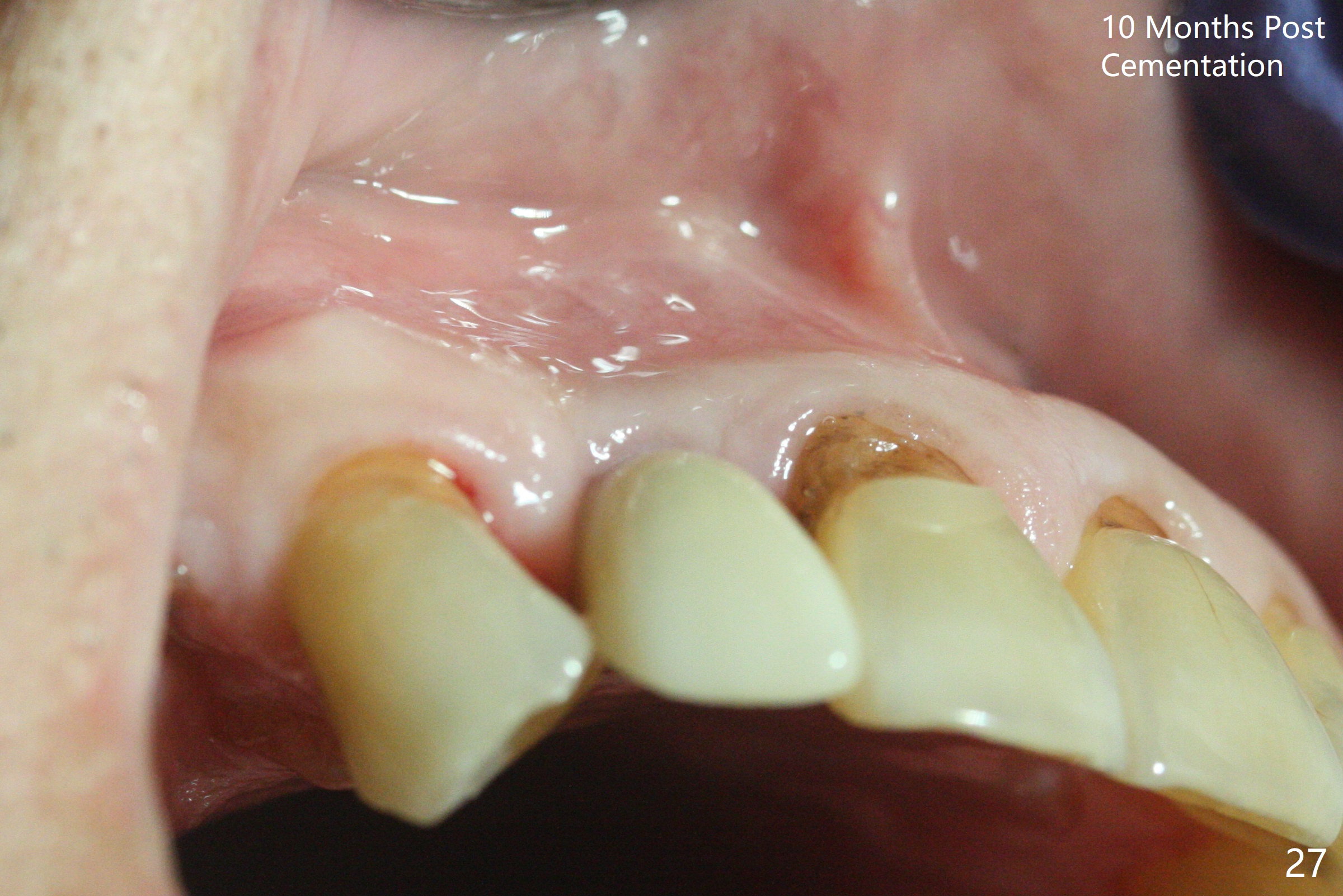
An apical abscess is present when the patient returns for immediate implant at #7 (Fig.1 *); a 2nd challenge is deep bite. After smooth extraction, the apical buccal plate is found to be perforated. Following debridement, a piece of gauze is placed in the apical defect for hemostasis, while osteotomy is initiated palatal (Fig.2). The apical defect seems to be extensive (Fig.3 yellow dashed line). A new trajectory is intended (red arrow) without much success. Before implant placement, bone graft is placed in the apical defect defect area, while a drill (Fig.4 D) is inserted in the finished osteotomy (Fig.5 O). In spite of seemingly large apical defect, the buccal crest bone exists (Fig.4 x). A 3x14(2) mm 1-piece implant is placed with stability; the first round of bone graft is apparently around the apical portion of the implant (Fig.6 *). The coronal end of the implant has to be adjusted several times buccopalatally to accommodate the deep bite. A 2nd round of bone graft following an immediate provisional closes the coronal space of the socket (Fig.7 *). CT will be taken to show the bone graft to repair the buccal plate defect when the patient returns for postop follow-up. In fact the defect is minimal in CT a month ago. The fistula does not disappear 1 week postop, but it is non tender (Fig.8). The patient complains of asymptomatic swelling in the right nostril. CT shows that the large buccal perforation is repaired with large amount of bone graft (Fig.9,10 *). It would be nicer to place the implant slightly more buccal apically (Fig.11 red lines; Fig.12 (preop design)). The buccoapical fistula disappears nearly 1 month postop (Fig.13). The apparently "lifeless" bone graft seems to be harmonious with the surrounding tissue (Fig.14). The periimplant gap reopens with implant mobility nearly 4 months postop (Fig.15), which is related to micro-movement associated with the immediate provisional. The latter is removed. A larger 2-piece implant will be placed in a 2-staged manner if needed (Fig.16). In fact the 3x14 mm straight 1-piece implant (Fig.17) has no mobility when it is retightened, but the trajectory remains buccal. Incision shows that there is no implant thread exposure. A 3x14 mm 15 degree angled 1-piece dummy implant is able to establish the correct trajectory, but there is no occlusal clearance (Fig.18). Micromovement during osteointegration may recreate loosening. Finally using Lindamann bur, the osteotomy is changed so that a 3.5x13 mm 2-piece implant does not need an angled abutment to establish occlusion (Fig.19). There is one palatal thread exposure. Allograft is placed circumferentially, followed by Human Amnion-Chorion Allograft and Collagen Plug. The wound does not heal 8 days postop (Fig.20), as related to the age (79 years old)? The wound appears to heal with a membrane on the surface (Amnion-Chorion one?) 3 weeks postop (Fig.21). The ridge looks wide 3.5 months postop (Fig.22,23). A 4.5x5.5(3) mm appears to be seated incompletely with a gap between the abutment and the implant (Fig.24<). A provisional is fabricated after heavy palatal reduction. Two months later, the provisional fractures. After repositioning the abutment with complete seating and torque (Fig.25), impression is taken. Although the buccal plate is concave, the gingiva remains healthy 10 months post cementation (Fig.26,27).
Return to Upper Incisor Immediate Implant, Trajectory II Xin Wei, DDS, PhD, MS 1st edition 05/07/2019, last revision 01/16/2021