


 |
 |
 |
 |
 |
 |
Paresthesia after Extraction of a Lower 2nd Molar
---- Sat - May 17, 2014 -----
S: 43 y/o BM PTC for limited exam with cc "LR tooth loose with pain", dental history: no fever or malaise, last cleaning unknown, MHR: NSF, NKDA
O: E/O: facial symmetry, no facial swelling, no trismus, I/O: OH: fair, heavy mastication, 14 lost crown and build up, 31 DB gingival erythema/edema/recession, mobility II with deep pocket, PA taken. It shows #31 +PARL (Fig.1)
A: 31 nonsalvageable
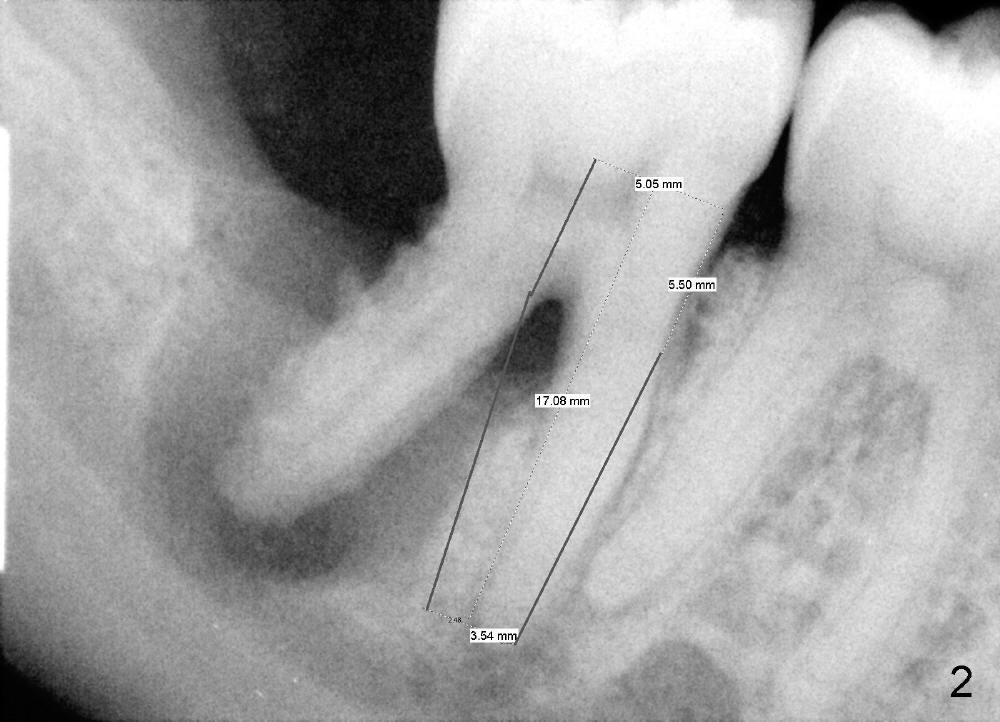
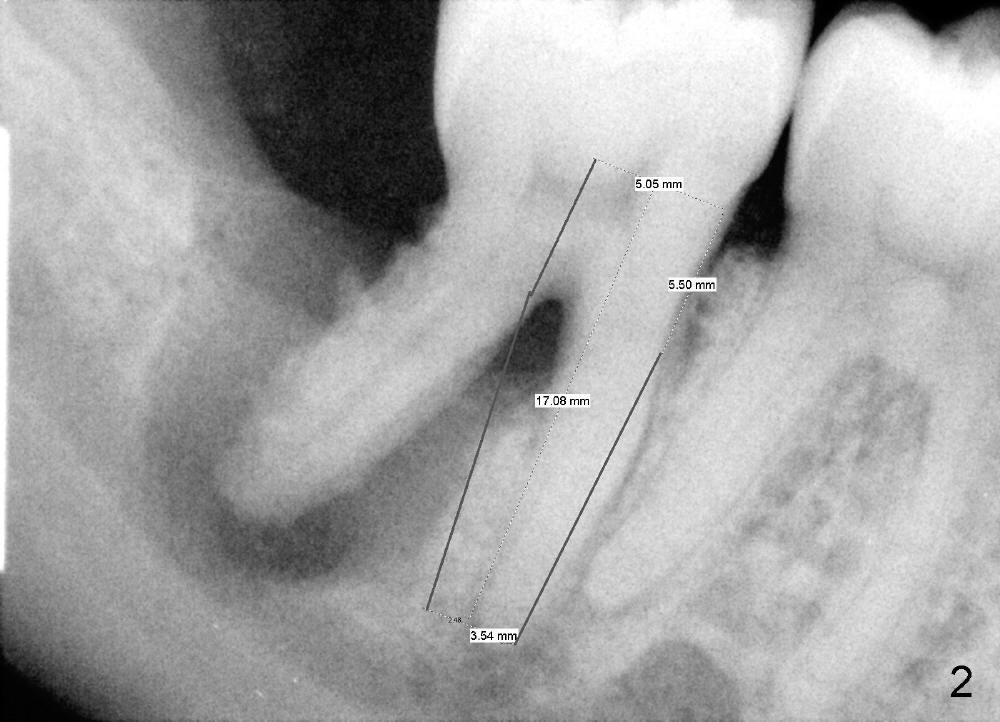
P: 31 Ext, immediate implant in the mesial socket (Fig.2), 14 redo bu, crown, treatment plan discussed
T: Amoxicillin, Chlorhexidine
NV: 31 Ext, implant
-
-------------- Thu - May 29, 2014 ---------------S: PT RTC for Tooth: 31 ext, "LR last tooth sensitive, swollen sometimes", no change in MH
O: OH fair, #31 DB gingiva erythematous and edematous, mild purulent exudate from pocket buccal
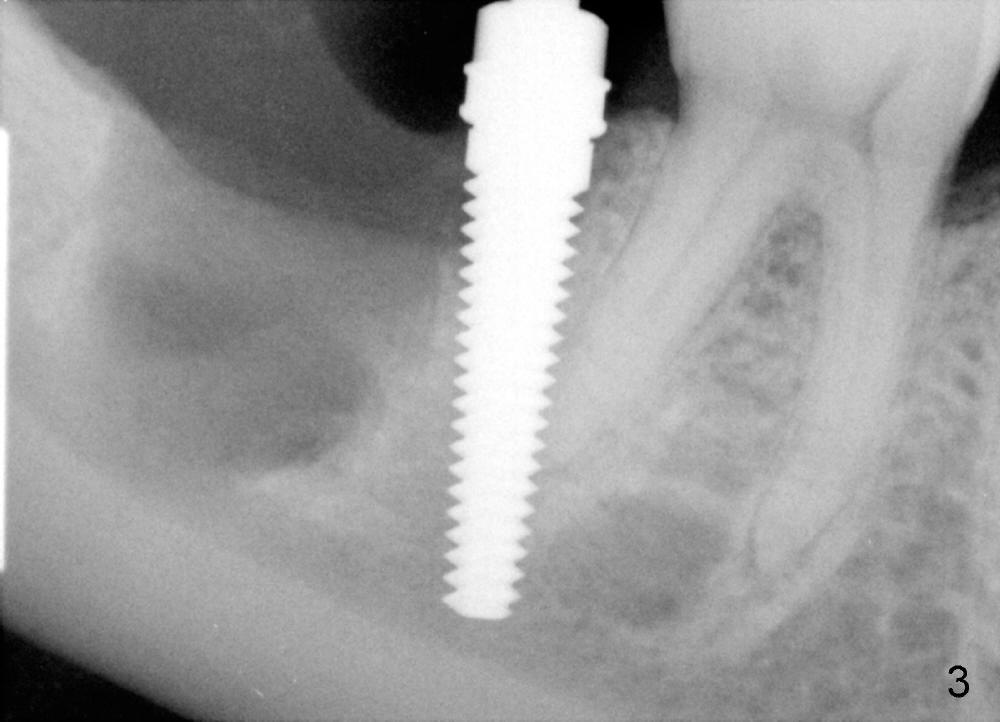
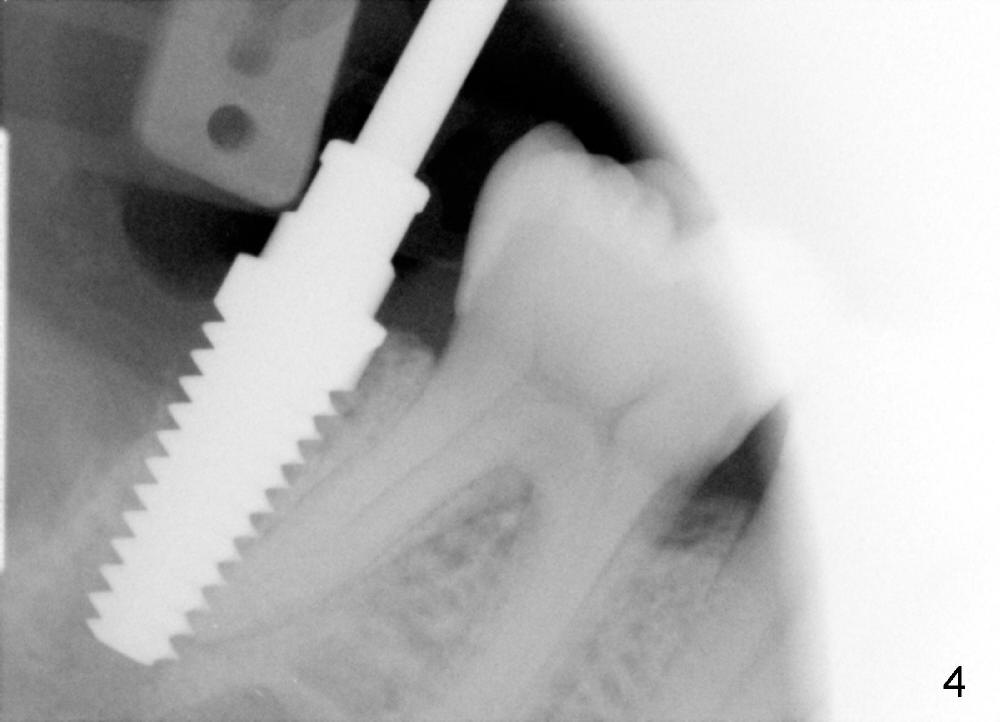
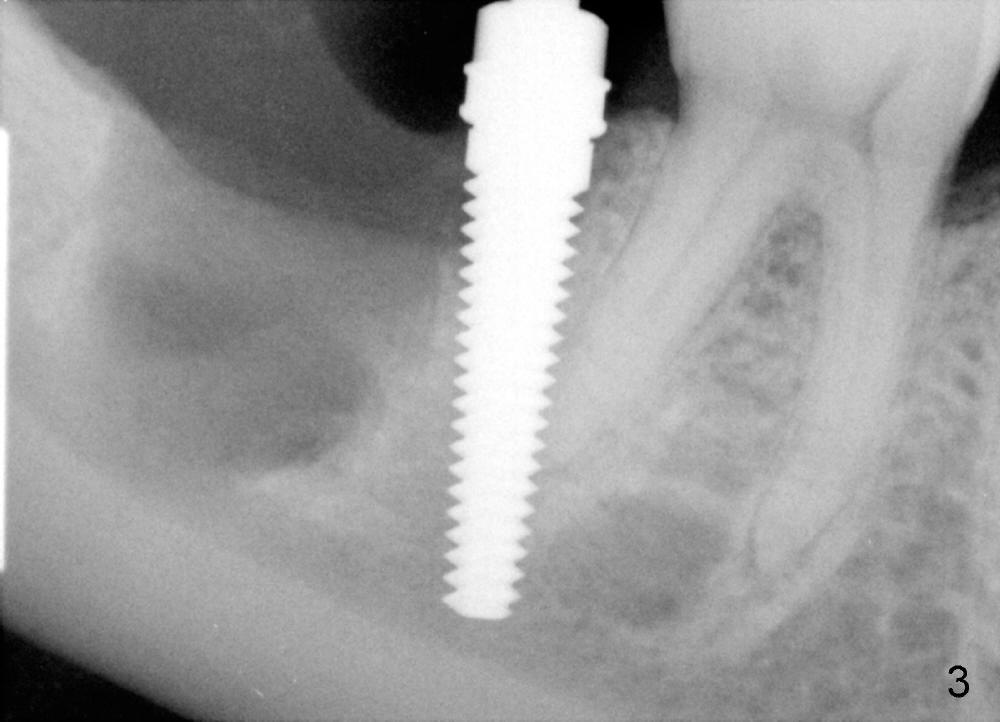
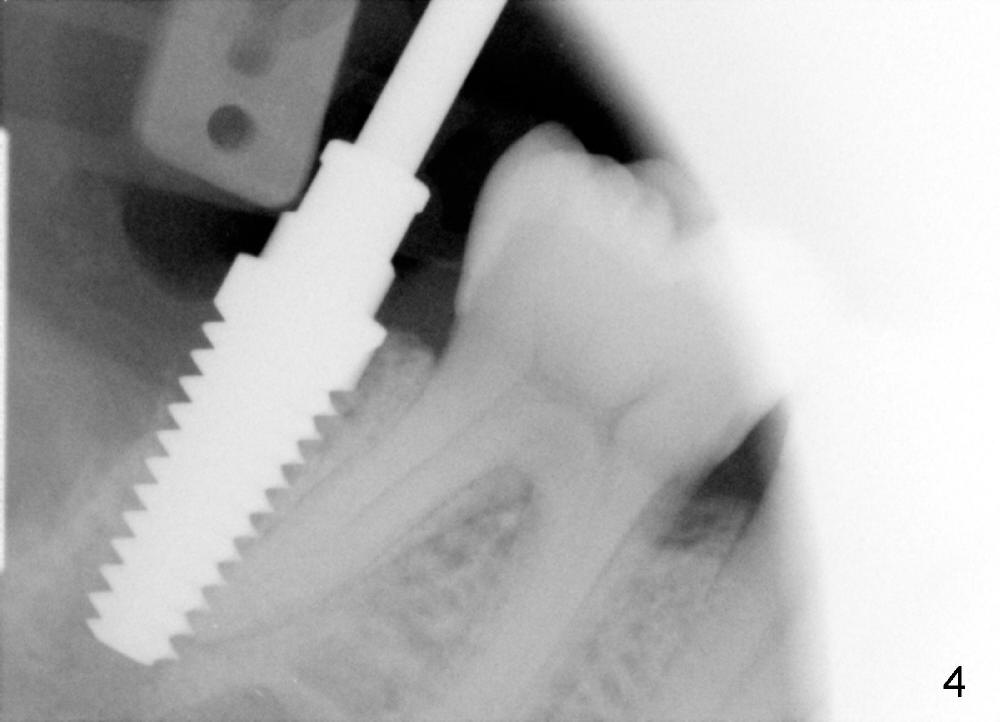
A: after obtaining verbal and written sx consent, Mepivacaine 54 mg, Xylo 34 mg, Septo 68, Epi 34 mcg infiltration, separated gingiva with periotome, pt had pain, Marcaine 9 mg, Xylo 34 mg, Epi 26 mcg infiltration and intraligamental injection, routine ext with forceps, curettage with serrated curette, lot of granulation tissue, until the bottom of the socket, close to presumptive inferior alveolar canal, tissue apparently running mesiodistally, easily removed without active hemorrhage, distal root has abundant calculus, distal socket apparently too large for implantation, copious irrigation, placed Clindamycin gauze x3, mesial socket flat (B-L width is much bigger than M-L one), inserted D1,2 spreader and D2 socket formers with difficulty, handles contact #30 distal crown, inserted RT 2,3,4 and tapered osteotomes 5x18 and 6x18 mm, trying to move the septum distally with much help, inserted 4.5x20 mm tap at 17 mm depth, stable, PA taken: tap close to #30 distal root, approaching IAN (Fig.3), changed to 5x17 tap at 14 mm without stability, when 6x17 tam is inserted at 14 mm, it is stable, PA taken: tap very close to #30 distal root (Fig.4), removed the tap (mesial wall of the mesial socket: no obvious perforation with distal root of #30) and droppd it into in the distal socket, PA: tap tip overlaps IAN canal (Fig.5), discussed possible nerve injury and touching neighboring root, pt agreed to abort implant placement and place bone graft. placed collagen plug (CollaForm-Plug, Absorbable Collagen Wound DRef CFP1020_5, Lot CFP1020_1301)) in the bottom of the socket (to make room for nerve regeneration), inserted ~.6 cc CANCELL Oss (Mineralized Cancellous Human Allograft, distributed by Implandent LTD, .850-1 mm, 03-0494763/03-0494749, Product Code 06412201, mixed with .3 mg Osteogen (300-400 micron, Osteoconductive Synthetic Bioactive Resorbable Graft, Impladent LTD) into sockets, placed another collagen plug on the top of bone graft, 4-0 chromic gut suture (figure 8 and 1 interrupted), perio dressing, hemostatic. Pt was doing well. POI (oral) and extra gauze given. Continue Amoxicillin, Chlorhexidine, Medrol and Norco, Vitamin B complex recommended
P: NV: RTC 1 wk f-u
--------------- Fri - Jun 13, 2014 ---------------
S: PT RTC for F-U, 16 days s/p #31 ext, injury to IAN, parethessia appears not to interfere with his daily lift, no change in MH
O: OH fair, #31 socket M: granulation tissue, D appears empty, defined paresthesia extent, took photo (Fig.6).
A/P: refer to OMFS for consult
Xin Wei, DDS, PhD, MS 1st edition 06/18/2014, last revision 02/07/2017