









 |
 |
 |
|
 |
 |
 |
|
 |
 |
 |
 |
 |
 |
 |
|
2nd Bone Graft
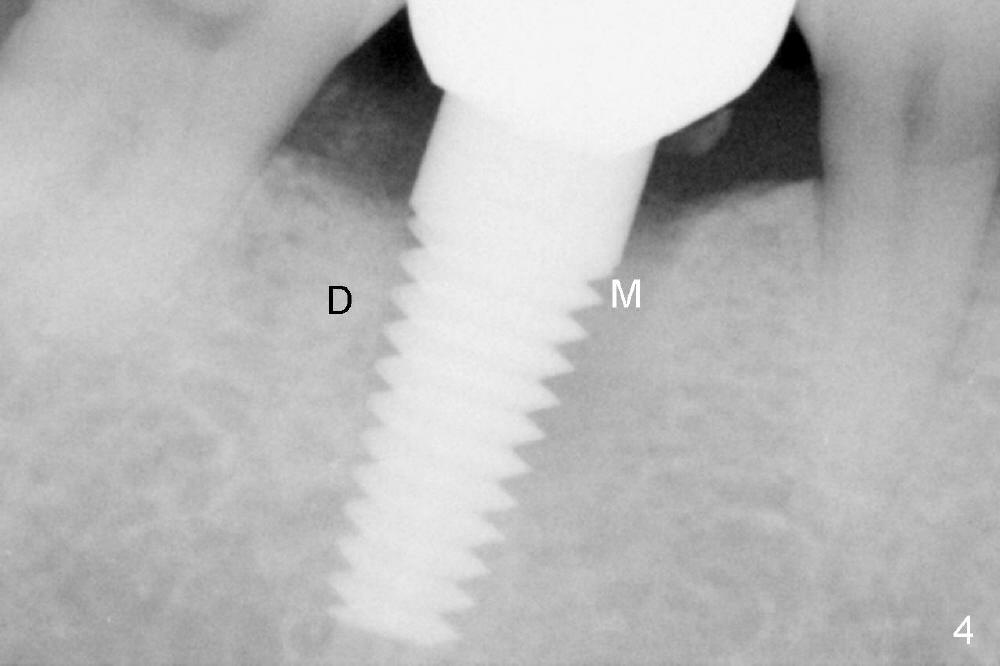
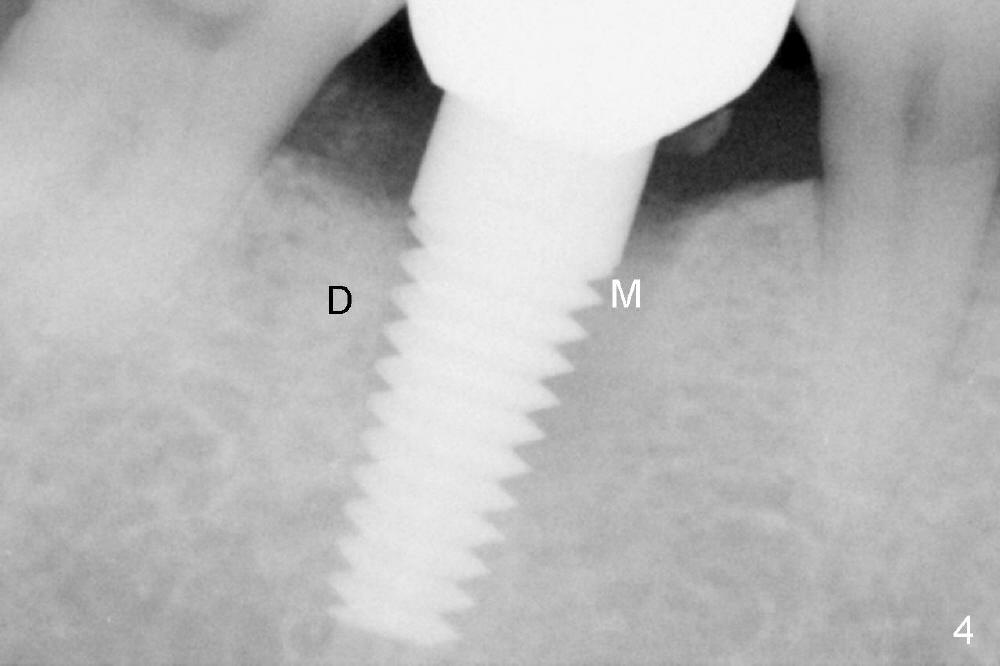
Thirteen months post bone graft via buccal approach, the patient has remained asymptomatic. There is no sign of infection buccally (Fig.1), but the lingual gingiva is erythematous (Fig.2 arrowheads) with deep pocket (Fig.3). Since the patient will be out of country for 7 months, exploration is going to be done immediately. Preop PA reveals mesial bone loss (Fig.4 M).
Upon flap reflection and granulation tissue curettage, the lingual threads are shown to be exposed with mesial bone resorption (Fig.5 <). The lingual defect is soaked with Clindamycin saturated gauzes (Fig.6 *), followed by copious irrigation, Emdogain application, bone graft and collagen dressing. The flap is sutured and covered by perio dressing.
The chronic infection with bone loss is probably due to two factors. No bone graft was placed at the time of immediate implant. The infection might come from the extraction site (due to incomplete debridement of the socket) or from a remote area: #9 endo perio lesion.
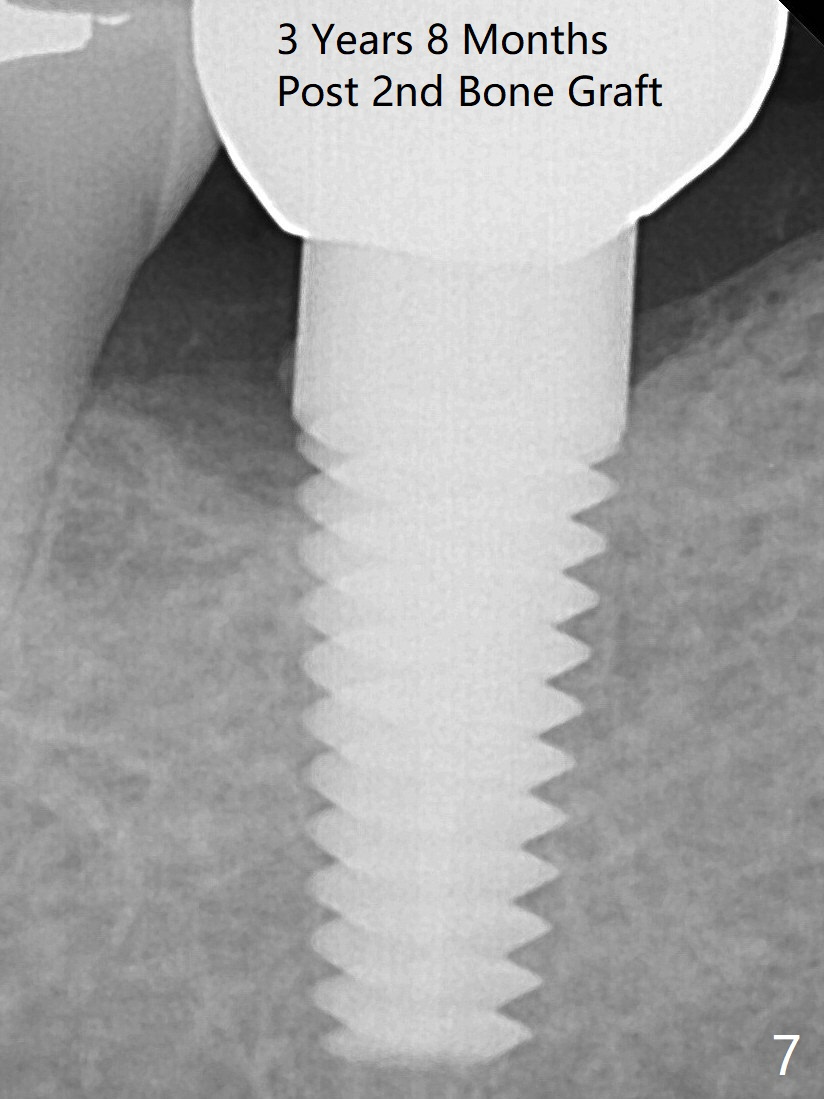
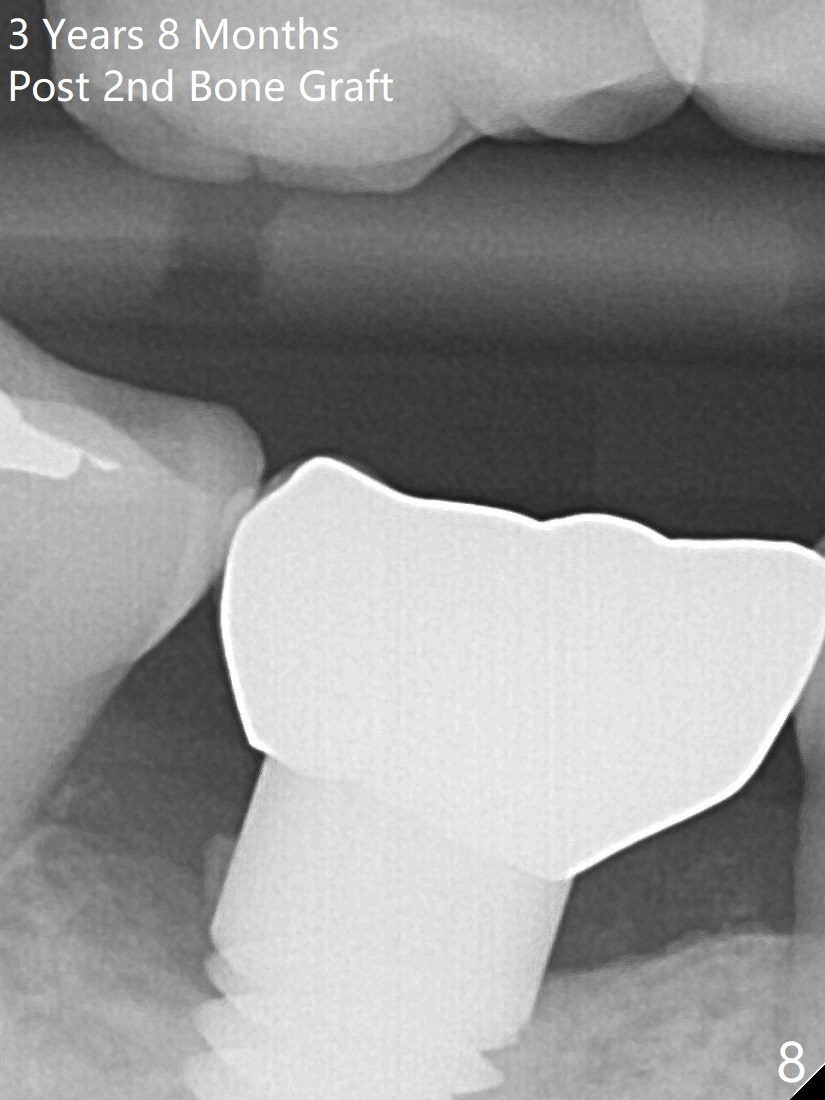
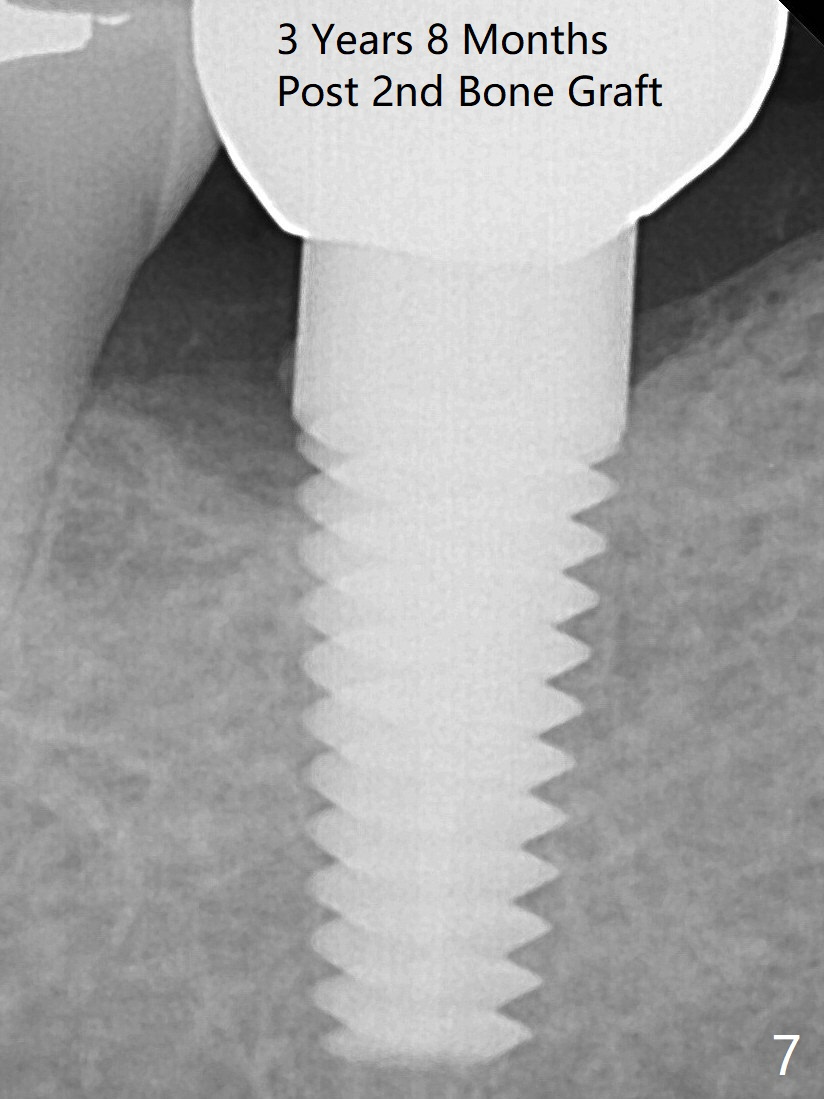
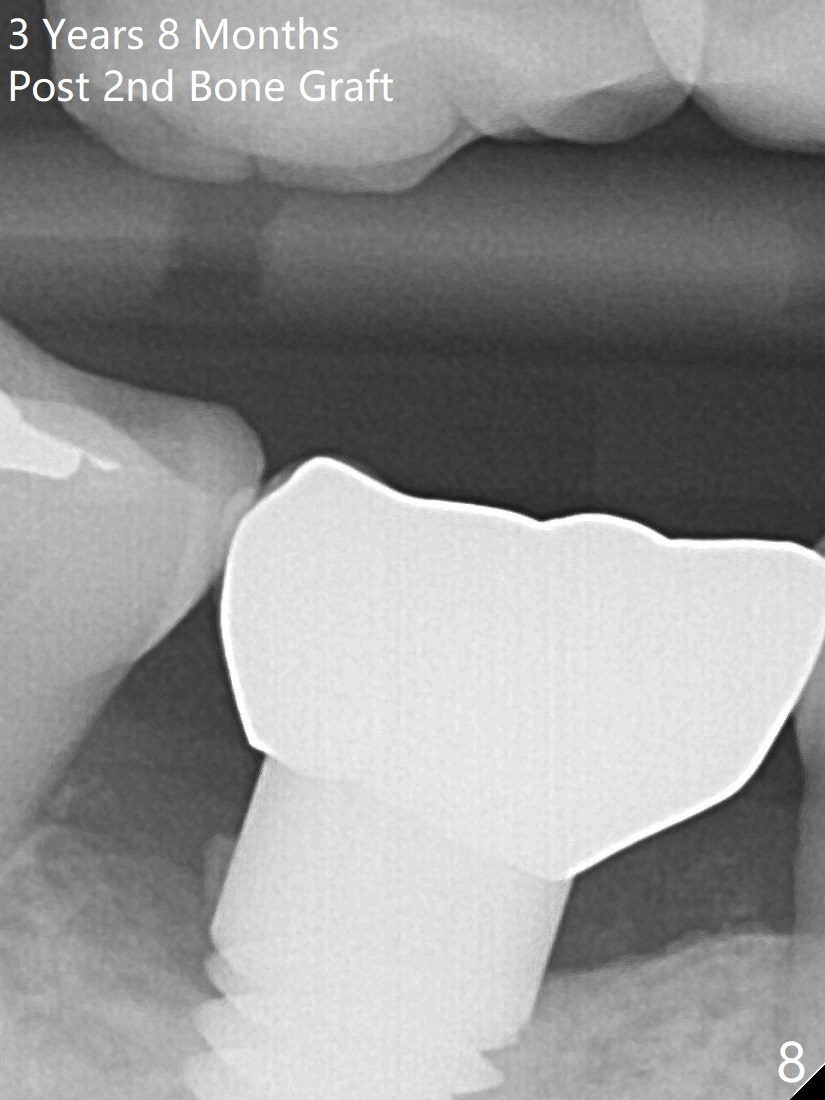
There is no symptom or sign of periimplantitis 3 years 8 months post 2nd bone graft (Fig.7-10). However, the patient complains of gingival hemorrhage 8 months later (Fig.11,12 (buccal), 13 (lingual view)). Water Pik is recommended.
Return to Bone Graft Lower Molar Immediate Implant 19 Xin Wei, DDS, PhD, MS 1st edition 11/01/2014, last revision 04/21/2019