

 |
 |
|
 |
||
 |
 |
 |
 |
 |
|
 |
|||||
First Case of Immediate Implant for Upper Bicuspid
In this case, we discuss how to get an immediate implant in and how to close the socket.
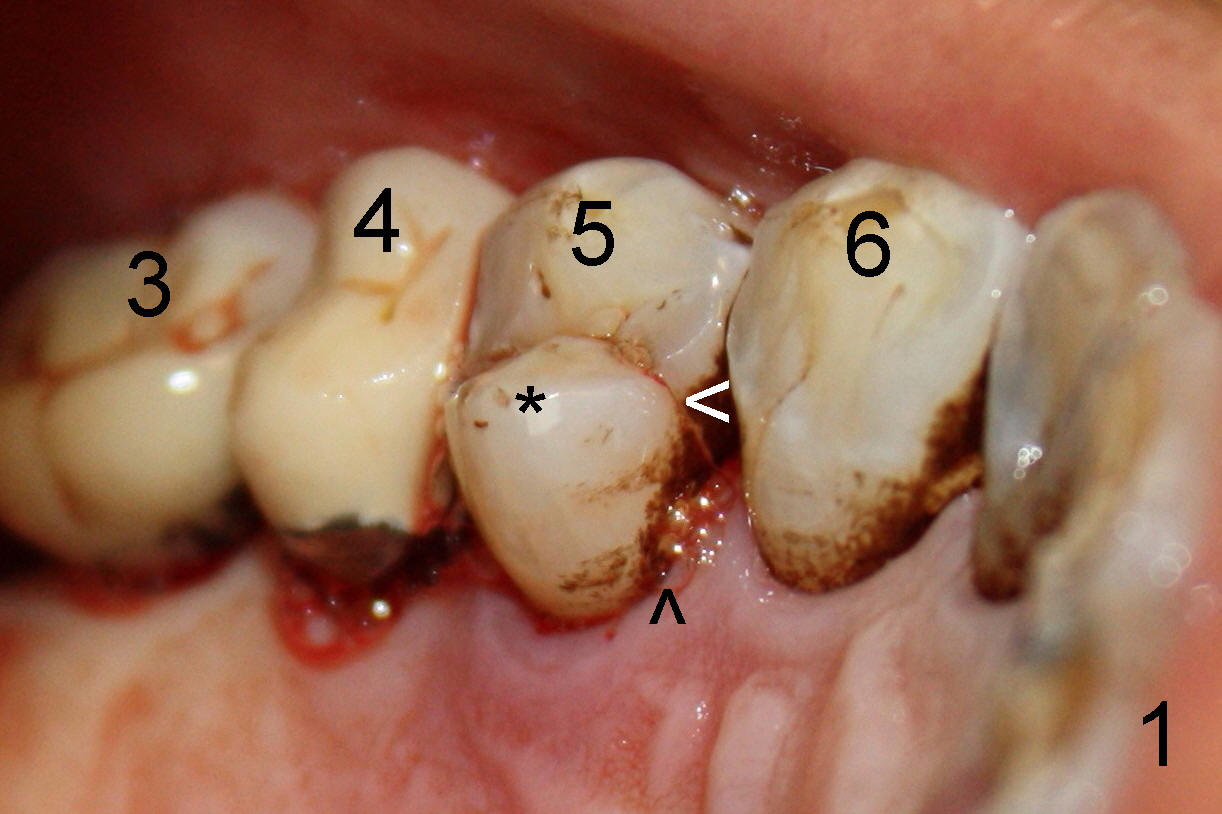
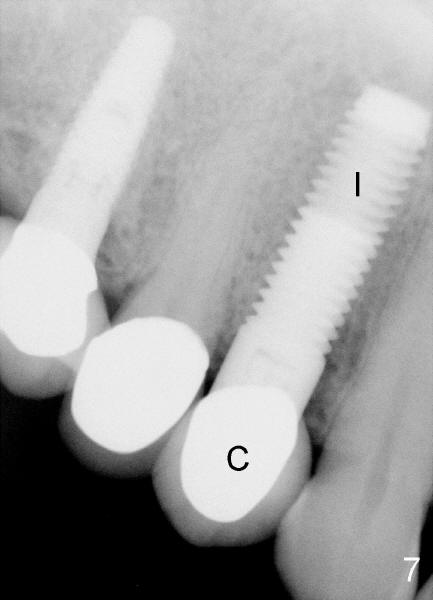
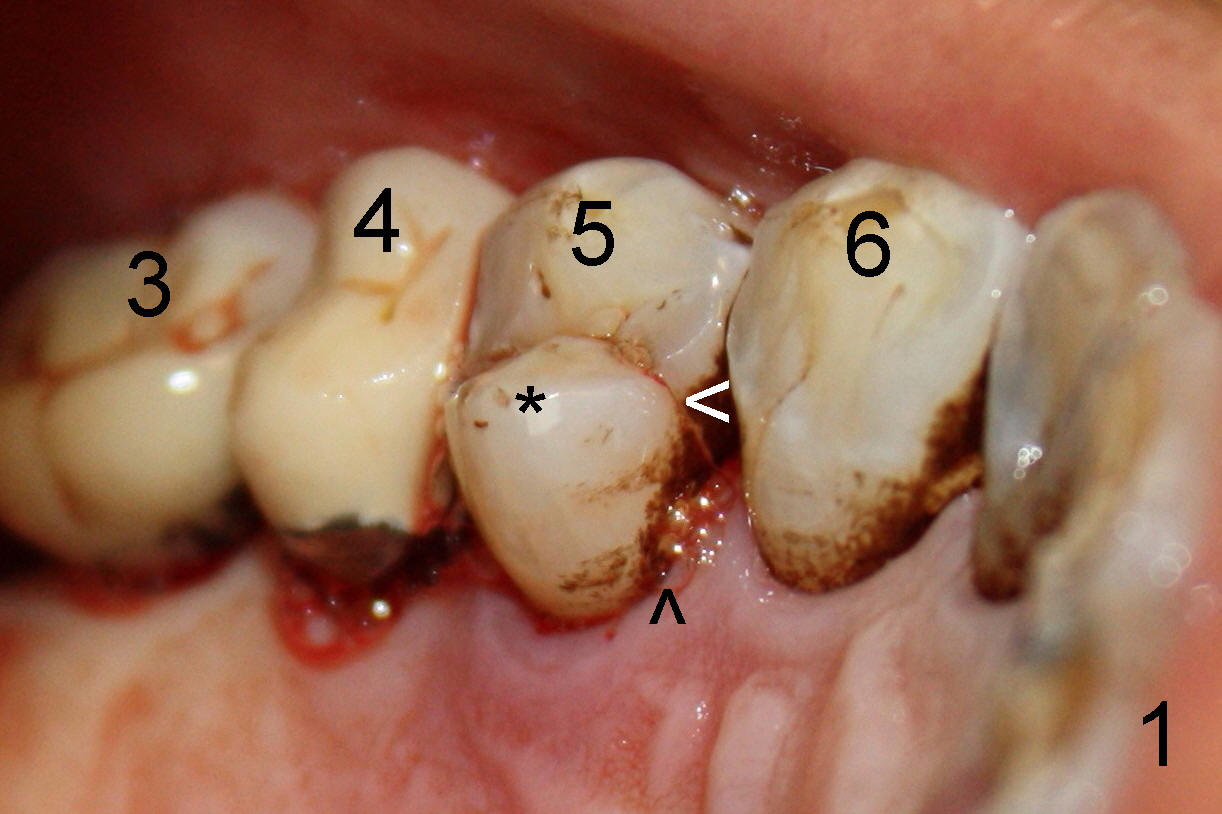
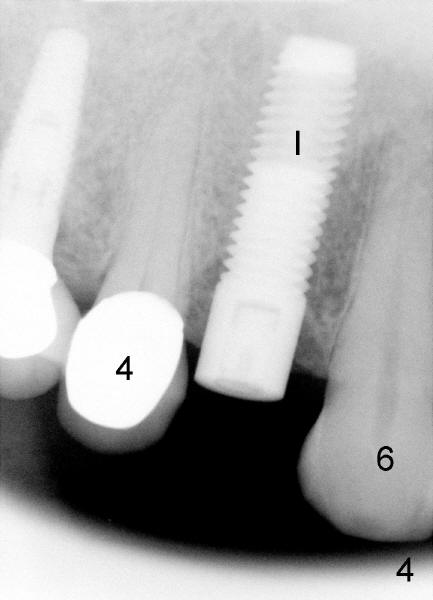
The patient is a 68-year-old male. There are multiple existing restorations, including #3,4 (Fig.1,3). The tooth #5 has a fracture line (Fig.1<). The lingual fragment is mobile (*). The pulp is exposed (Fig.3 ^).
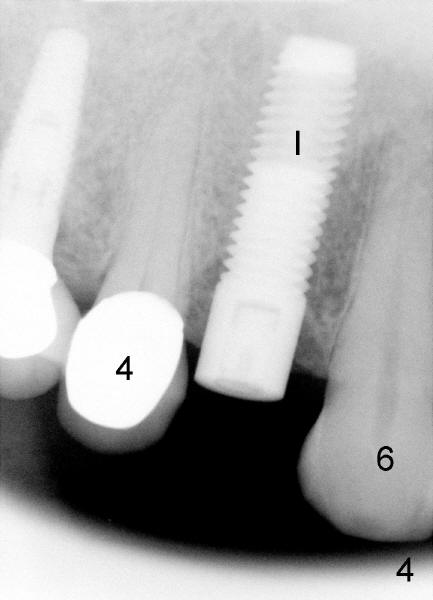
Extraction involves sectioning the crown from the roots and splitting the roots with surgical fissure bur. Osteotomy is initiated with 2 mm pilot drill in the lingual socket toward the septum at the depth of 20 mm, followed by pointed tapered osteotomy 2-5 mm at the same depth. There is not much resistance when 5x20 mm tapered tap is engaged. Following using 4.5x20 mm rounded pointed osteotome with some binding, a 5x20 mm cylinder tissue-level implant is placed (Fig.4 I). The socket is closed by advancing the buccal flap with underscoring the periosteum.
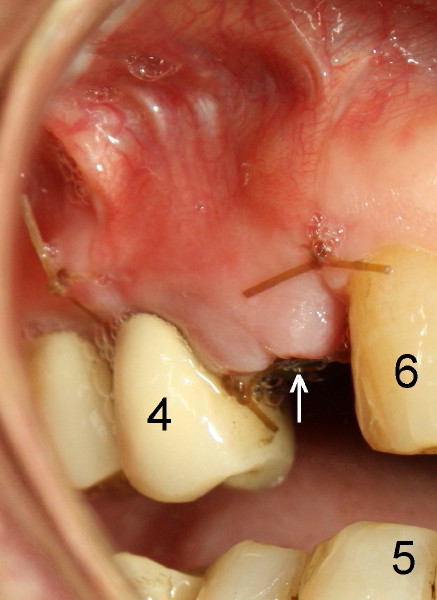
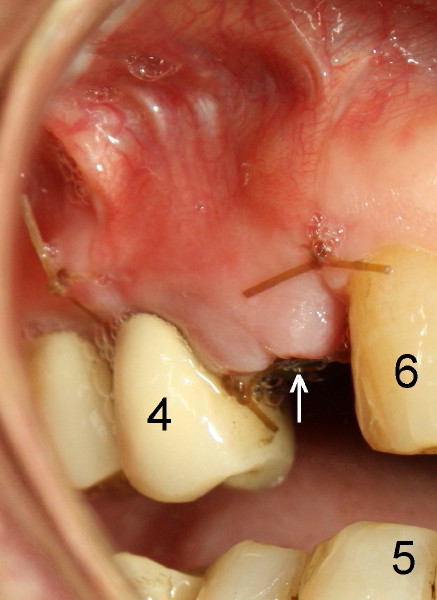
Fig.5 photo is taken one week after placement of implant (arrow). The sutures had not been dissolved.
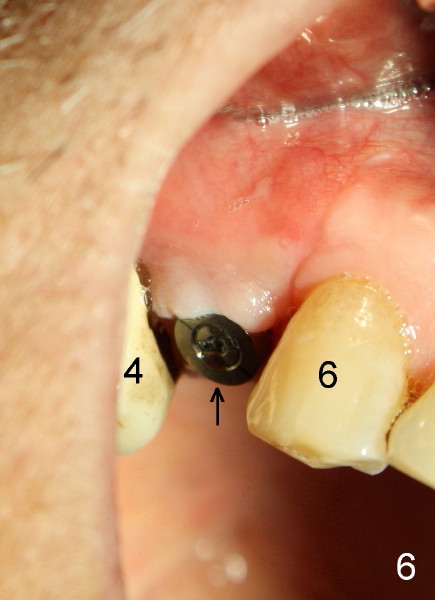
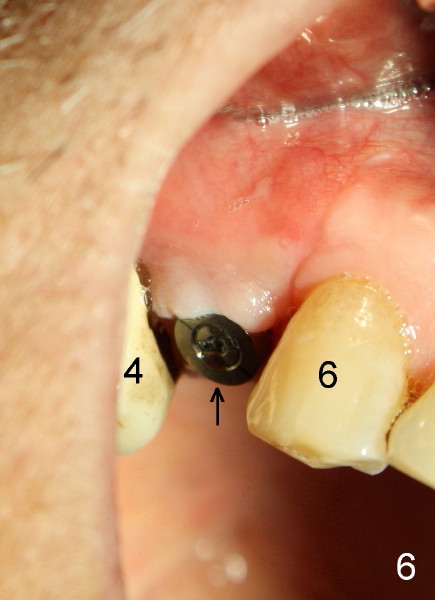
Fig.6 is taken three months after implant placement. The wound has healed around the implant (arrow). The papillae are displaced, most likely due to flap raising to close the socket.
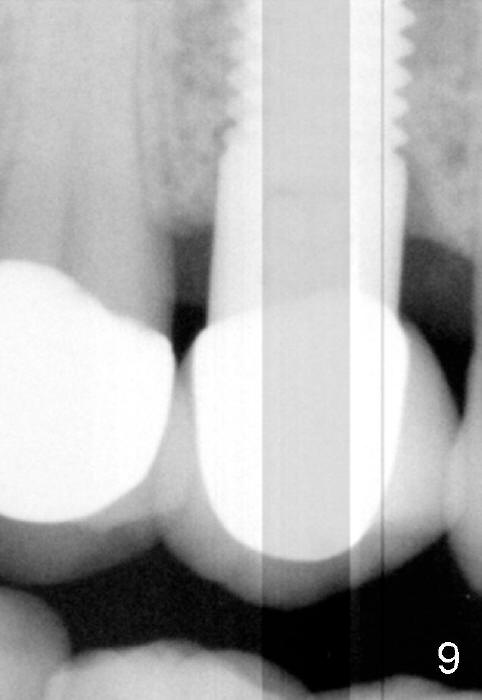
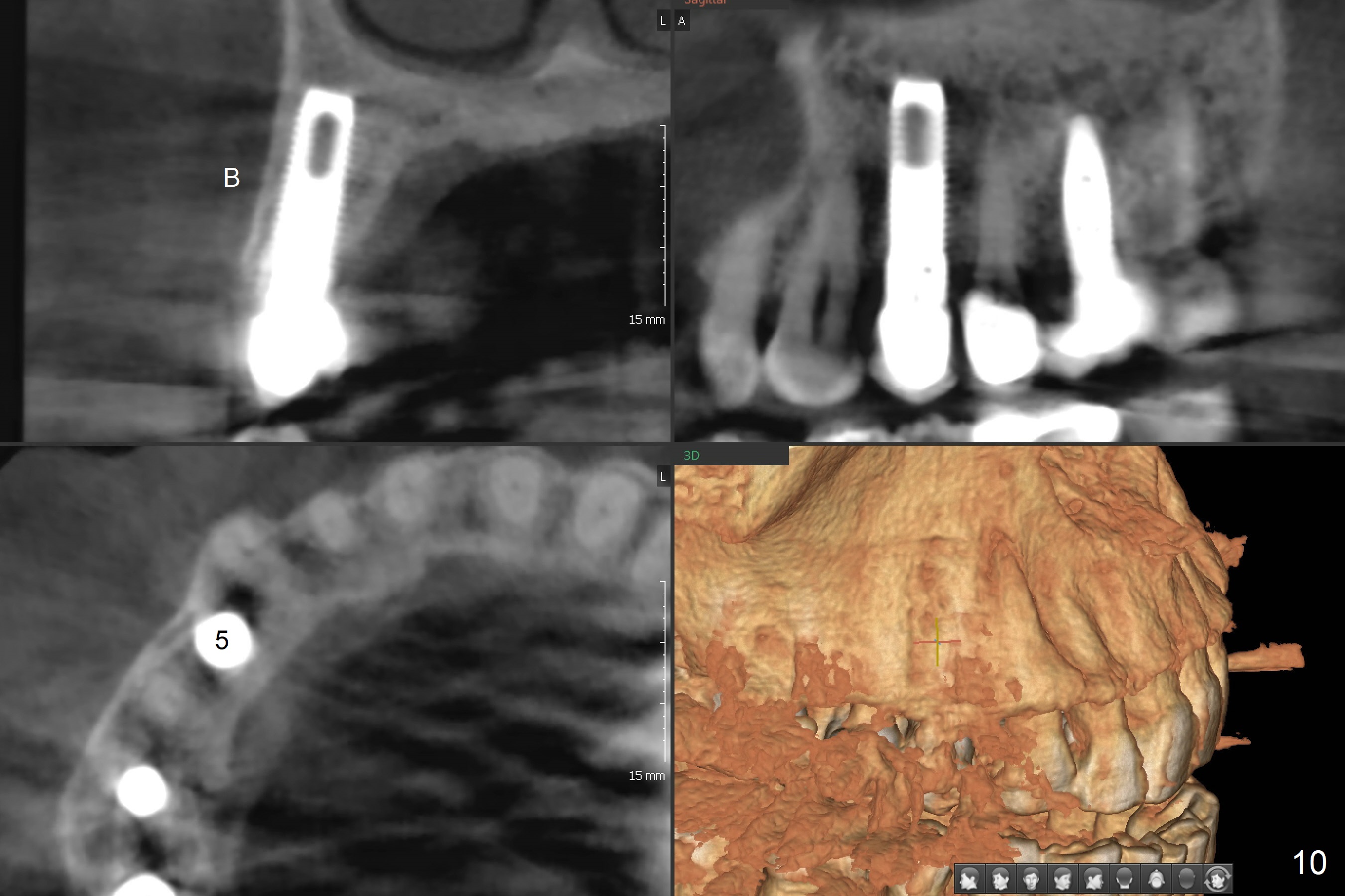
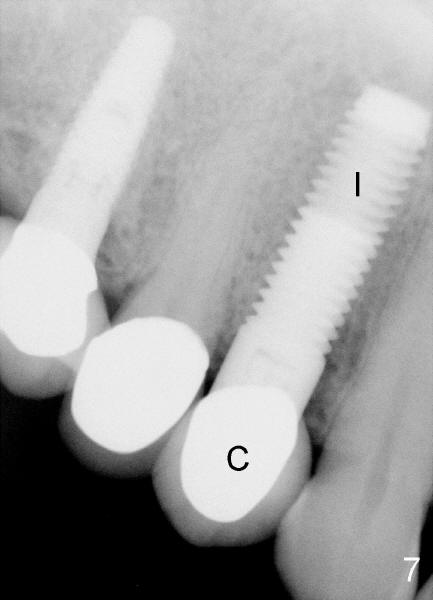
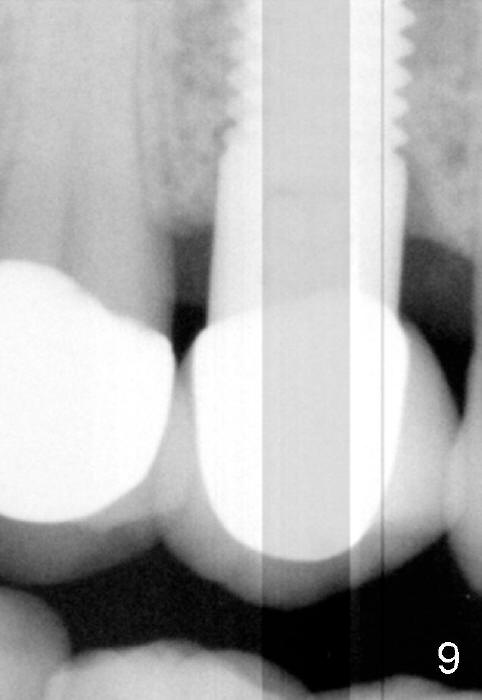
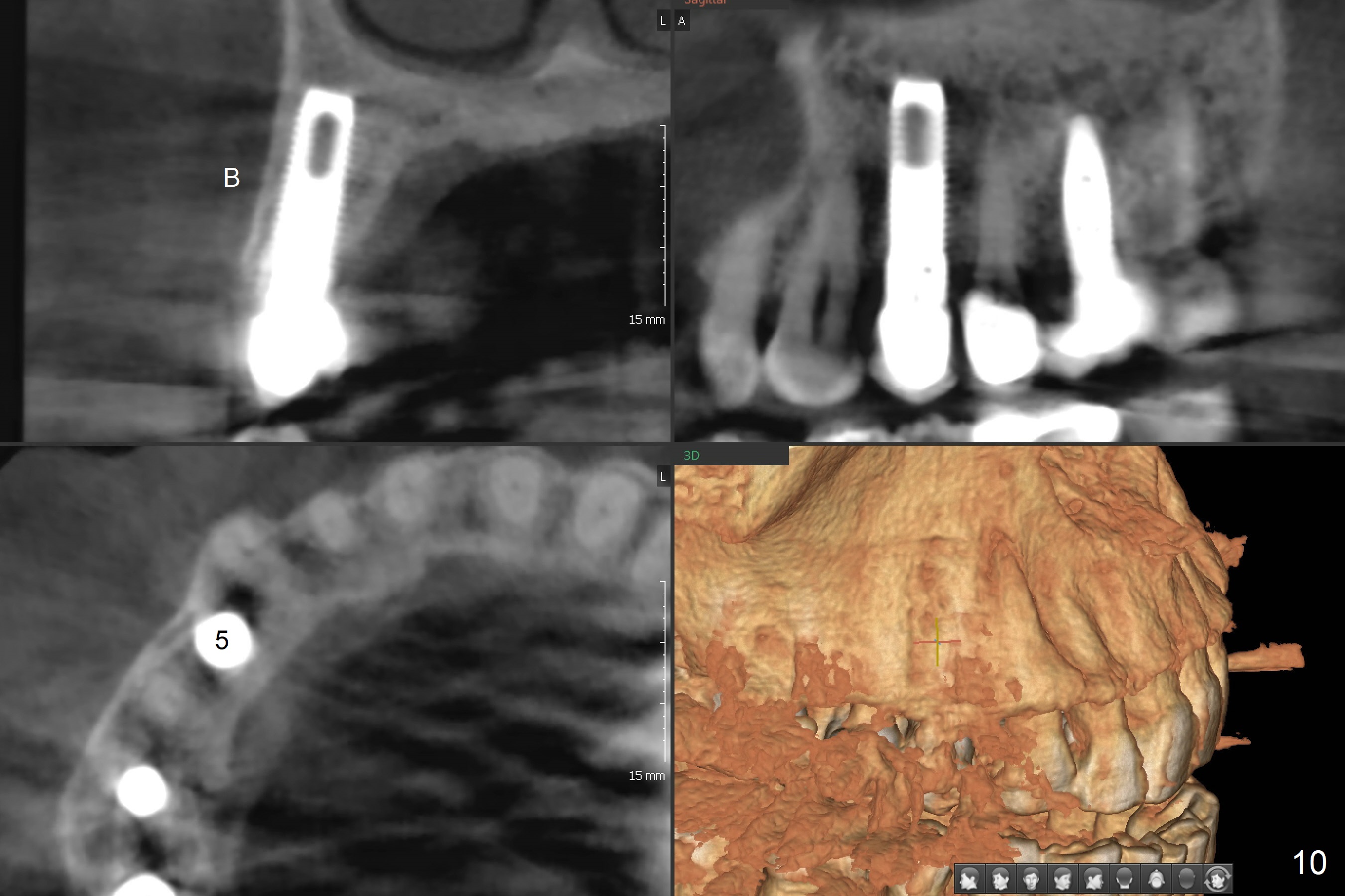
A crown is cemented 3 and a half months post implant placement. Fig.7 shows the crown (C) 3 months after cementation. The patient has had no problem in chewing with the new tooth for 9 months (Fig.8: #5). The flap surgery also causes recession of the second bicuspid (compare to Fig.5). Gingival issues may be noted by young female patients. Therefore, flap surgery should be avoided for cosmetic purpose. Instead, immediate provisionalization is a better solution to socket closure. In spite of soft tissue issue, there is no bone loss around the implant 2 years and 2 months in function (Fig.9, as compared to Fig.4,7). The bone remains stable 6.5 years post cementation (Fig.10 CBCT).
Upper Bicuspid Immediate Implant, Long term follow up of this case #13 14 Xin Wei, DDS, PhD, MS 1st edition 12/18/2011, last revision 06/12/2019