





 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
|
Immediate Implant and Sinus Lift
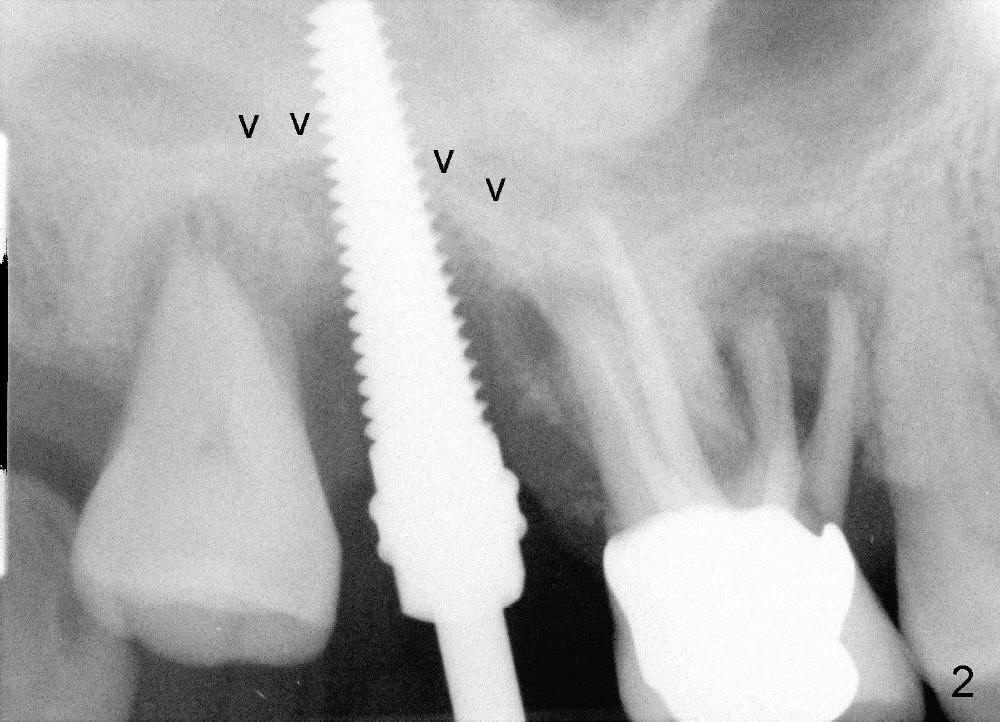
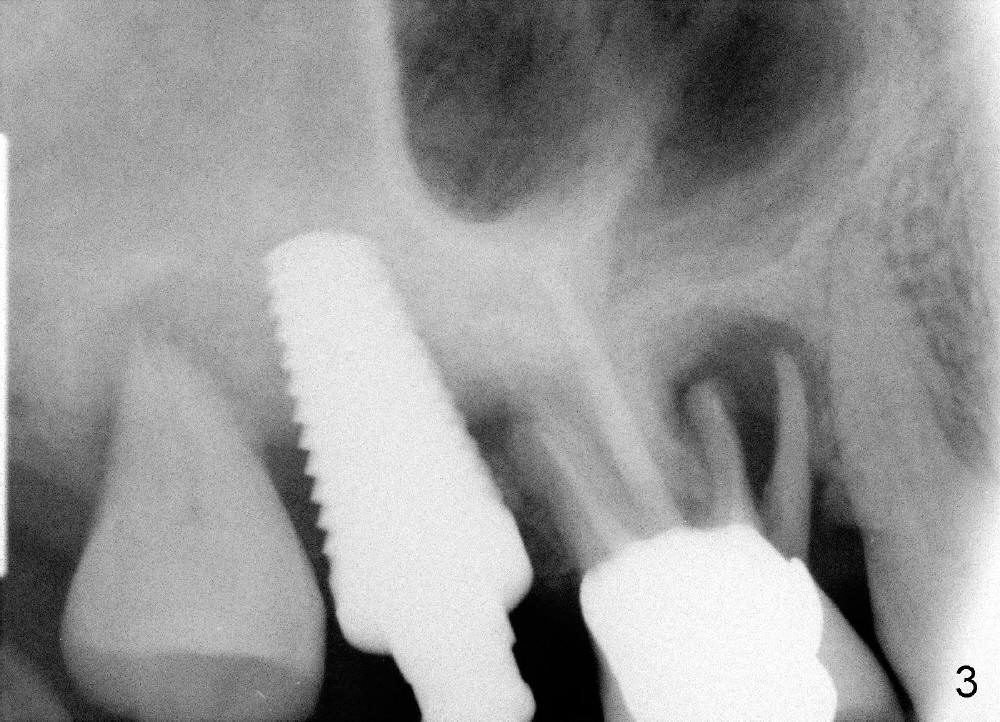
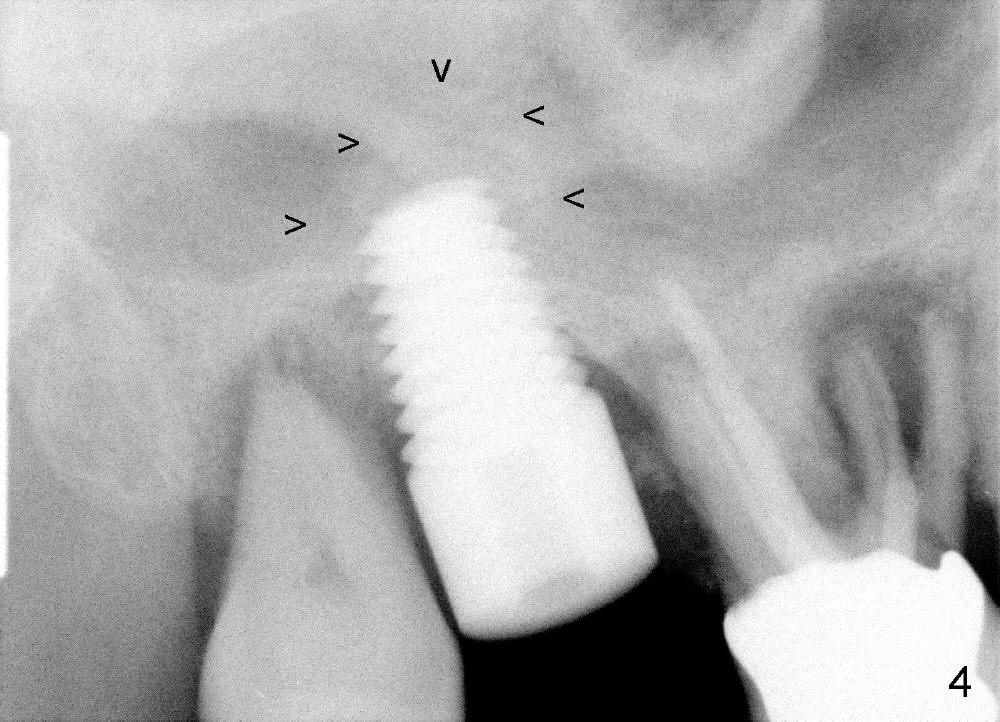
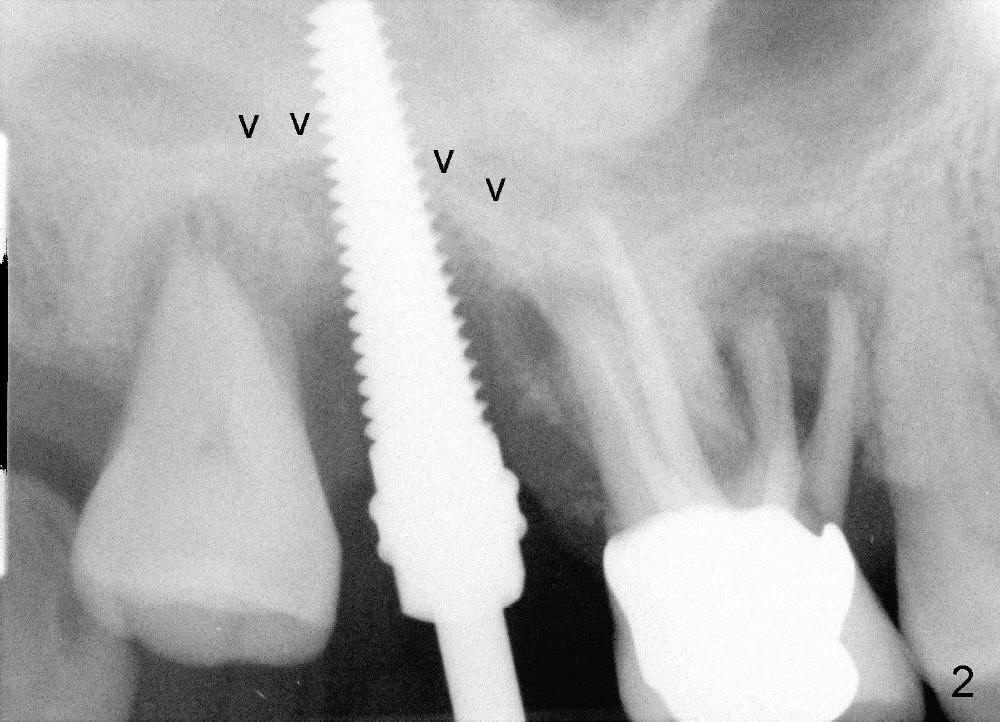
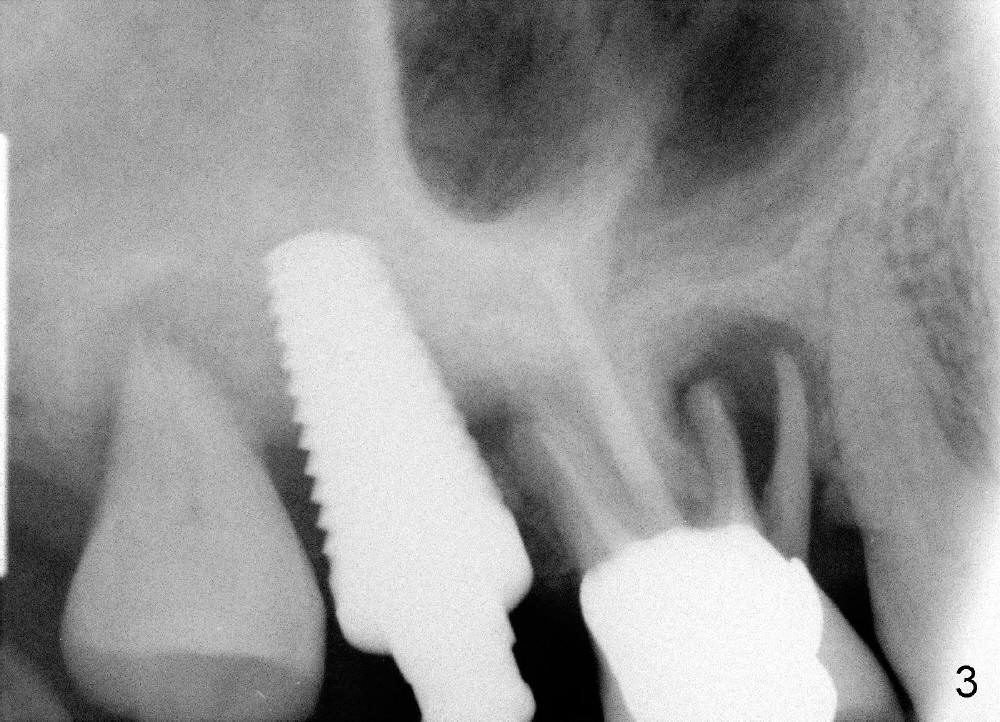
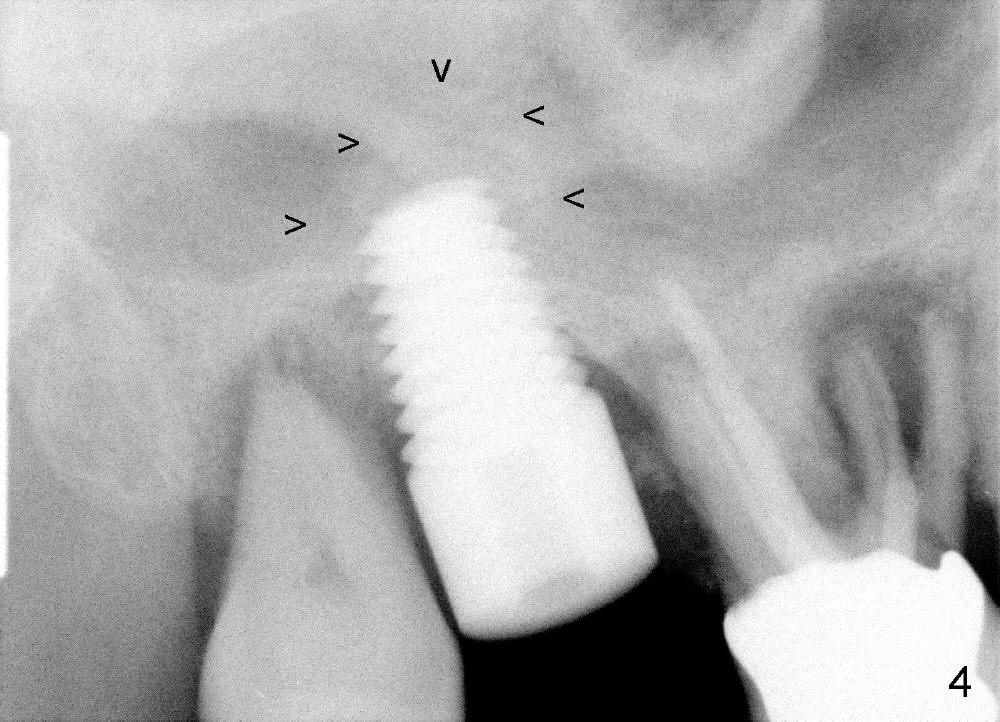
The upper right molars are deemed non-salvageable in a 60-year-old man (Fig.1). The tooth #2 is symptomatic. It is treated first. After extraction, osteotomes are used to create osteotomy (bone being solid) and sinus lift, followed by insertion of tap (Fig.2: 4.5x20mm). Arrowheads in Fig.2 indicate the upper border of the sinus floor. It appears that instrument is intruded too much into the sinus. Clinically the sinus membrane is perforated, as shown by nose blowing. The next bone manipulation instruments (taps 5-7 mm in diameter) should be shortened (17 mm). Fig3 shows a 7x17 mm tap in place with stability. Placement of 7x17 mm implant is associated with sinus lift (Fig.4 arrowheads).
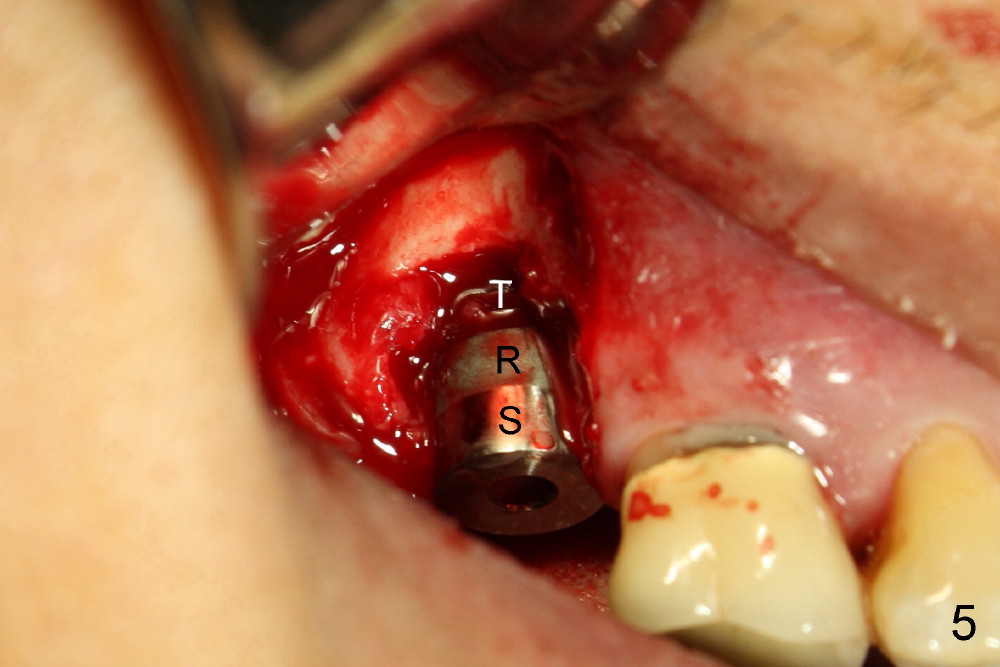
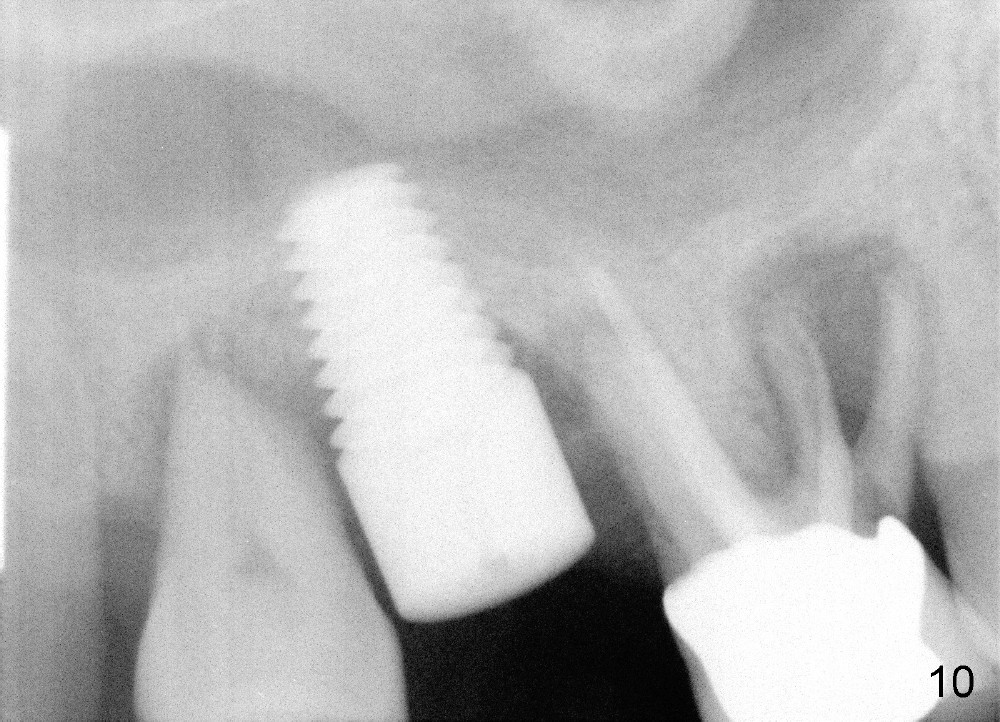
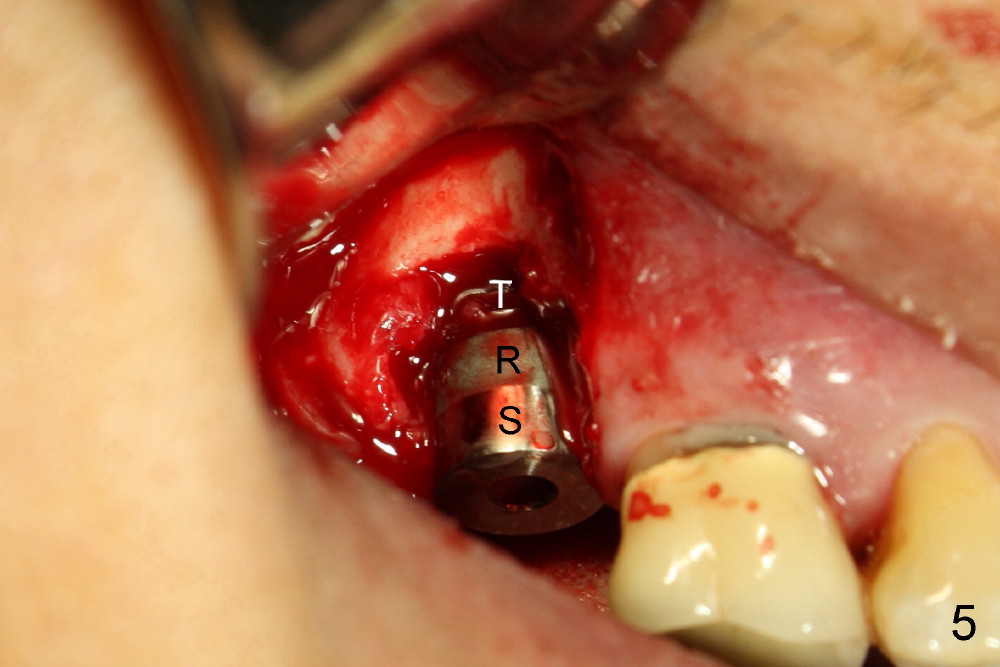
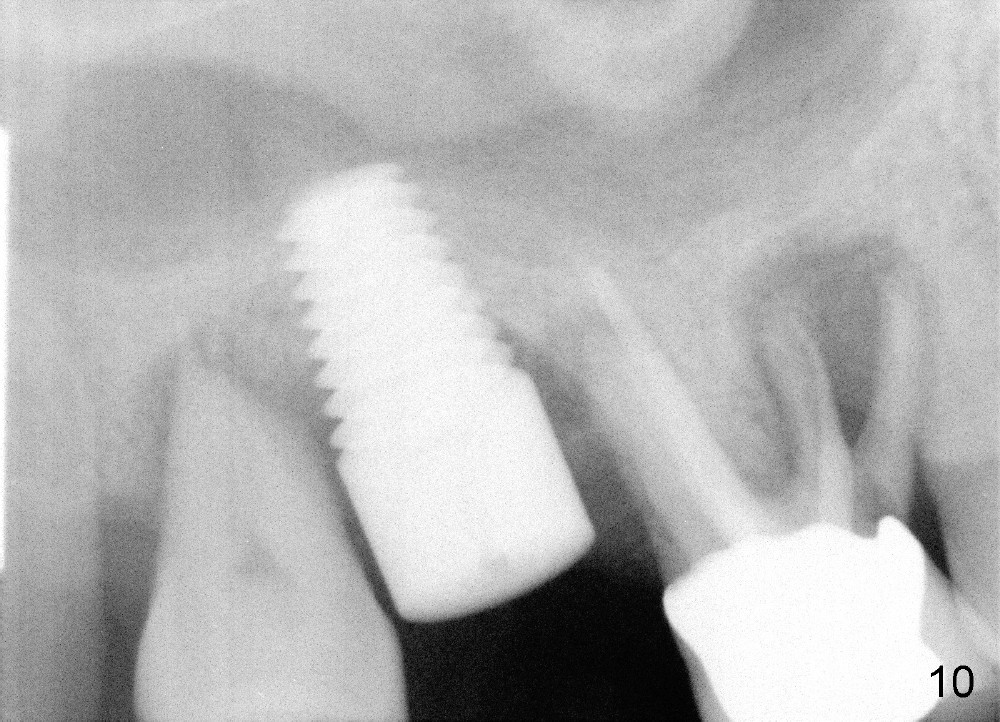
The implant threads (T) are exposed buccally. A flap is raised (Fig.5) with periosteum underscored. After placement of Osteogen (HA 300-500 Ám) and Collaform (a collagen membrane, Fig.6*), the flap is sutured. There is no intra- or post-op nasal hemorrhage. The wound heals (Fig.7 (5 days postop), 8 (18 days)). It is apparent that the membrane (Fig.7 *) is replaced by the healing gingiva (Fig.8 *). Three months postop, the buccal gingiva looks normal (Fig.9) around the stable implant (Fig.10).
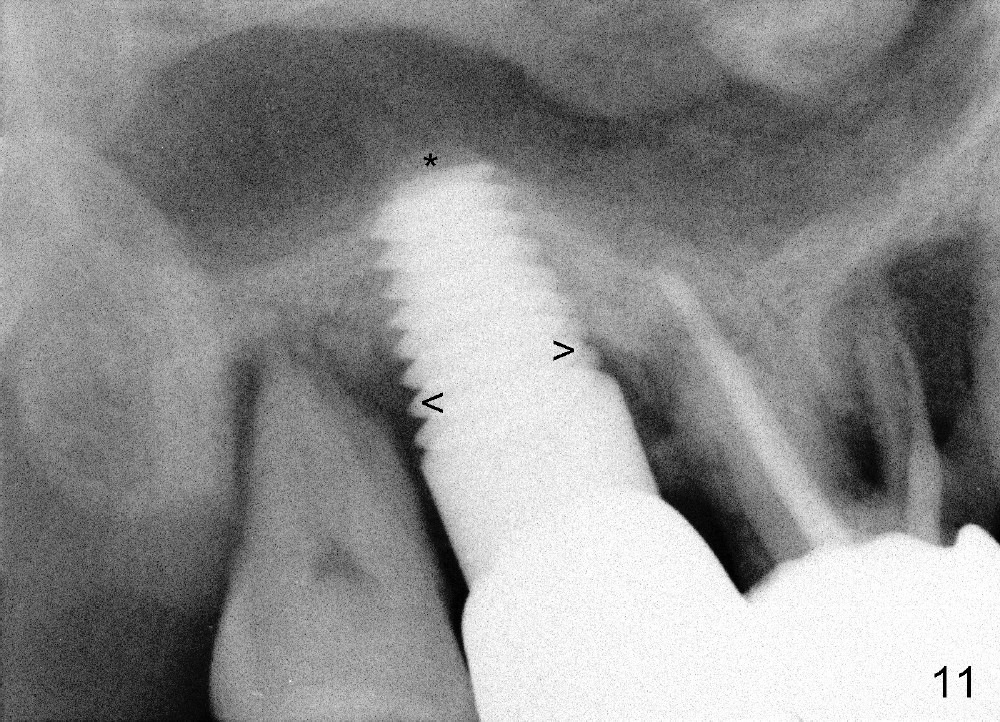
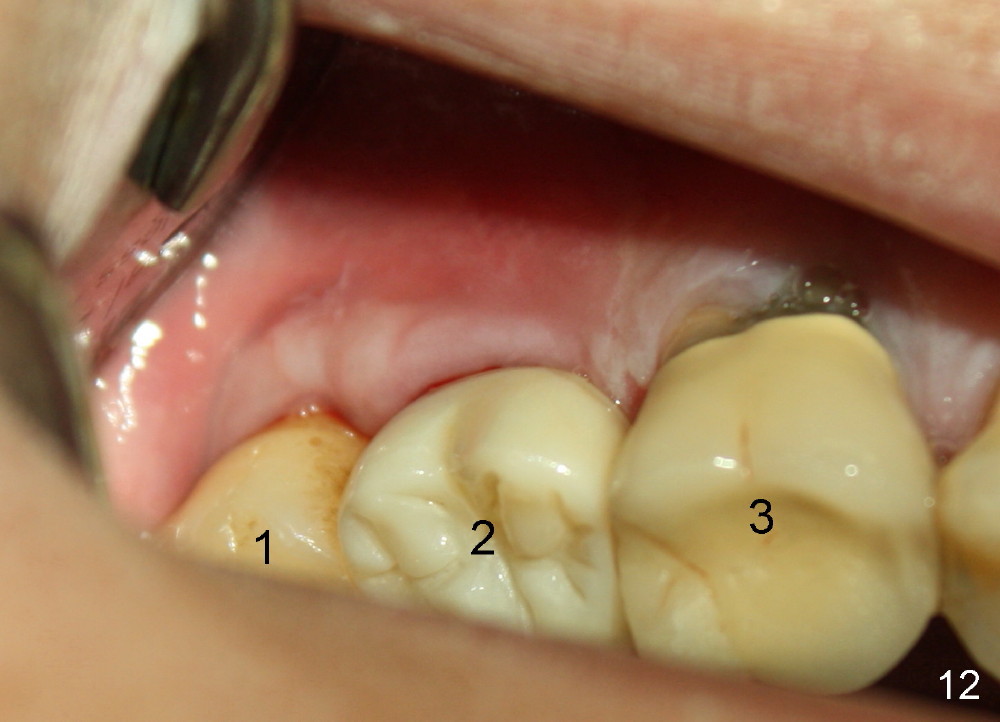
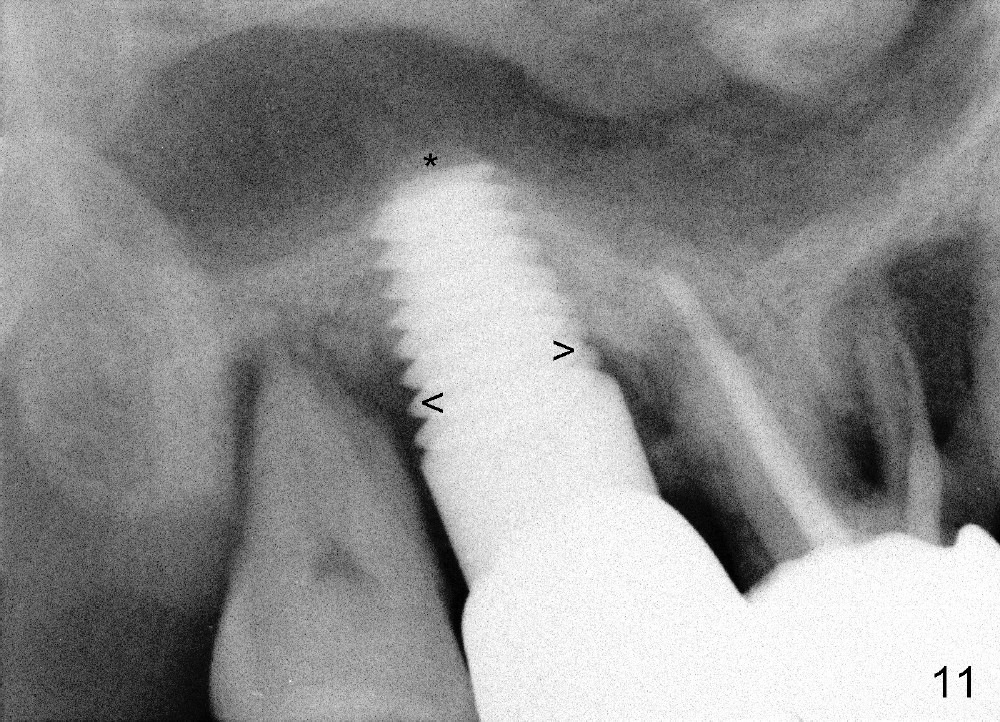
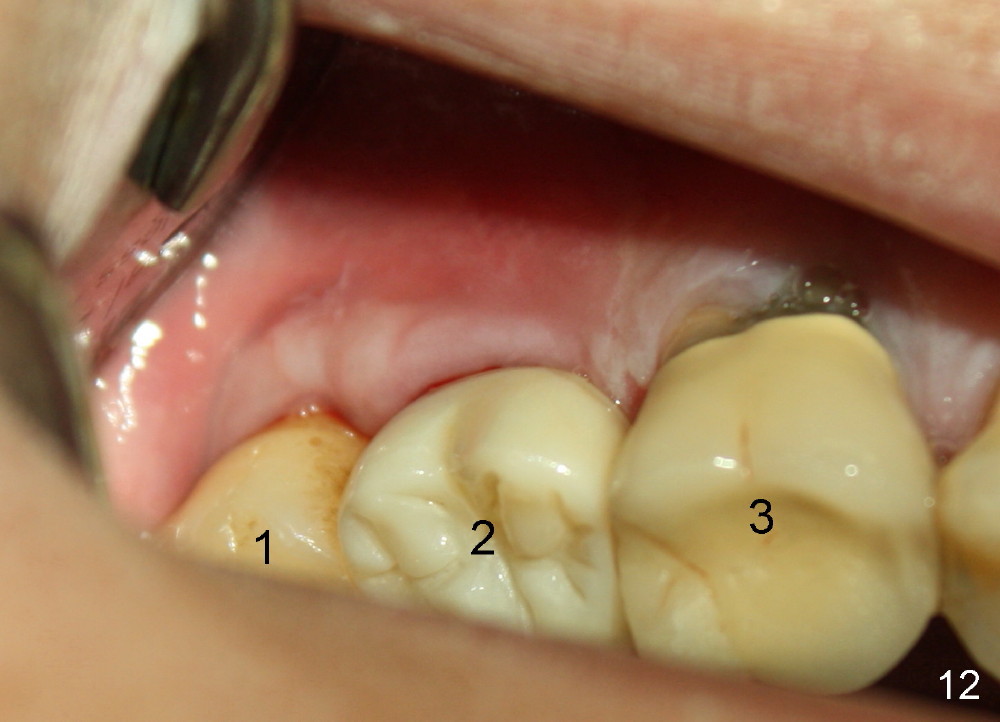
Six months post cementation, the patient returns for follow-up (Fig.11-14) with chief complaint of food impaction between the upper right last 2 teeth. It is difficult to remove. The distal 2nd thread appears not to be covered by the bone, whereas the mesial one is (compare Fig.11 arrowheads). The buccal gingiva is apparently within normal limit (Fig.12) except the distal (Fig.13 >). The distolingual gingiva recession is much more severe (Fig.14). There are deep pockets with tenderness in the abnormal sites. The tooth #1 has #2 mobility with tenderness. The patient agrees to have it extracted and restored with an implant, since the tooth #32 is functional. Bone graft will be placed in the lingual aspect of the implant at the site of #2.
Xin Wei, DDS, PhD, MS 1st edition 01/12/2014, last revision 11/08/2014