
 |
 |
 |
 |
 |
 |
 |
 |
Remove Implant with Periimplantitis
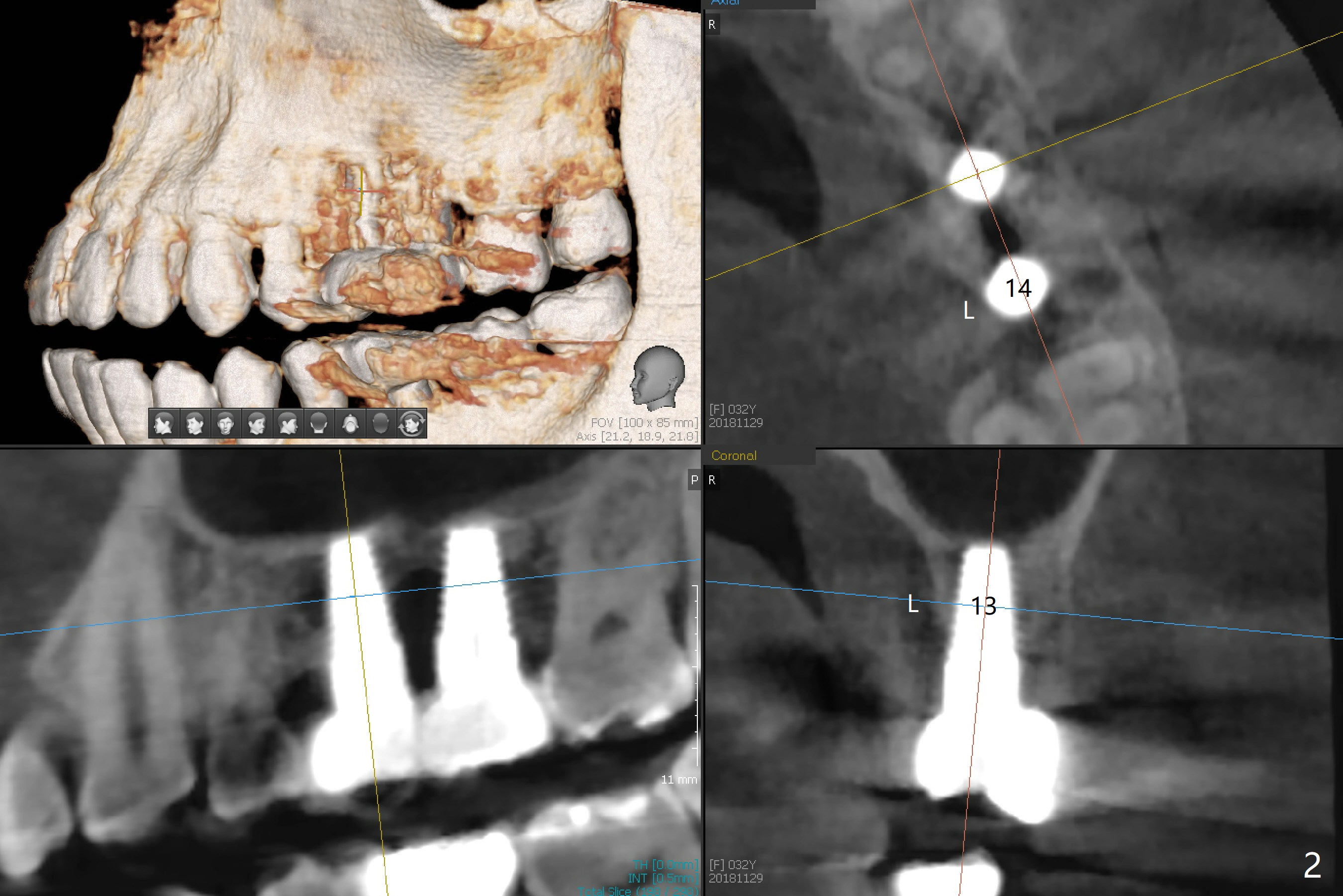
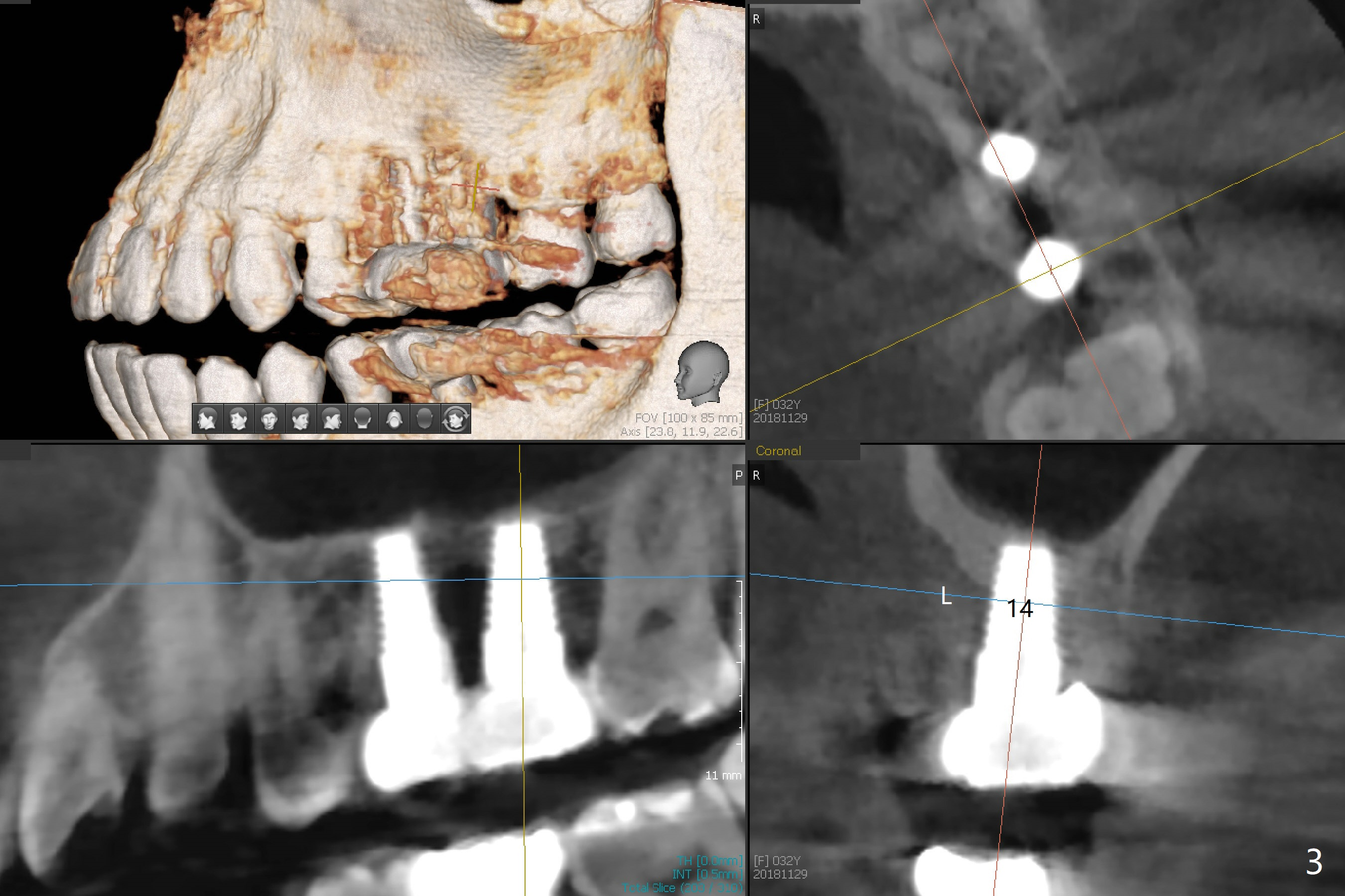
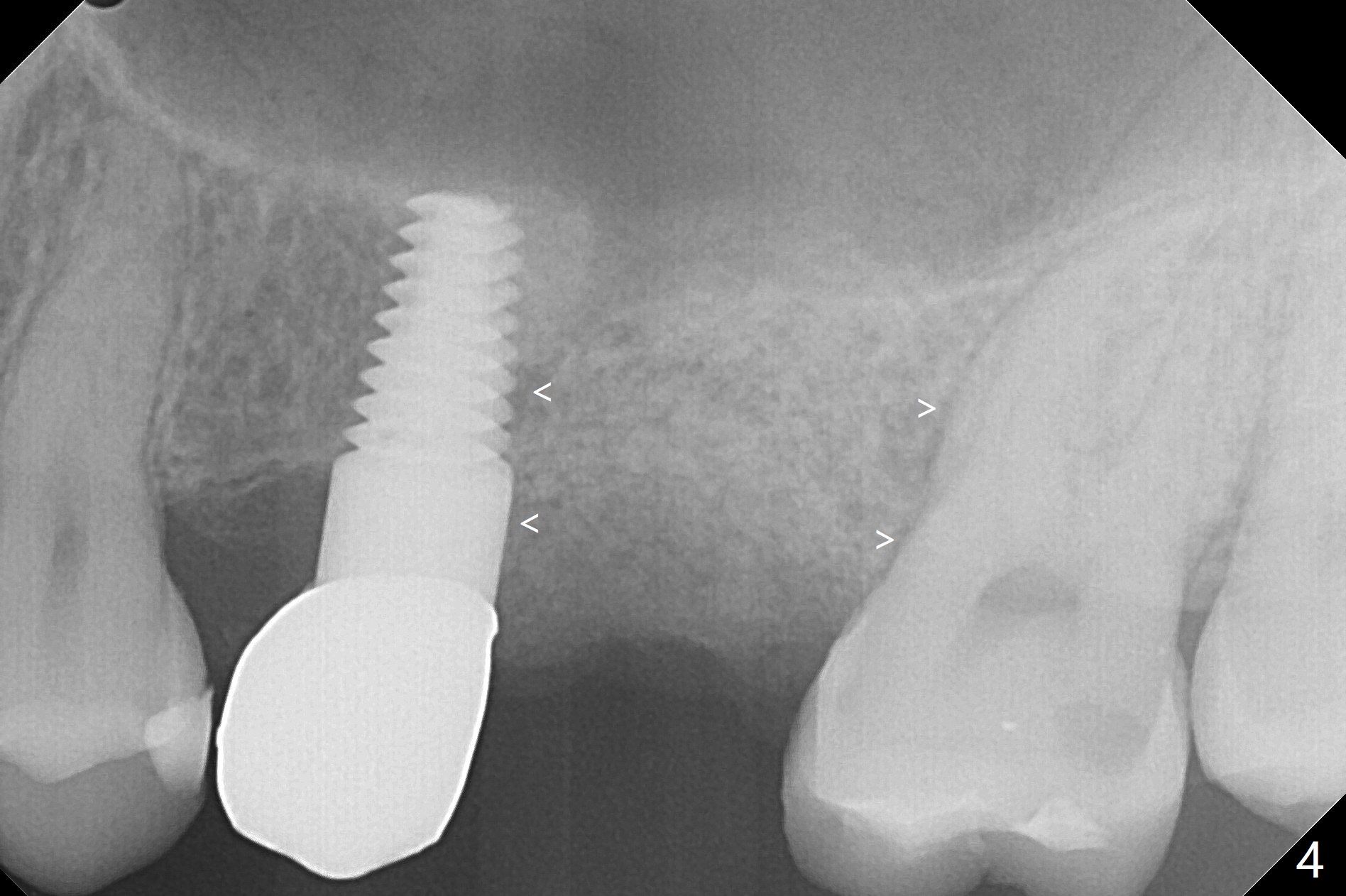
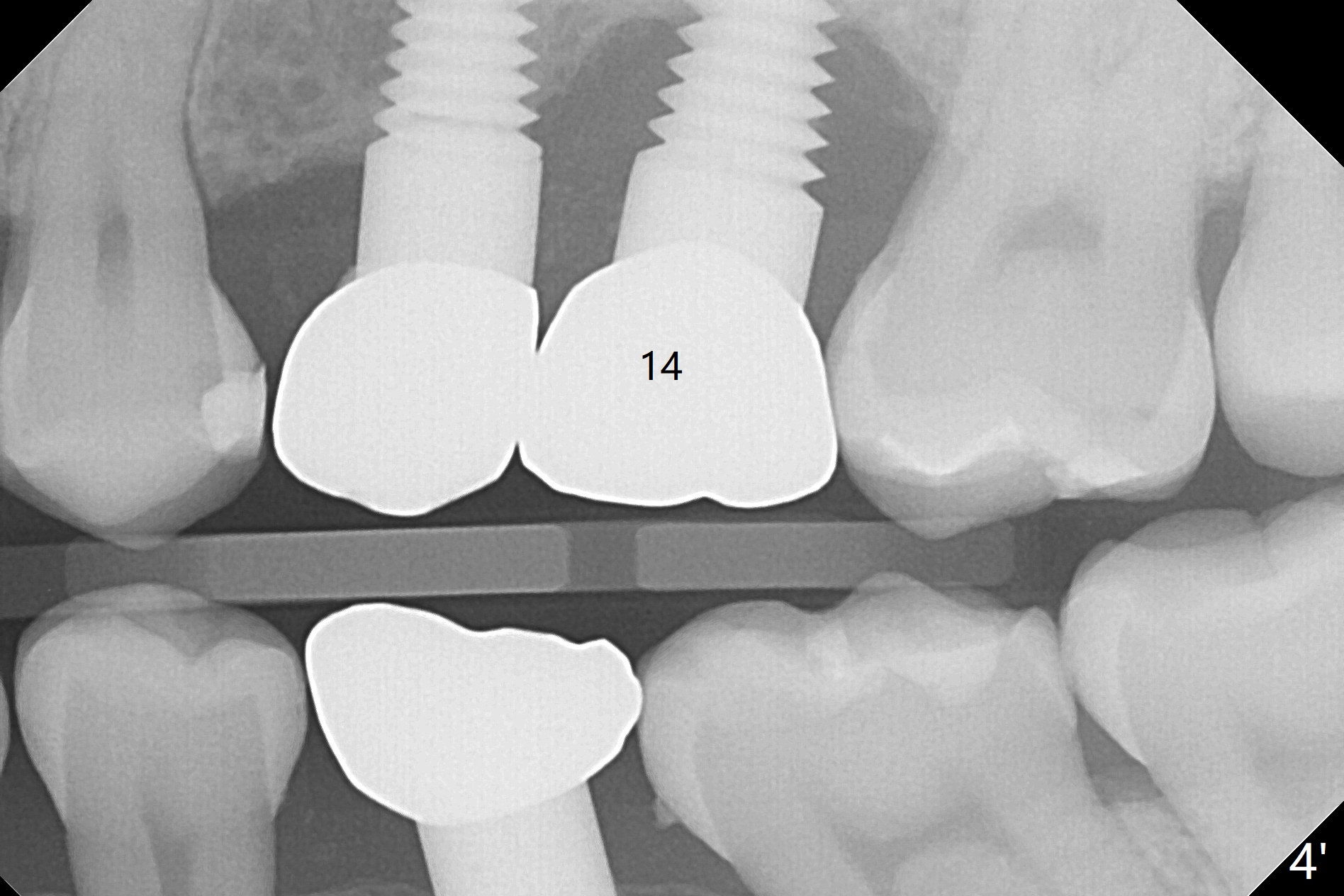
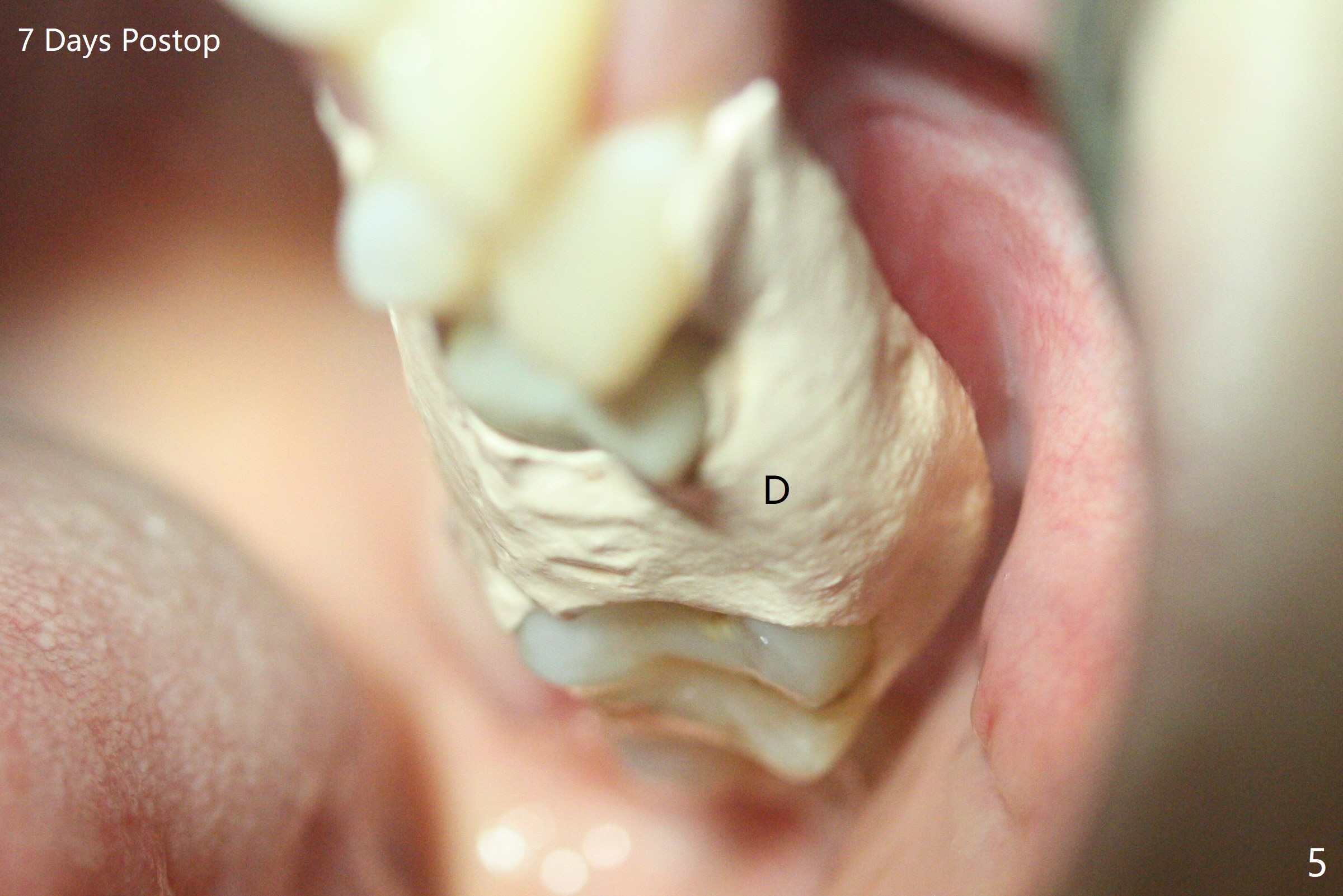
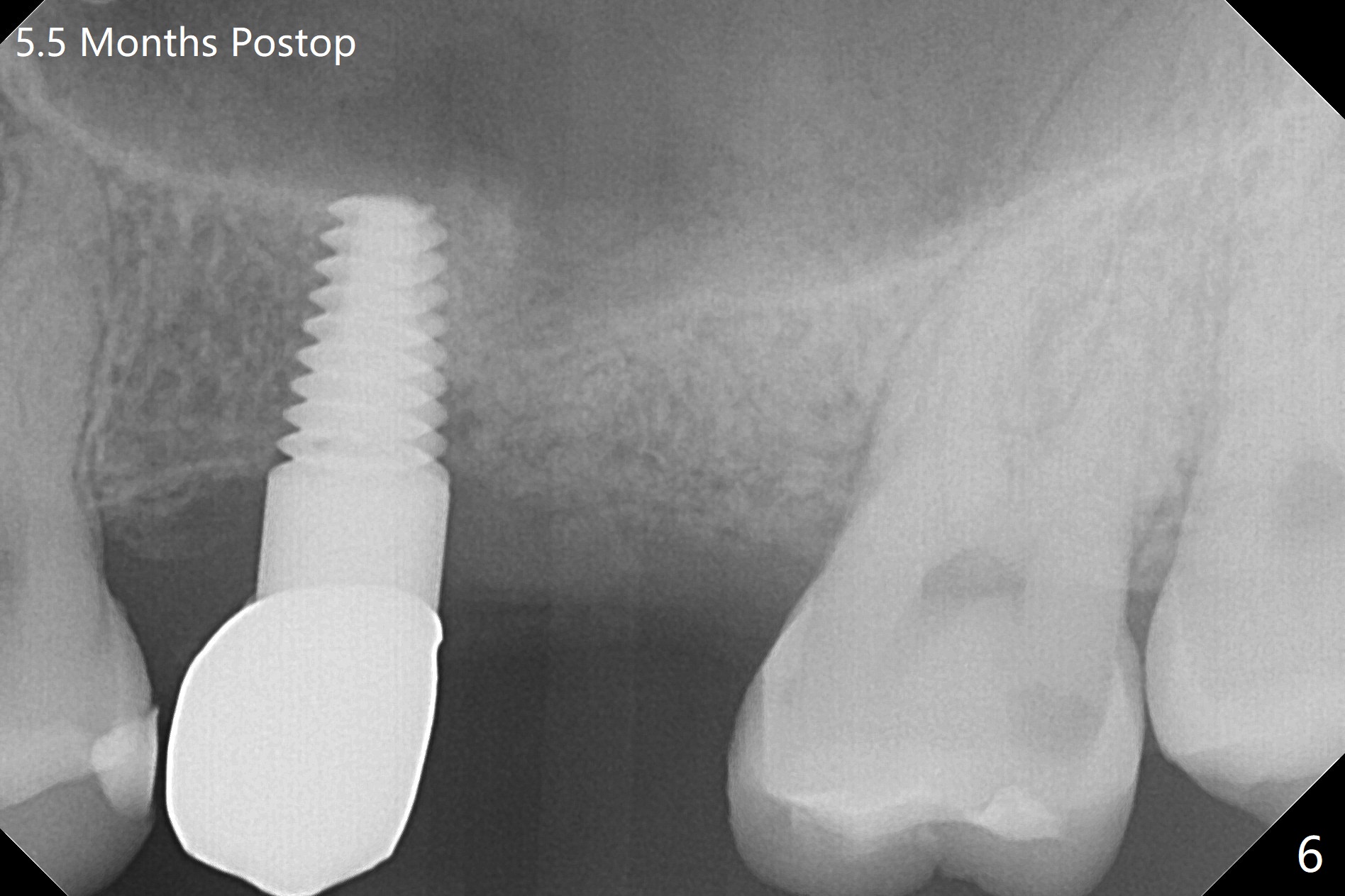
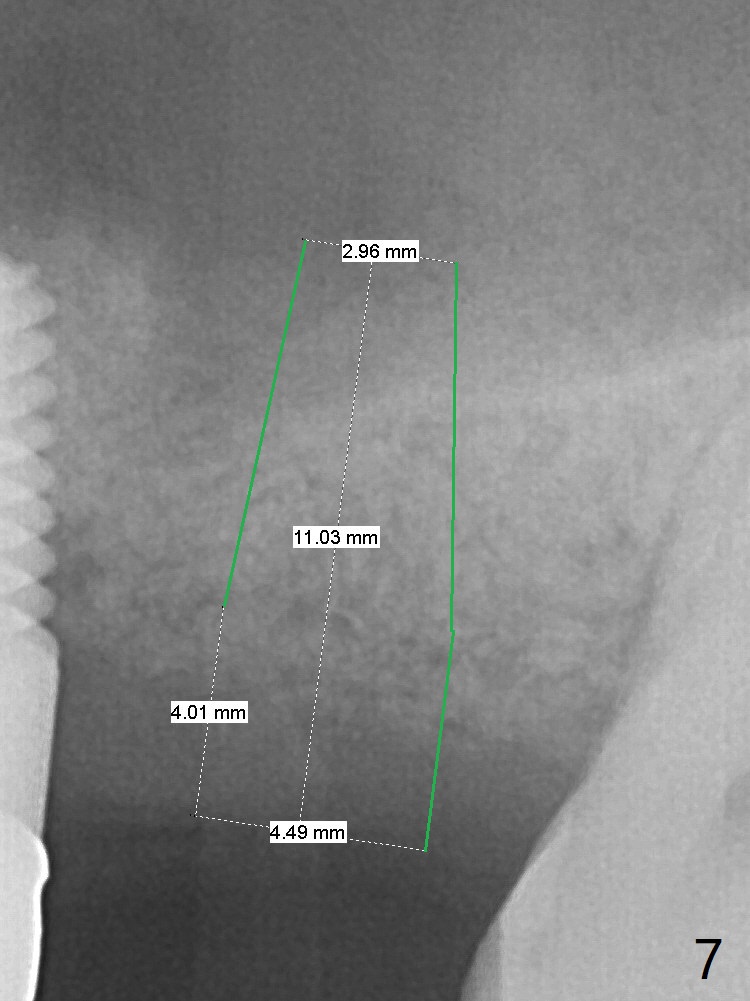
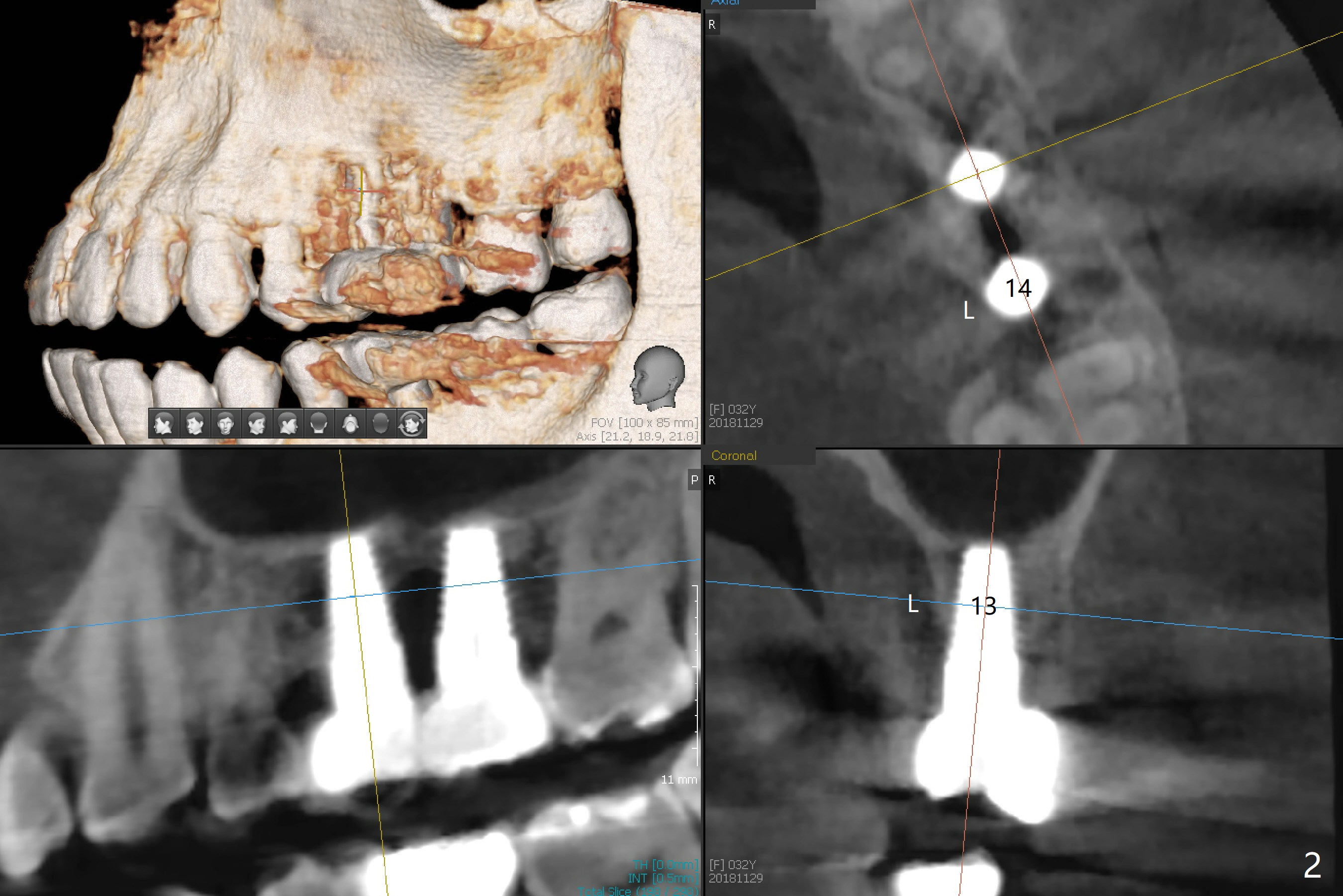
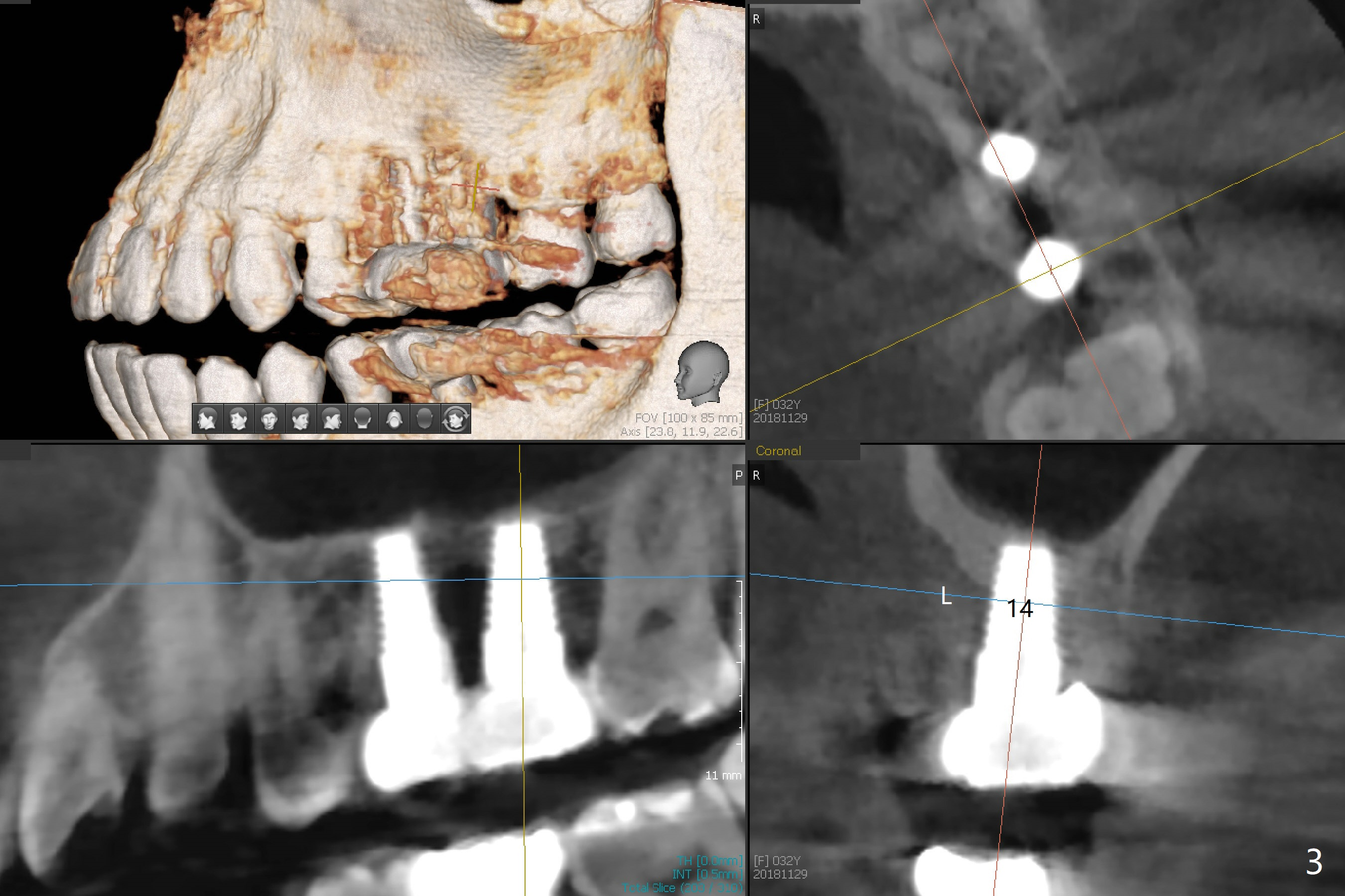
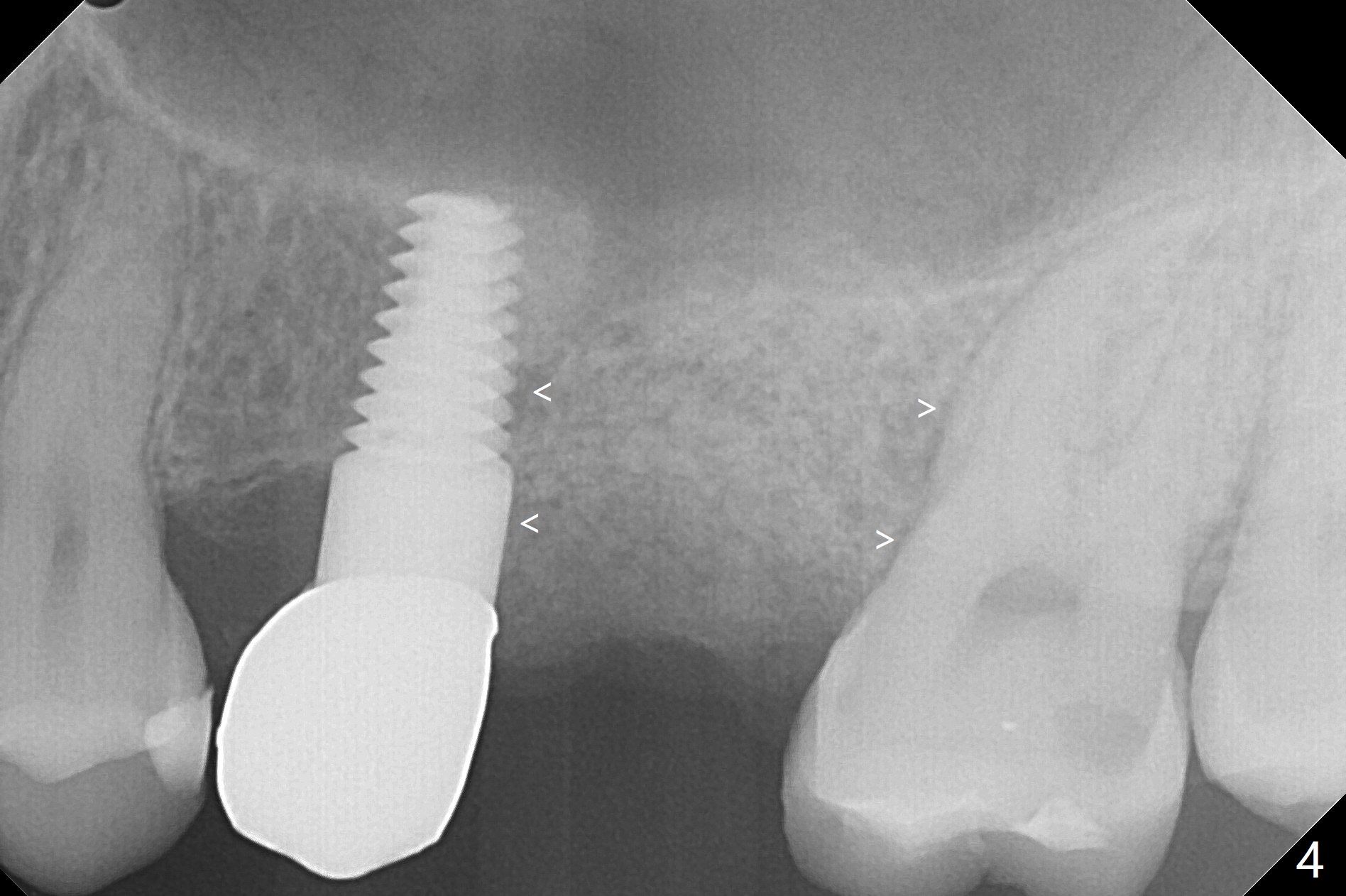
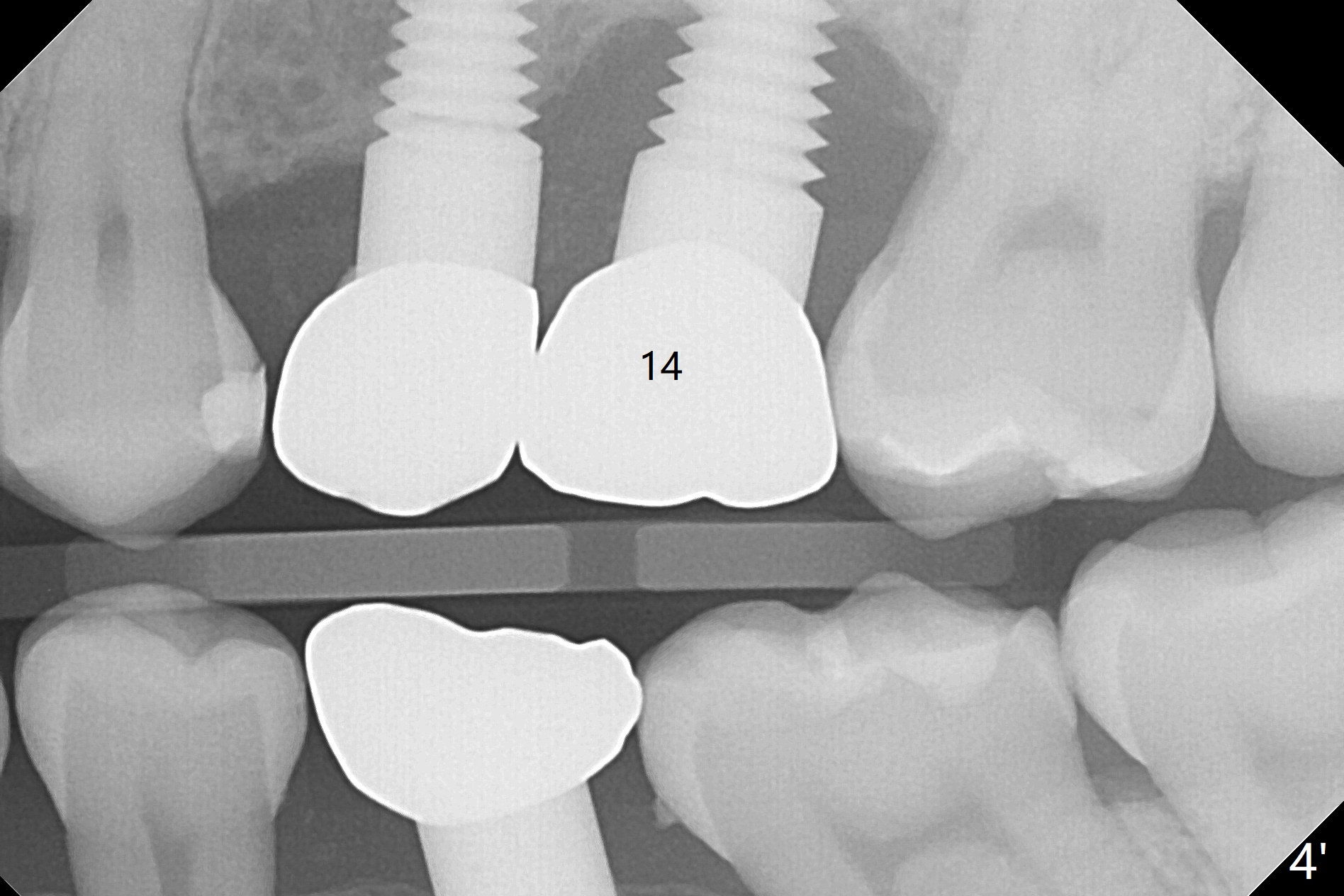
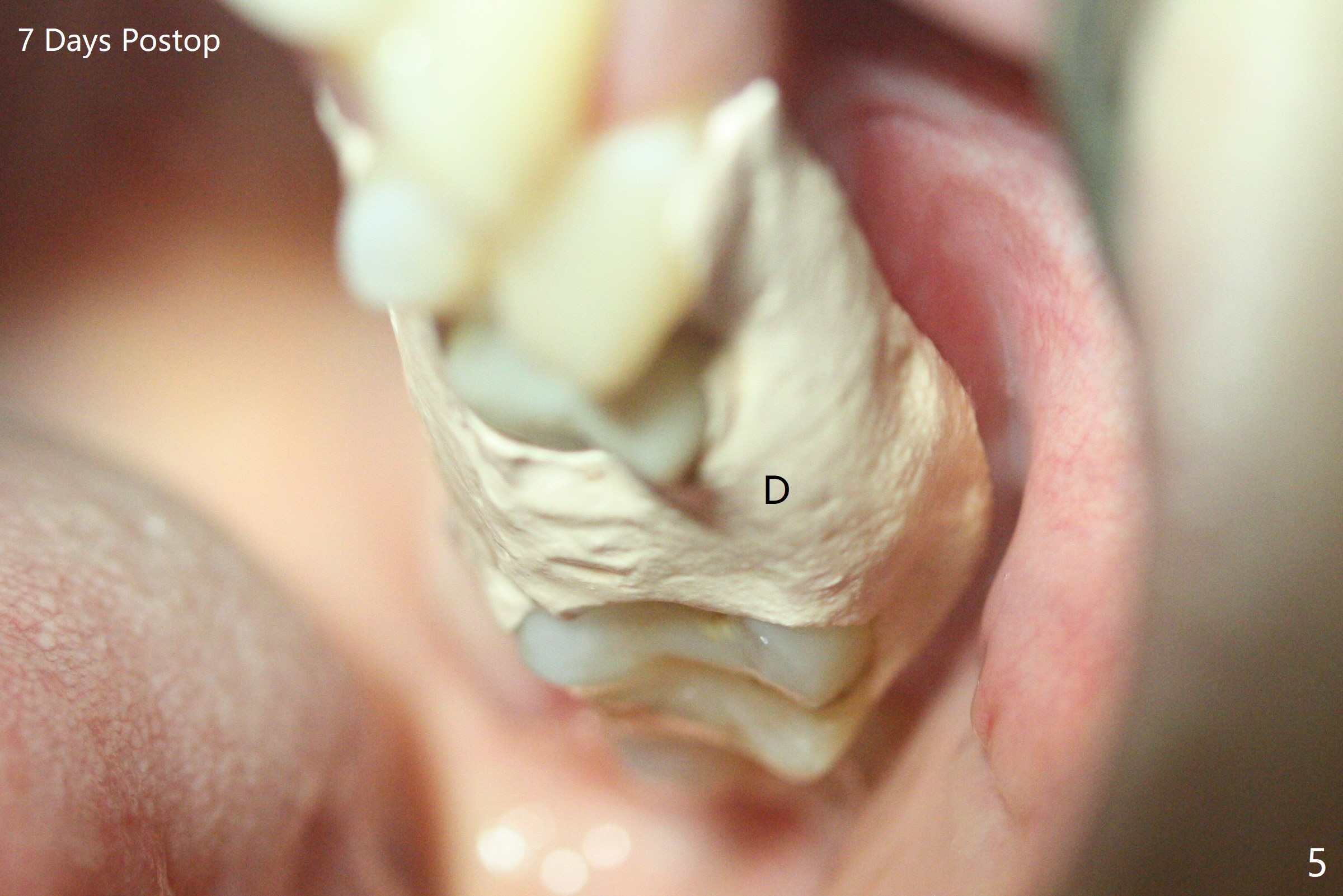
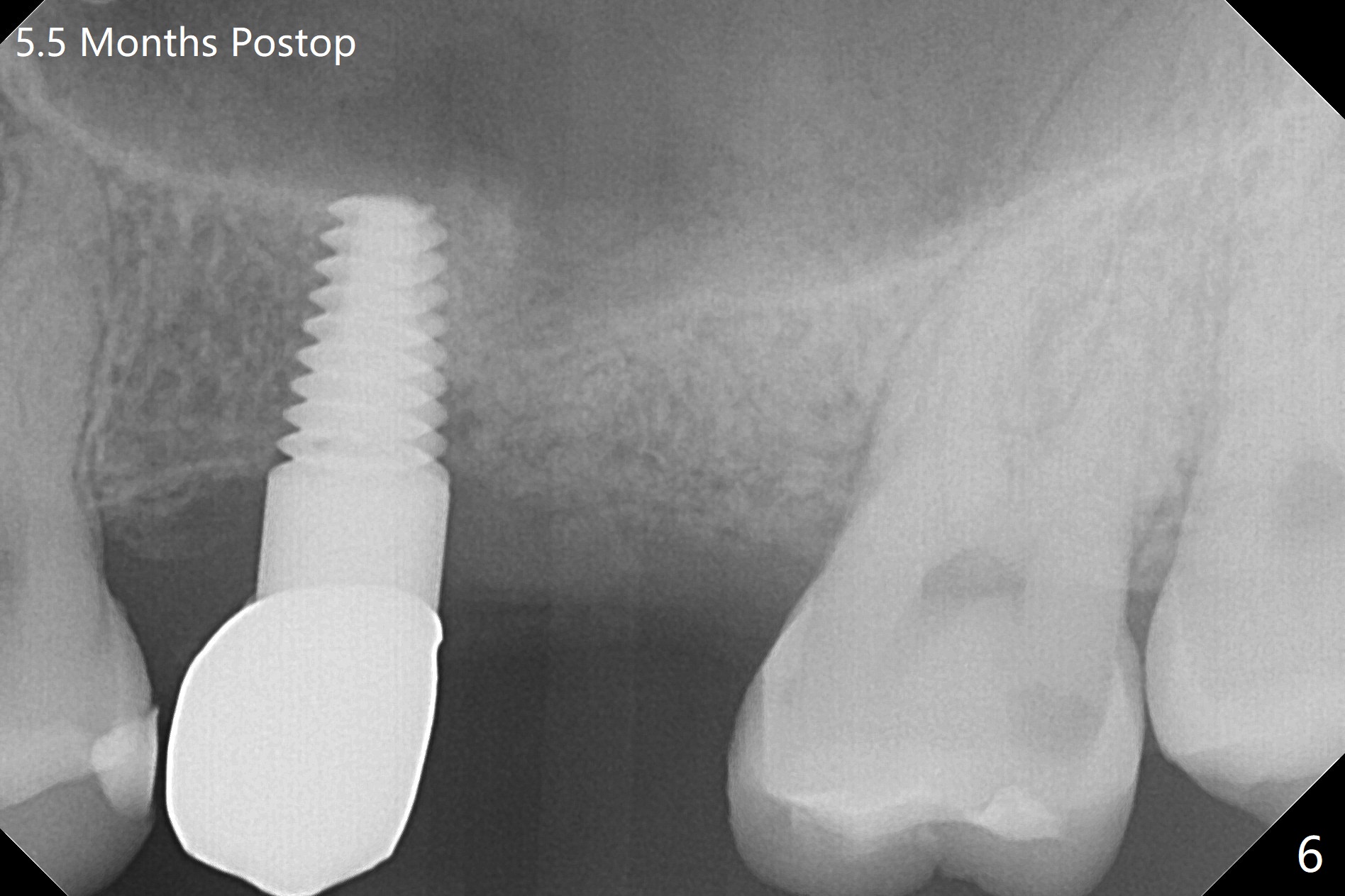
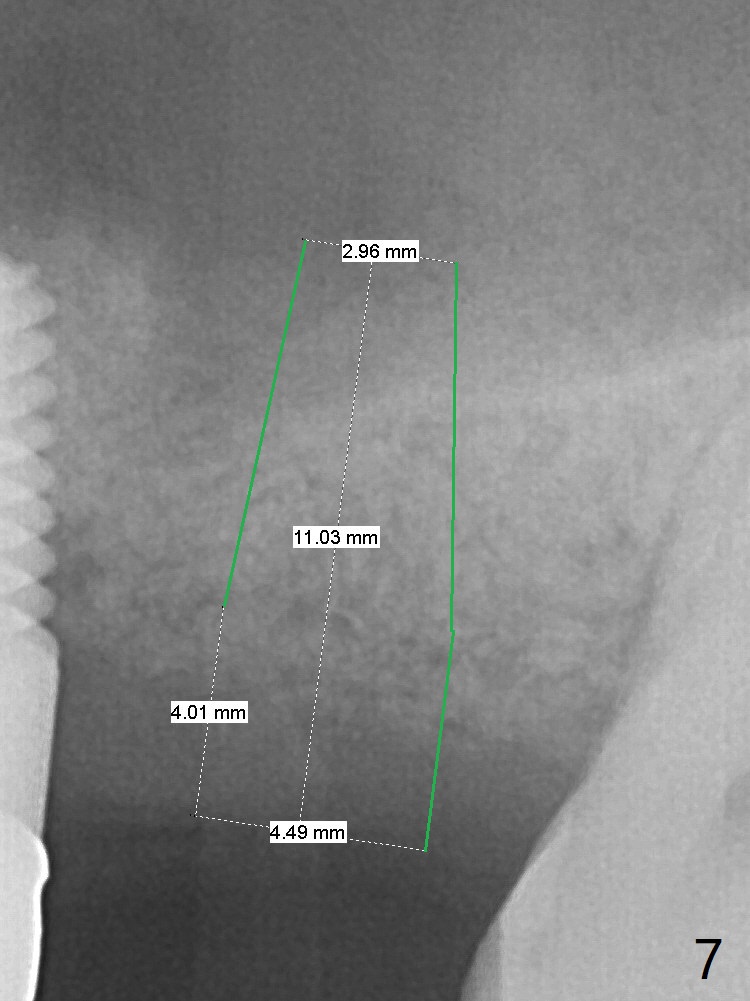
A 32-year-old woman develops periimplantitis (severe hemorrhage and deep pockets) at #14 three years 7 months post cementation (Fig.1). A 4.5x11 mm implant is placed with flap at #13 after failure for the 1st time (Fig.2), while a 5x11 mm implant is placed flapless with sinus membrane perforation. Uniposts are cemented with Ketac. The lingual plate at #14 is defective (Fig.3). The implant at #14 will be removed flapless, followed by Osteogen plug (most likely sinus floor defect) and bone graft. After healing, an implant will be placed with guide. By breaking the proximal contacts, the crown, abutment and implant at #14 are shaken loose using forceps. Finally the crown breaks off. Make a slot on the top of the abutment and use a screw bit to turn the abutment/implant counterclockwise. There is abundant granulation tissue with arterial hemorrhage associated with granulation tissue removal. The defect involves the distal surface of the implant at #13 and the mesial surface of the tooth #15. Therefore bone graft is deposited in these surfaces (Fig.4 arrowheads, as compared to preop BW, Fig.4'). The periodontal dressing seems to remain in place asymptomatic 7 days postop (Fig.5). The bone height 5.5 months postop should be enough for implantation (Fig.6). To avoid marker associated with guided surgery, free hand will be adopted. Sinus lift with PRF is expected. To place in the middle of the ridge buccopalatally, incision will be made with bone expansion.
Return to Upper Molar Immediate Implant, Trajectory II Xin Wei, DDS, PhD, MS 1st edition 12/01/2018, last revision 08/28/2019