







.jpg)
 |
 |
 |
||
 |
 |
 |
||
 |
 |
 |
 |
|
 |
 |
 |
 |
|
 |
 |
 |
 |
.jpg) |
Prevents Getting Worse
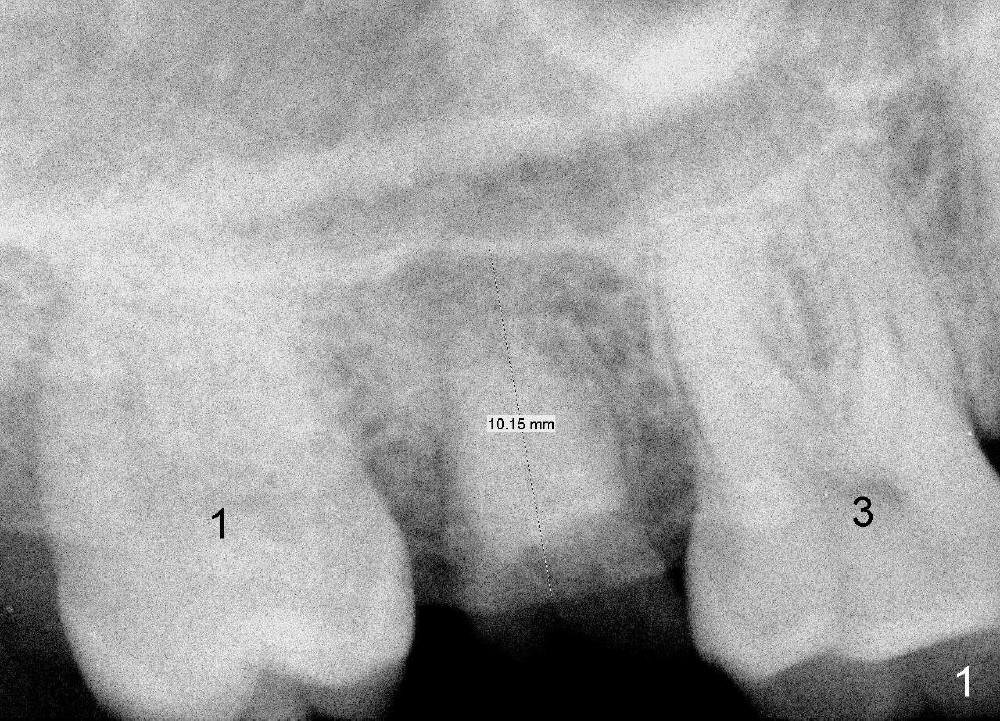
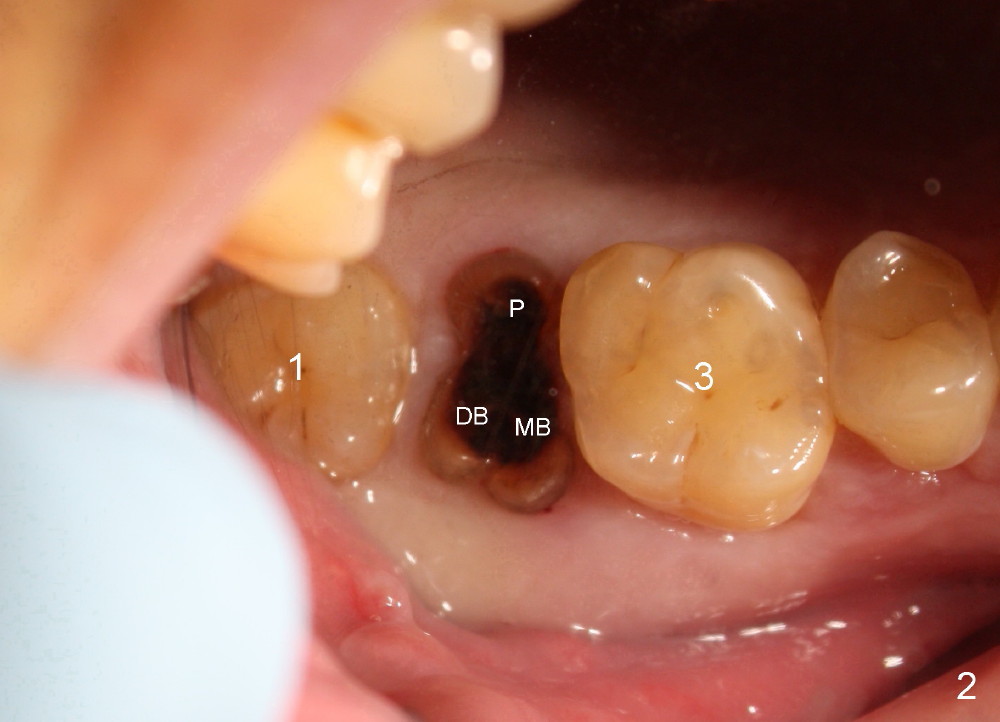
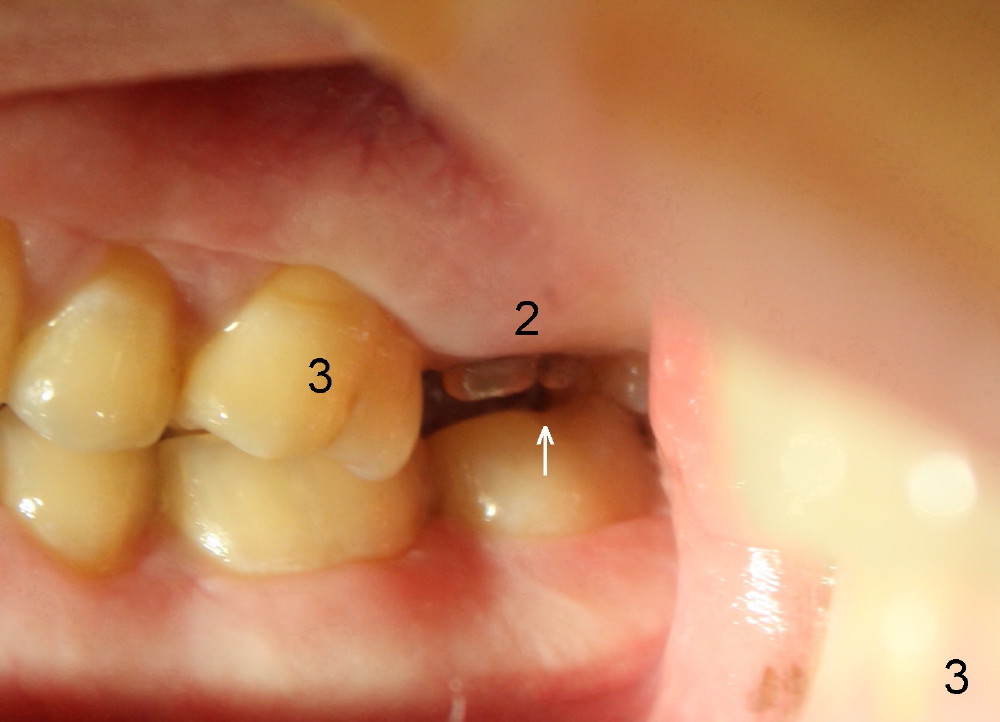
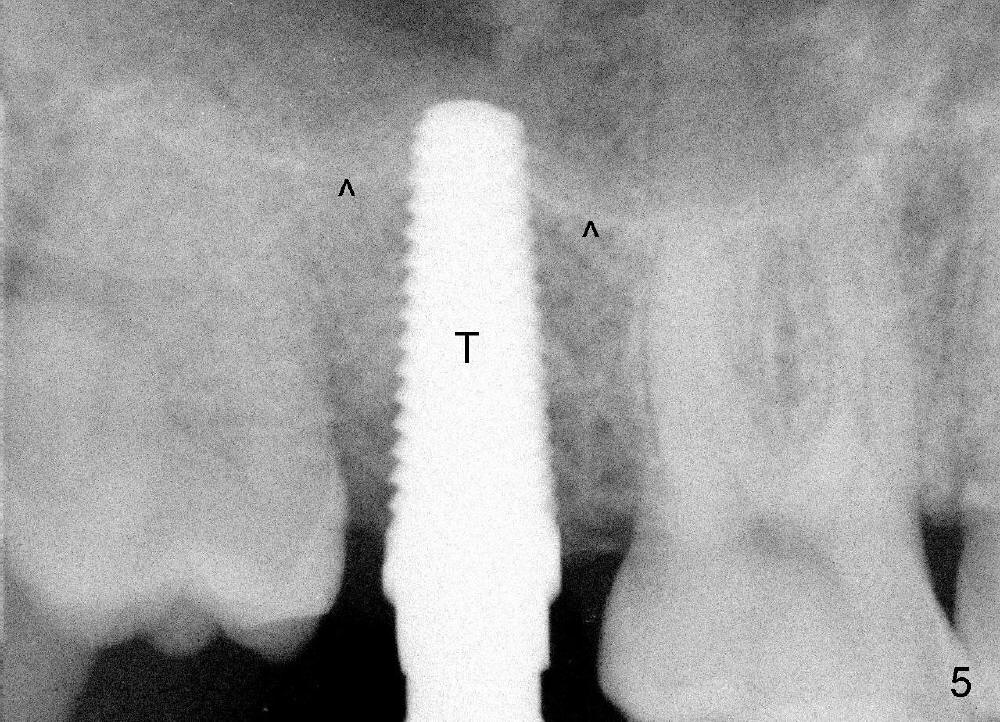
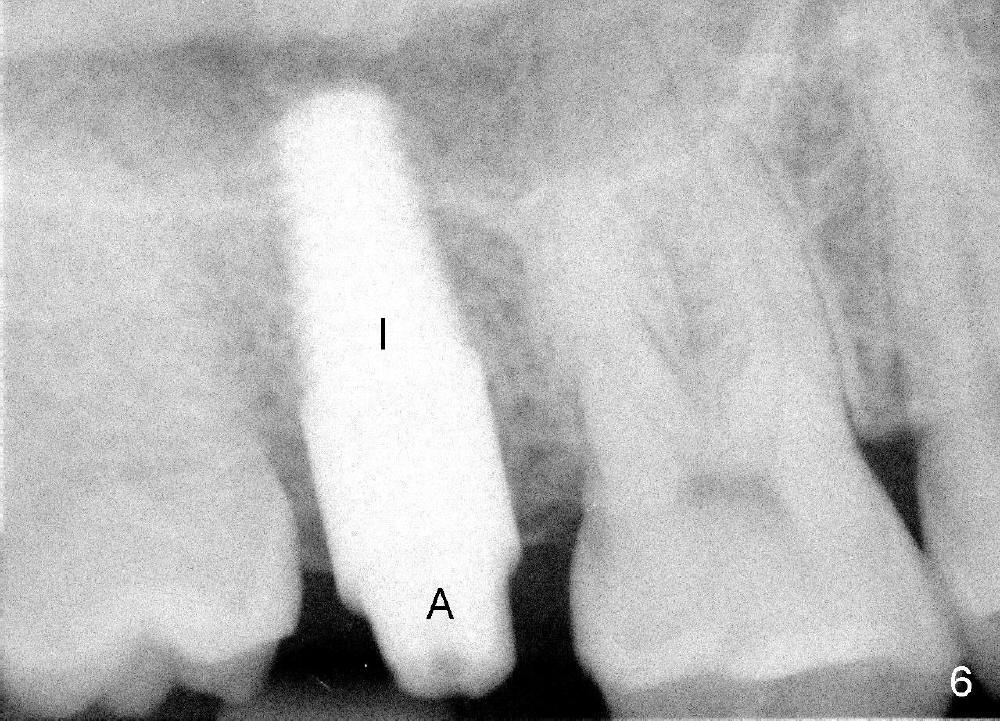
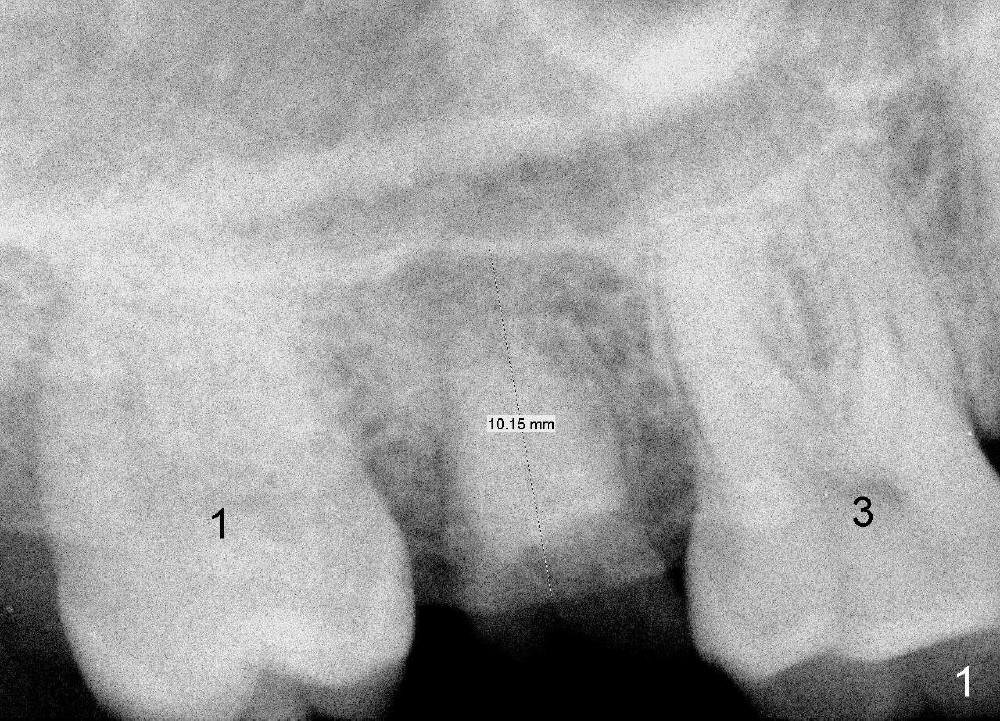
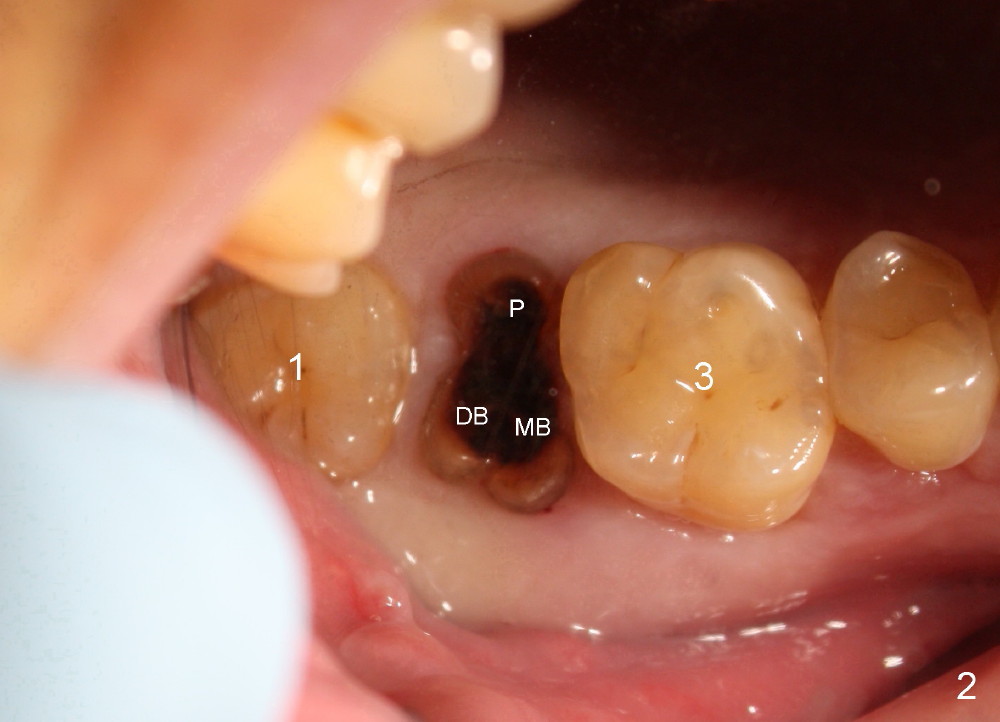
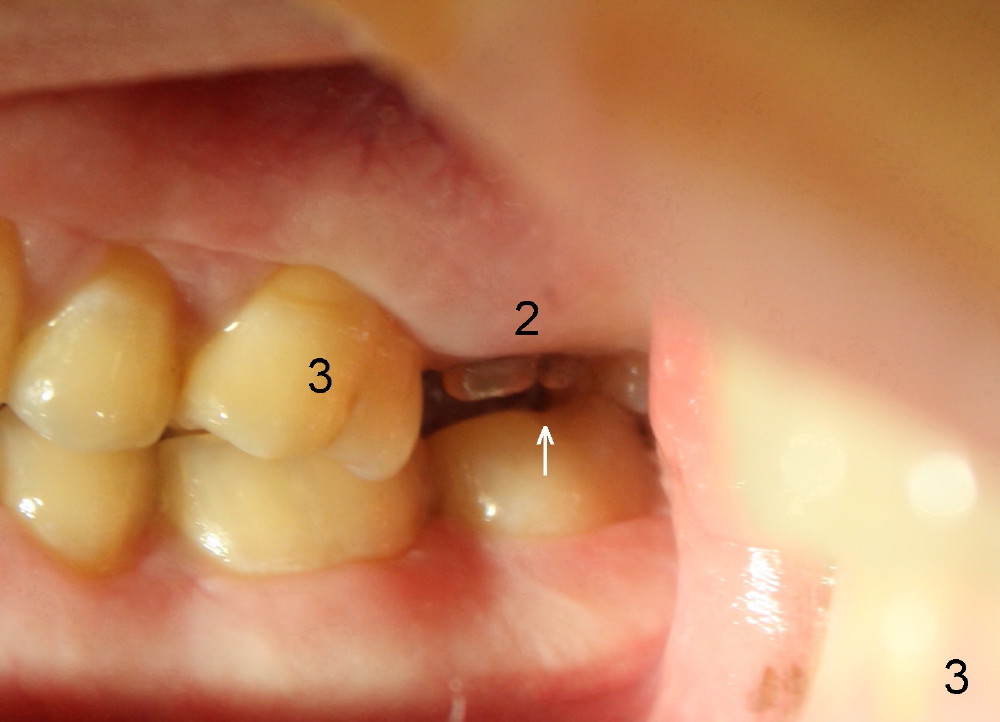
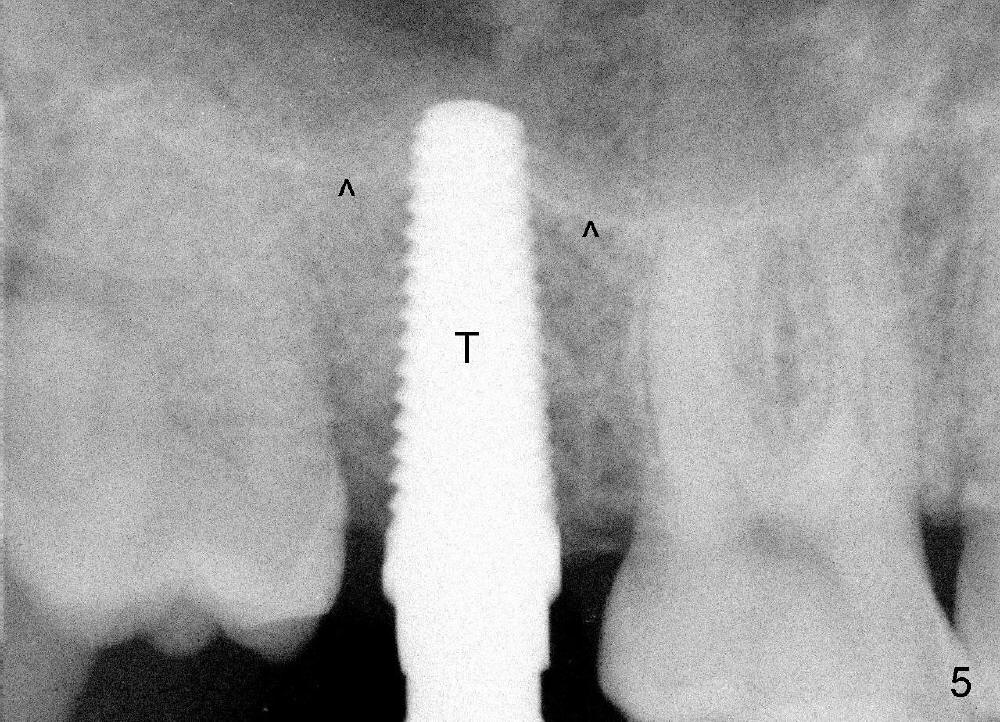
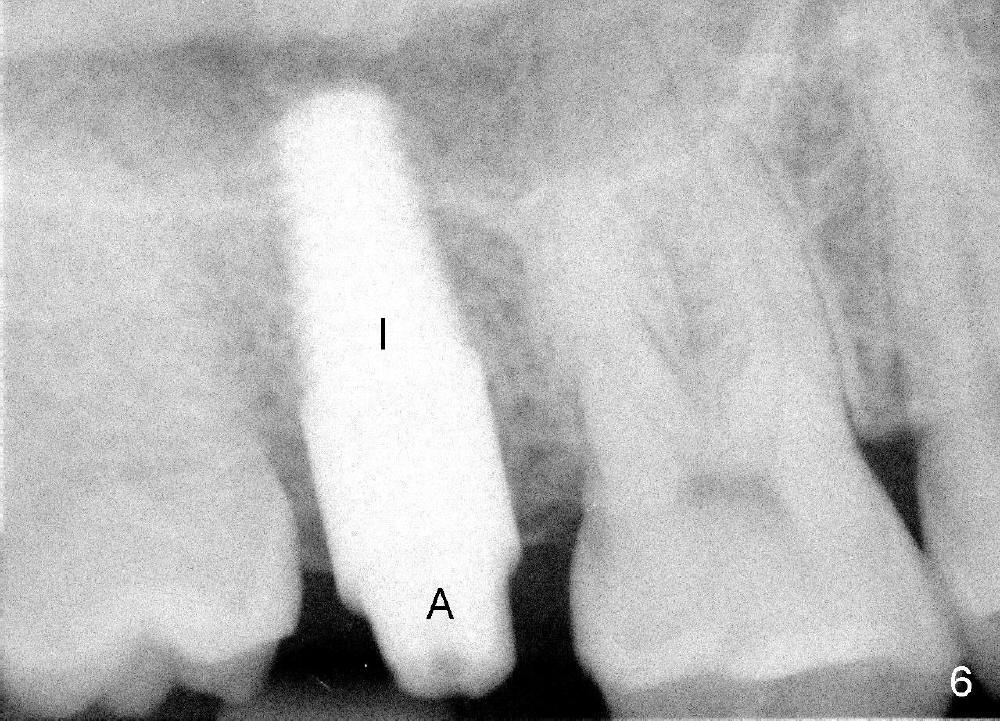
A 42-year-old man is afraid of dentistry. Residual roots of #2 remain untreated for at least 2.5 years (Fig.1). Both the mesiodistal space and the height are limited and unfavorable to restoration (Fig.2,3). Finally he agrees to have treatment, since the tooth #15 is worn so much that it is sensitive to mastication. When the tooth #2 is extracted, the socket is triangular without septum (Fig.4); the bottom of the socket is flat and easy for osteotomy. A 5x17 mm tap has obtained stability once it is placed ~ 14 mm deep (Fig.5). A 5x14 mm implant is placed with insertion torque > 60 Ncm (Fig.6 I), followed by placement of 4x3 mm abutment (A).
To prevent the narrow spaces from getting worse during osteointegration, an immediate provisional is to be fabricated. There is not enough occlusal clearance when the abutment is reduced ~1.5 mm. The abutment is removed; the implant is placed ~ 1 mm deeper with primary stability. Then the occlusal clearance is sufficient; the provisional is made. Mixture of autogenous bone, allograft and Osteogen is placed in the remaining buccal and lingual sockets (Fig.7 *). The provisional is temporarily cemented (Fig.8 P), which keeps the bone graft in place.
This case has demonstrated an additional advantage of immediate provisional. Fabrication of the immediate provisional can immediately indicate whether there is sufficient occlusal clearance. The length of the abutment can be adjusted. More importantly, the depth of the implant can be adjusted. It is much harder to solve occlusal clearance once the implant is osteointegrated. The opposing tooth may need orthodontic intrusion.
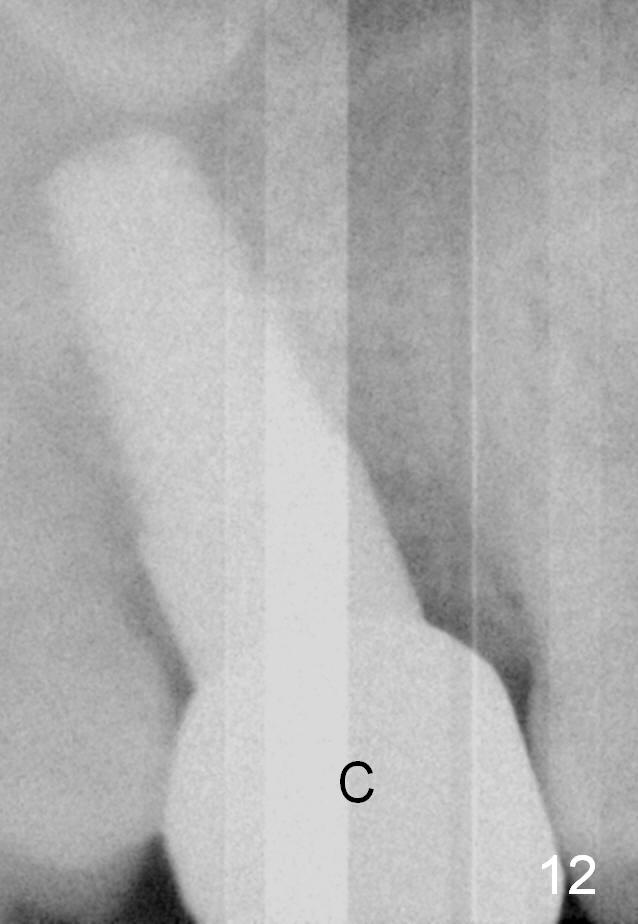
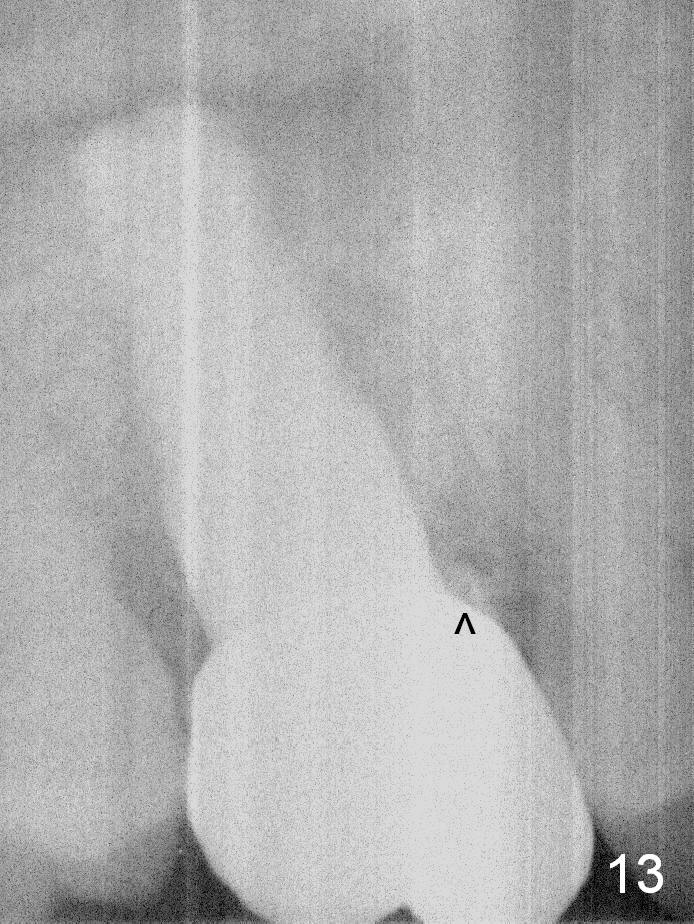
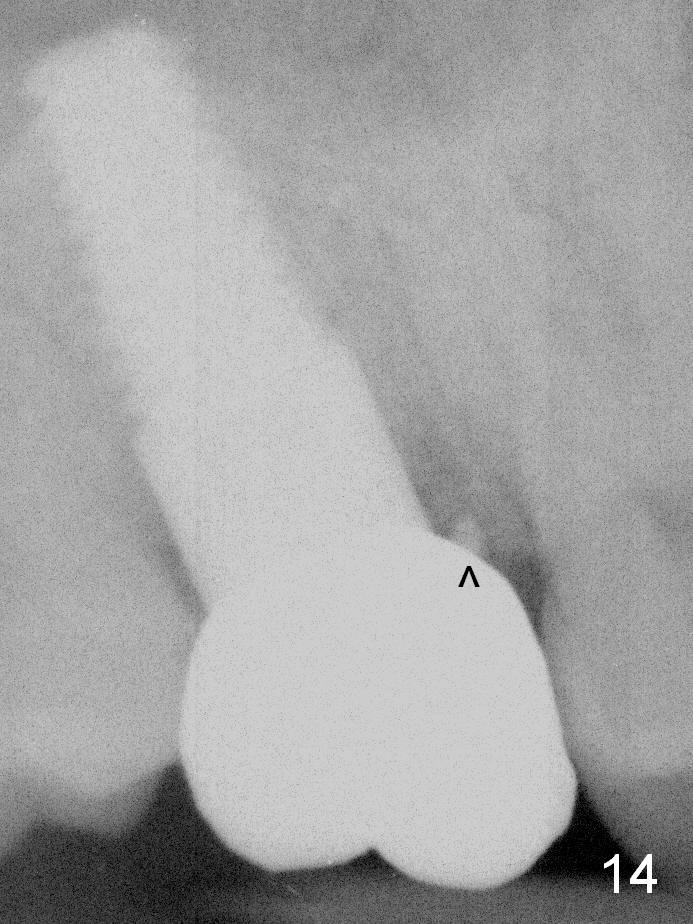
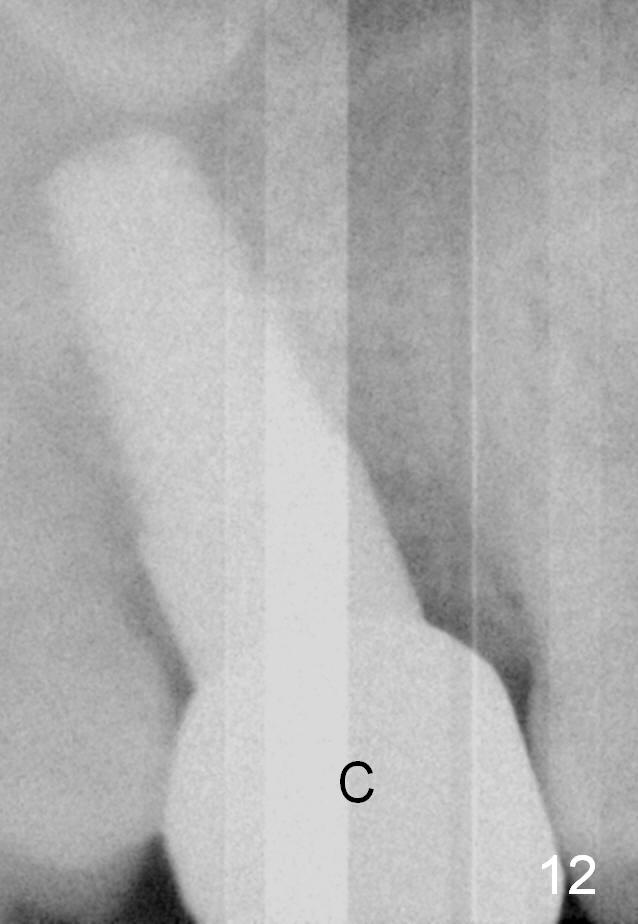
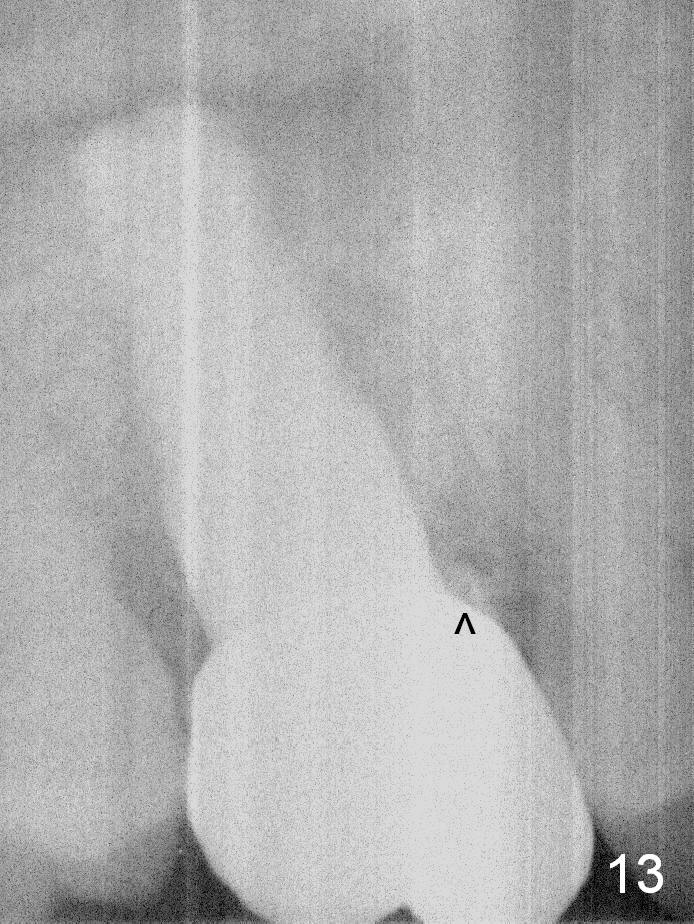
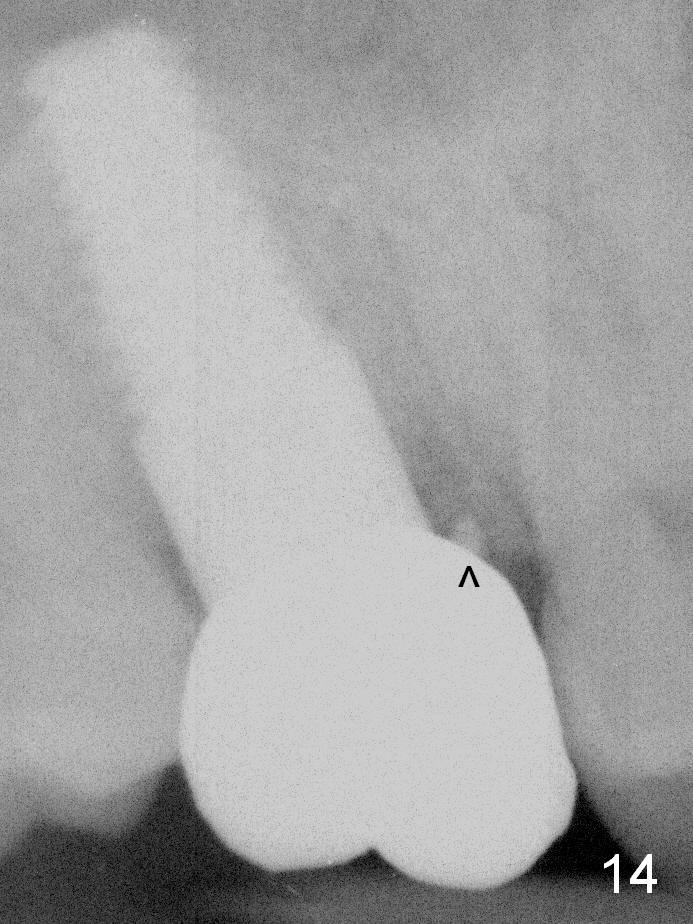
The implant remains stable 2.5 months postop without abnormal bone resorption (Fig.9). Since the provisional has dislodged on several occasions, impression is taken for final restoration. When the provisional is removed 3 months postop, the margin of the restoration is shown to be subgingival (Fig.10 arrowheads), but is distinctly separated from the gingiva. This is due to the presence of the provisional (its margin were fabricated slightly deeper). The provisional is also intentionally fabricated slightly larger than the final restoration. When the latter is cemented, there is space to remove extra cement trapped subgingivally (Fig.11). No cement is visible post cementation (Fig.12 (C: crown)). Eighteen months post cementation, the patient returns for recementation. After laser gingivectomy and Panavia resin bonding, PA shows residual cement (Fig.13 ^). After repeated removal with Piezo scaler and explorer, the residual cement appears to be smaller, which is ignored at the time of X-ray taking (Fig.14 ^). More dismayed is tight mesial contact. Water pik is recommended. When peri-implantitis develops later on, make an incision for cement removal. If the crown is dislodged soon, check whether the existing abutment is loose, remove acrylic in the access hole and remove the abutment. Install a new 4x3 mm one. Trim the abutment carefully and more on the opposing tooth.
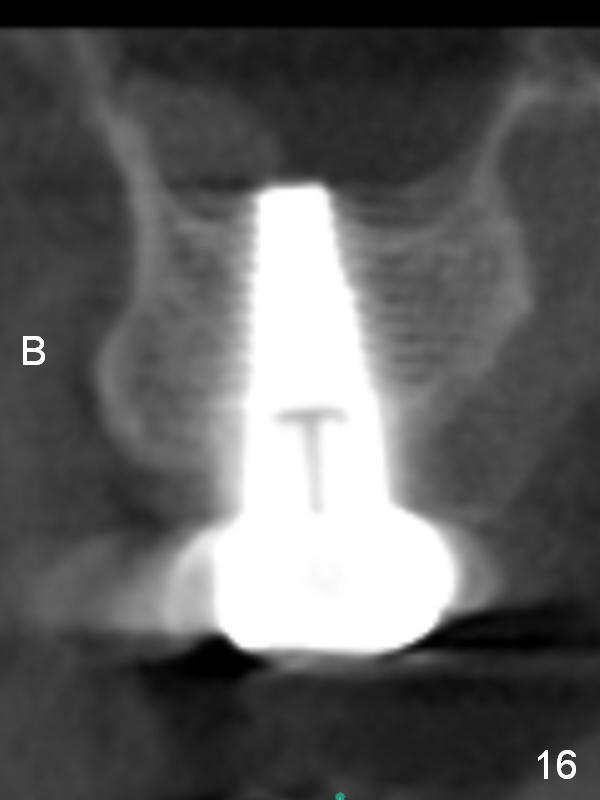
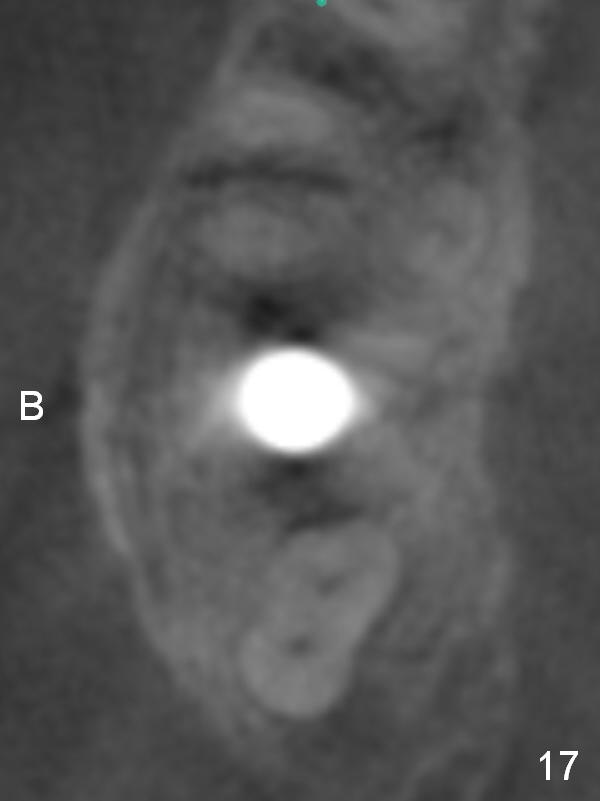
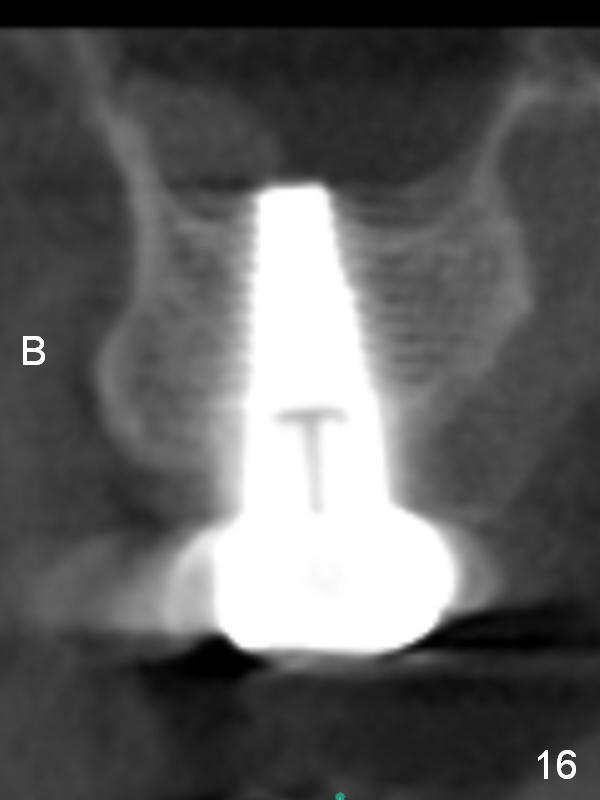
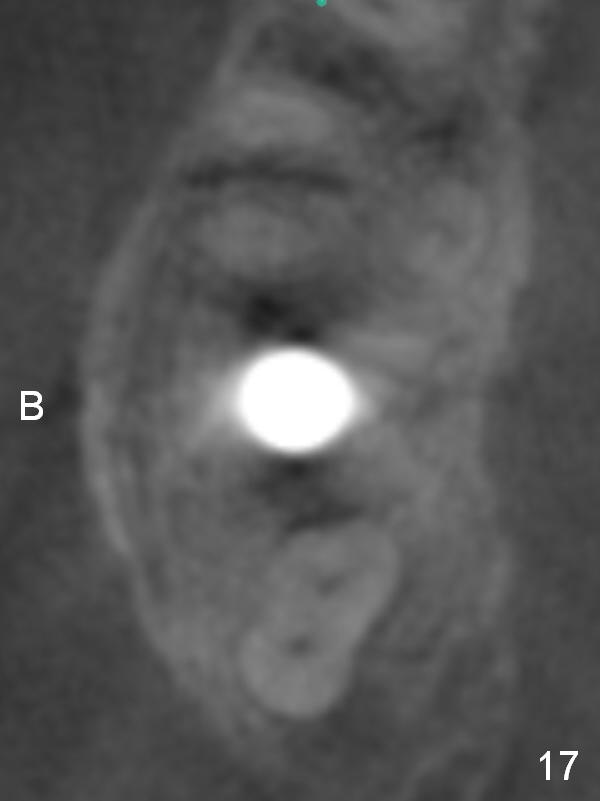
CBCT taken 23 months post cementation shows no abnormality (Fig.15-17). On the contralateral side, the apex of the tooth #15 is immediately inferior to the sinus floor (Fig.18 (sagittal section), 19 (coronal section)). The immediate implant seems to be unavoidably entering the sinus. The implant seems to be normal 3 year 5 months post cementation.
Return to Upper Molar Immediate Implant,
Posterior Immediate Provisional,
CT Follow-up,
Intrusion
Xin Wei, DDS, PhD, MS 1st edition 11/06/2014, last revision 01/07/2020