
.jpg)
_1333x1000.jpg)






 |
.jpg) |
_1333x1000.jpg) |
 |
 |
|
 |
 |
 |
 |
||
 |
 |
 |
|||
1-Piece Implant with 4 mm Cuff for Periodontally Affected Lower Incisor
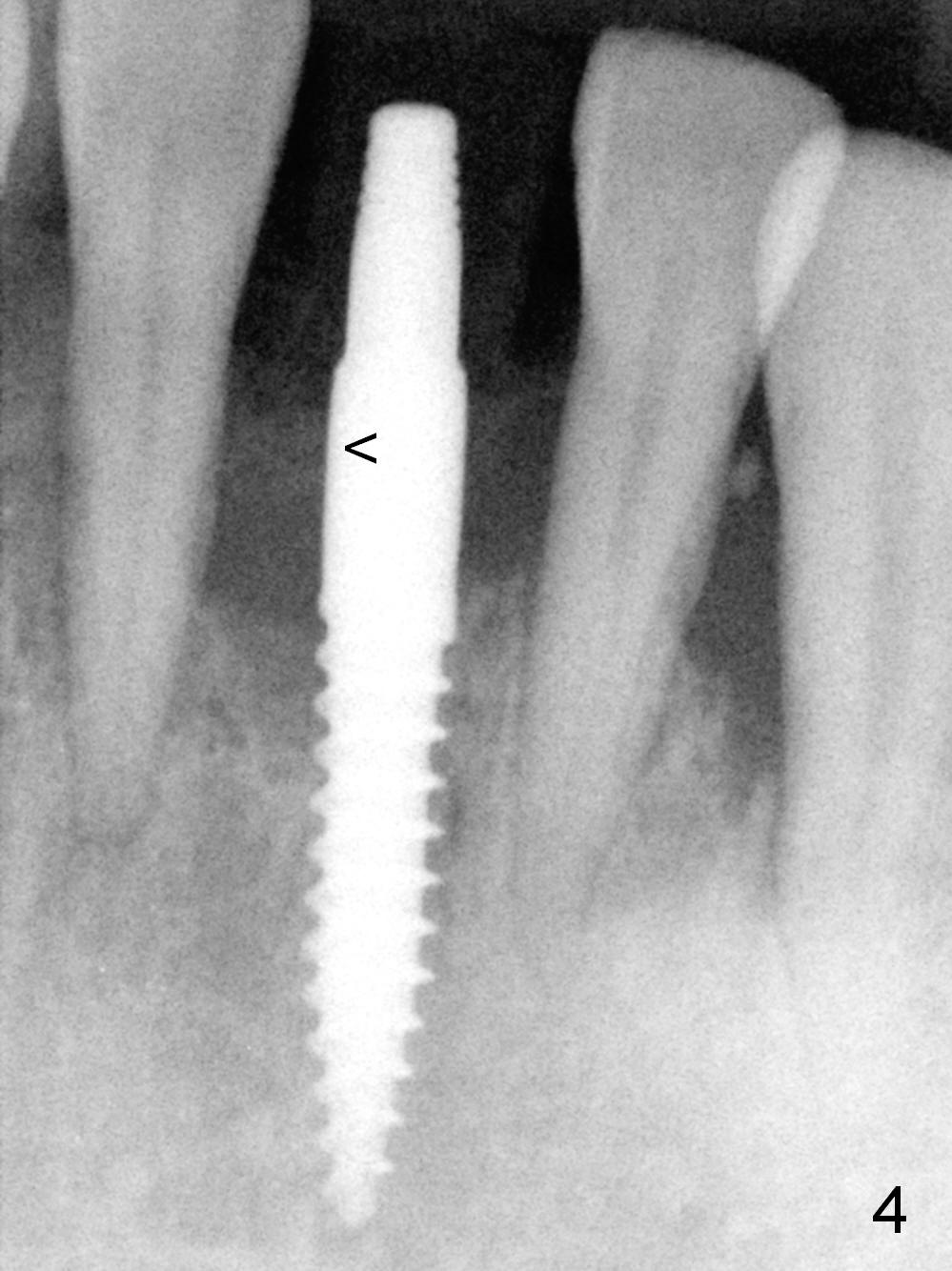
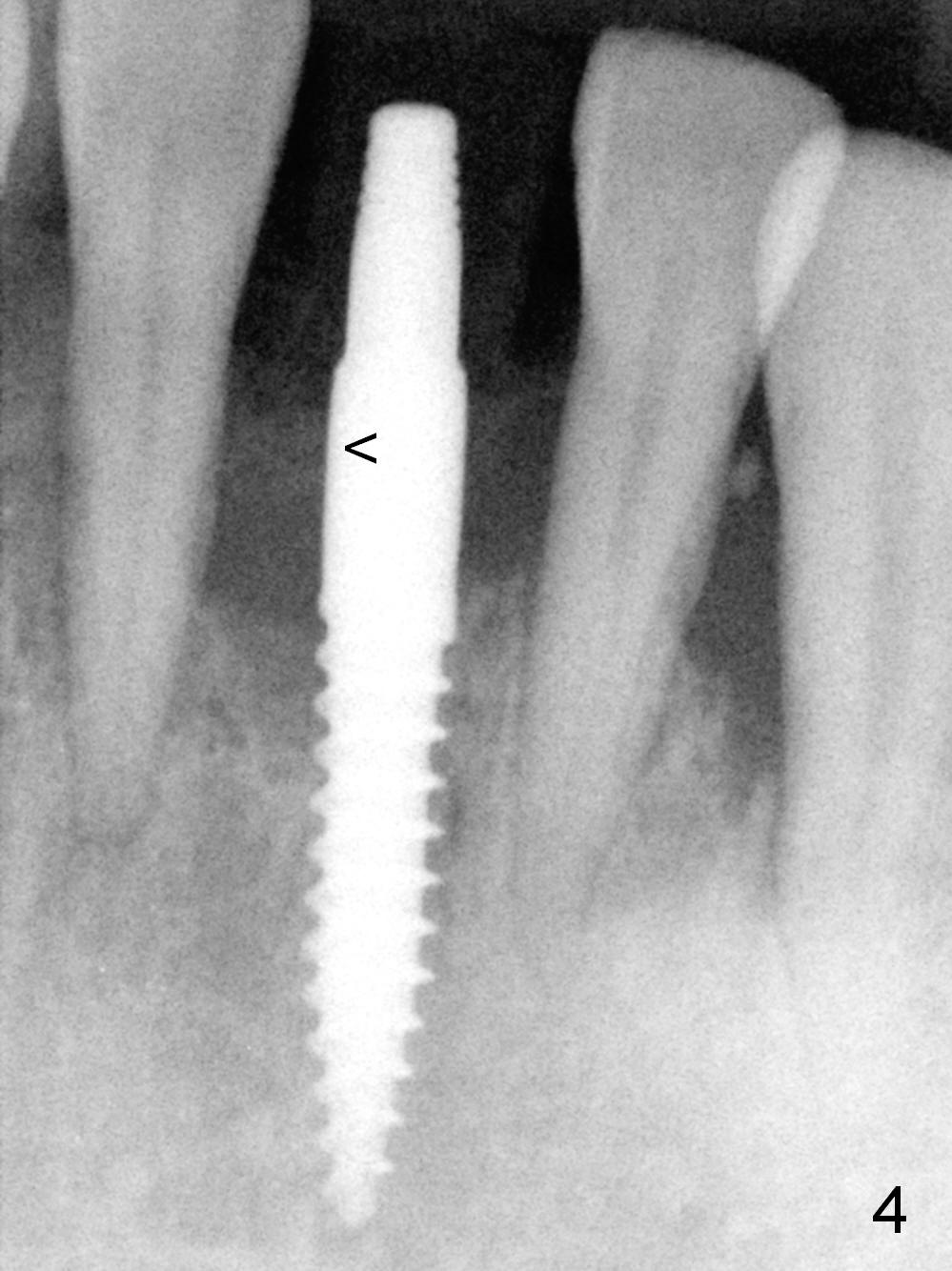
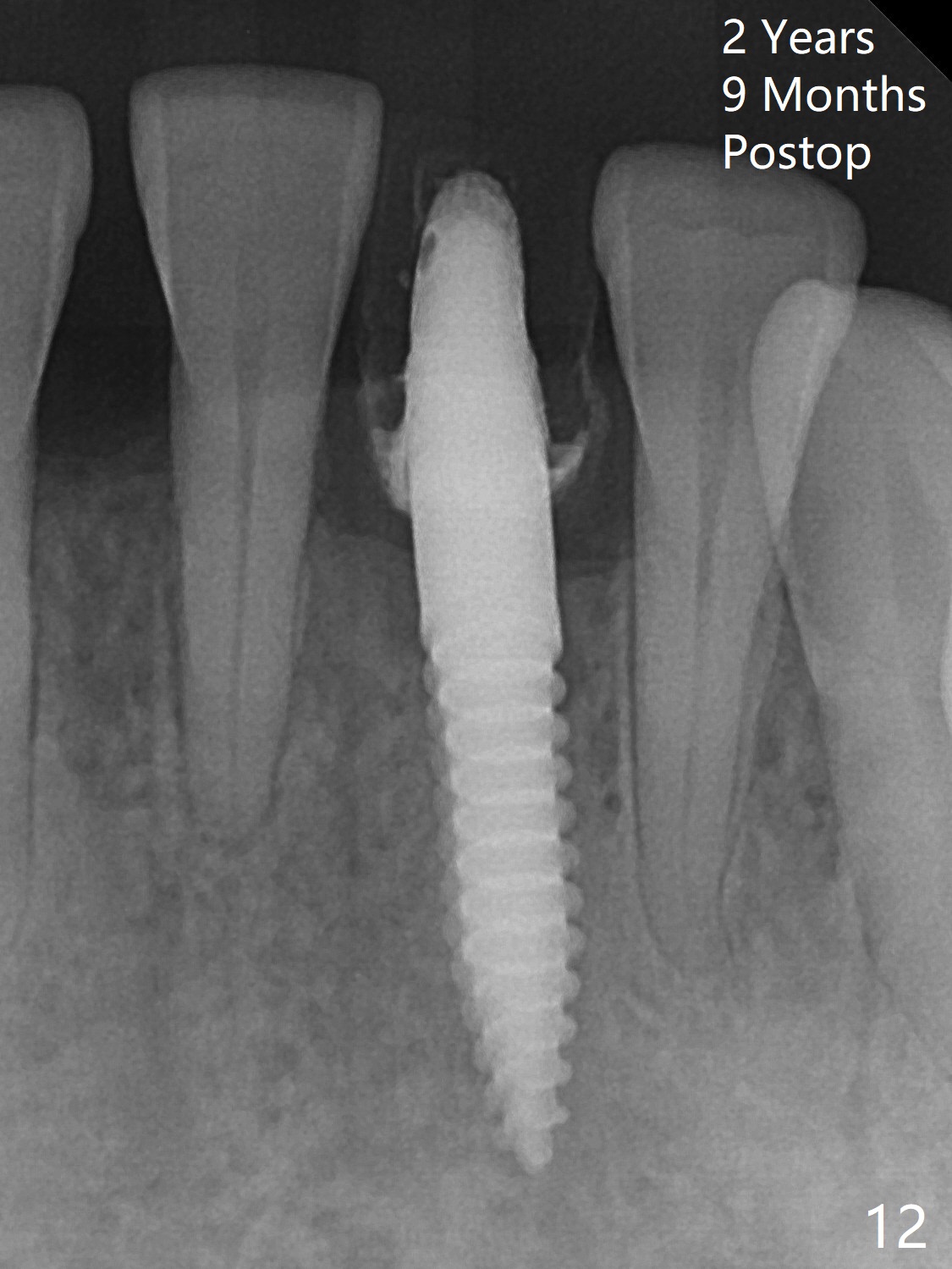
Preop examination shows that the tooth #25 is labially displaced. The mobility is the same as that of #23. It does not make sense to splint the tooth #25 to #23 and 26. Besides, the patient is extremely nervous. Before lower quadrant scaling & root planing, the tooth #24 is extracted; the socket is packed with gauze soaked with Clindamycin and 2% Xylocaine, 1:50,000 Epinephrine for prolonged period of time. But hemostasis is difficult to obtain, since hemorrhage is from the inflamed lingual gingiva. The buccolingual position of the osteotomy is determined by digital palpation over the buccal and lingual plates. When a 1.5 mm pilot drill (Fig.1) is withdrawn from the osteotomy, the latter is slightly buccal. When a 3x14 (4) mm 1-piece implant is being placed, palpation shows no buccal or lingual perforation. The insertion torque is more than 35 Ncm (Fig.2,3). The 4 mm cuff is chosen because of the thick gingiva. When the implant is further seated (Fig.4), the most coronal thread of the implant is subcrestal except mesially. With bone graft (Fig.4 <), the chance of postop infection due to thread exposure should be low. An immediate provisional is fabricated to keep the graft in place, followed by perio dressing.
The patient complains of bulk of the lingual margin of the provisional 20 days postop (Fig.5 *). It appears that the buccal plate has started to be atrophic (Fig.6 ^, Fig.7 *).
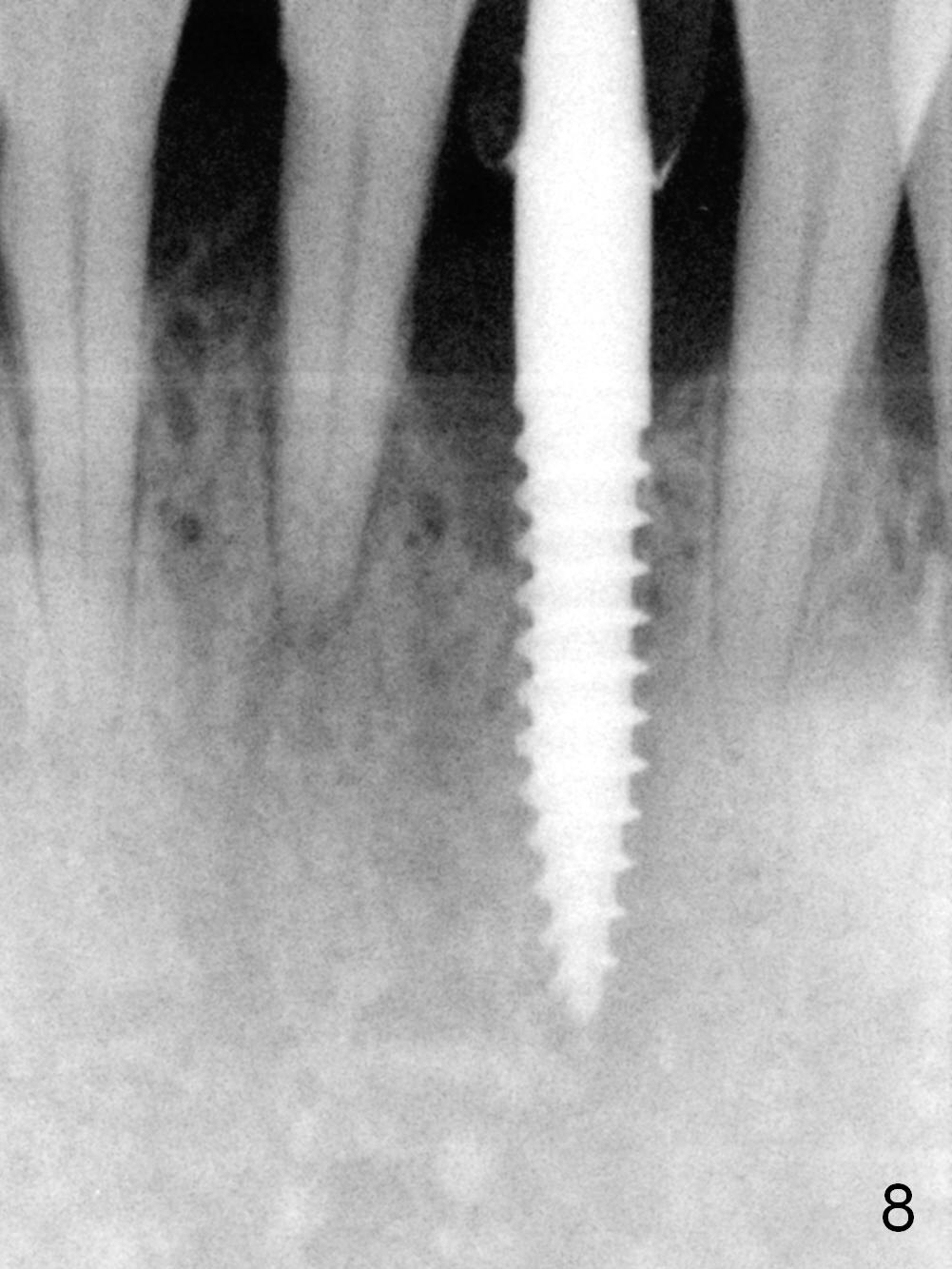
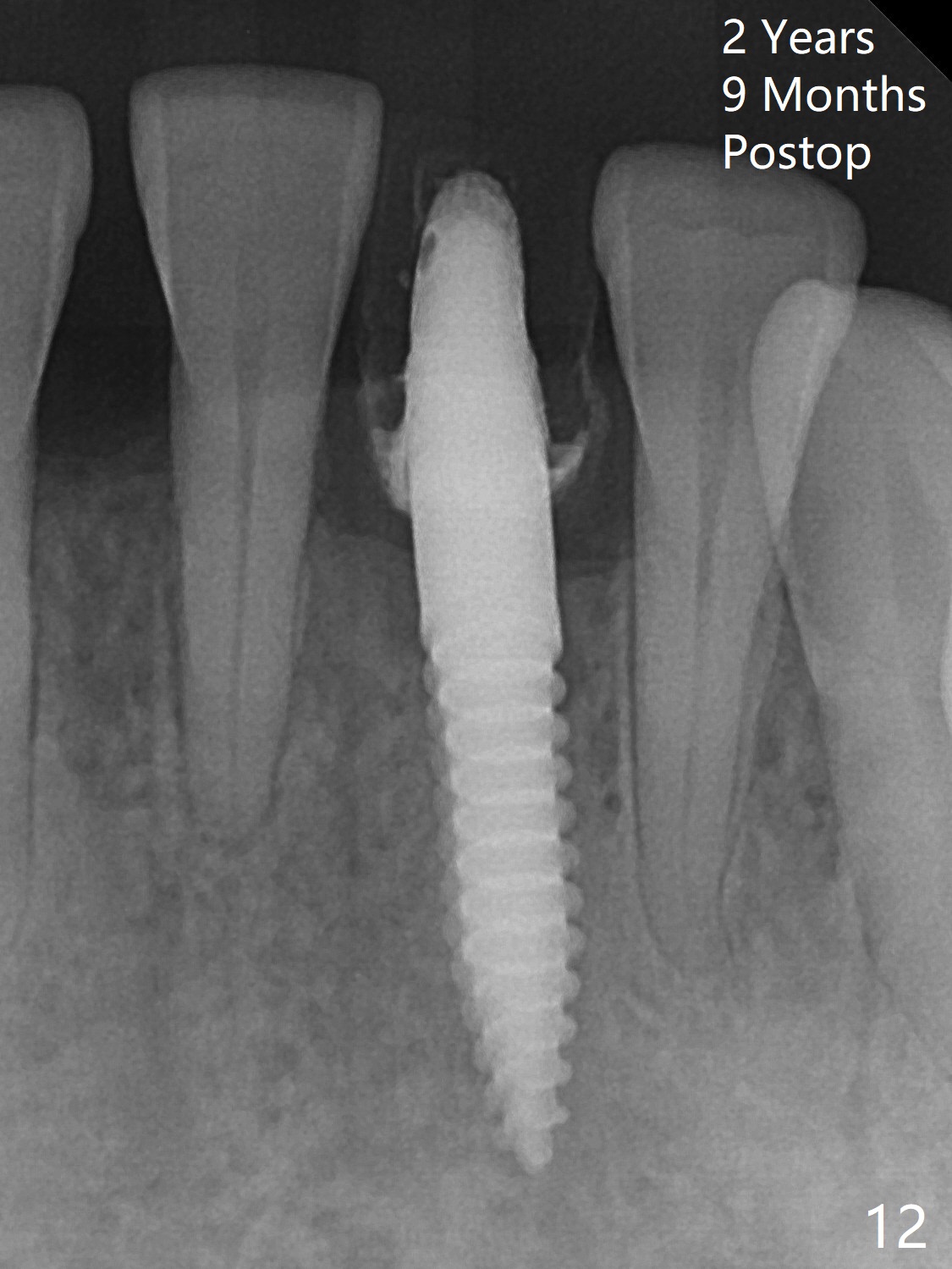
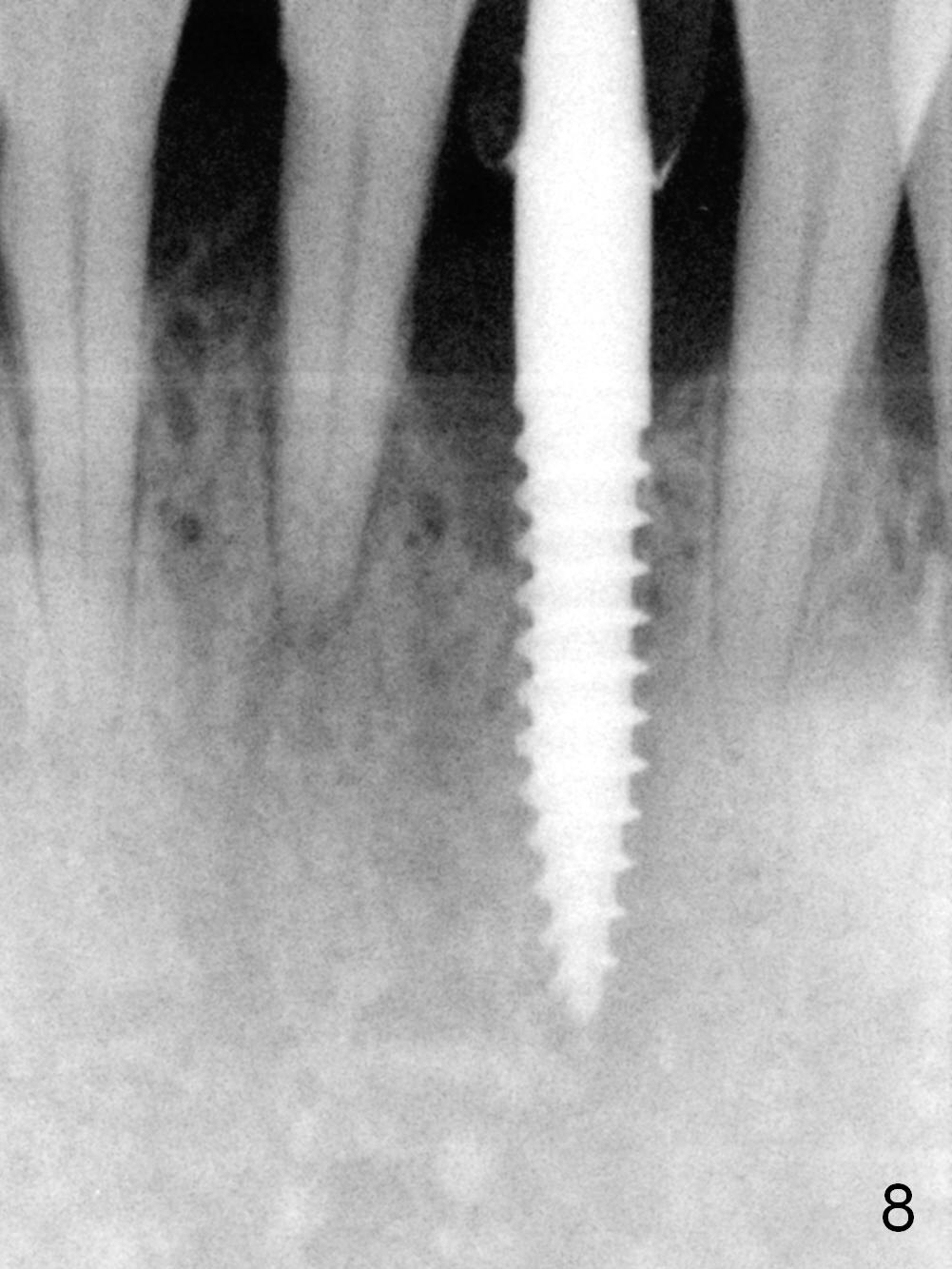
He returns again 4 months postop without implant thread exposure (Fig.8); the gingiva is healthy around the provisional (Fig.9). After taking impression (Fig.10), the patient is concerned about the shifting of #23 and 25 (Fig.11). If he agrees with limited orthodontics, check the alignment of the provisional. Trim the distal surface of the provisional so that the tooth #23 can be moved mesially without interference.
Return to
Lower Incisor Immediate Implant
Xin Wei, DDS, PhD, MS 1st edition 01/11/2016, last revision 10/07/2018