



 |
 |
 |
|||
 |
 |
 |
 |
 |
 |
 |
 |
 |
|||
 |
|||||
Cosmetics and Immediate Implant at the Upper 1st Bicuspid
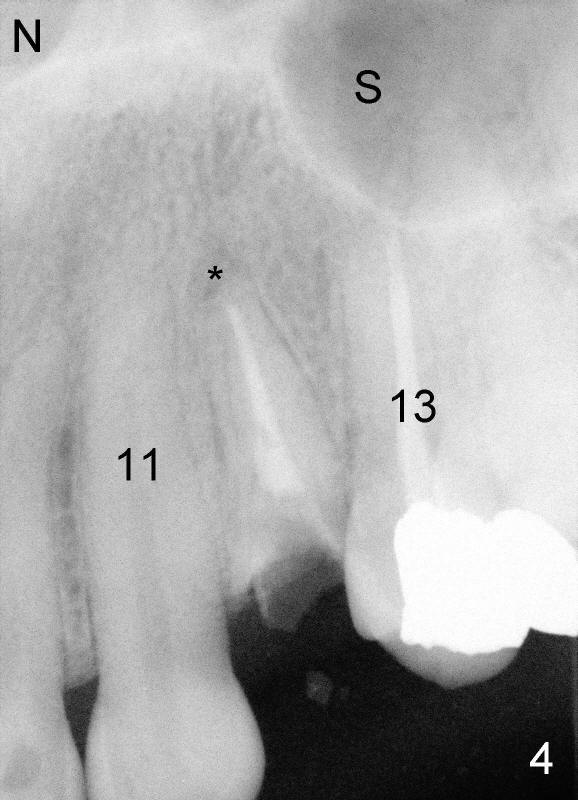
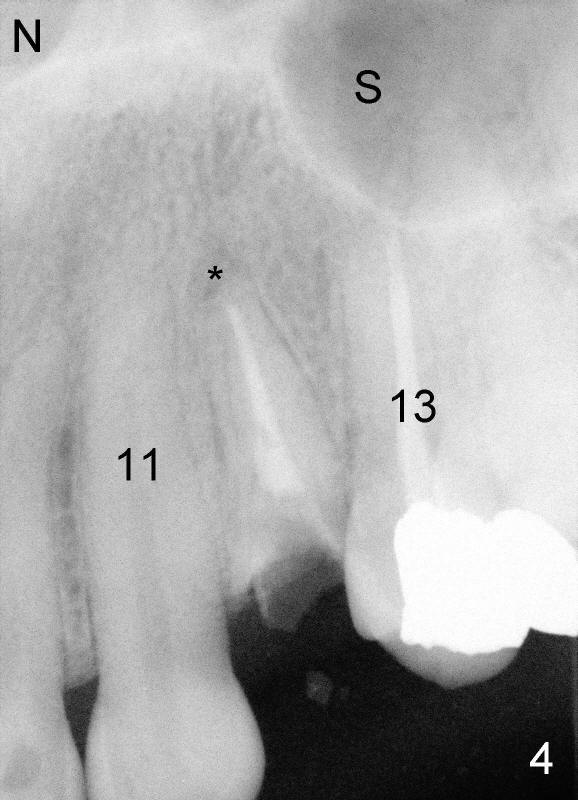
The second patient who is going to have an immediate implant in the upper bicuspid region is a 41-year-old lady. She is extremely scared of dental treatment. The second challenge is a periapical lesion associated with residual roots (Fig.1,2,4, as compared to freshly fractured tooth in the first case).
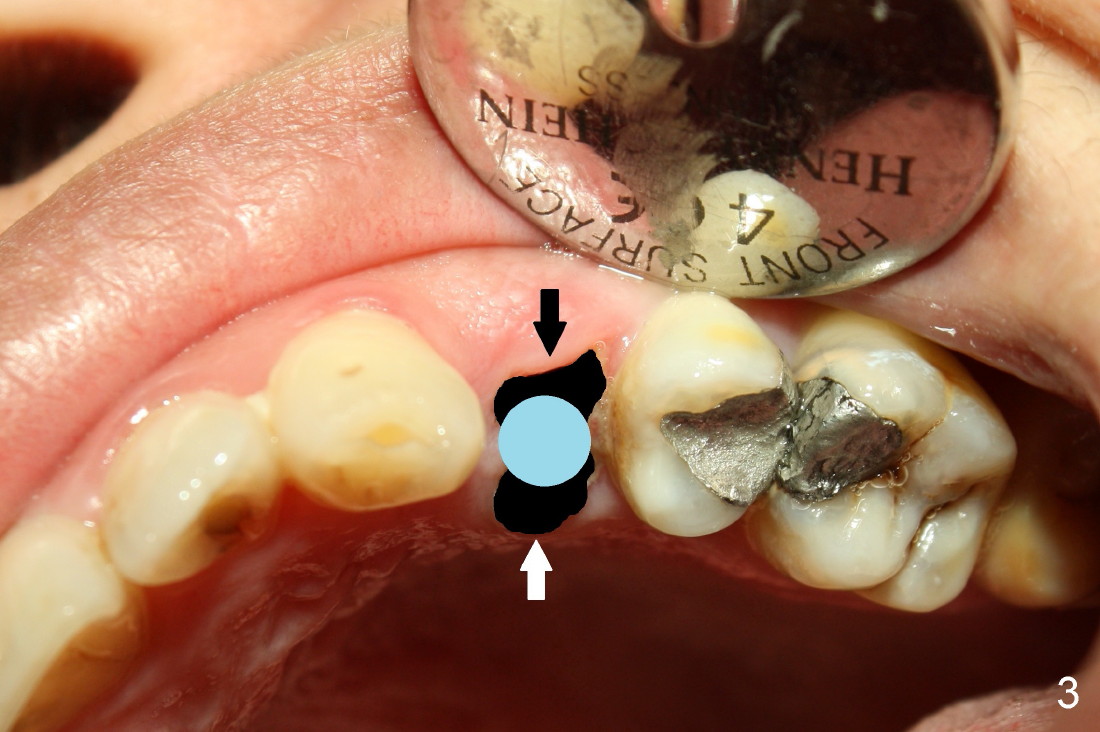
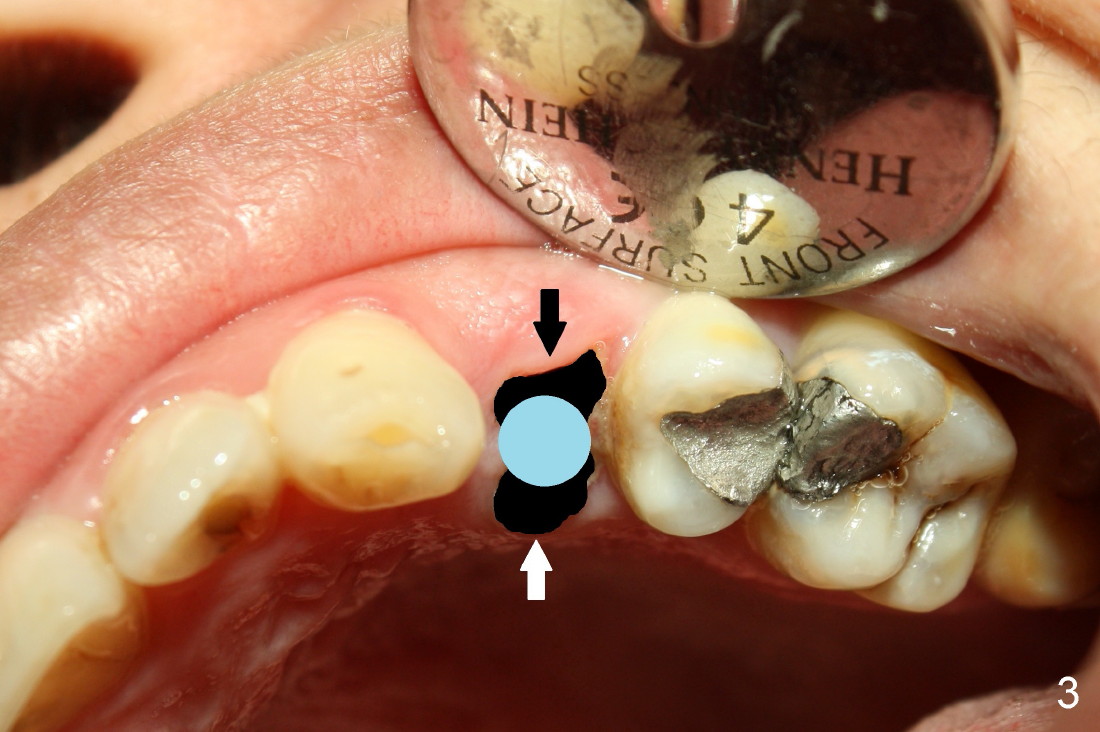
Fig.2 (occlusal view) shows the oval socket (buccolingual width vs. the mesiodistal one). It appears that when a rounded implant is placed, the buccal and lingual flaps should be raised and and advanced to close the socket (Fig.3).
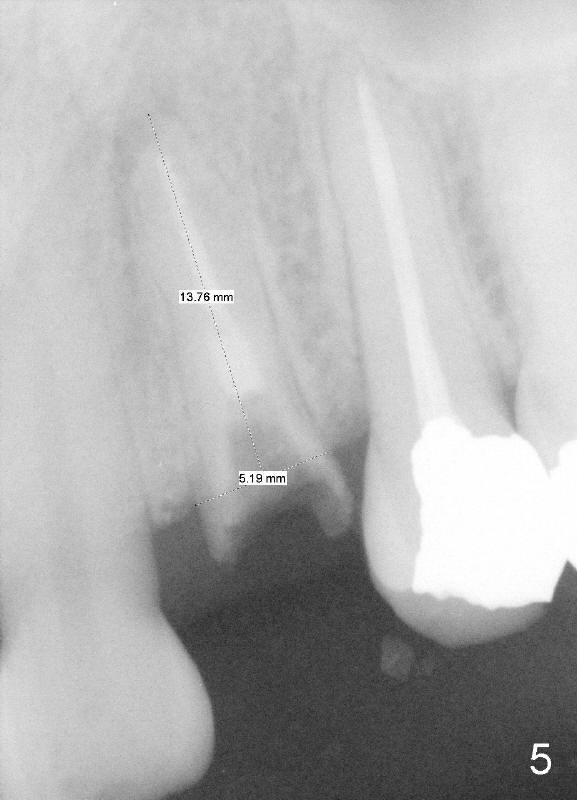
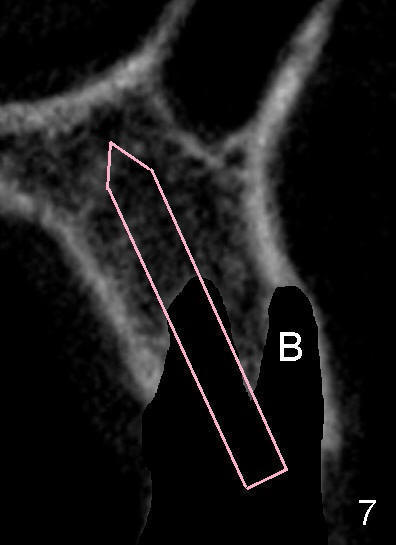
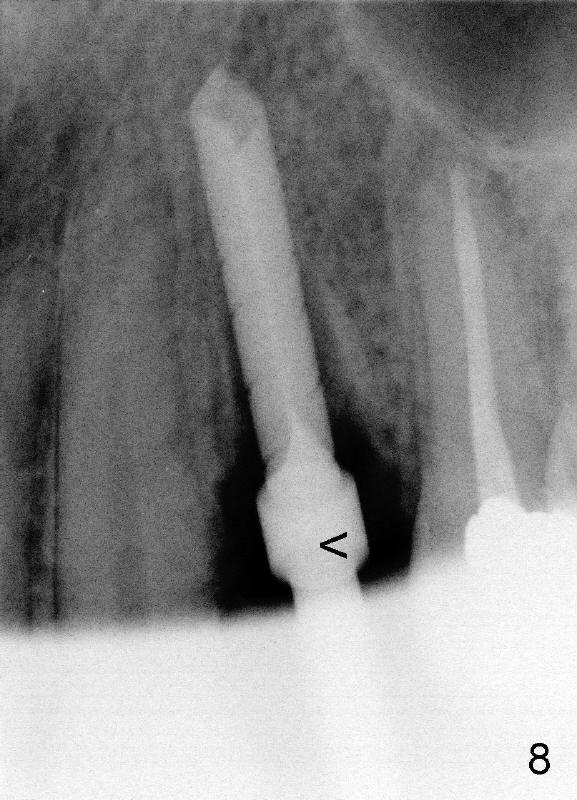
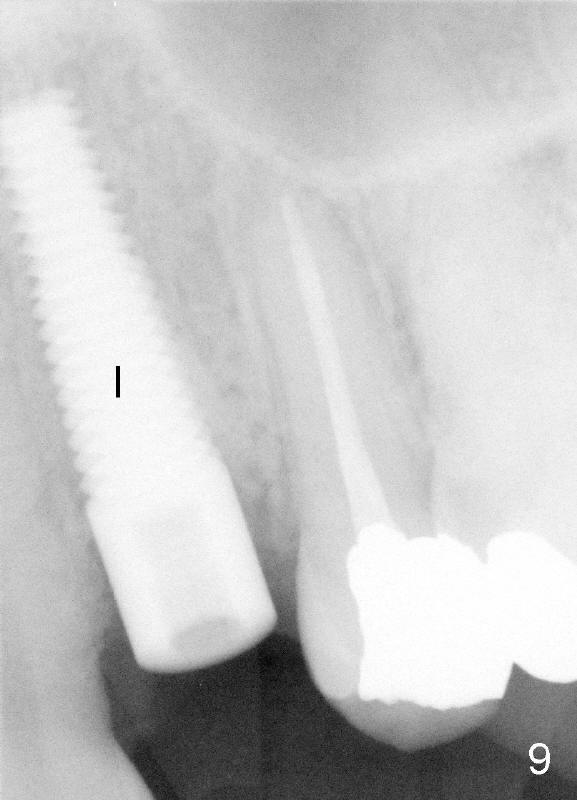
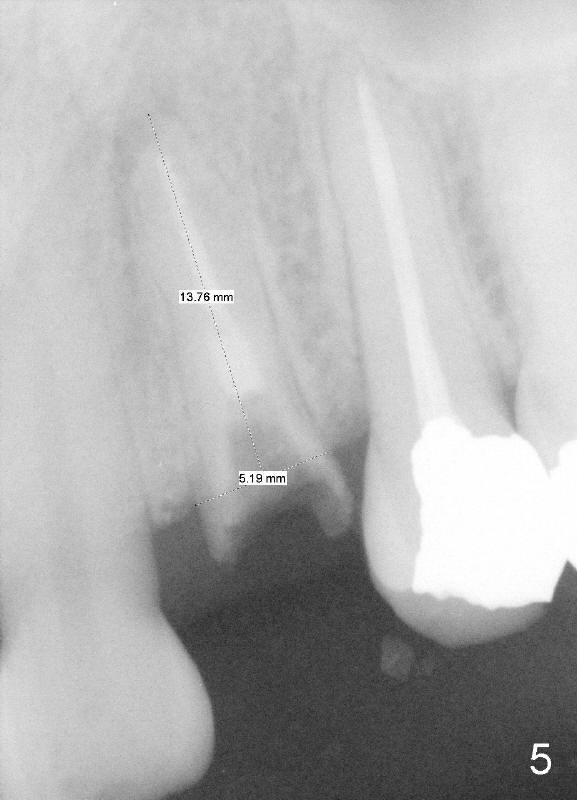
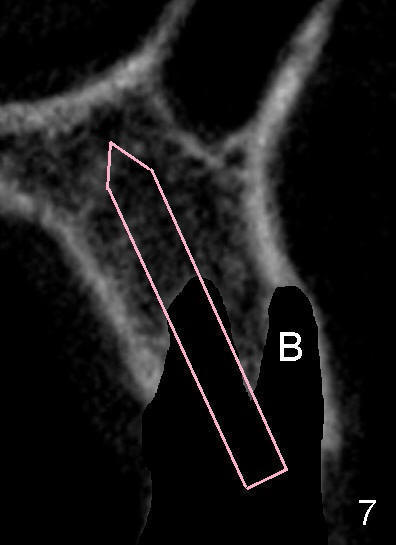
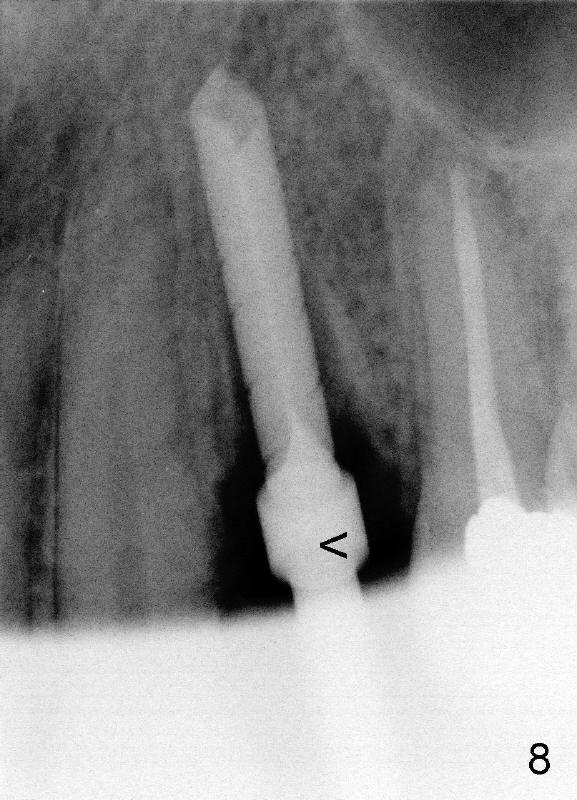
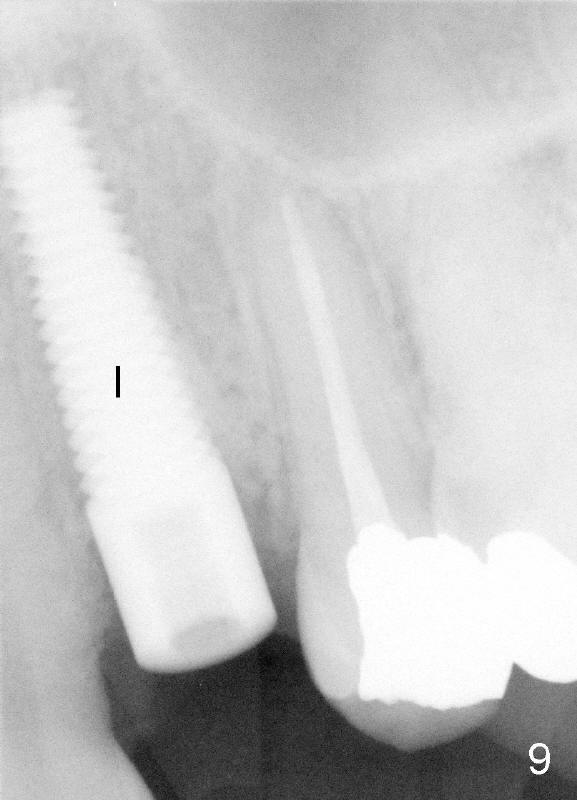
After tooth extraction, the osteotomy is initiated in the palatal socket (compare Fig.6,7 (CBCT, not the same case) with a pilot drill (pink outline). The osteotomy is enlarged by a series of reamers until the apical diameter (3.5 mm, Fig.8) of the prospective tapered implant (5x20 mm, Fig.9 I). The socket is obliterated by the tapered implant (Fig.9) with simultaneously achieving primary stability. This looks less over engineering than the first case.
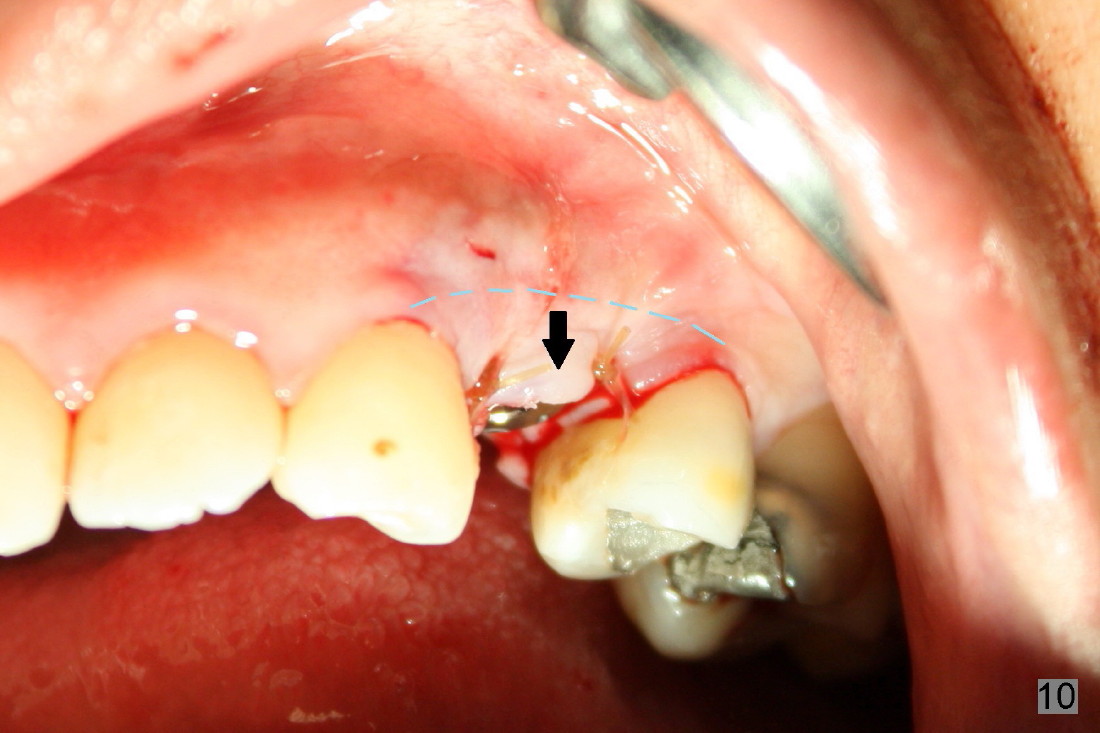
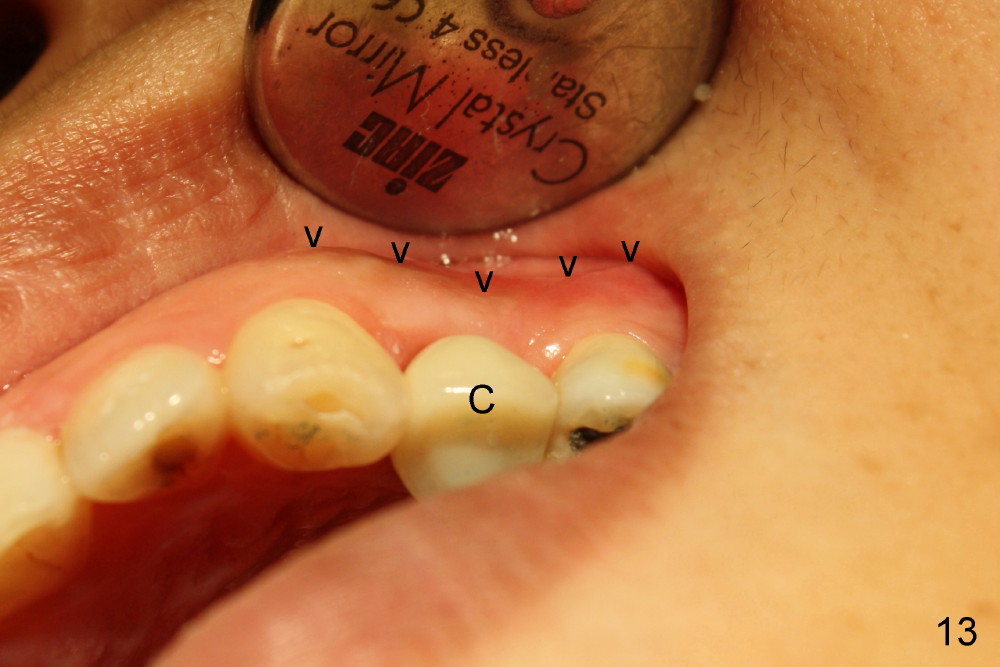
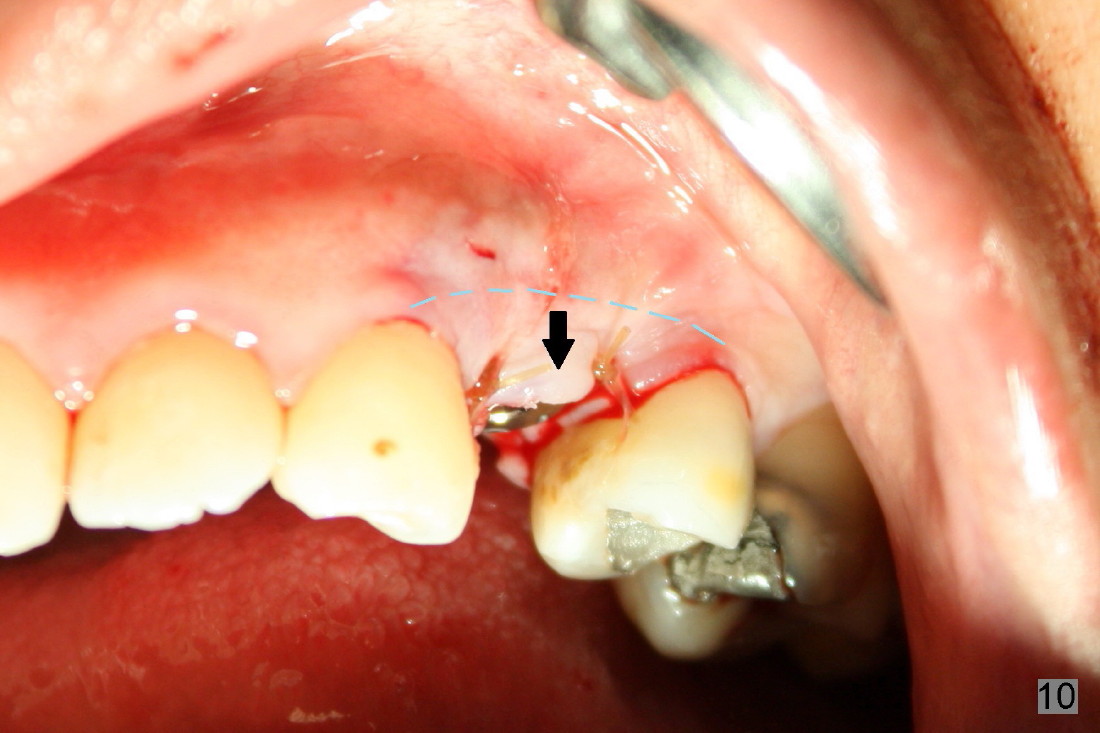
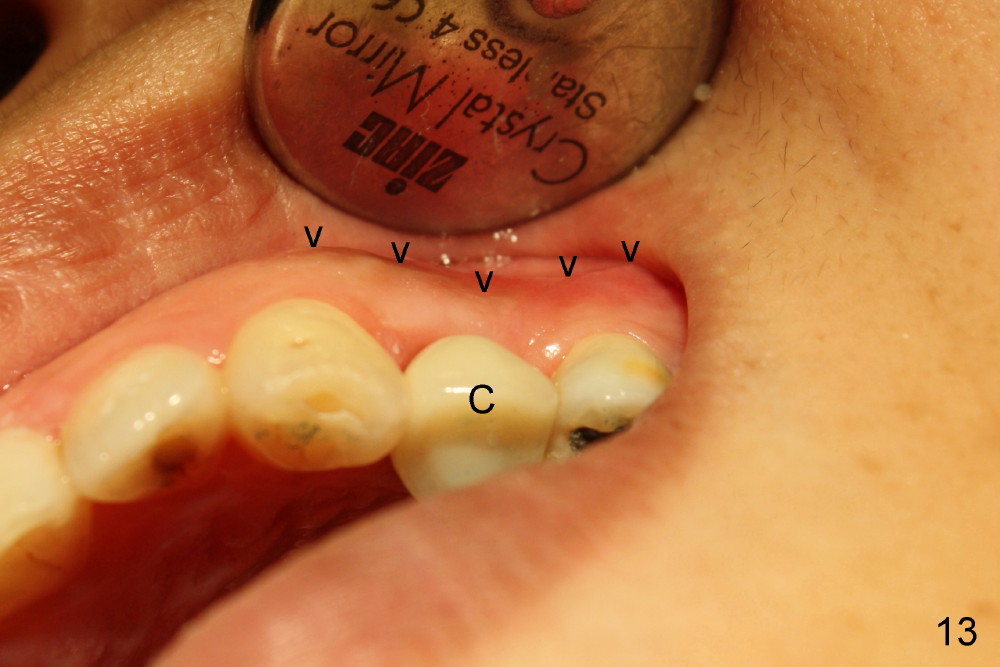
The closure of the socket involves raising and advancing both buccal and lingual flaps (Fig.10,11). When a crown is cemented, the patient is not pleased with recessive papillae (Fig.12 (arrowheads),13). It appears that flaps should be avoided to prevent cosmetic issue. Immediate implant is not enough for cosmetics; immediate provisional can close the extraction socket and support the papillae.
Upper Bicuspid Immediate Implant
Xin Wei, DDS, PhD, MS 1st edition 12/02/2012, last revision 09/09/2018