




 |
 |
 |
 |
||
 |
 |
 |
 |
||
 |
 |
 |
 |
||
 |
 |
 |
 |
||
Can Immediate Implant be Placed Next to Infection?
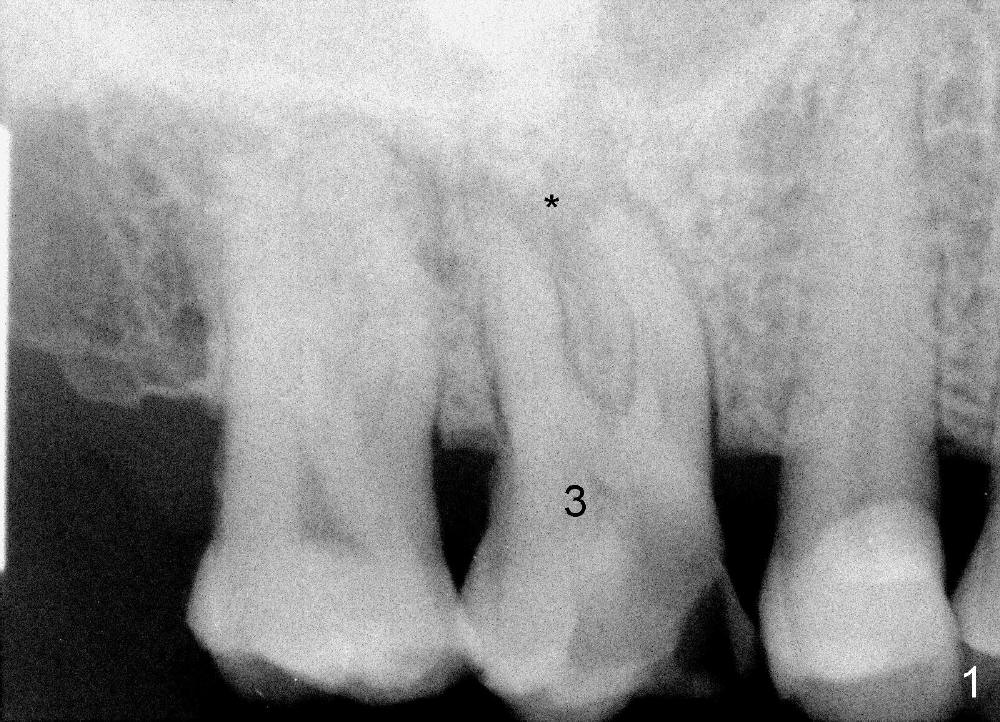
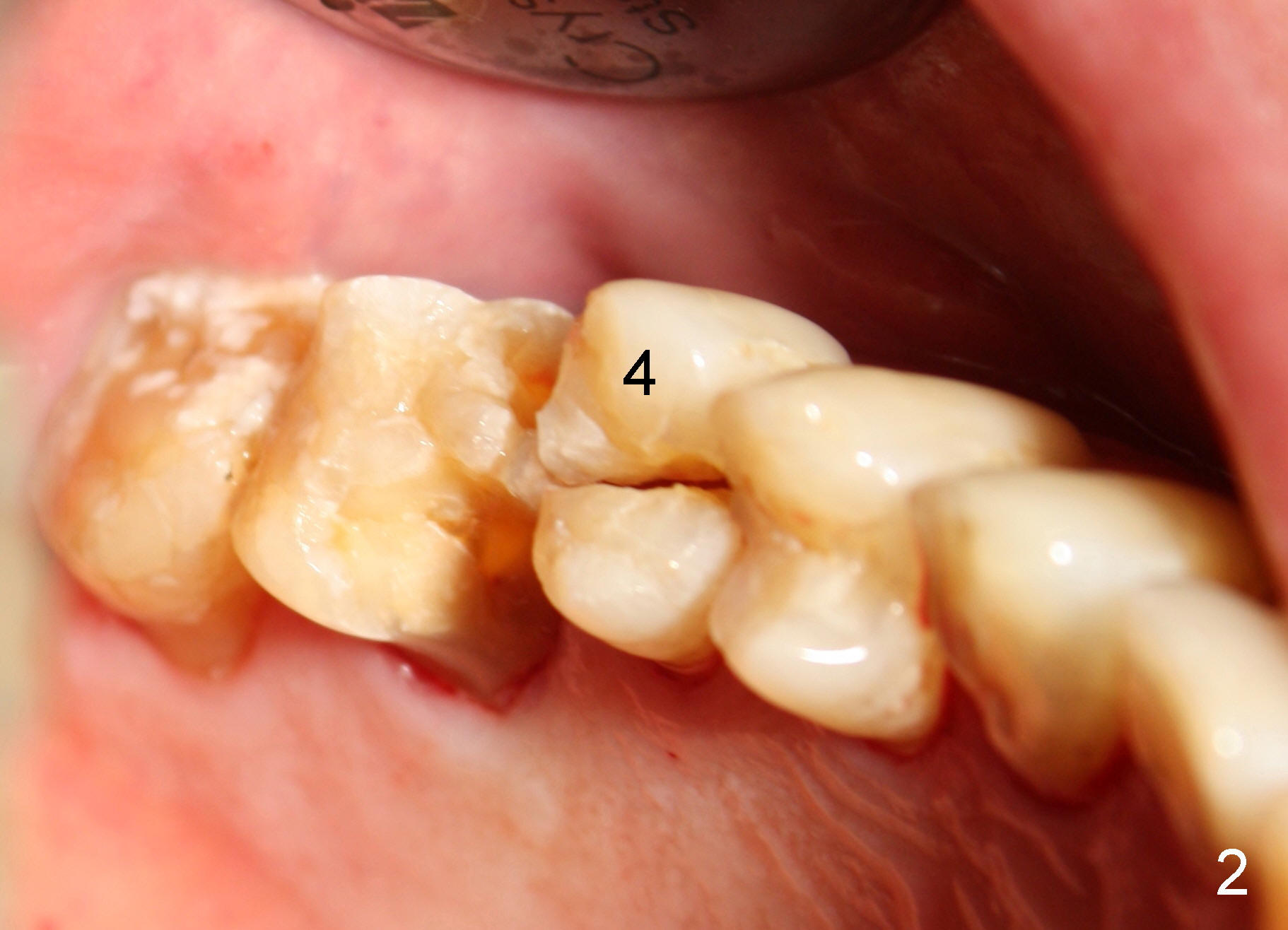
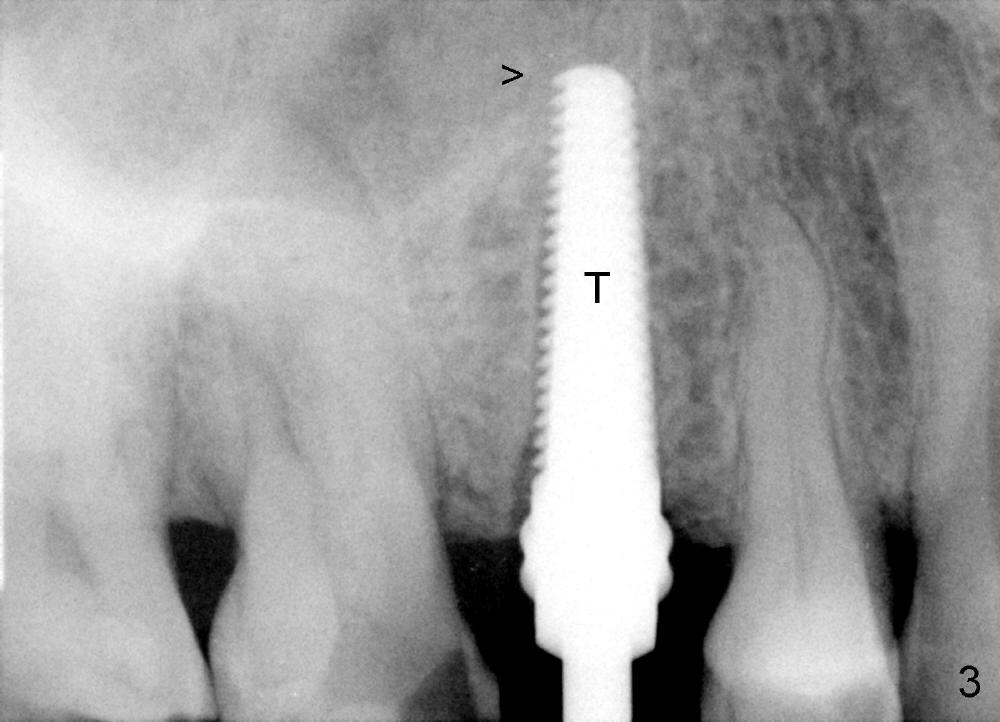
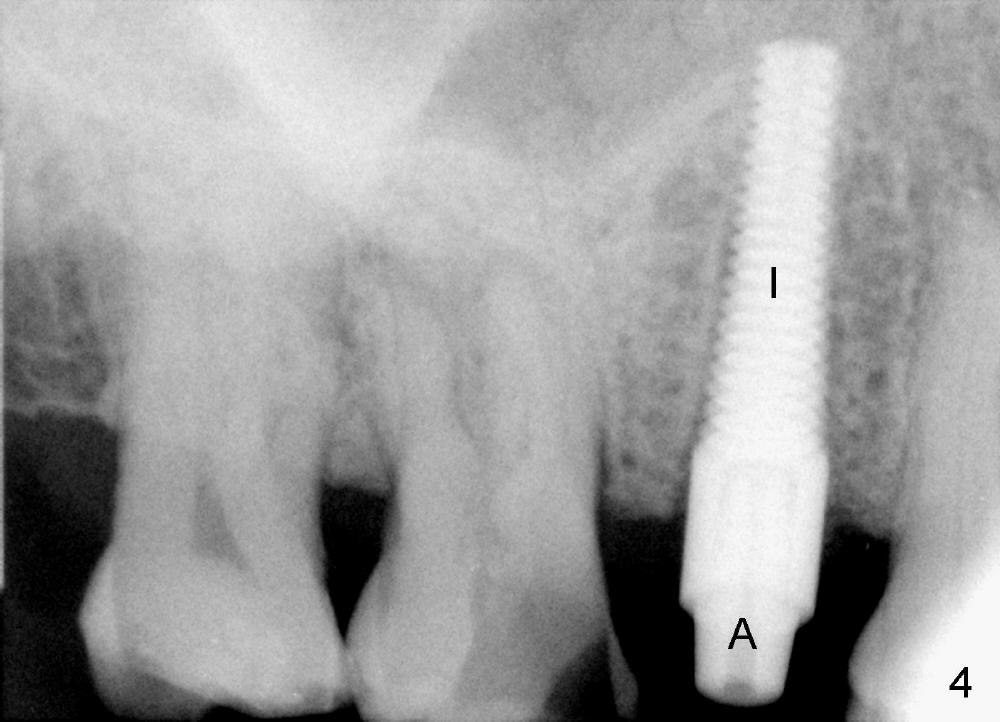
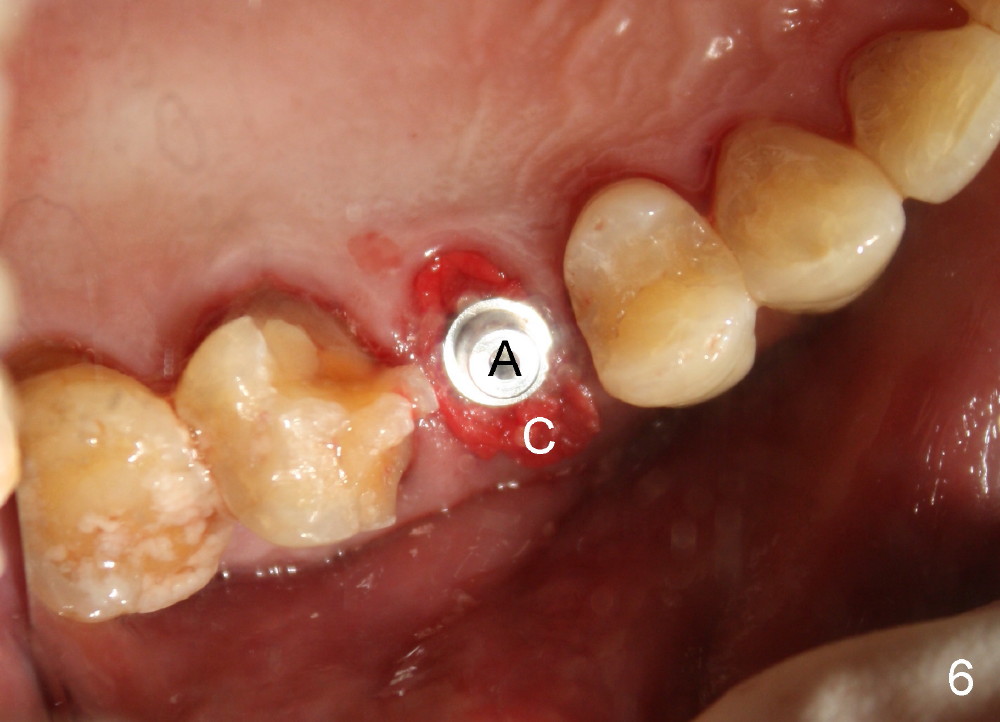
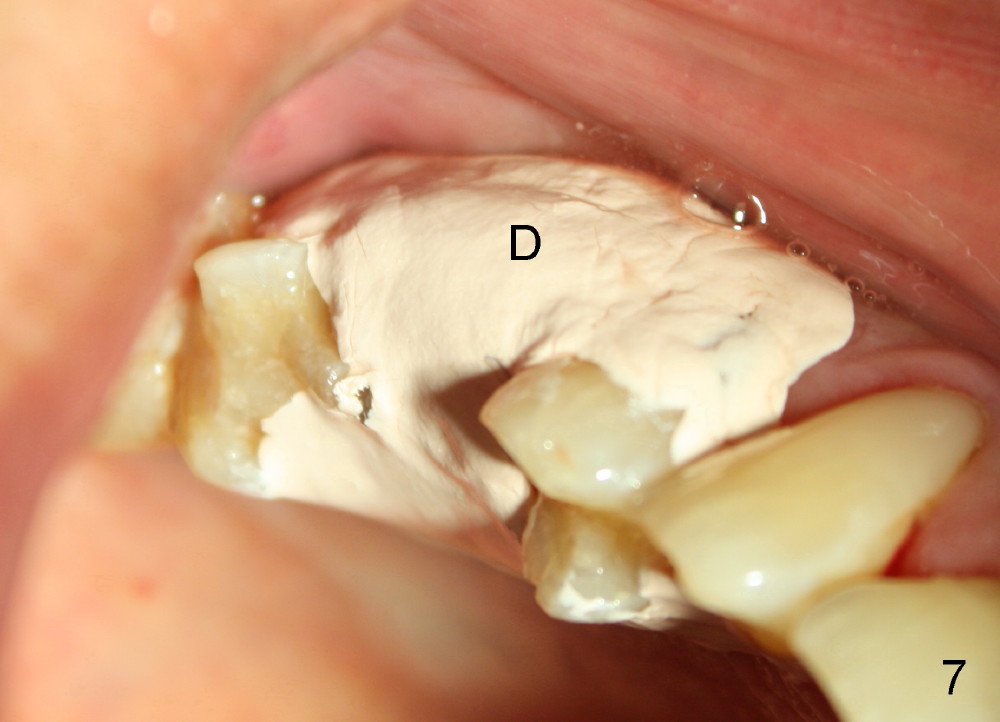
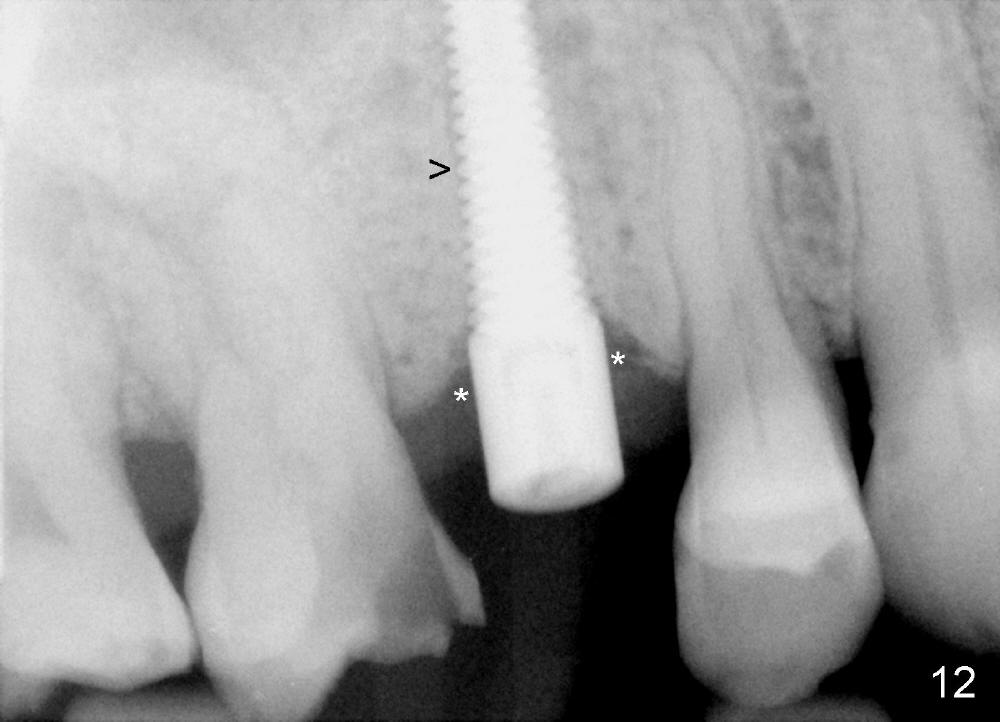
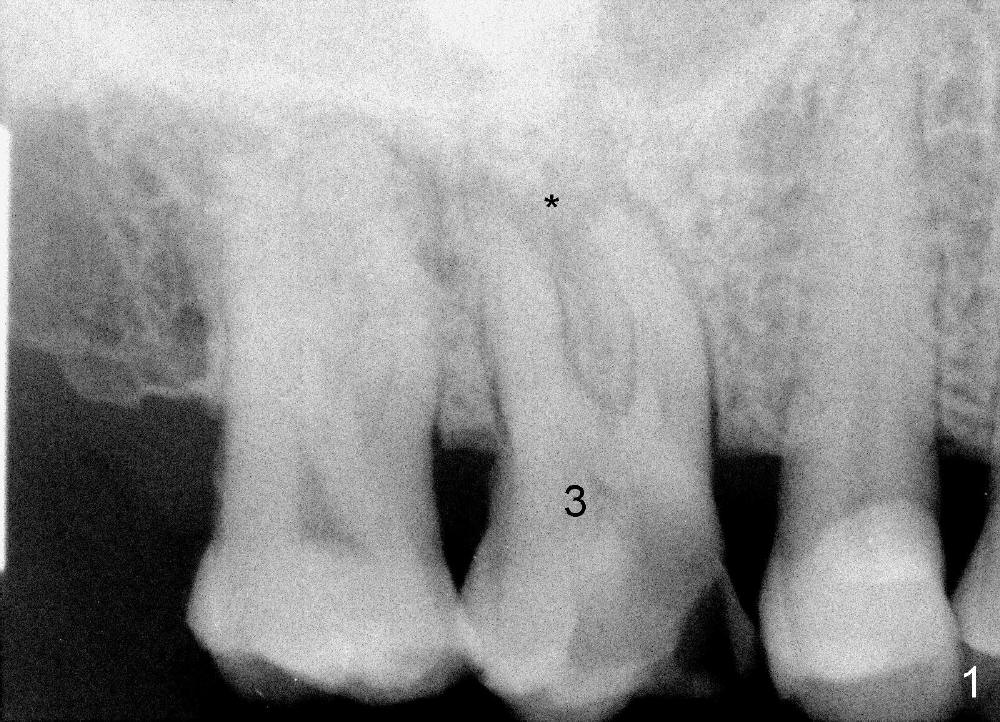
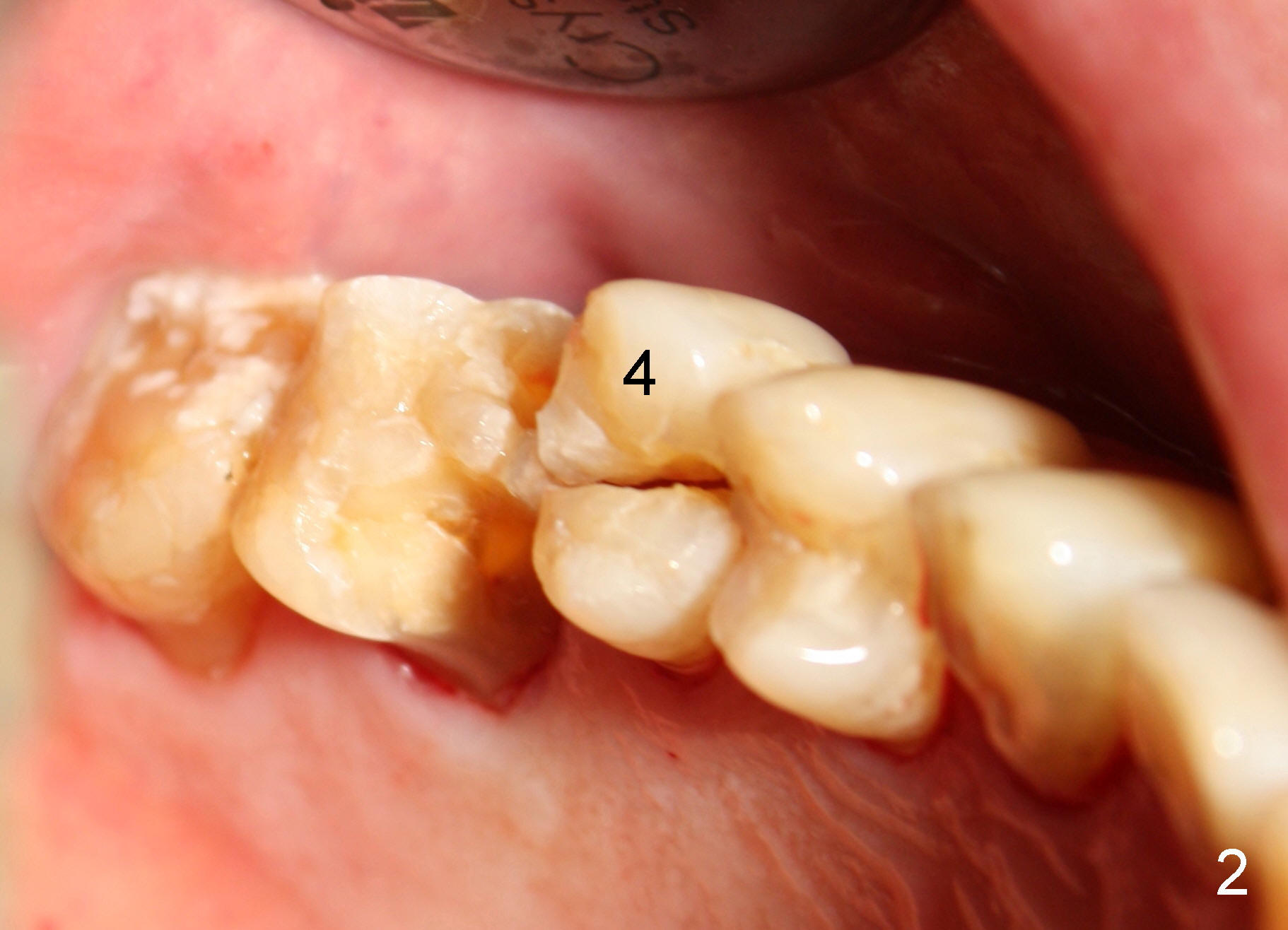
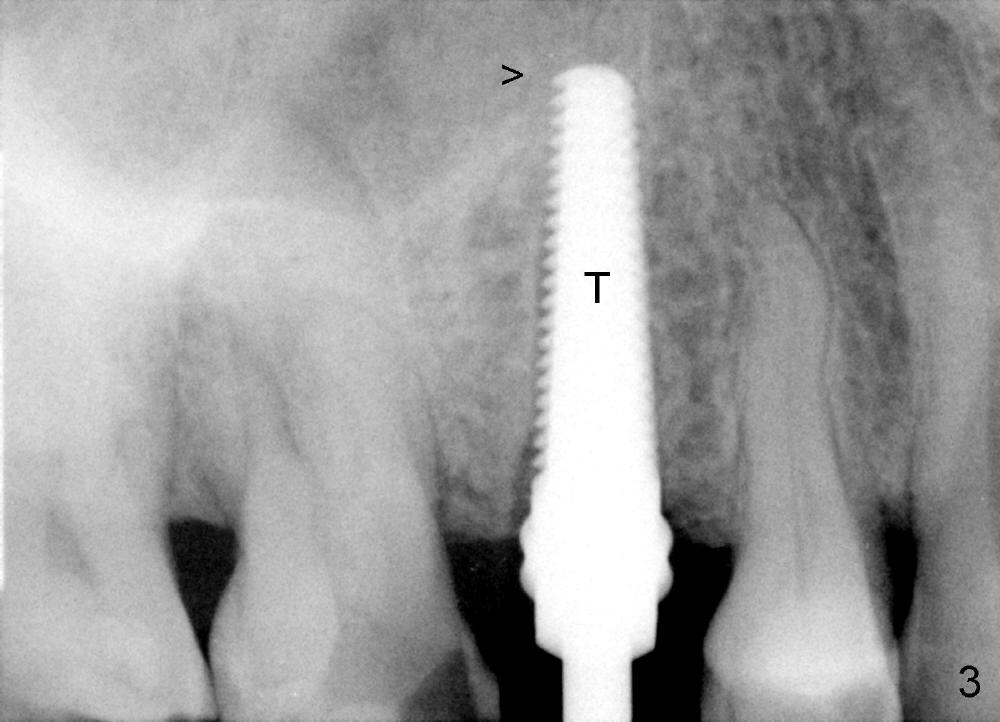
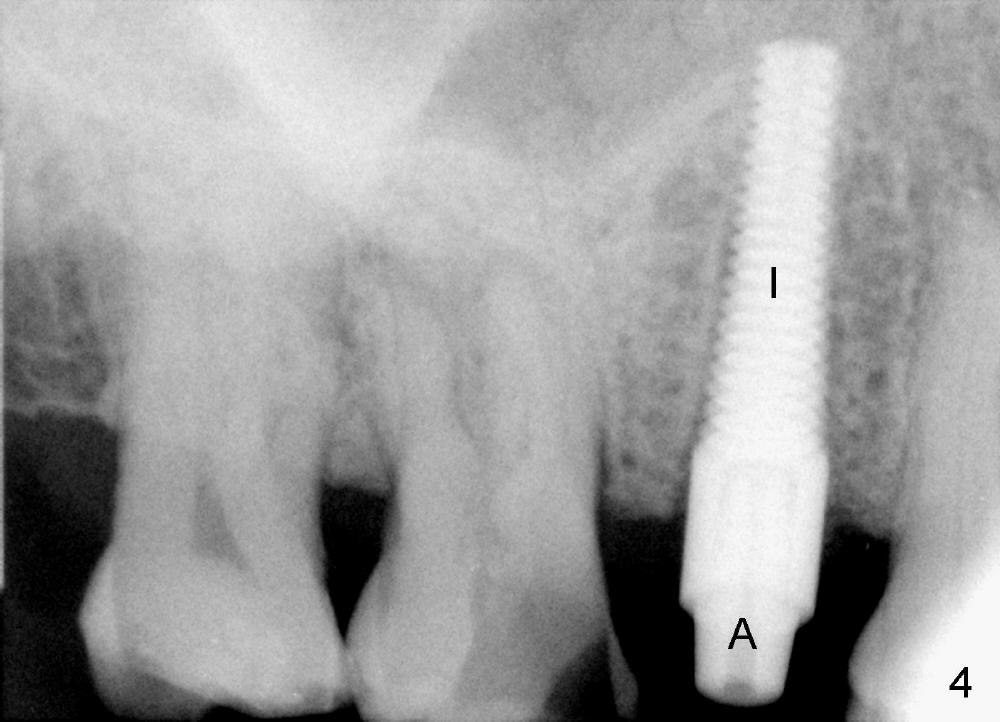
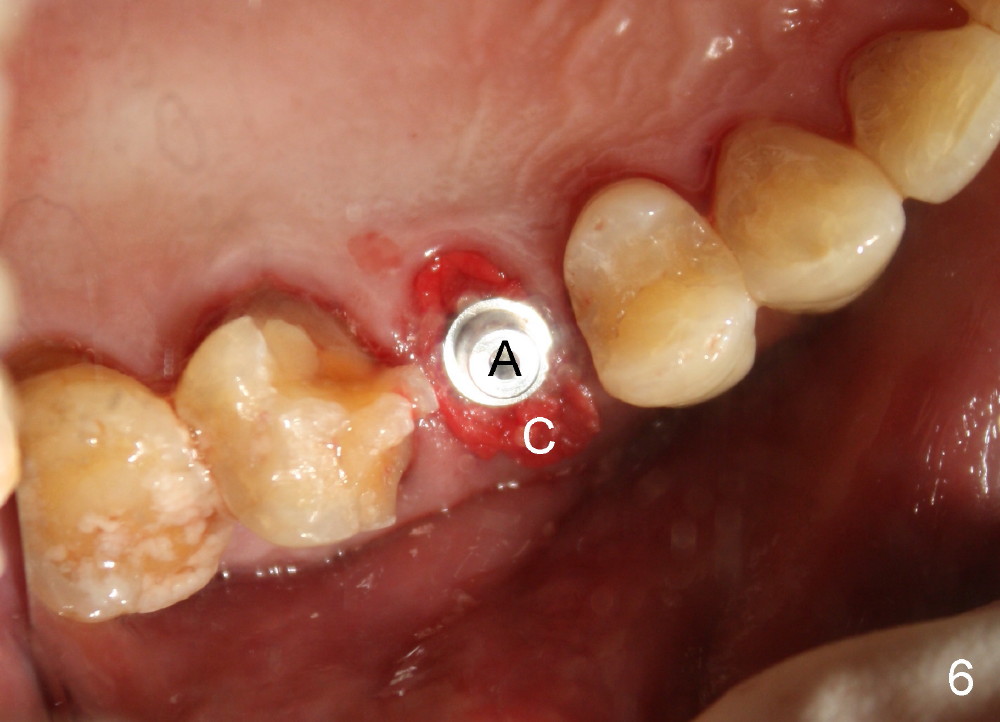
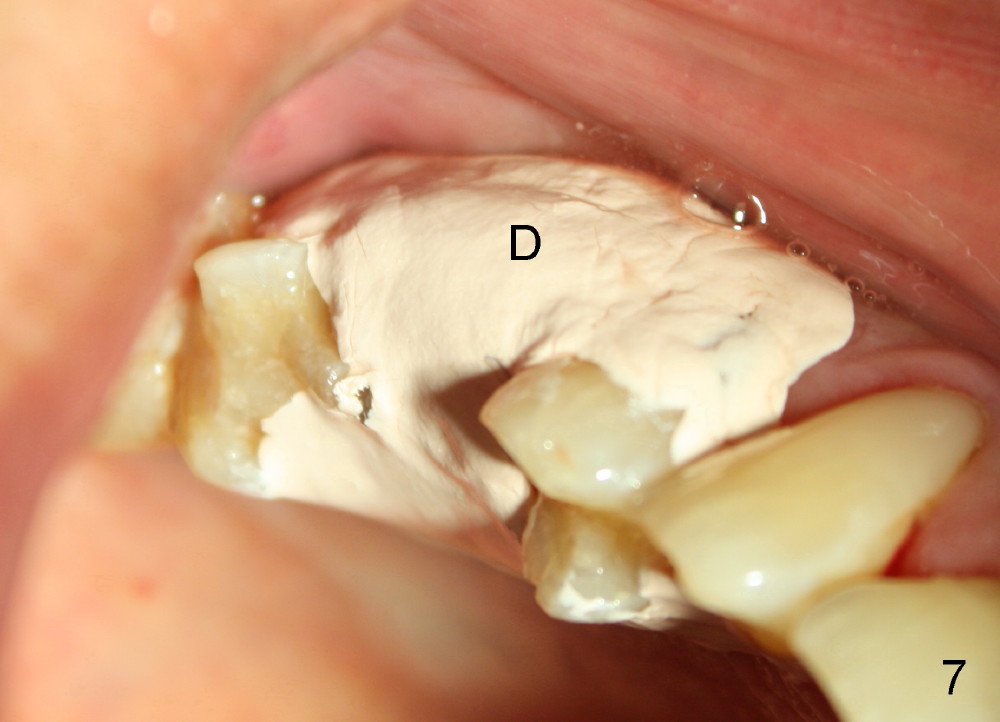
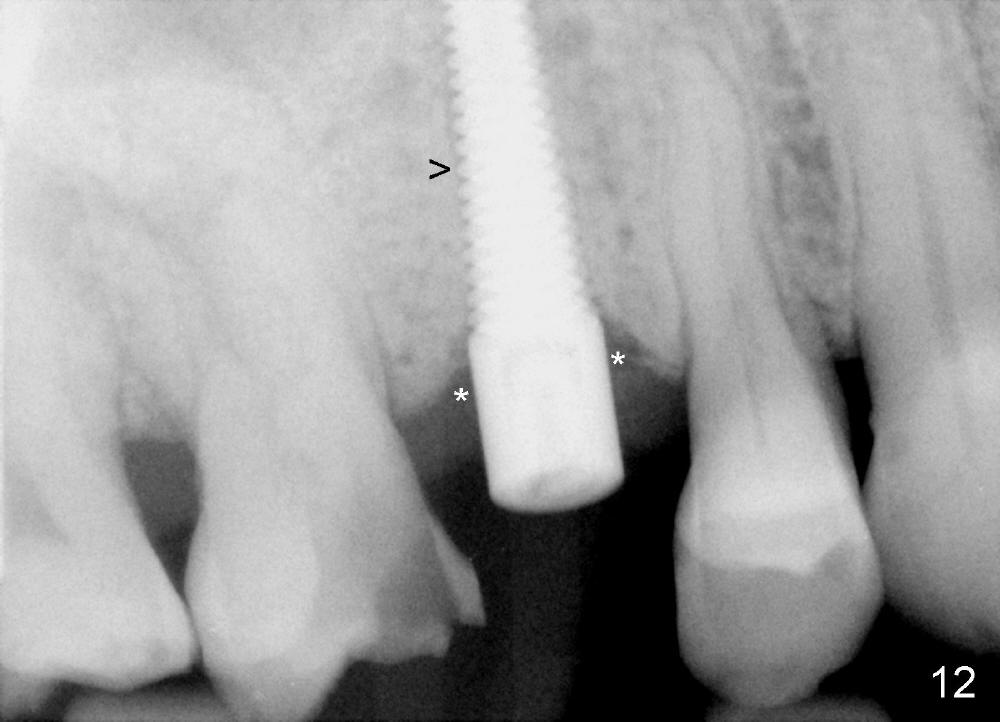
A 72-year-old man is a bruxer with #3 cusp fracture with chronic periapical radiolucency (Fig.1 *) and #4 acute crack. It appears reasonable to take care of emergency (#4 extraction and immediate implant (Fig.3-7: 4.5x20 mm, 45 Ncm)) followed by root canal therapy or extraction for #3. Eight (Fig.8) and 14 (Fig.9-11) days postop, the patient is doing fine and the wound heals normally. But he does not agree any treatment for #3, since it is asymptomatic in spite of a fistula associated with the tooth (Fig.8,9 >). Three months postop, the patient is still asymptomatic and is ready for #4 restoration since the tooth #28 cracks. Follow-up PA shows the persistent distal gap (Fig.12 >, as compared to Fig.4), accompanied with crestal bone resorption (*). Clinically the implant has mild mobility and light tenderness. The patient still refuses #3 treatment. It appears that the implant has failed to osteointegrate. In brief, do not place an immediate implant next to active infection.
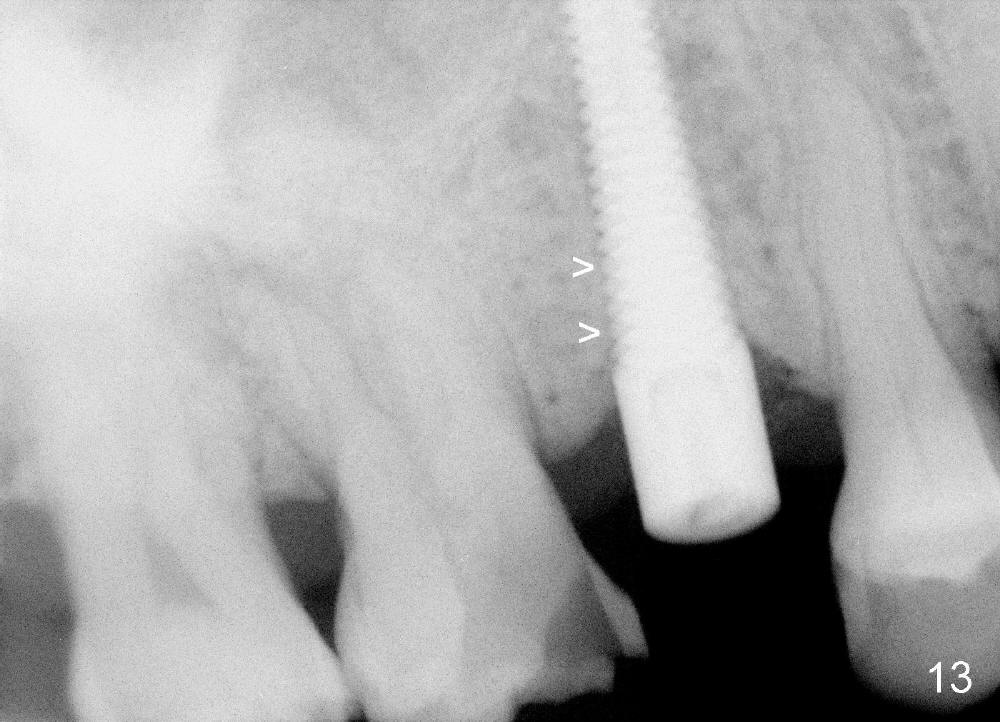
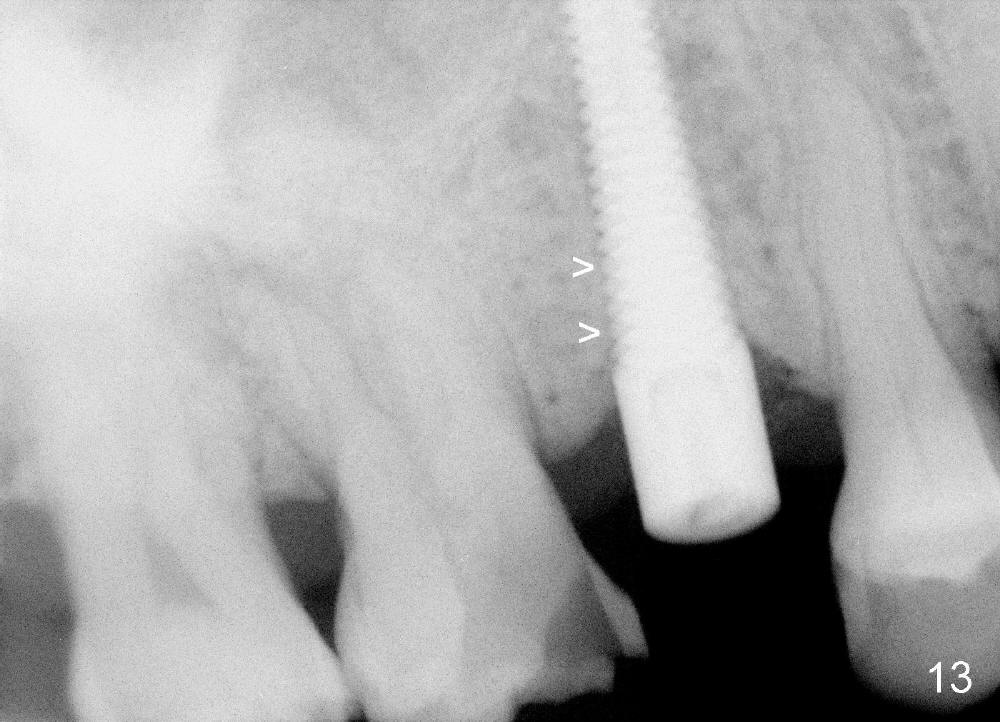
Five and a half months postop, the distal gap appears to have reduced (Fig.13 >). Clinically the implant is stable and is ready for restoration. It is advisor able to watch those asymptomatic immediate implants with minimal mobility. It takes time to osteointegrate the immediate implant considering the peri-implant space.
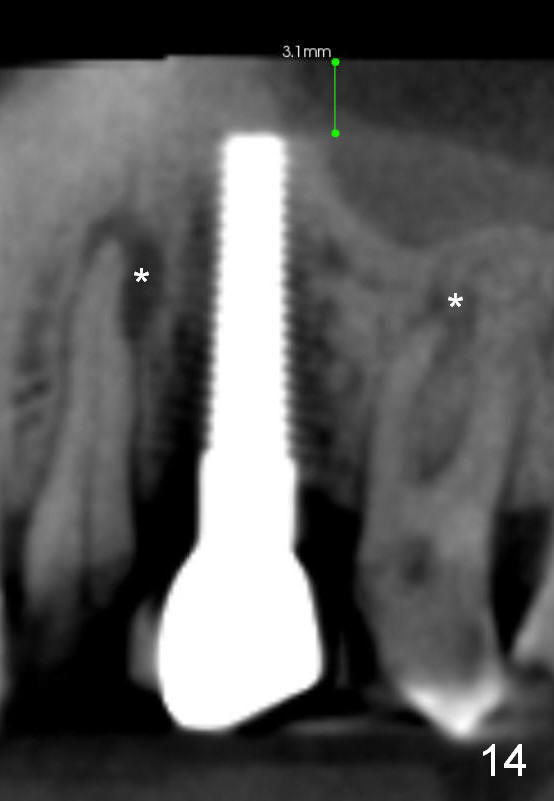
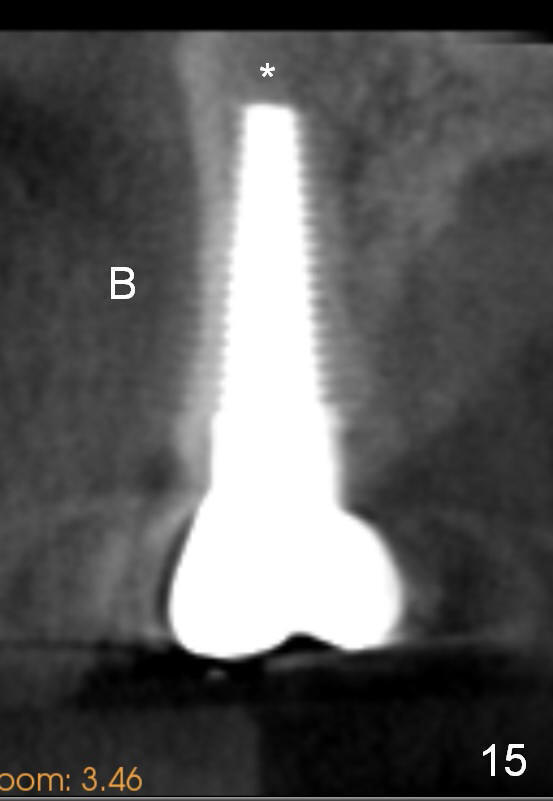
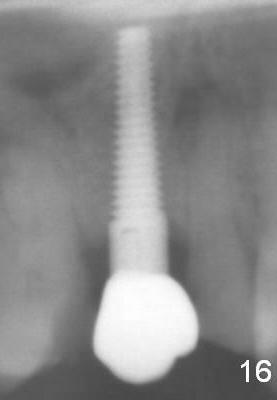
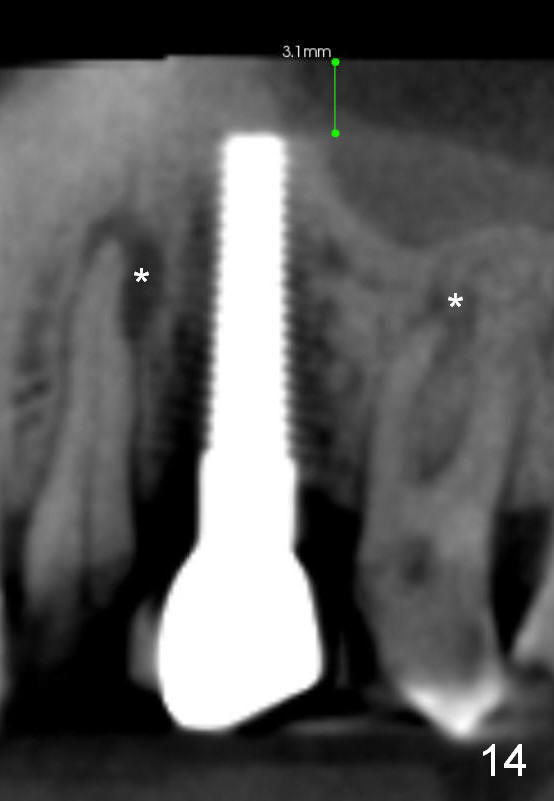
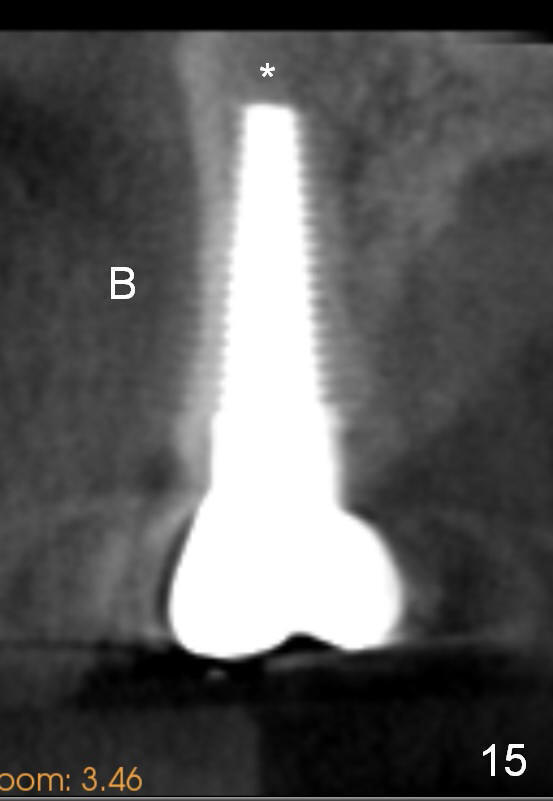
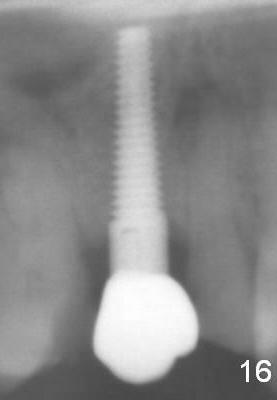
Eight months post cementation, CBCT shows periapical infection of the neighboring teeth (Fig.14 *). There is still apical bone for a longer implant (Fig.14 green line, Fig.15 *). The implant functions 1.5 years post cementation. When the implant at the lower bicuspid fails, the patient reveals that he is a diabetic. The latter is the main reason of delayed healing.
Return to Upper Bicuspid Immediate Implant
Next to Infection
Immediate
Implant Complications,
13,
28,
21
Xin Wei, DDS, PhD, MS 1st edition 10/28/2014, last revision 08/06/2018