







 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
+ |
How to Cover the Defect?
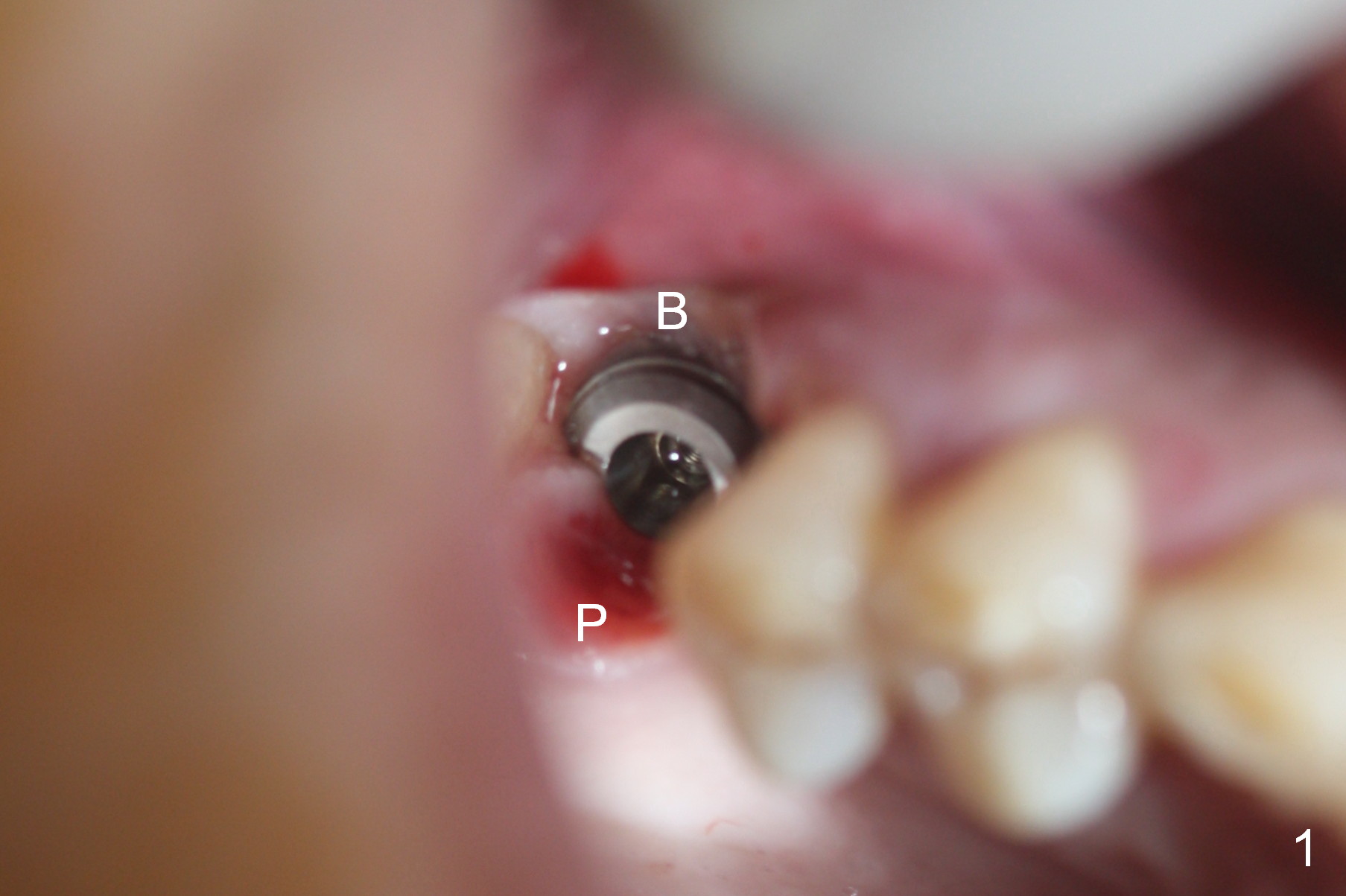
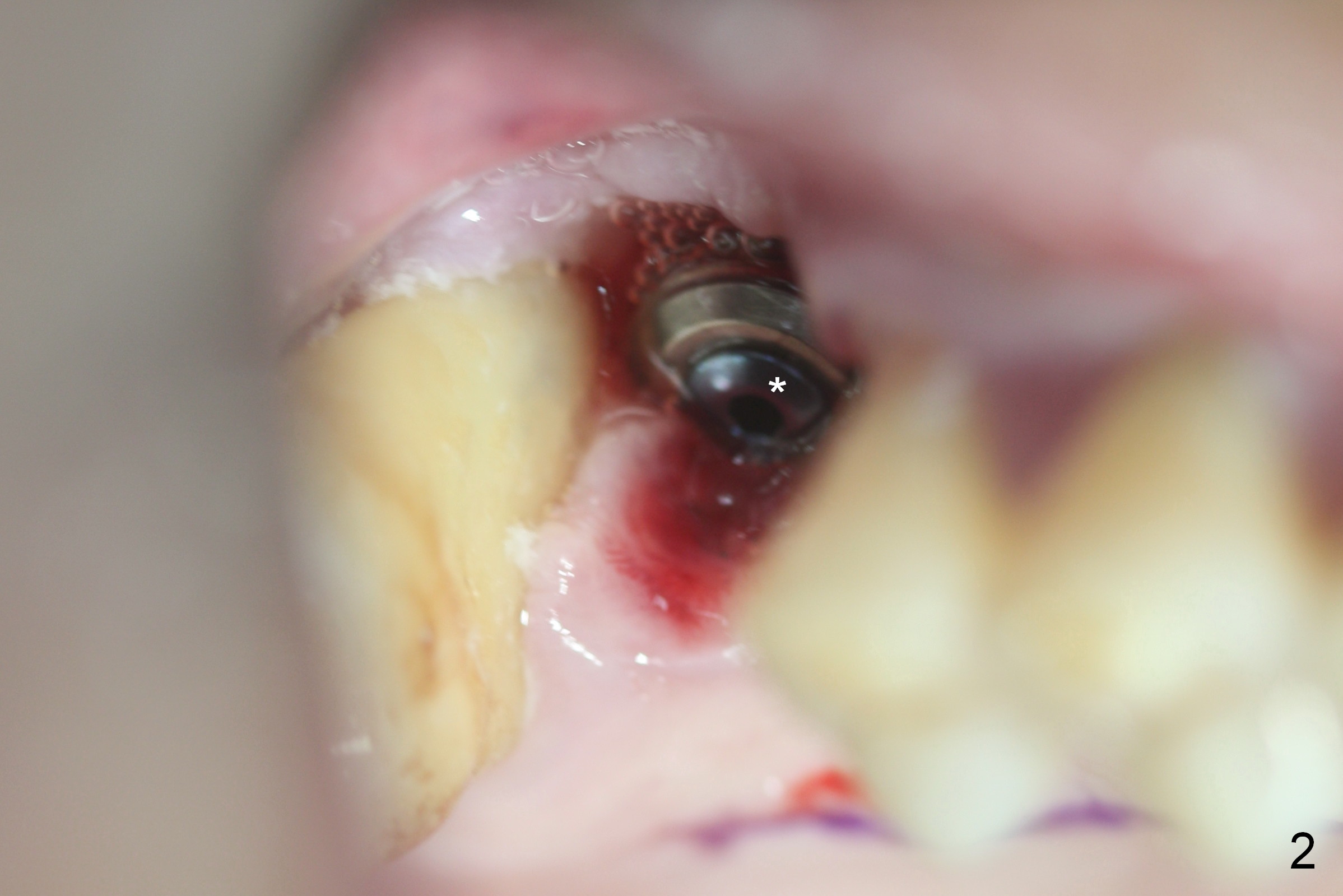
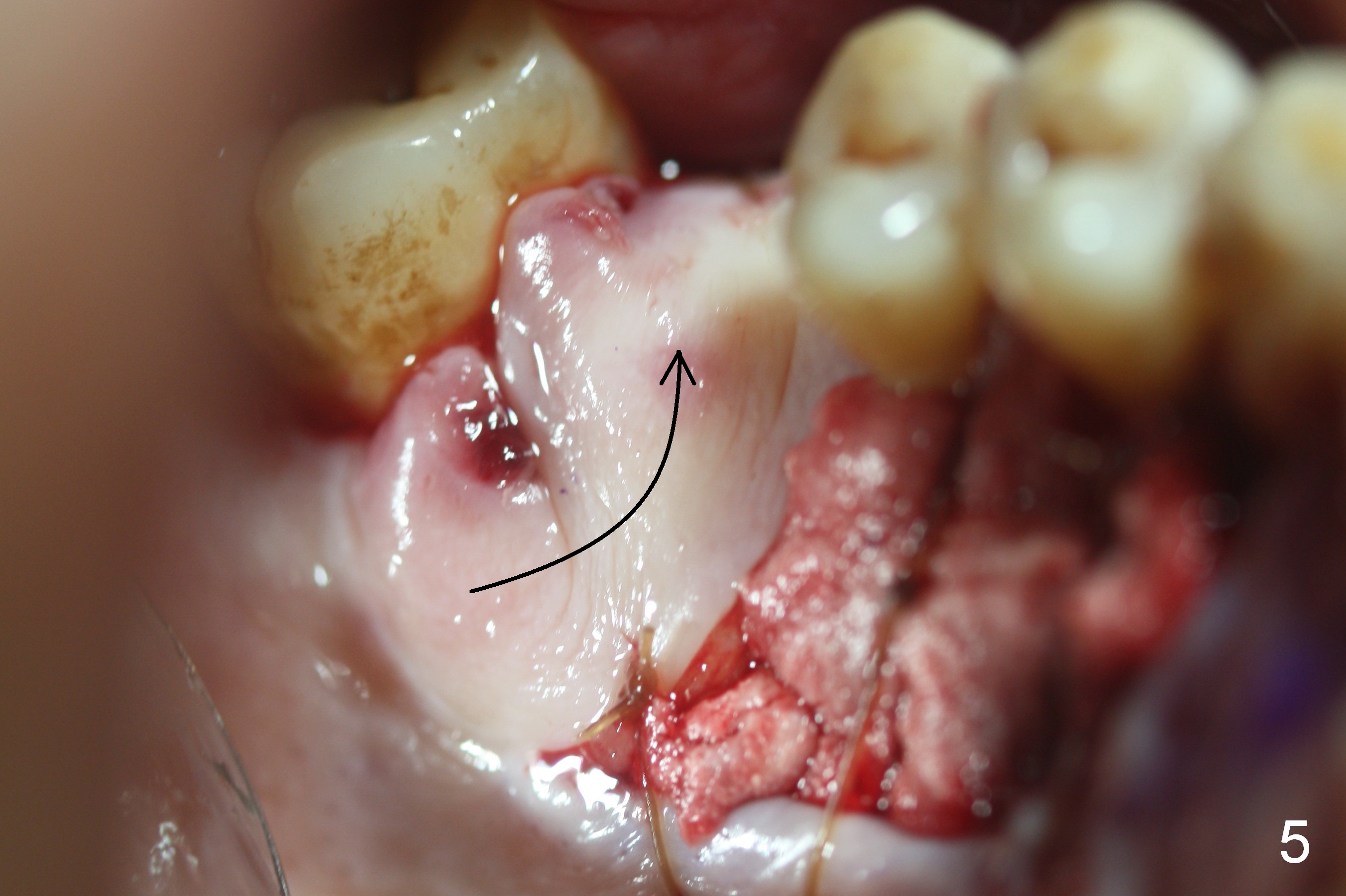
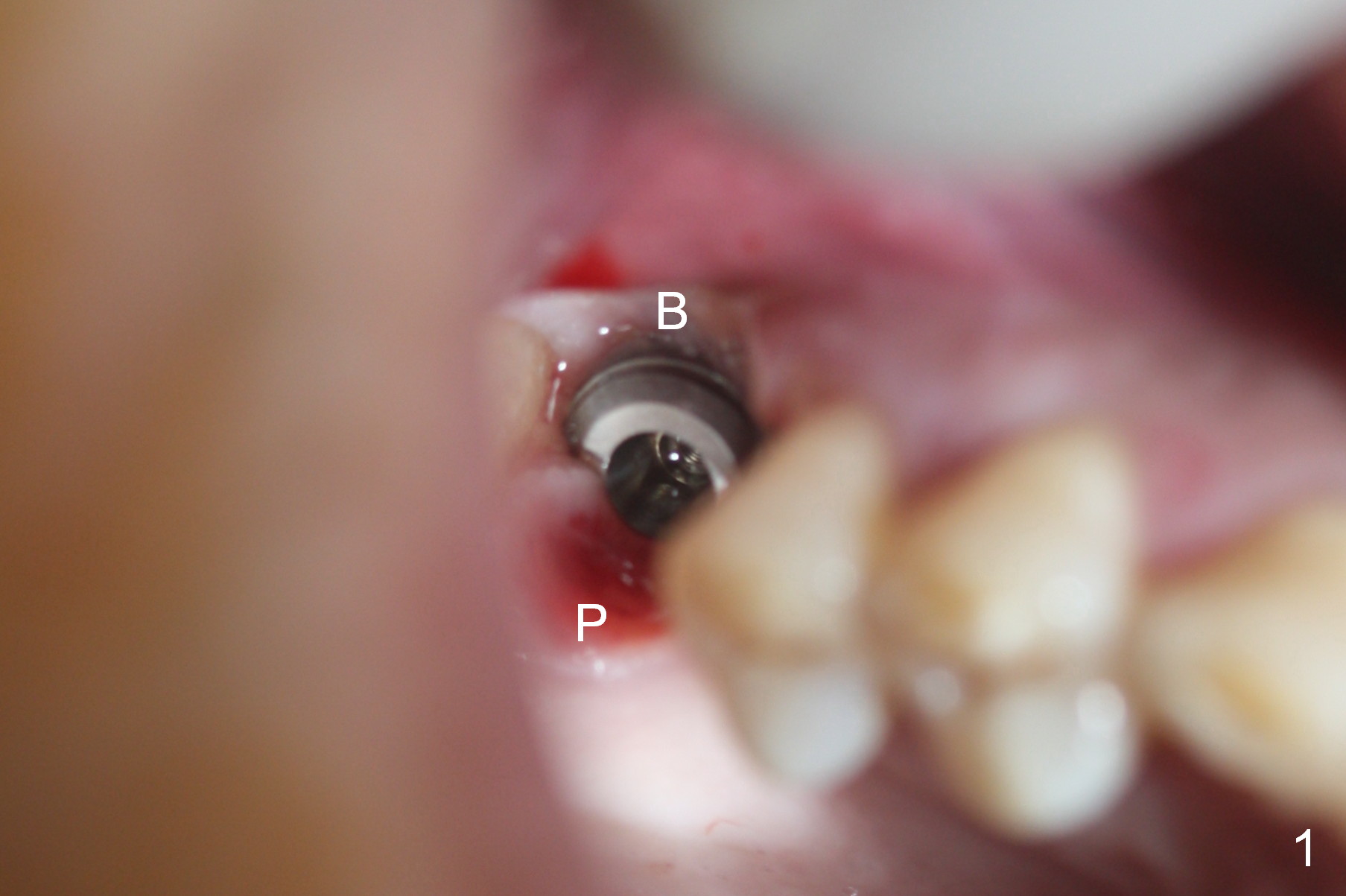
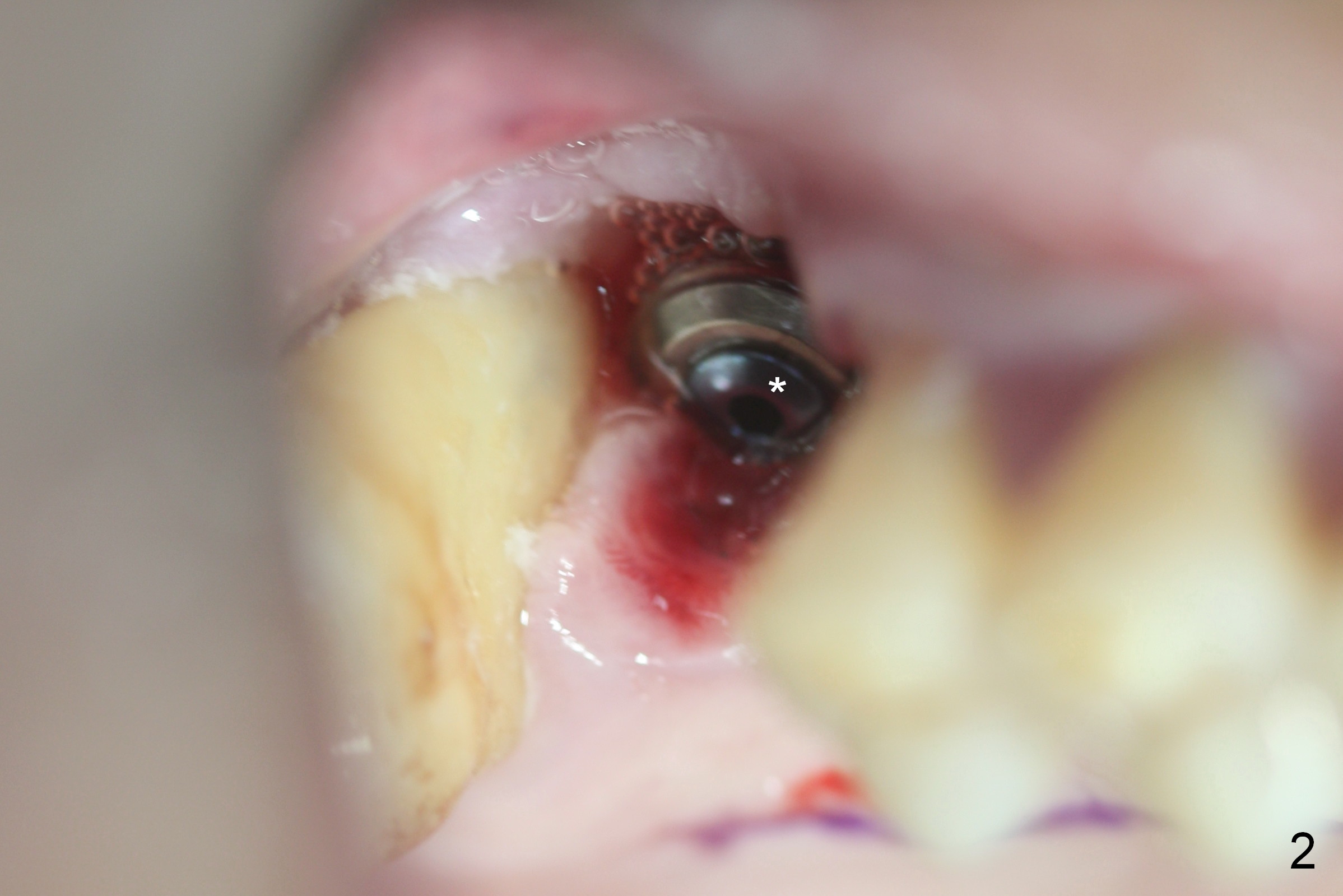
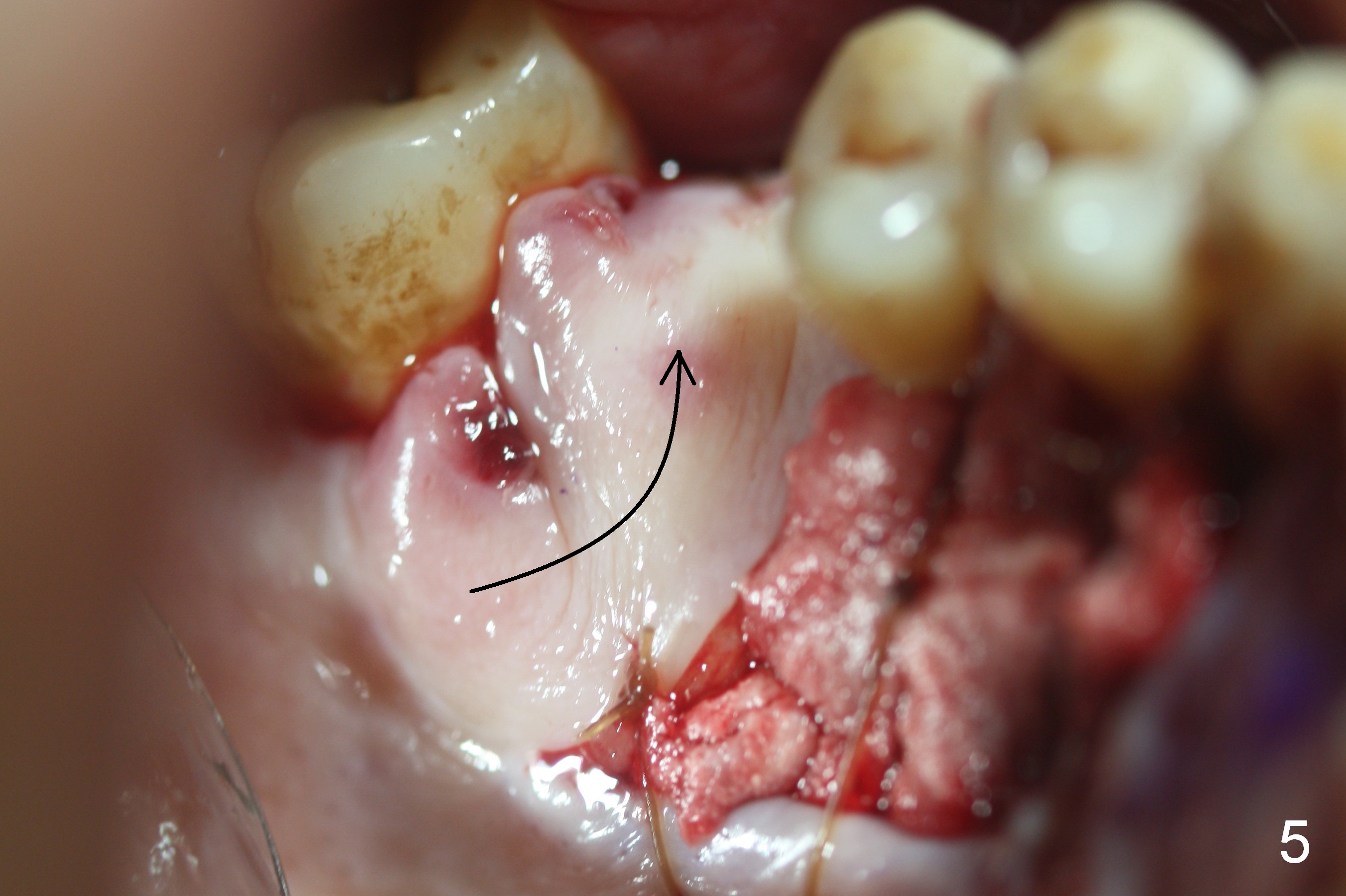
Seven months post placement, the implant crown and abutment are removed. The implant is osteointegrated (i.e., cannot be removed). The buccal (B in Fig.1) gingiva is thin and low, whereas the palatal (P) one is thick and tall. After a cover screw is placed (Fig2 *) as well as allograft, a pedicled palatal flap is designed (Fig.3) and rotated (Fig.5) to cover the buccal defect. The donor site is covered with collagen plug (Fig.4 C). There is excess tissue at the tip of the flap (Fig.6,7). In fact the flap should have been shorter and narrower (to reduce gingival recession and sensitivity, Fig.8).
The 2nd drawback of this surgery is lack of bone graft buccal to the implant. When the flap heals, consider bone grafting before uncover.
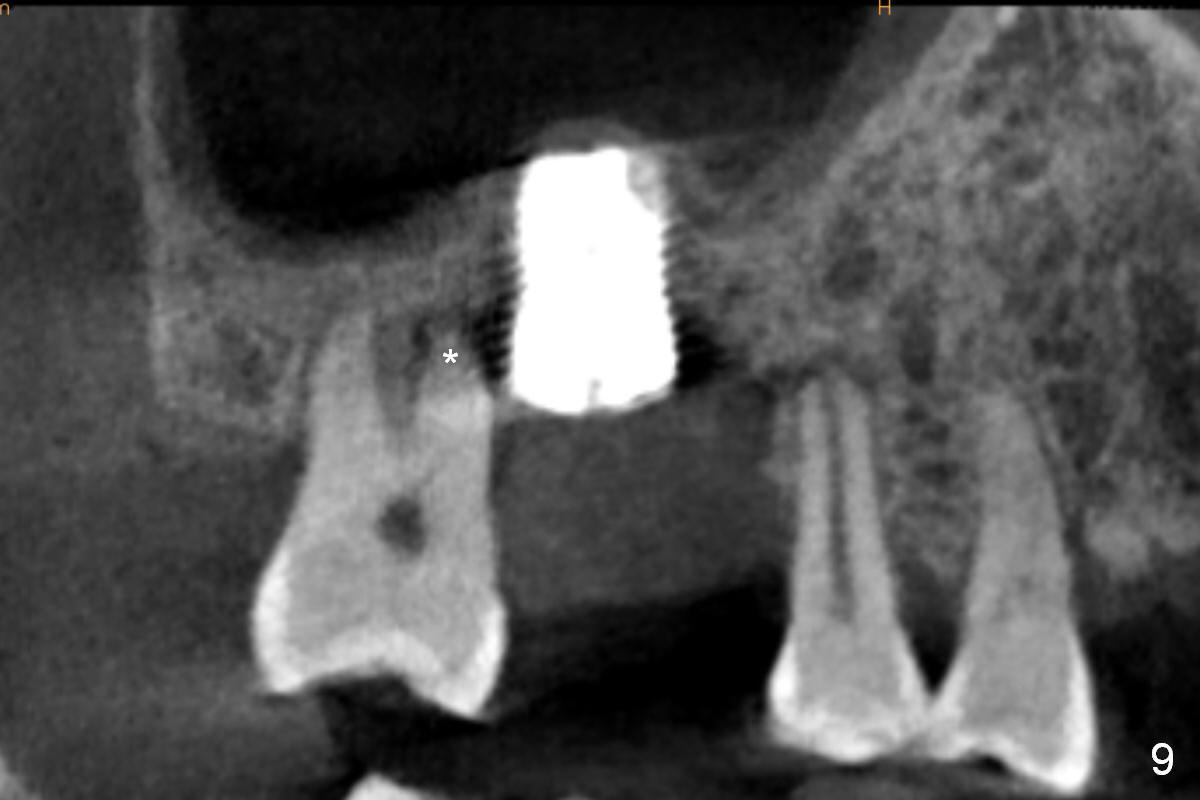
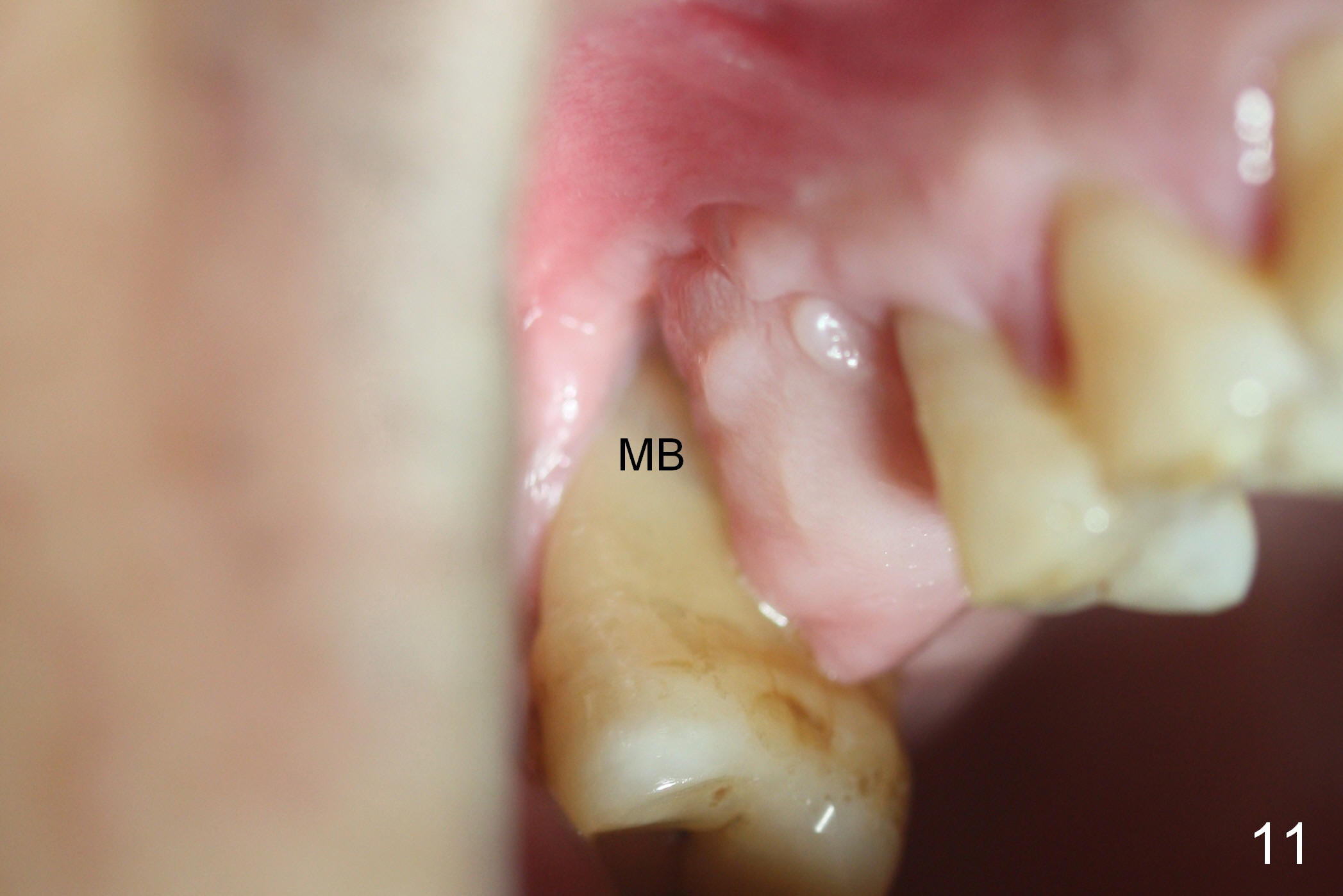
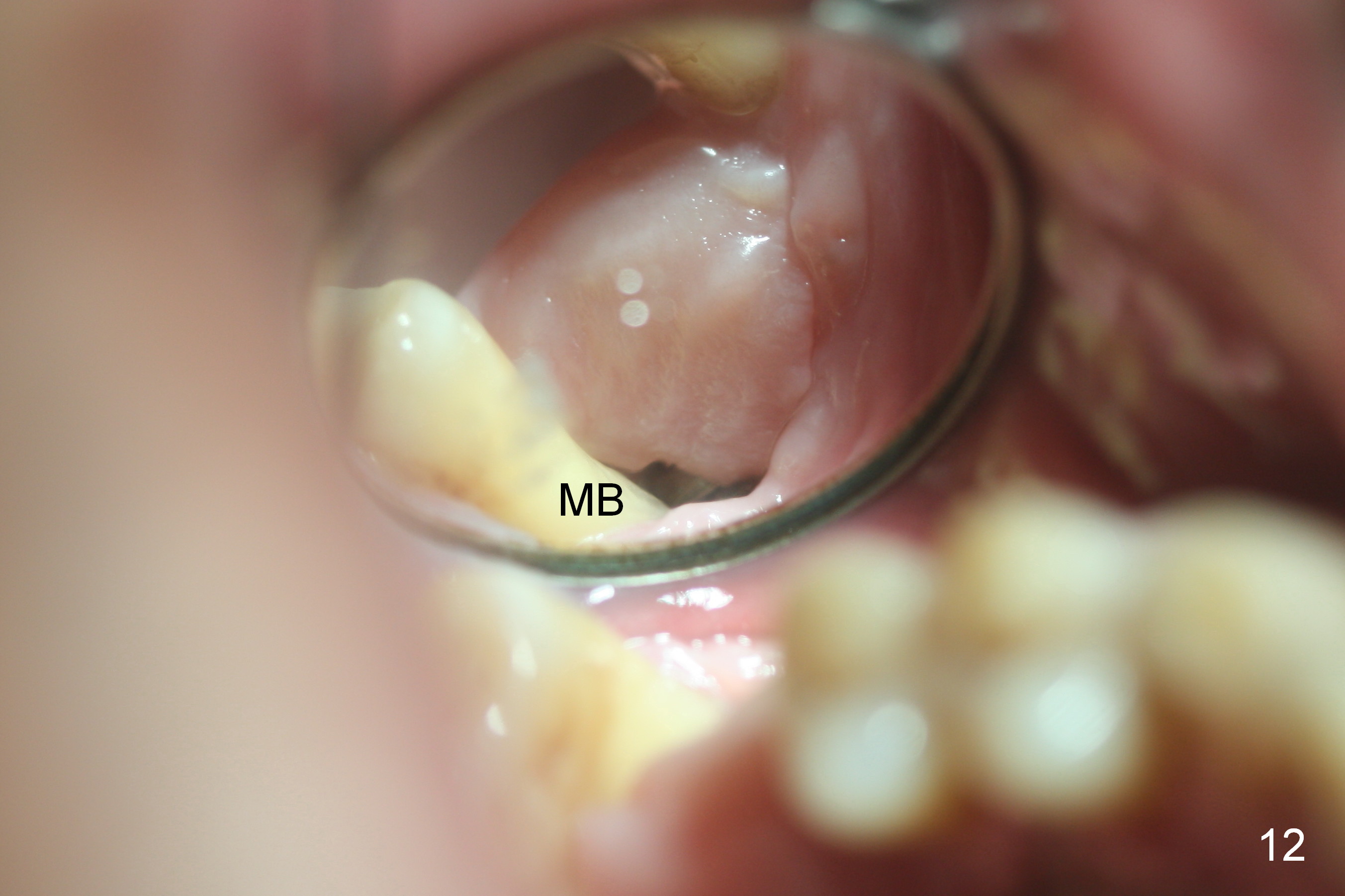
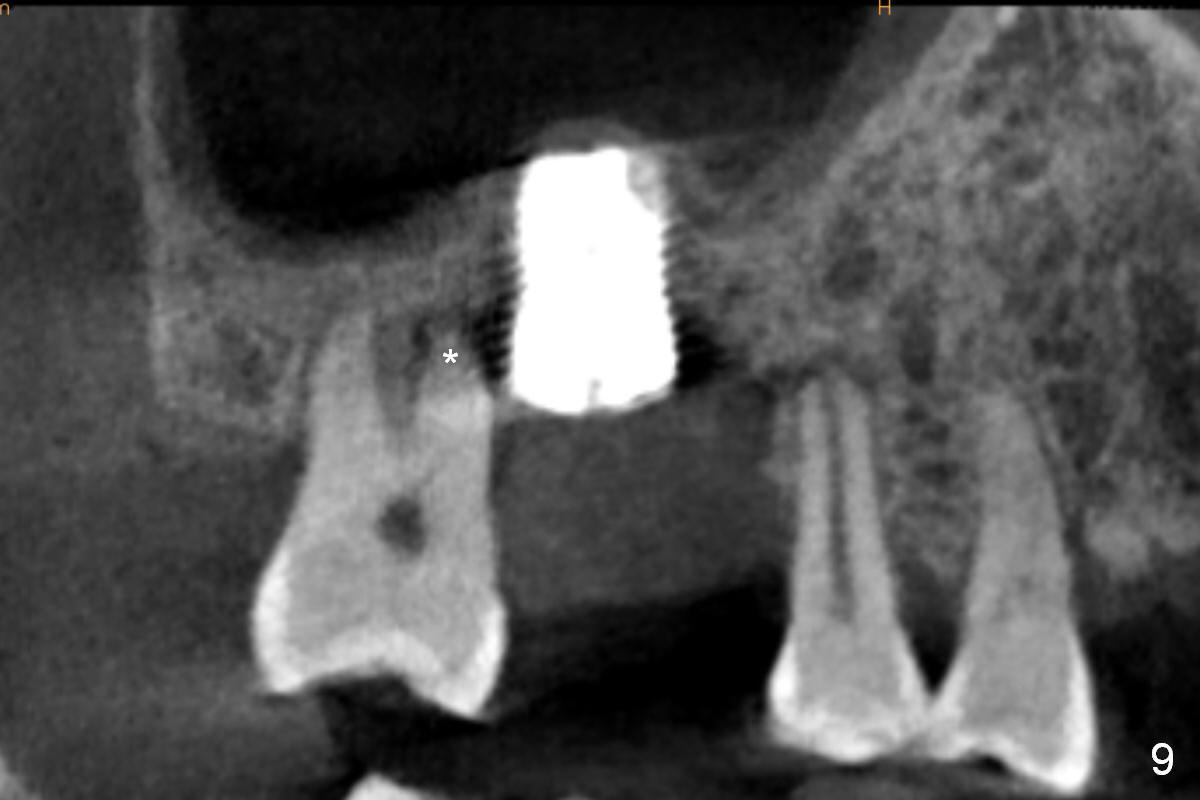
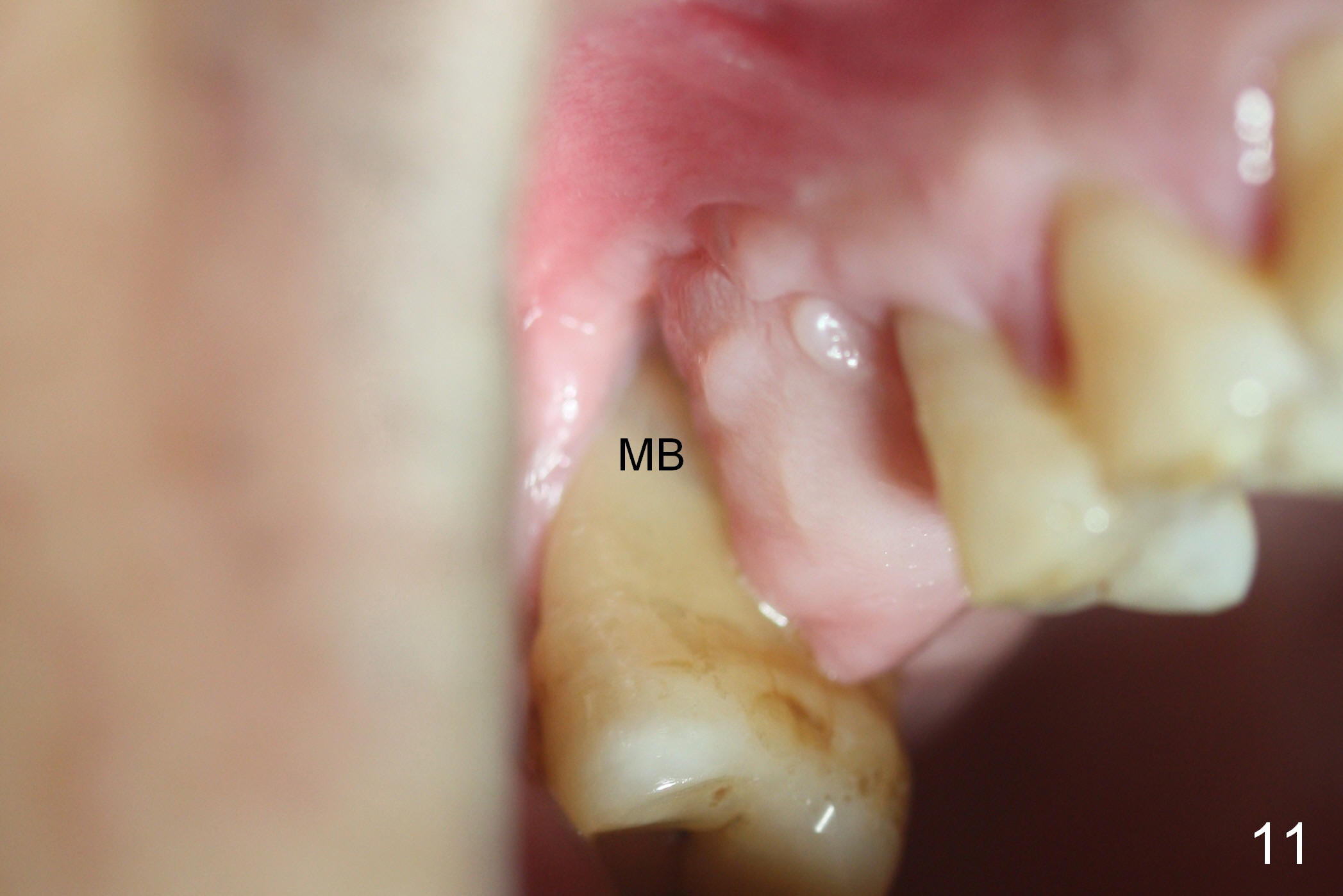
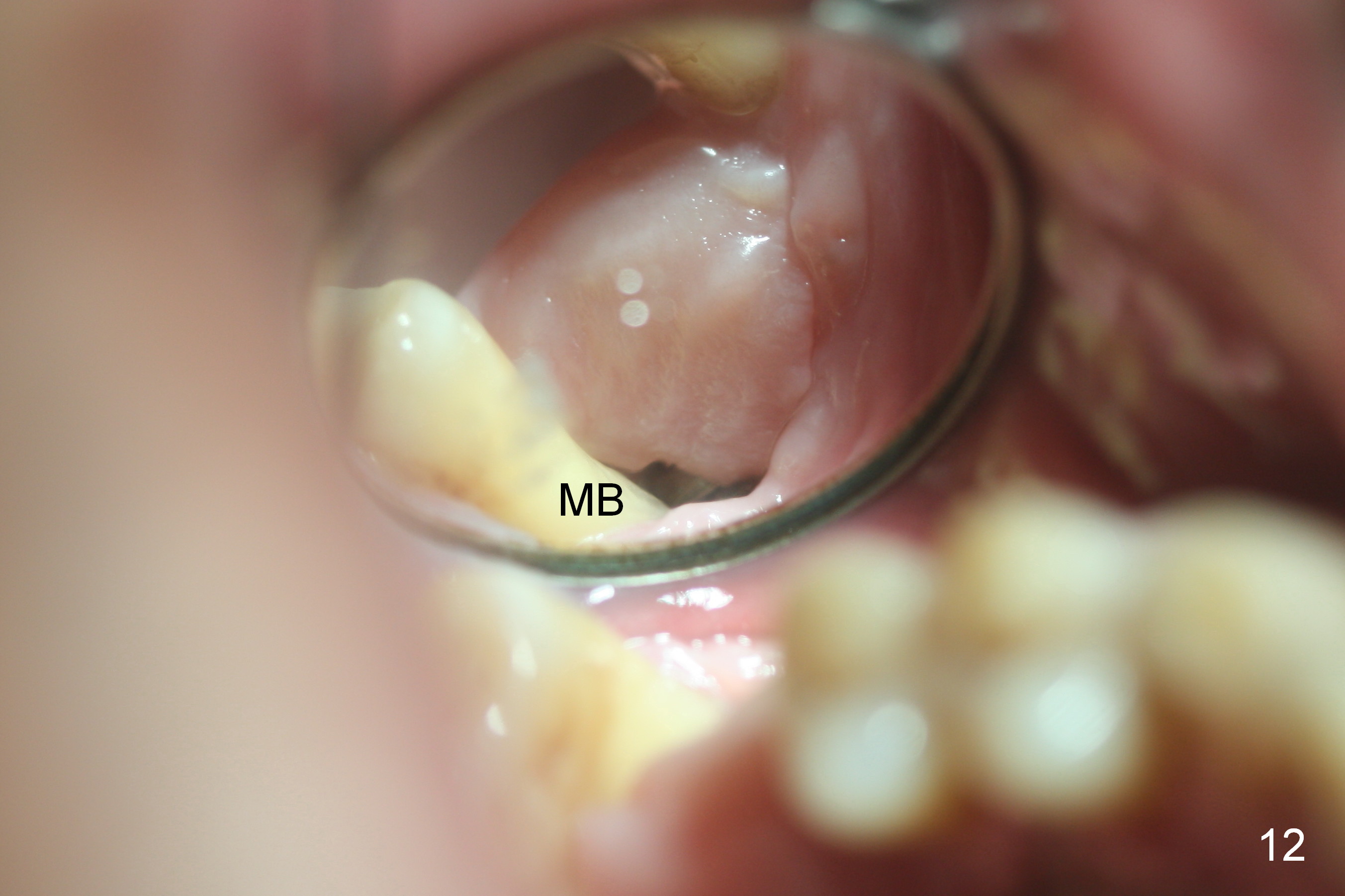
In fact the flap does not heal well next to the mesiobuccal root of the tooth #2 (Fig.11,12, 25 days postop). Postop CT shows that there is radiolucency around the mesiobuccal apex of the tooth #2 (Fig.9 *). The bone appears to have superficial necrosis in the anterior portion of the donor site (Fig.10 *). The base of the flap looks normal (Fig.13).
PRF will be placed over the exposed palatal bone after debridement (surgical handpiece). The membrane will be fixed in place with suture and a new palatal stent. It is the best to extract the tooth #2, followed by bone graft and collagen plug.
On 03/31/2016 PRF, allograft/Osteogen and collagen plug are placed in the distal portion of the recipient site. It appears that the wound is re-gapping 14 days later. The patient finally agrees to have #2 extracted. In addition to the materials mentioned above, bone may be harvested in the tuberosity and #2 socket (also reduce socket size) and placed around the implant. The procedure is similar to socket preservation. Take photos of the donor site of the palatal flap, which is healing.
On 04/28/2016, the tooth #2 is extracted, the buccal flap is raised and granulation tissue is removed from the mesiobuccal (Fig.14 MB) and palatal (P) sockets. The buccal and palatal edges of the extraction socket are wide (arrowheads). They are removed to reduce tension of socket closure and used to cover the exposed implant surface. The buccal envelop incision is extended mesially involving 2 papillae (*). The buccal flap is raised as superiorly as possible with the periosteoum underscored. On the top of the bone graft are PRF membrane, 6-month membrane and collagen plug. The socket and transferred palatal flap are not completely closed.
In fact the implant remains exposed 5-6 weeks postop. The bone graft has dislodged. PRF will be prepared to cover the wound and facilitate soft tissue healing.
When the palatal (Fig.15 P) and buccal flaps are fully raised, approximately 3 mm coronal implant is not covered by the bone circumferentially. It appears better to remove the implant. After removing bone around the implant for 2 mm in depth, a small elevator is used to loosen the implant. When the implant is removed, the sinus membrane is immediately above the site without tear. A piece of PRF membrane is laid against the sinus membrane prior to bone graft placement. On the top of the graft are placed 3 layers of PRF membranes. The buccal and palatal flaps are approximated as much as possible with 4-0 Chromic gut suture with insertion of collagen membrane in the remaining gap. A palatal stent is advised to wear. Smoke cessation is recommended. Finally the tooth #2 and the implant at #3 are removed for infection resolution. An implant will be placed at #3.
Return to Upper Molar Immediate Implant
Xin Wei, DDS, PhD, MS 1st edition 03/03/2016, last revision 04/09/2017