.jpg)

,.jpg)
 |
 |
 |
 |
 |
 |
 |
|
.jpg) |
 |
 |
|
 |
 |
,.jpg) |
|
RPD as a Surgical Guide
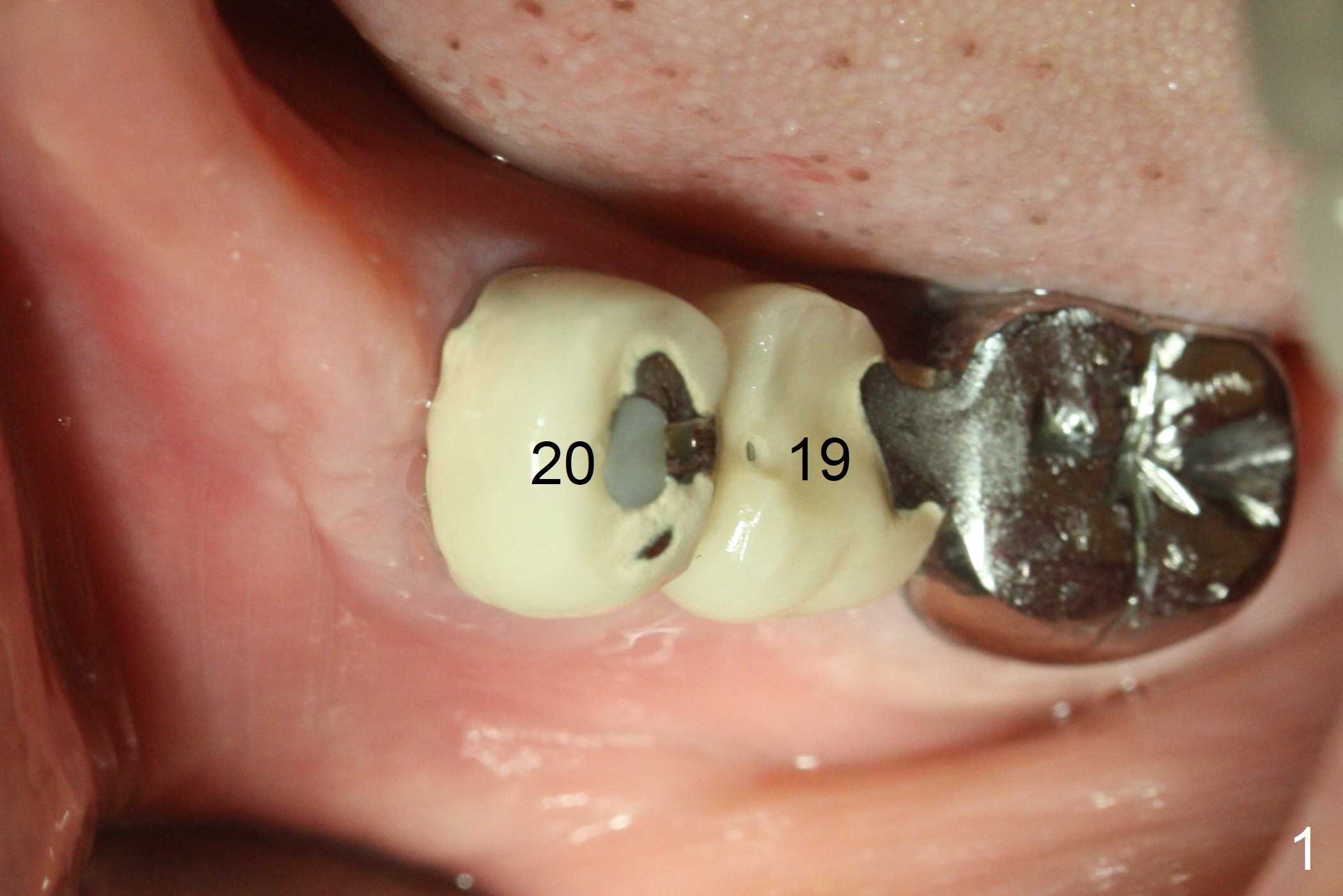
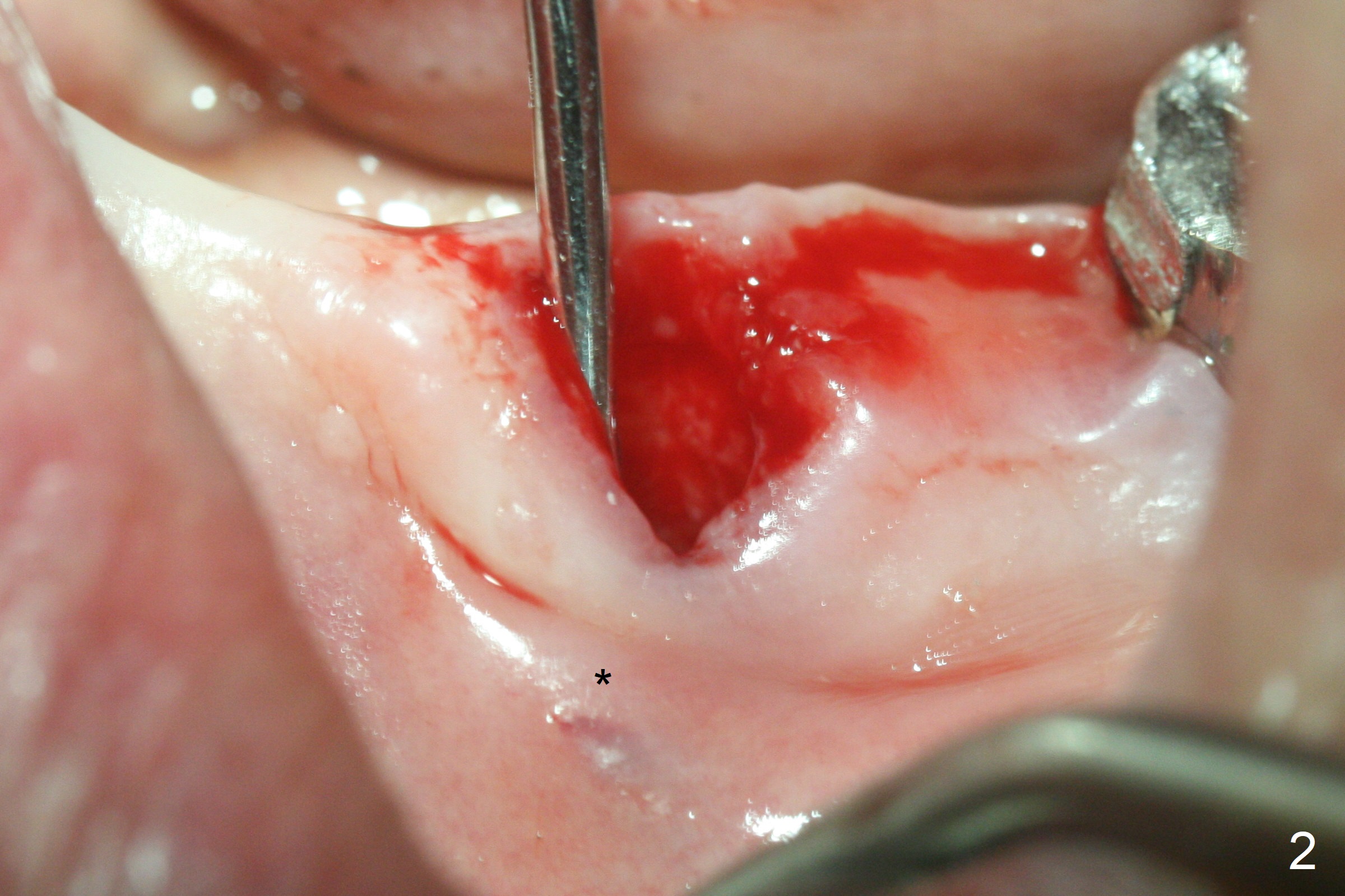
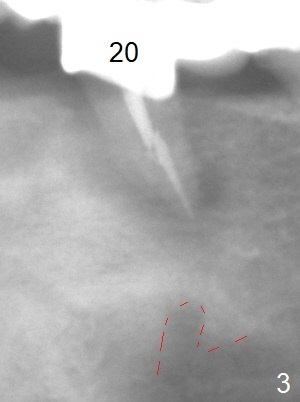
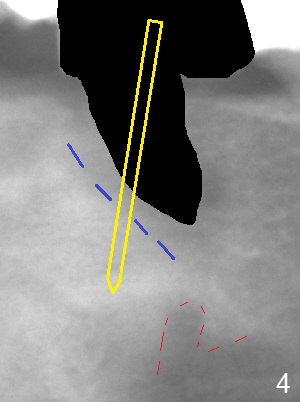
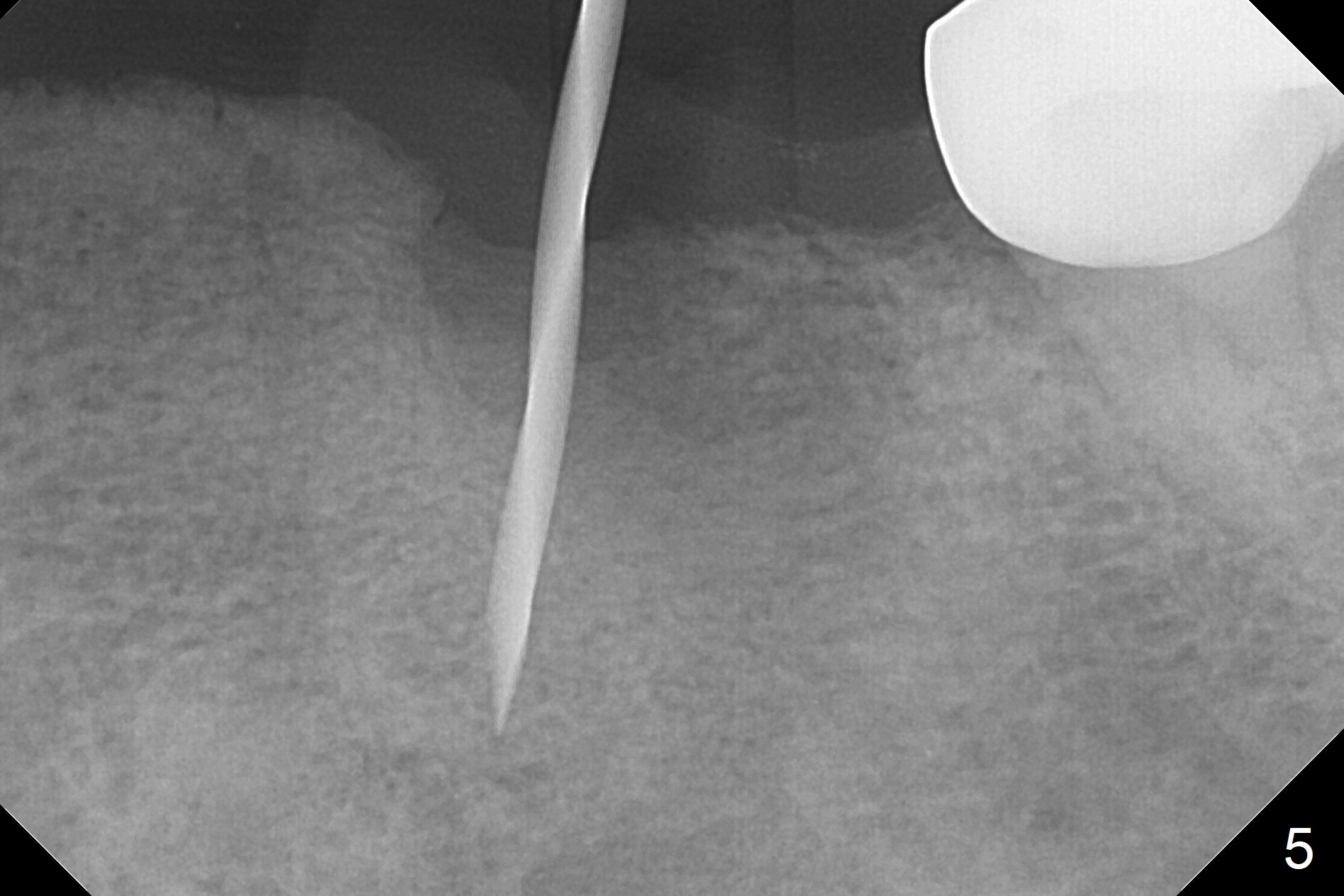
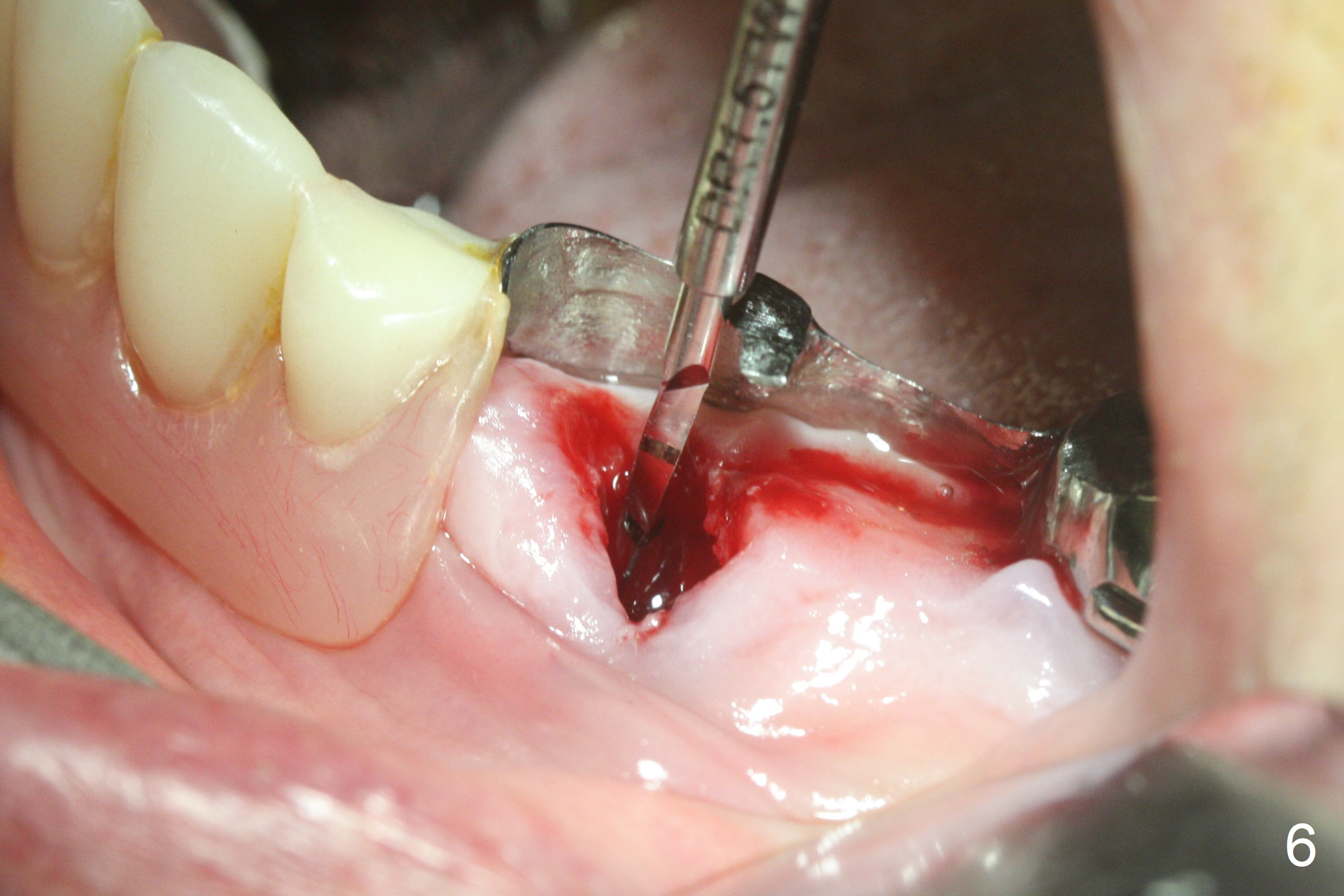
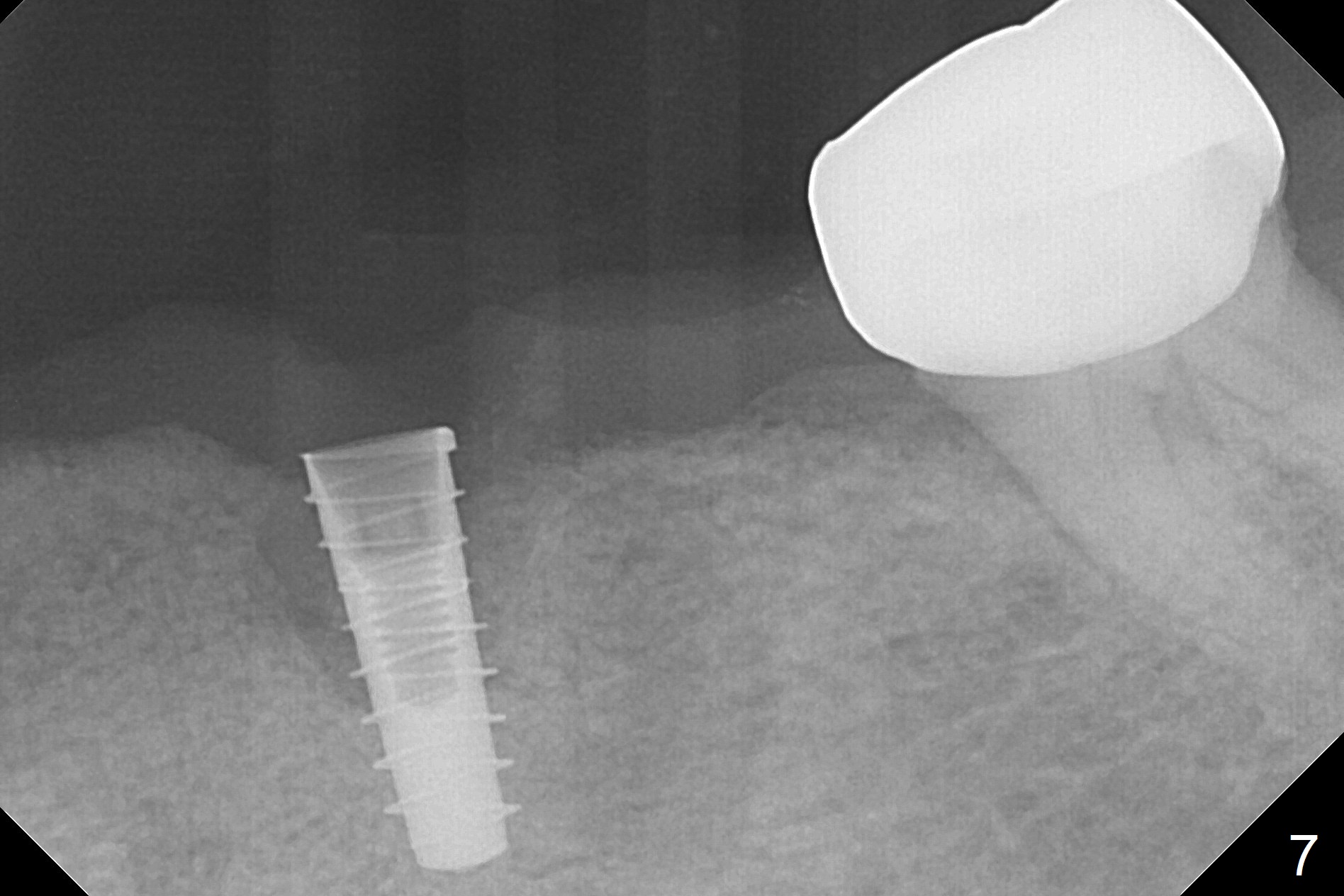
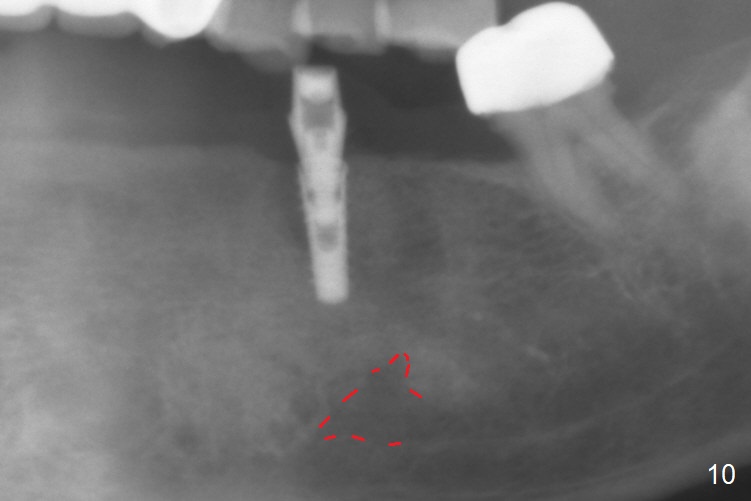
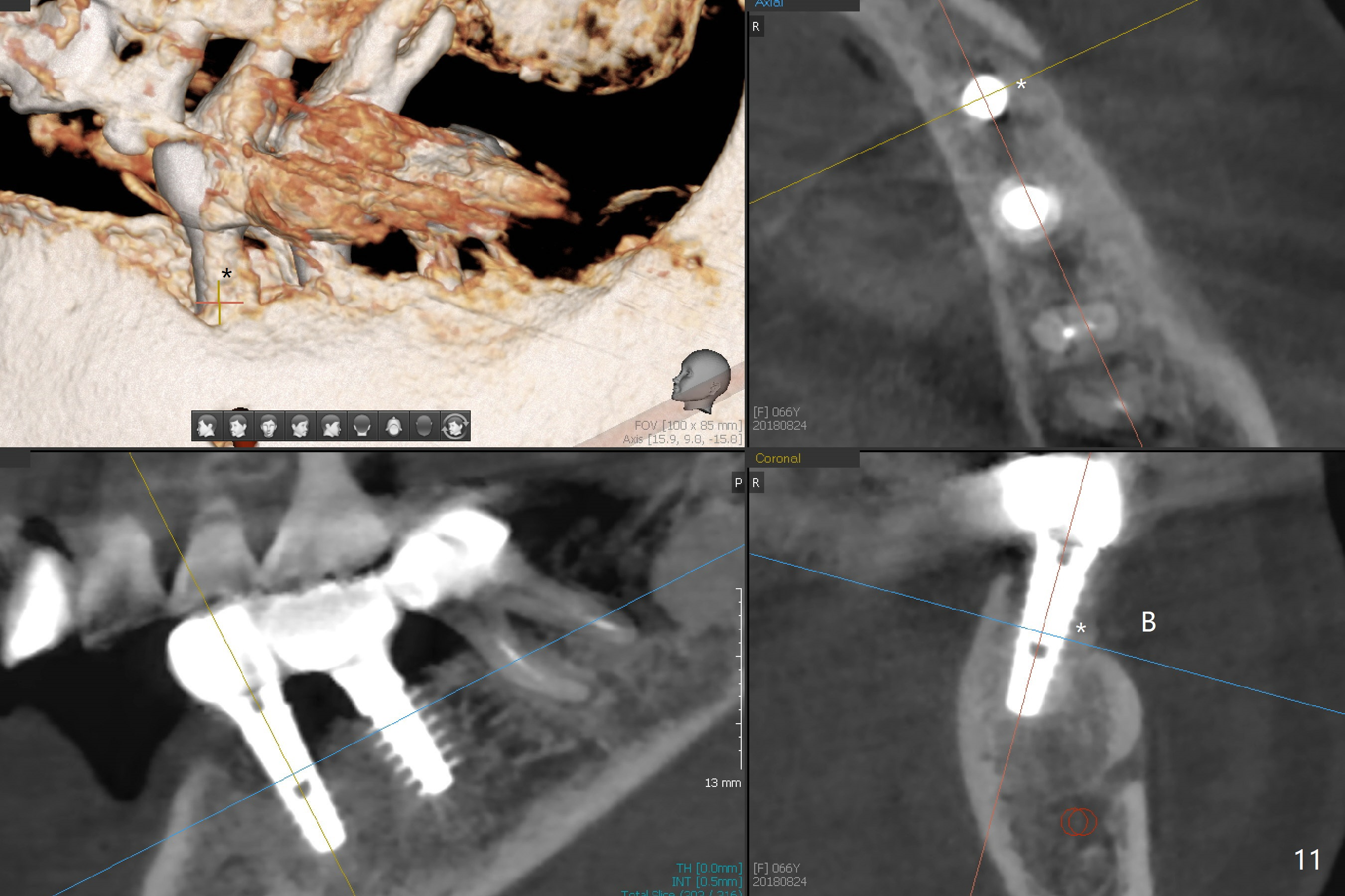
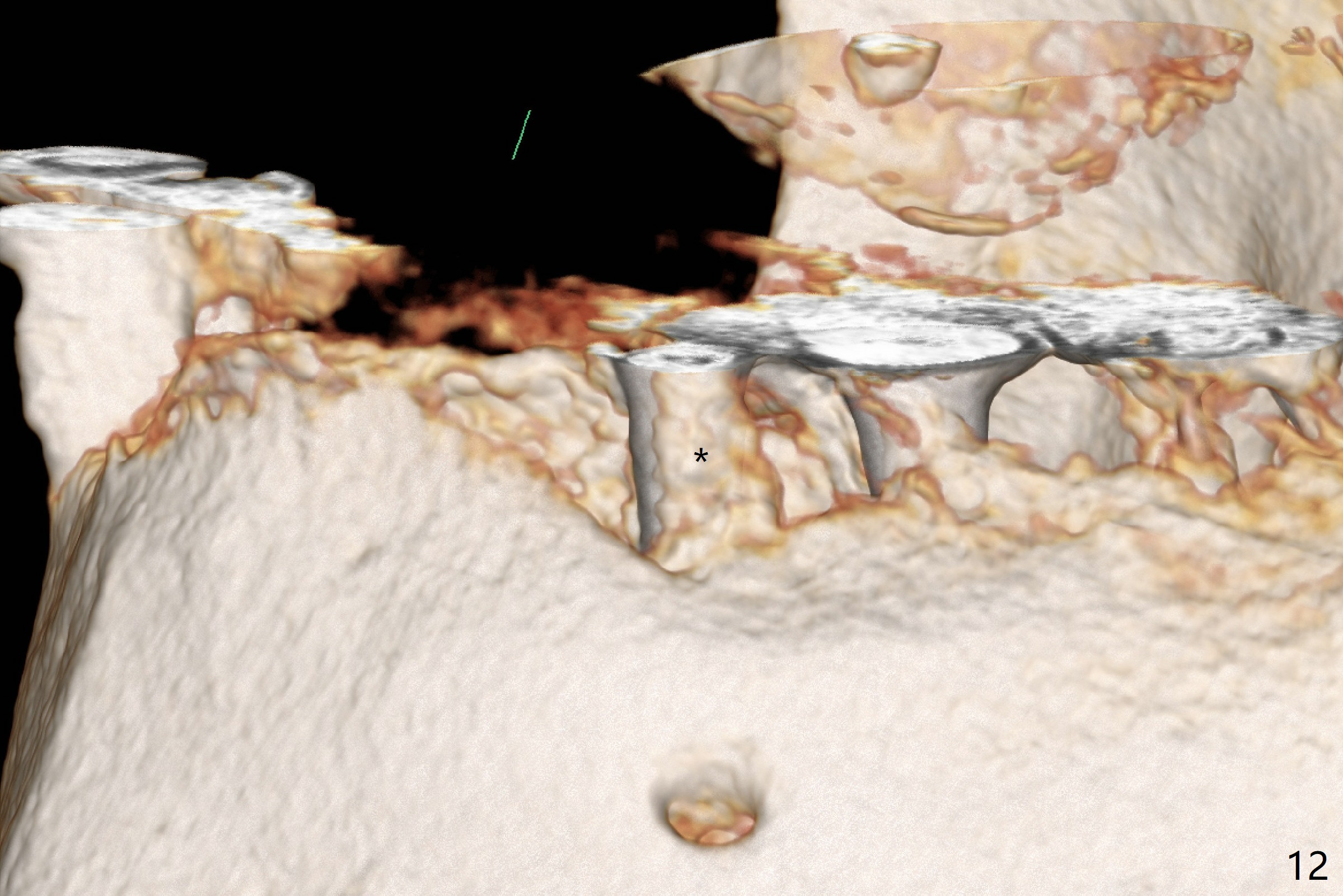
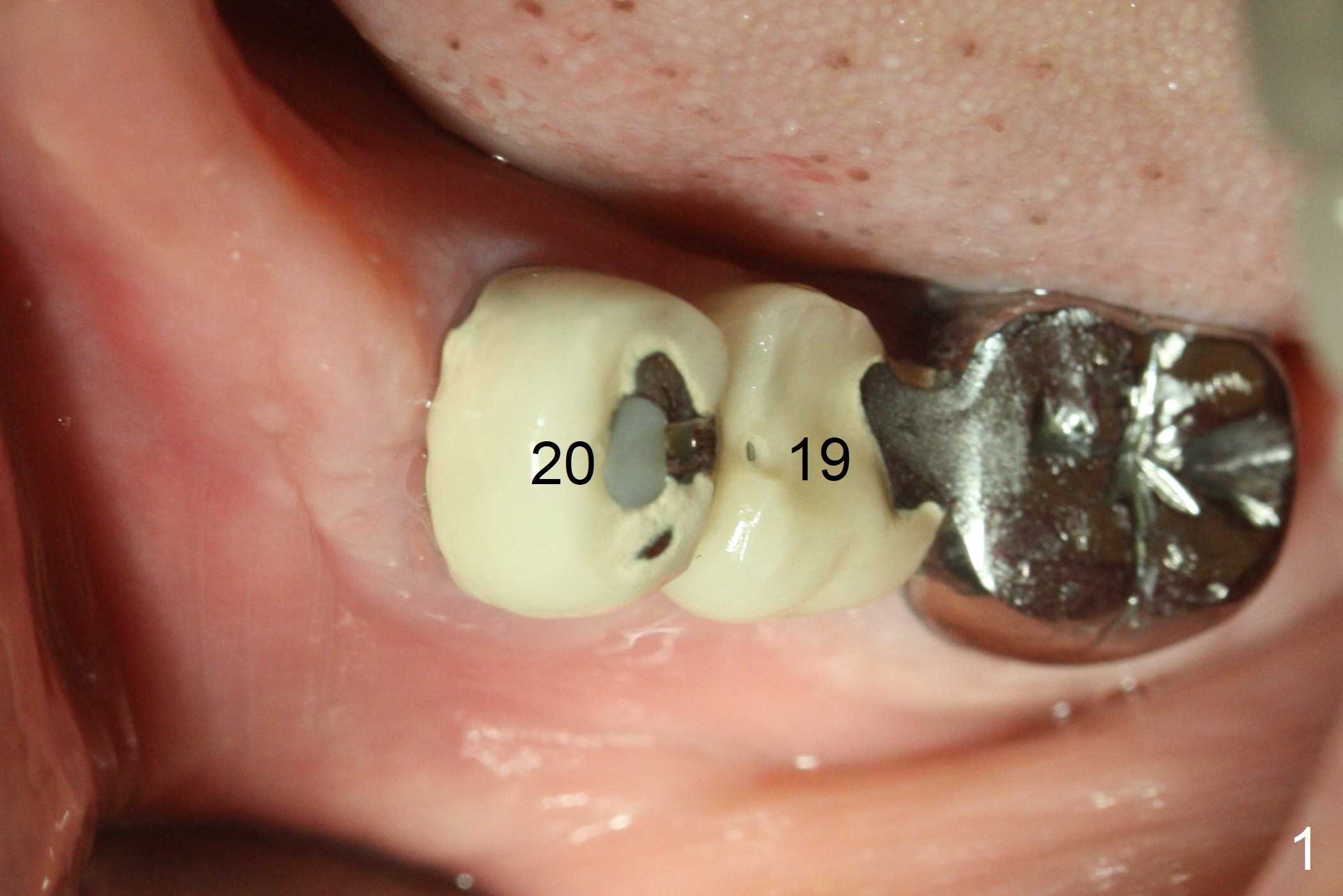
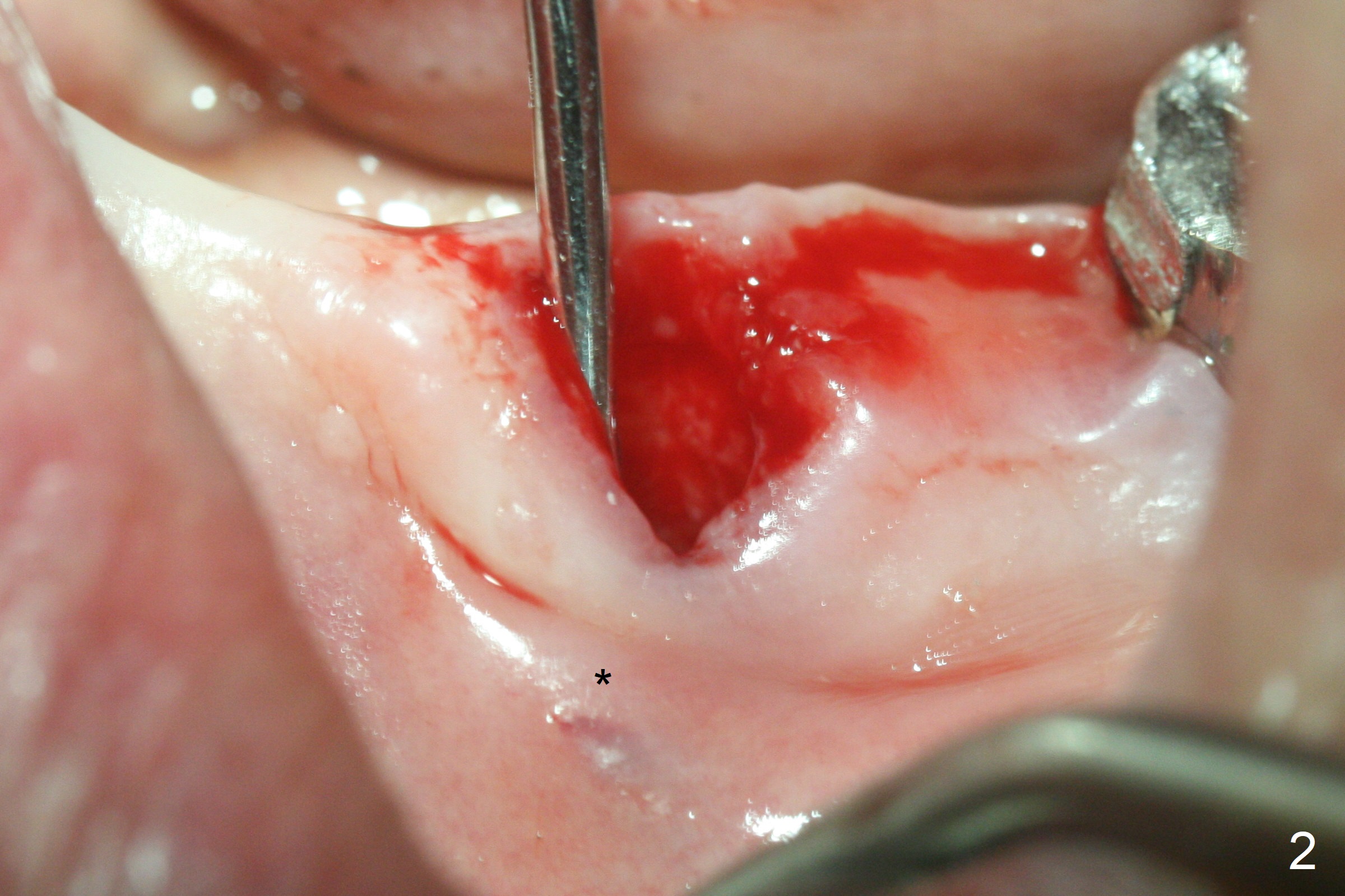
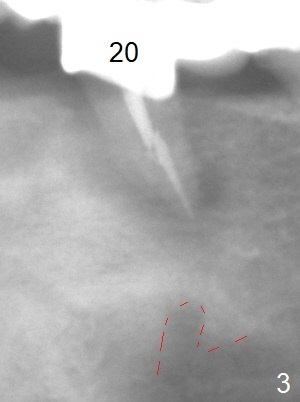
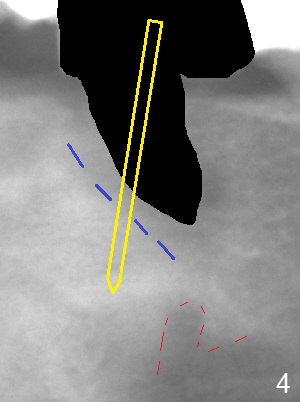
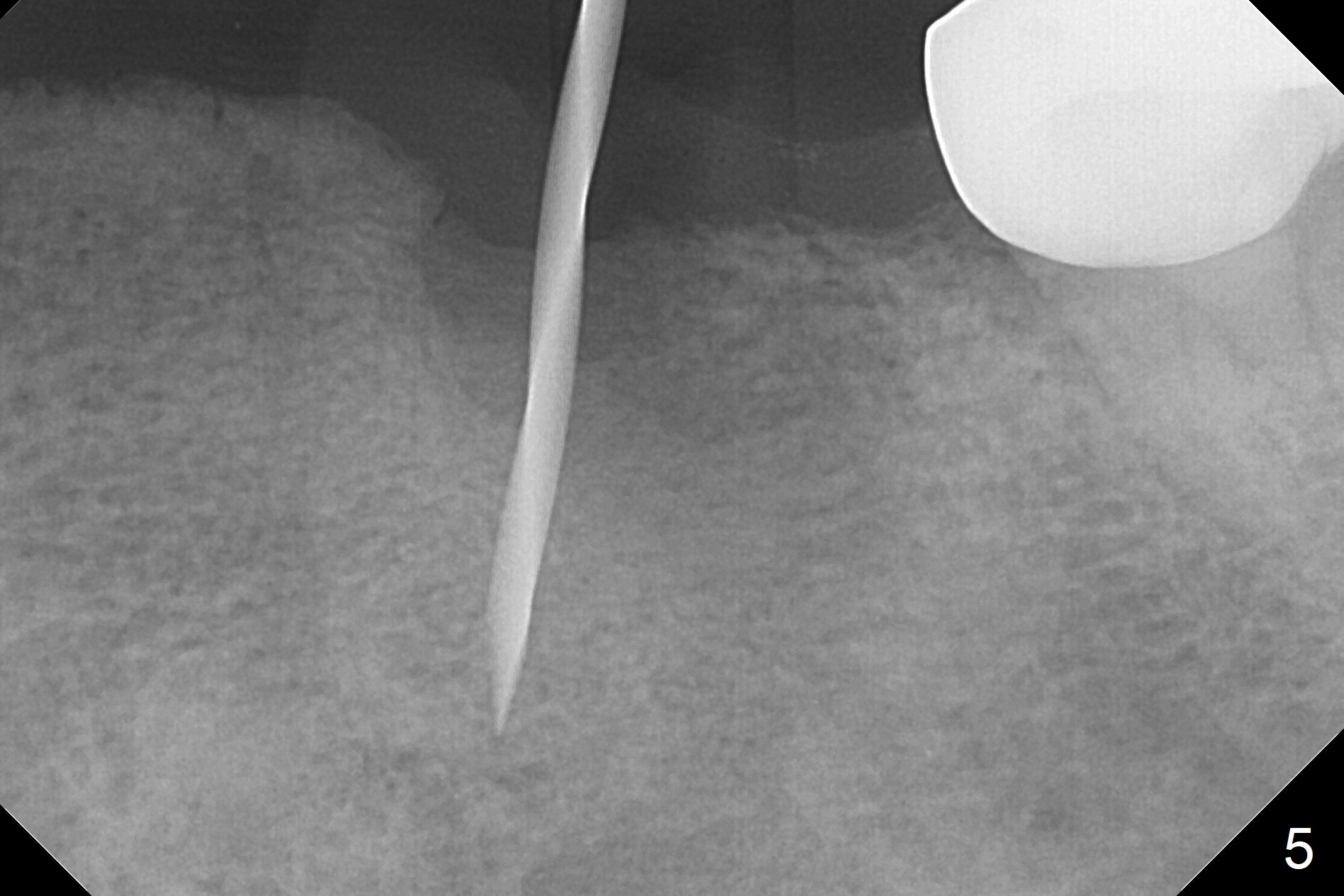
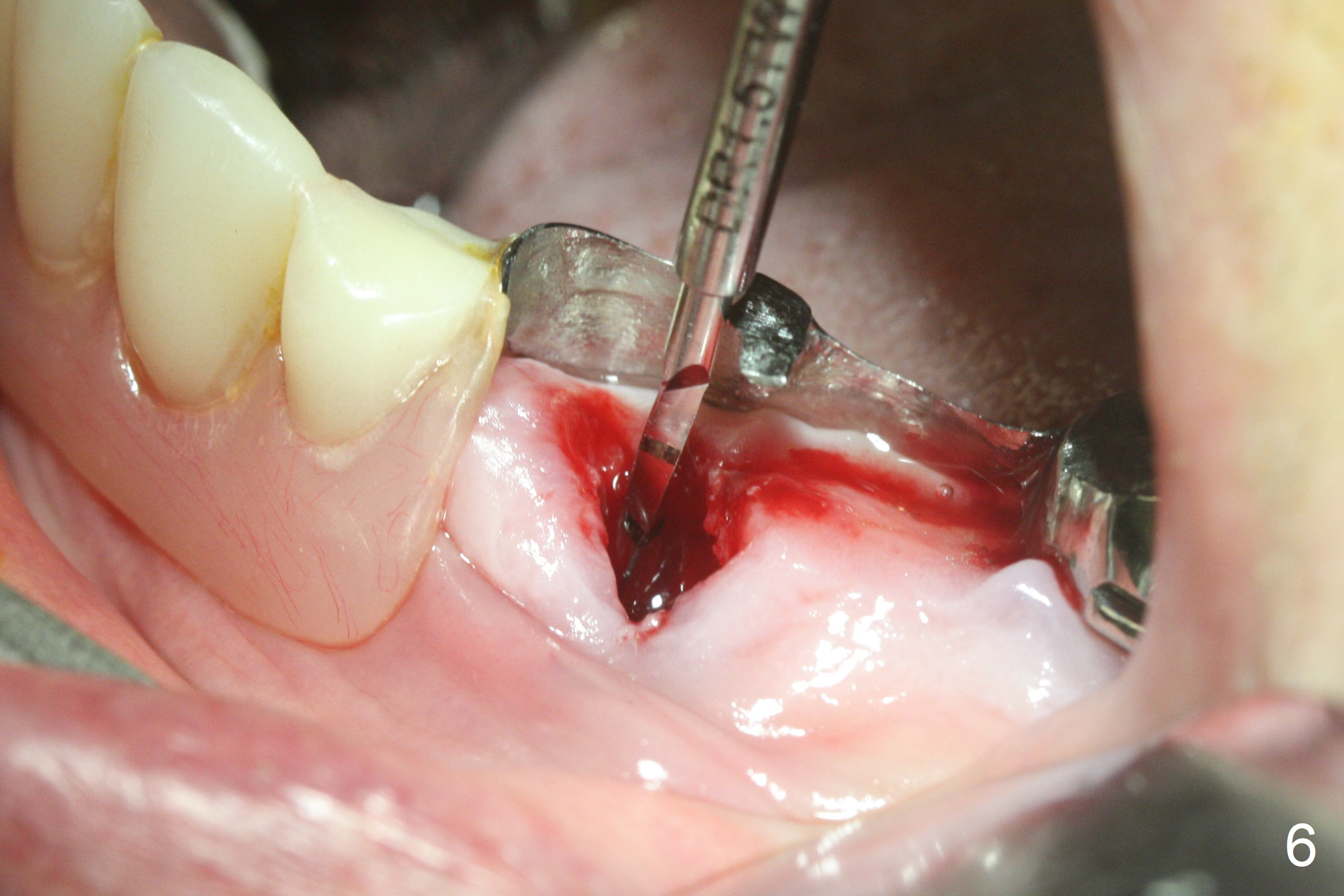
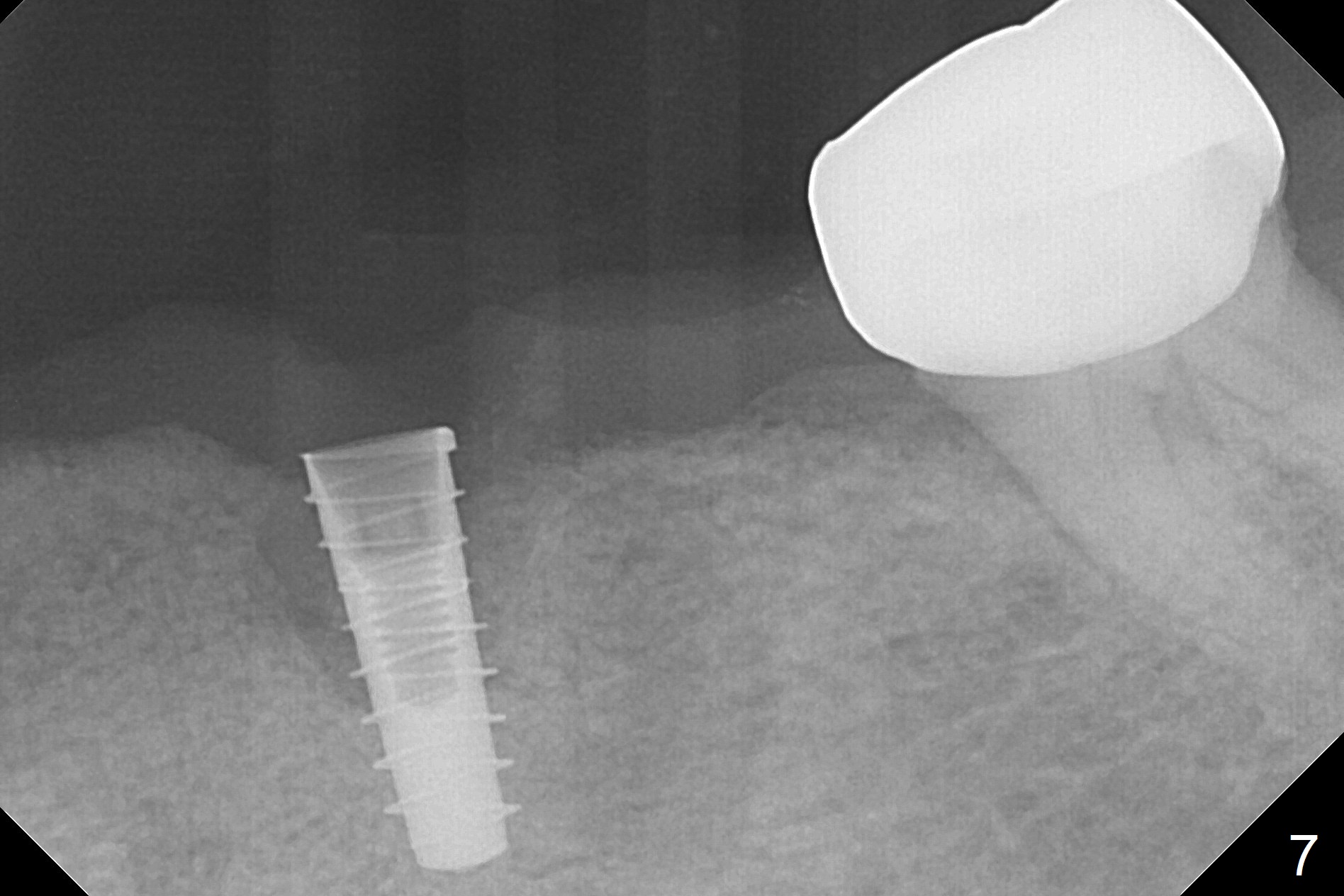
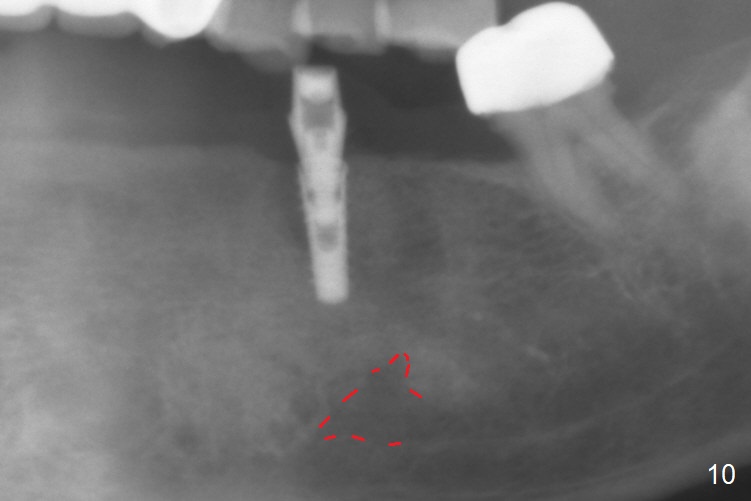
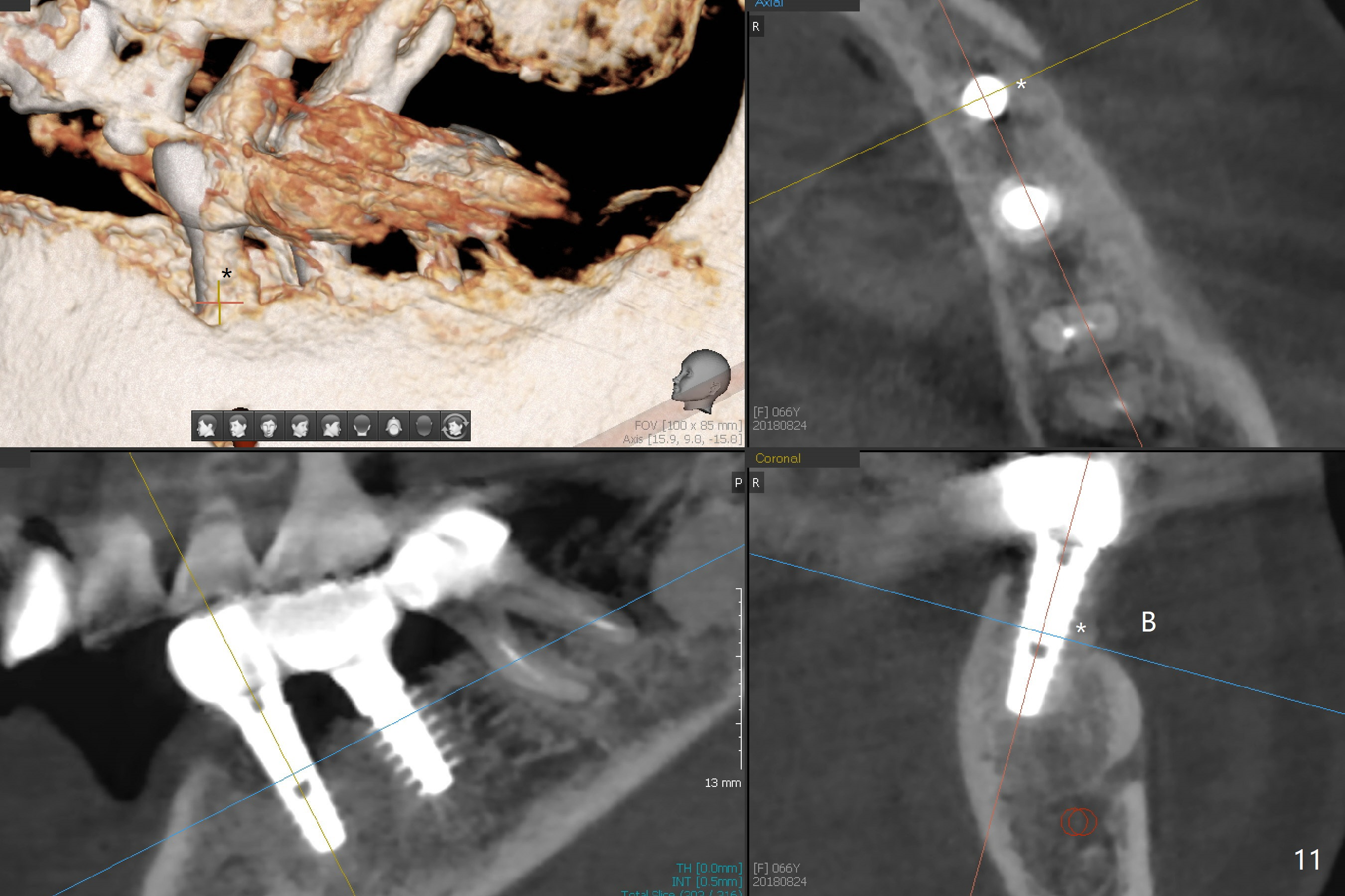
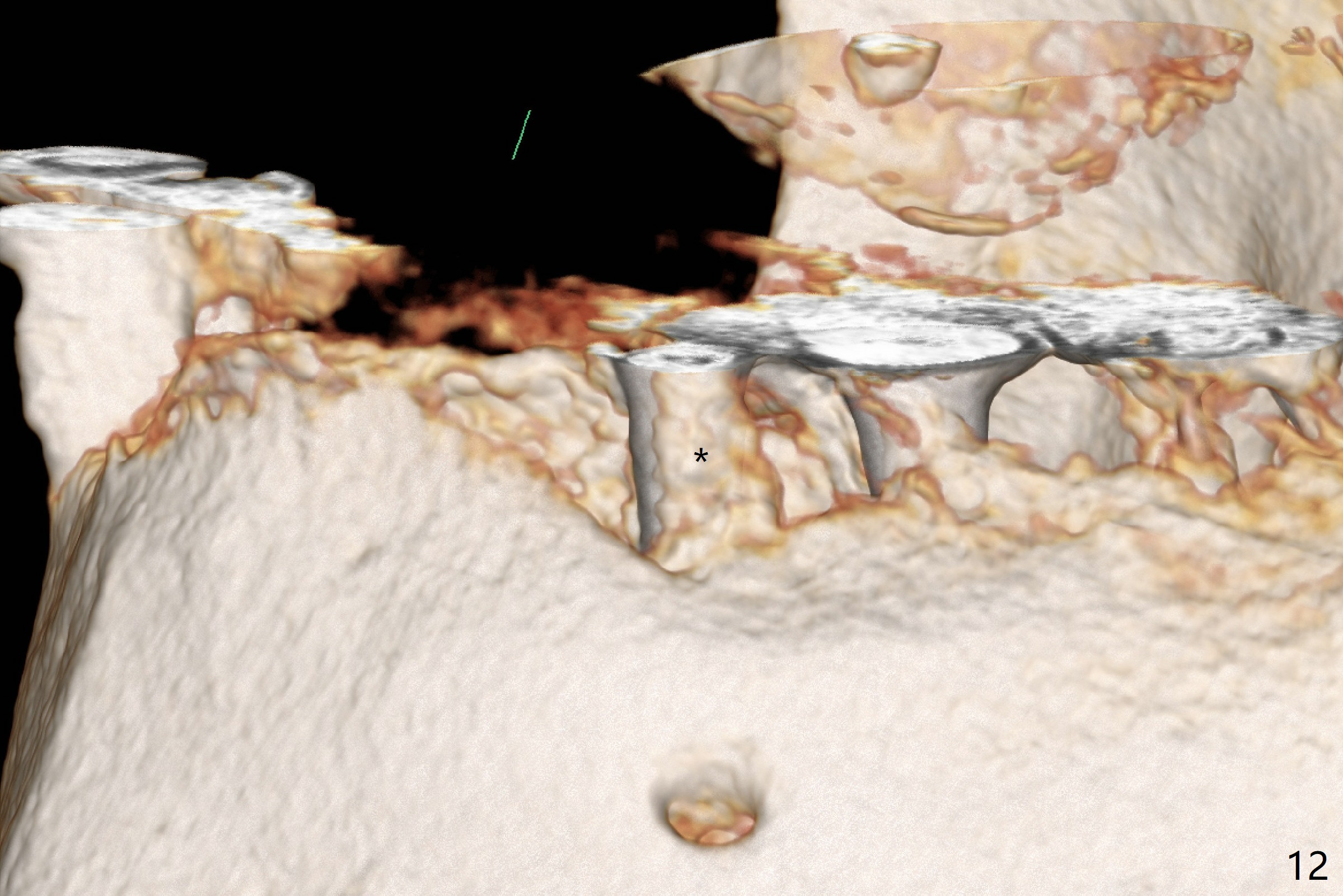
After removal of the pontic at #19 and retainer at #20 (Fig.1) and of vertically fractured root, the buccal plate is found to be defective (Fig.2 *). An implant will be placed as lingual as possible. Since the apex of the affected tooth is coronal to the Mental Loop (Fig.3 red dashed line), an osteotomy (Fig.4 yellow arrow) to be established in the mesial slope (blue dashed line) after extraction (black area) appears to be safer than that along the long axis of the tooth. The initial osteotomy is accomplished by free hand (Fig.5), but when the lower RPD is inserted, the superior end of the 1.5 mm pilot drill is distal (Fig.6). When the trajectory is corrected using the RPD as a surgical guide at the same depth (17 mm gingival level), brisk hemorrhage is from the osteotomy without severe pain. After hemostasis is achieved by packing the socket with Osteogen plug and bone graft and packing bone graft into the osteotomy, 3.3 mm Magic Drill is used for 14 mm. A 4x11 mm IBS implant is placed with 60 Ncm (Fig.7). The implant is then placed deeper, followed by placement of a 4.5x4(3) mm abutment and further bone graft (Fig.8). Finally the implant/abutment complex is apparently in an acceptable mesiodistal position with a large buccal gap which has been filled by bone graft (Fig.9 *). In fact the Mental Loop seems to have been not violated in the procedure (Fig.10). X-ray is taken 3 and 6 months postop. Bone graft (Fig.11,12 (CBCT) *) appears to remain over the buccal (B) surface of the implant coronally 13 months postop (7 months post cementation). The gingiva at #19 and 20 is apparently healthy 8 months post cementation except mild recession at #20 (Fig.13).
Return to
Lower Premolar Immediate
Implant #19
3,4
Xin Wei, DDS, PhD, MS 1st edition 07/11/2017, last revision 09/25/2018