







 |
 |
||
 |
 |
||
 |
 |
 |
|
 |
 |
 |
|
 |
|||
Quick Atrophy after Extraction
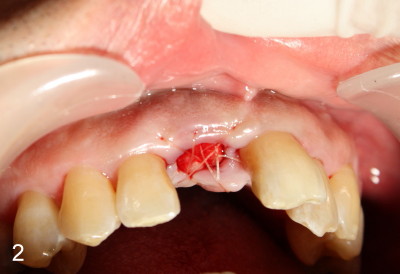
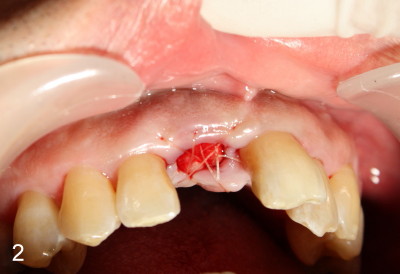
The upper right central incisor is nonsalvageable for 37-year-old man (Fig.1). After atraumatic extraction, localized scaling is performed. Collagen plug is inserted. PGA suture is used to keep the plug in place.
Four weeks later, the patient returns for #10 root canal therapy. There is purulent discharge from the apical labial region of #8 (not shown) with mild tenderness.
The patient is scheduled to return 1 week later for #8 socket debridement and irrigation. The labial aspect has undergone atrophic changes (Fig.3,4). More surprisingly is that the labial plate is found to be lost during socket debridement. The labial plate seems to be intact at extraction. Otherwise socket preservation must have been done.
Does this post-extraction infection happens often, but without being noticed?
Four quadrant scaling and root planing should have been conducted prior to
extraction to reduce infection in this case. Note calculus in the lower
anteriors (Fig.1). Does immediate implant with bone graft prevent
loss of the labial plate? What should we do for this case now?
Wait for 2-3 months before implant placement? Or bone graft after the
infection is under control?
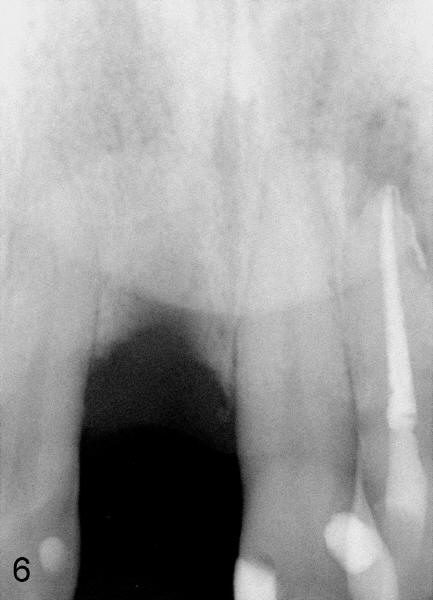
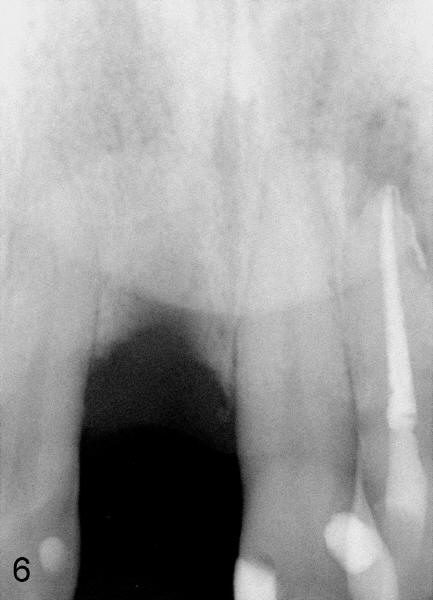
Two months after socket debridement, the wound appears to have healed with mild to moderate buccal plate atrophy (Fig.5). Bone height is ~ 21 mm (Fig.6). D2 short or long implant is planned. Is this appropriate?
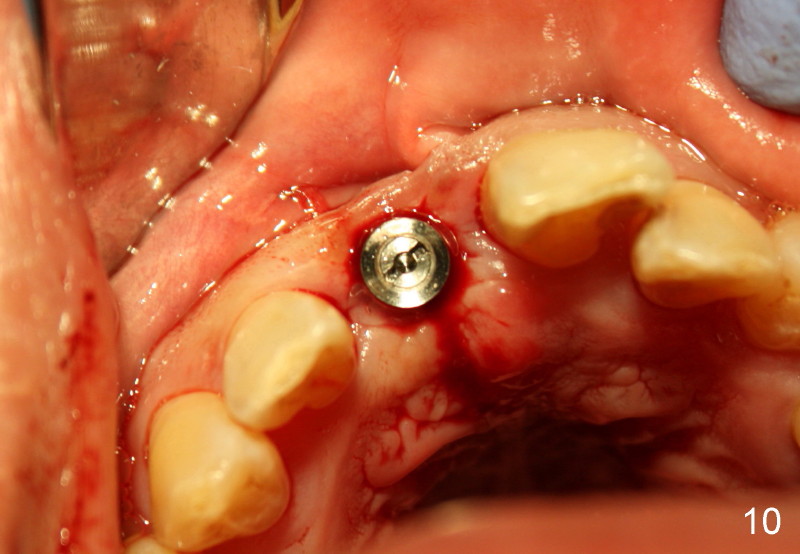
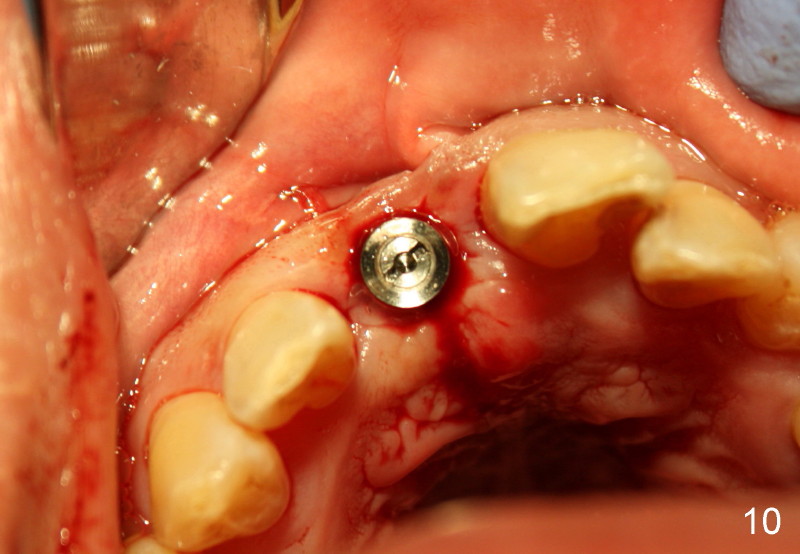
Two more weeks later, D2 implant (4.5x5.5x20 mm) is placed (Fig.9,10). Fig.7 D2 thin socket former at ~ 16 mm depth, Fig.8 D2 medium socket former at ~ 19 mm.
Implant threads are at crest level (Fig.9). Is there any potential problem?
The implant heals well, two weeks postop (Fig.11). The buccal plate atrophy seems to be improved (arrowheads, as compared to Fig.4,5).
Xin Wei, DDS, PhD, MS 1st edition 09/09/2011, last revision 12/04/2011